Abstract
Objective
To characterize inappropriate shock delivery during pediatric in-hospital cardiac arrest (IHCA).
Design
Retrospective cohort study.
Setting
An international pediatric cardiac arrest quality improvement collaborative (PediRES-Q).
Patients
All IHCA events from 2015 to 2020 from the pediRES-Q Collaborative for which shock and ECG waveform data were available.
Interventions
None.
Measurements and Main Results
We analyzed 418 shocks delivered during 159 cardiac arrest events, with 381 shocks during 158 events at 28 sites remaining after excluding undecipherable rhythms. We classified shocks as 1) appropriate (VF or wide complex ≥150/min); 2) indeterminate (narrow complex ≥150/min or wide complex 100–149/min); or 3) inappropriate (asystole, sinus, narrow complex <150/min, or wide complex <100/min) based on the rhythm immediately preceding shock delivery. Of delivered shocks, 57% were delivered appropriately for VF or wide complex rhythms with a rate ≥ 150/min. Thirteen percent were classified as indeterminate. Thirty percent were delivered inappropriately for asystole (6.8%), sinus (3.1%), narrow complex <150/min (11%), or wide complex <100/min (8.9%) rhythms. Eighty-eight percent of all shocks were delivered in intensive care units or emergency departments, and 30% of those were delivered inappropriately.
Conclusions
The rate of inappropriate shock delivery for pediatric IHCA in this international cohort is at least 30%, with 23% delivered to an organized electrical rhythm, identifying opportunity for improvement in rhythm identification training.
Keywords: Defibrillation, children, ventricular tachycardia, ventricular fibrillation
INTRODUCTION
Approximately 15,000 children suffer in-hospital cardiac arrest (IHCA) in the United States each year.(1, 2) Cardiac rhythms amenable to defibrillation (ventricular fibrillation [VF] and pulseless ventricular tachycardia [pVT]) are documented by clinicians in up to 27% of pediatric IHCA events.(3) Early defibrillation is associated with improved outcomes in children with shockable rhythms and current American Heart Association (AHA) Pediatric Advanced Life Support (PALS) guidelines recommend both early defibrillation and high-quality cardiopulmonary resuscitation (CPR) in children suffering from cardiac arrest due to VF or pVT.(4, 5) In children with a first documented rhythm of VF/pVT, sustained return of spontaneous circulation (ROSC) ranges from 50% to 77%, with survival to discharge ranging from 21% to 43%.(3, 4, 6–8) In a single-center study of adult IHCA and OHCA patients, the rate of inappropriate shock delivery (defined as shock delivery to non-VF/pVT rhythms) was 26%, with 20% of all shocks delivered to an organized rhythm.(9) In contrast, the inappropriate interpretation of non-shockable rhythms as shockable by automated external defibrillators (AEDs) is only between 4 and 6%, and is typically due to artifact from chest compressions.(9, 10)
Characterization of inappropriate defibrillation attempts during pediatric cardiac arrest is unknown. Inappropriate attempts to defibrillate for non-shockable rhythms may result in harm due to conversion of organized rhythms into VF/pVT, myocardial injury, inappropriate interruption of chest compressions, or delay of alternative effective therapies.(11, 12) Understanding the character and burden of inappropriate shocks is necessary to develop targeted training. To address this knowledge gap, we aimed to characterize inappropriate shocks during pediatric IHCA in a large, international pediatric cardiac arrest quality collaborative.
METHODS
Study Design and Setting
We performed a retrospective cohort study using data collected between 2015–2020 from the Pediatric Resuscitation Quality (pediRES-Q) Collaborative (ClinicalTrials.gov: NCT02708134), a multi-center international collaborative of 50 children’s hospitals.(13) The study (Quality of Pediatric Resuscitation in a Multicenter Collaborative: an Observational Study) is approved by the Institutional Review Board of the Research Institute at the Children’s Hospital of Philadelphia (initial approval date July 14, 2015; effective approval date September 28, 2022; approval number 15–012099). Trained personnel collected data for pediatric cardiac arrest, including pre-existing conditions, demographics, and outcomes in accordance with standard Utstein-style definition for cardiac arrest.(14) The Data Coordinating Center (Children’s Hospital of Philadelphia) trains research staff, hosts, and performs quality assurance on data entered into the REDCap (Research Electronic Data Capture) tool.(15, 16) The study is also approved by local institutional review boards or research ethics boards, per regional institutional requirements, and meets criteria for a waiver of consent per Code of Federal Regulations 45 CFR 46.116(d) and 45 CFR 46.408(a) and in accordance with paragraph 26 in the Helsinki Declaration.
Patients
We included patients less than 18 years of age with at least one cardiac arrest submitted to pediRES-Q from 2015–2020 with complete monitor/defibrillator files (ZOLL R-Series, Chelmsford, MA) who received defibrillation during the IHCA event. Rhythms that were undecipherable due to artifact were excluded from analysis.
ECG Waveform Analysis
A pediatric electrophysiologist (DLA) and a pediatric cardiac intensivist (TTR) analyzed the waveform recorded by the monitor/defibrillator via the defibrillator pads immediately prior to shock delivery. They independently classified rhythms immediately prior to shock as: 1) appropriate (VF or wide complex ≥150/min); 2) indeterminate (narrow complex ≥150/min or wide complex 100–149/min); 3) inappropriate (asystole, sinus, narrow complex <150/min, or wide complex <100/min). We chose these categories to delineate between clearly appropriate shocks (i.e., VF or a wide complex tachycardia), shocks that may be appropriate in some clinical contexts (i.e., a narrow tachycardia without clear sinus origin or slower wide-complex tachycardias that may have been intended as cardioversion), and clearly inappropriate shocks. Investigators did not have access to clinical data while determining rhythm categories and all patients were presumed to be pulseless and in cardiac arrest as they were receiving CPR. Disagreements were resolved by consensus of the two reviewers, and none required arbitration by a third expert reviewer.
Data Analysis
We summarized demographic, clinical, and shock data using descriptive statistics. Data analysis was performed using R Statistical Software (v4.1.2; R Core Team 2021).
RESULTS
From January 2015 to December 2020, there were 1,554 cardiac arrest events in the pediRES-Q database with 884 available defibrillator files with 418 delivered shocks in 159 unique IHCA events. After excluding undecipherable shocks (N = 37), 381 shocks delivered during 158 events at 28 sites remained, with a median duration of CPR of 26 minutes (IQR 9, 47) minutes. The median age of patients was 6.4 years (IQR: 0.8–13.8), with 44 (28%) events in children less than 1 year, 47 (30%) in 1 to 8 year-olds, and 67 (42%) in 9 to 17 year-olds. Eighty-three (53%) of patients had a cardiac illness category and 139 (88%) events occurred in an intensive care unit (ICU) or emergency department. ROSC was achieved in 74 events (47%), return of circulation via ECMO in 37 events (23%), and 47 did not survive the event (30%). Ninety-eight patients (62%) survived to 24-hours and 61 (39%) survived to discharge (Table 1).
Of delivered shocks, 219 (57%) were delivered appropriately for VF (139, 36%) or wide complex rhythms with a rate ≥150/min (80, 21%) (Figure 1). Forty-nine (13%) were classified as indeterminate, delivered for narrow complex ≥150/min (31, 8.1%) or wide complex 100–149/min (18, 4.7%) rhythms. One-hundred and thirteen (30%) were delivered inappropriately for asystole (26, 6.8%), sinus (12, 3.1%), narrow complex <150/min (41, 11%), or wide complex <100/min (34, 8.9%) rhythms. Thus 23% of inappropriate shocks were for organized electrical rhythms. Furthermore, of shocks delivered in ICUs or emergency departments (N = 337), 101 (30%) were inappropriate. Of shocks delivered in other in-hospital locations (operating rooms or inpatient wards, N = 44, 12%), 27% were inappropriate (Figure 1).
Figure 1.
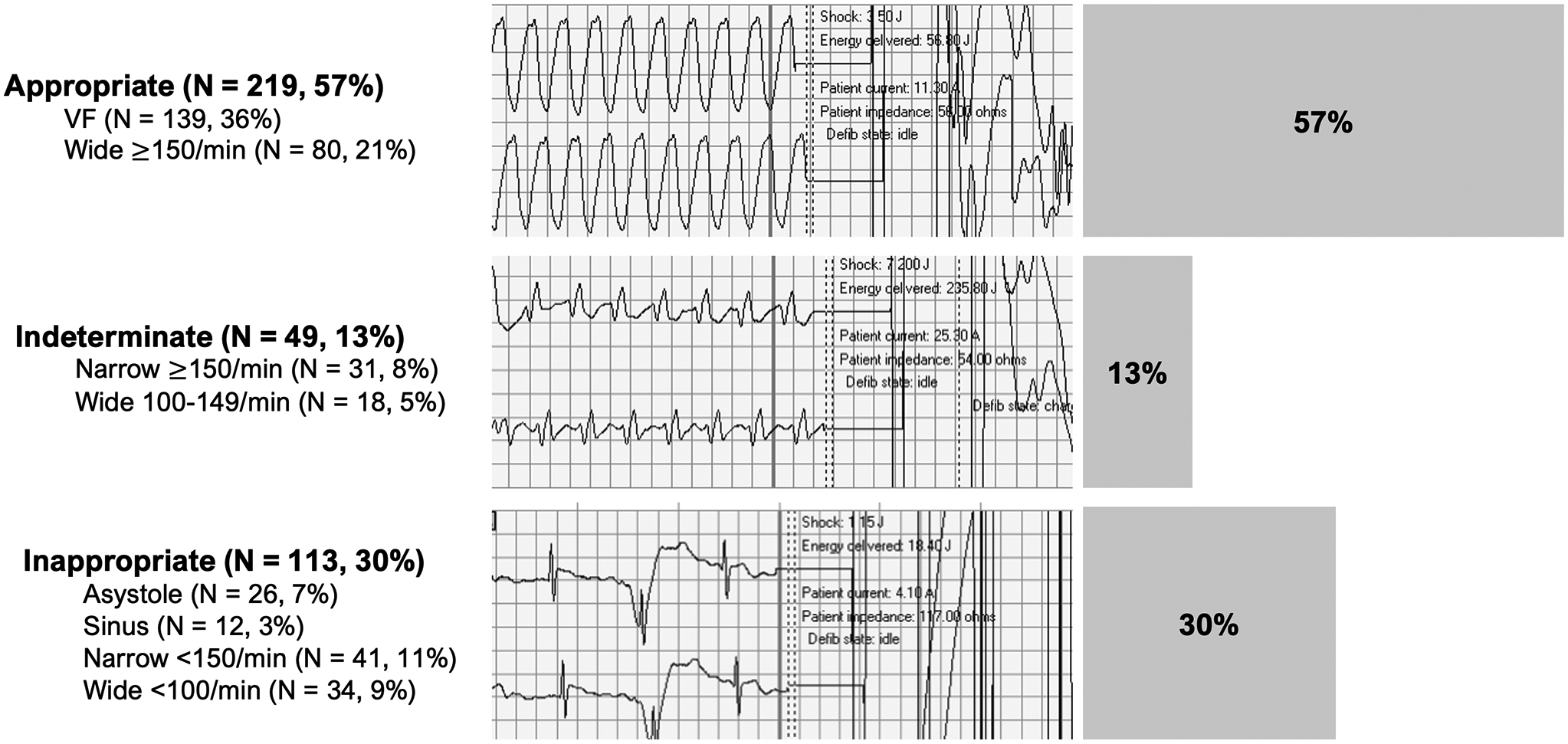
Rhythm categories with representative ECG waveforms
To evaluate for first shock accuracy, we conducted a subanalysis of available rhythms just prior to the first shock in each event. Seventy-two first rhythms were identified as VF/pVT by the treating clinicians; 66 had first rhythms that were decipherable. Despite the treating clinician classification as VF/pVT, 47 of 66 (71%) were delivered appropriately, 6 (9%) were classified as indeterminate, and 13 (20%) were delivered inappropriately.
DISCUSSION
In this large, international cohort of pediatric IHCA events requiring CPR, we found that 30% of shocks delivered were inappropriate, with 80% of the inappropriate shocks delivered to organized electrical rhythms: sinus rhythm, narrow complex <150/min, and wide complex <100/min. Ninety percent of inappropriate shocks were delivered in critical care and emergency department areas. In addition, of the 8.1% of events identified and self-reported as an initial rhythm of VF or pVT by the treating clinicians, only 71% were confirmed as appropriately shockable rhythms on expert review. This suggests opportunity for improvement in rhythm identification training.
Our findings in a pediatric international cohort are remarkably similar to findings in adults.(9) In a cohort of 635 manual shocks and 530 automated shocks, the authors found 26% of manual shocks were delivered to non-VF or non-VT rhythms, similar to our rate of 30%. In the same cohort, 8% of inappropriate shocks resulted in a rhythm change to either asystole, VF, or pVT. The rate of inappropriate shocks delivered by AEDs was significantly less at 6%. However, AEDs required longer pauses to perform rhythm interpretation. In children, automated rhythm detection is highly accurate (17), suggesting that automated rhythm interpretation may be less likely to deliver inappropriate shocks and may be a useful adjunct for IHCA.
Due to the nature of our data, we are unable to identify specific harms from inappropriate defibrillation attempts in this cohort. However, in porcine models the delivery of more shocks or higher energy shocks are associated with myocardial dysfunction.(11, 12, 18) In addition, organized rhythms can be converted into VF/pVT by inappropriate shock delivery.(9)
Even in critical care areas, such as ICUs and emergency departments, 30% of all shocks delivered were delivered inappropriately and 89% of all inappropriate shocks in our cohort were delivered in critical care areas. This suggests that despite the presence of highly trained personnel with experience in cardiac arrest care and advanced life support certification, inappropriate shocks are commonly delivered.
The rate of inappropriate clinician interpretation in our study calls into question the accuracy of prior studies that have relied on clinician interpretation of rhythm alone.(3, 4, 7) In our cohort, 20% of first shocked rhythms and 30% of all shocked rhythms were misinterpreted as shockable. It is unclear if differences between pediatric and adult shock efficacy (6, 19) are based upon unique pediatric physiology, or misinterpretation of non-shockable rhythms.
Our report characterizes actual rhythms for which shocks were delivered during pediatric IHCA and identifies challenges for clinicians when interpreting rhythms during CPR events. There are several limitations to our methodology: 1) we are unable to determine the immediate post-shock rhythm as the clinicians usually immediately re-started CPR, creating compression artifact, thus we cannot identify if the inappropriate shocks resulted in patient harm or if practice change is required to prevent harm. 2) We cannot determine true epidemiologic “prevalence” of shockable rhythms, as we were limited to IHCA events that were shocked and where there was complete and interpretable pre-shock rhythm data from monitor-defibrillator downloads, and 3) We may have underestimated the prevalence of inappropriate shocks. Our experts gave discretionary “benefit of the doubt” to clinicians, classifying any rhythm that did not meet usual FDA VF/pVT criteria into a liberally defined “indeterminate” category. Thus, our independent expert review and interpretation of the rhythms by a pediatric cardiac intensivist (TTR) and a pediatric electrophysiologist (DLA), ensured that they were very conservative in their prospective definition and report of “inappropriate shock”.
CONCLUSIONS
Across an international pediatric cardiac arrest network, the rate of inappropriate shock delivery for pediatric IHCA was at least 30%, with 23% delivered to an organized electrical rhythm. This presents an opportunity for improvement in rhythm identification training.
Supplementary Material
Supplementary Table 1. Demographic and resuscitation characteristics of subjects
Research In Context.
In pediatric in-hospital cardiac arrest, the rate of defibrillation attempts delivered to rhythms other than VF or pVT is not known
Previous pediatric studies have relied on bedside clinician reporting of rhythms, and the rate of inappropriate shock delivery in adults may be as high as 26%
In this cohort of international pediatric cardiac arrest patients, 30% of defibrillation attempts were delivered to non-shockable rhythms
At the Bedside.
In our pediatric in-hospital cardiac arrest cohort, 30% of shocks were delivered to non-shockable rhythms
No prior studies have examined the rate of inappropriate shock delivery in children
Clinicians should interpret rhythms carefully during compressions pauses in pediatric cardiac arrest and consider improving rhythm identification training
Funding
Unrestricted educational and research grant support of Laerdal Medical (2006–2013) and ZOLL Medical (2014–2022) to the Children’s Hospital of Philadelphia, and Pediatric Critical Care Medicine Endowed Chair Funds (VMN).
Disclosures
DEN and VMN disclose that The Children’s Hospital of Philadelphia receives support from an unrestricted research grant from ZOLL Medical (Chelmsford, MA). DEN and VMN disclose that The Children’s Hospital of Philadelphia receives funding from an unrestricted research grant from The American Heart Association (Chicago, IL). SVP is an employee of ZOLL Medical Corporation. The remaining authors have no disclosures to report.
Footnotes
Copyright Form Disclosure: Drs. Gray, Nadkarni, and Dewan’s institutions received funding from Zoll Medical. Dr. Atkins received funding from the National Institutes of Health (NIH) and the Pediatric Heart Network. Dr. Nadkarni’s institution received funding from the Laerdal Foundation, and RQI Partners; he received funding from Society of Critical Care Medicine as the President Elect 2023–2024. Dr. Pandit received funding from Zoll Medical; disclosed that he is an employee of Zoll Medical. Dr. Dewan received support for article research from the NIH. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Holmberg MJ, Ross CE, Fitzmaurice GM, et al. : Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States. Circ: Cardiovascular Quality and Outcomes 2019; 12 [PMC free article] [PubMed] [Google Scholar]
- 2.Atkins DL, Everson-Stewart S, Sears GK, et al. : Epidemiology and Outcomes From Out-of-Hospital Cardiac Arrest in Children. Circulation 2009; 119:1484–1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samson RA, Nadkarni VM, Meaney PA, et al. : Outcomes of In-Hospital Ventricular Fibrillation in Children. The New England Journal of Medicine 2006; 354:2328–39 [DOI] [PubMed] [Google Scholar]
- 4.Rodríguez-Núñez A, López-Herce J, García C, et al. : Pediatric defibrillation after cardiac arrest: initial response and outcome. Critical Care 2006; 10:R113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Topjian AA, Raymond TT, Atkins D, et al. : Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020; 142:S469–S523 [DOI] [PubMed] [Google Scholar]
- 6.Meaney PA, Nadkarni VM, Atkins DL, et al. : Effect of Defibrillation Energy Dose During In-Hospital Pediatric Cardiac Arrest. Pediatrics 2011; 127:e16–e23 [DOI] [PubMed] [Google Scholar]
- 7.Rodríguez-Núñez A, López-Herce J, del Castillo J, et al. : Shockable rhythms and defibrillation during in-hospital pediatric cardiac arrest. Resuscitation 2014; 85:387–391 [DOI] [PubMed] [Google Scholar]
- 8.Tibballs J, Carter B, Kiraly NJ, et al. : External and internal biphasic direct current shock doses for pediatric ventricular fibrillation and pulseless ventricular tachycardia. Pediatric Critical Care Medicine 2011; 12:14–20 [DOI] [PubMed] [Google Scholar]
- 9.Kramer-Johansen J, Edelson DP, Abella BS, et al. : Pauses in chest compression and inappropriate shocks: A comparison of manual and semi-automatic defibrillation attempts. Resuscitation 2007; 73:212–220 [DOI] [PubMed] [Google Scholar]
- 10.Calle PA, Mpotos N, Calle SP, et al. : Inaccurate treatment decisions of automated external defibrillators used by emergency medical services personnel: Incidence, cause and impact on outcome. Resuscitation 2015; 88:68–74 [DOI] [PubMed] [Google Scholar]
- 11.Tang W, Snyder D, Wang J, et al. : One-Shock Versus Three-Shock Defibrillation Protocol Significantly Improves Outcome in a Porcine Model of Prolonged Ventricular Fibrillation Cardiac Arrest. Circulation 2006; 113:2683–2689 [DOI] [PubMed] [Google Scholar]
- 12.Xie J, Weil MH, Sun S, et al. : High-Energy Defibrillation Increases the Severity of Postresuscitation Myocardial Dysfunction. Circulation 1997; 96:683–688 [DOI] [PubMed] [Google Scholar]
- 13.Niles DE, Duval-Arnould J, Skellett S, et al. : Characterization of Pediatric In-Hospital Cardiopulmonary Resuscitation Quality Metrics Across an International Resuscitation Collaborative*. Pediatric Critical Care Medicine 2018; 19:421–432 [DOI] [PubMed] [Google Scholar]
- 14.Nolan JP, Berg RA, Andersen LW, et al. : Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Template for In-Hospital Cardiac Arrest: A Consensus Report From a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia). Circulation 2019; 140:e746–e757 [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Minor BL, et al. : The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics 2019; 95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atkins DL, Scott WA, Blaufox AD, et al. : Sensitivity and specificity of an automated external defibrillator algorithm designed for pediatric patients. Resuscitation 2008; 76:168–174 [DOI] [PubMed] [Google Scholar]
- 18.Guensch DP, Yu J, Nadeshalingam G, et al. : Evidence for Acute Myocardial and Skeletal Muscle Injury after Serial Transthoracic Shocks in Healthy Swine. PLOS ONE 2016; 11:e0162245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nadkarni VM, Larkin GL, Peberdy MA, et al. : First Documented Rhythm and Clinical Outcome From In-Hospital Cardiac Arrest Among Children and Adults. JAMA 2006; 295:50–57 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Demographic and resuscitation characteristics of subjects


