Abstract
Objective:
In a large multi-site cohort of Veterans who underwent Roux-en-Y gastric bypass (RYGB) or laparoscopic sleeve gastrectomy (LSG), we compared the five-year suicidal ideation and attempt rates with matched non-surgical controls.
Summary Background Data:
Bariatric surgery has significant health benefits but has also been associated with adverse mental health outcomes.
Methods:
Five year rates of suicidal ideation and suicide attempts of Veterans who underwent RYGB or LSG from FY2000-2016 to matched non-surgical controls using sequential stratification using cumulative incidence functions (ideation cohort n=38,199; attempt cohort n=38,661 after excluding patients with past-year outcome events). Adjusted differences in suicidal ideation and suicide attempts were estimated using a Cox regression with a robust sandwich variance estimator.
Results:
In the matched cohorts for suicidal ideation analyses, the mean age was 53.47 years and the majority were males (78.7%) and white (77.7%). Over 40% were treated for depression (41.8%), had a non-recent depression diagnosis (40.9%), and 4.1% had past suicidal ideation or suicide attempts more than one year prior to index. Characteristics of the suicide attempt cohort were similar. Regression results found that risk of suicidal ideation was significantly higher for surgical patients (adjusted hazard ratio (aHR) = 1.21, 95% confidence interval (CI): 1.03–1.41), as was risk of suicide attempt (aHR=1.62, 95% CI: 1.22–2.15).
Conclusions:
Bariatric surgery appears to be associated with a greater risk of suicidal ideation and attempts than non-surgical treatment of patients with severe obesity, suggesting that patients need careful monitoring for suicidal ideation and additional psychological support after bariatric surgery.
Keywords: obesity, surgery, bariatric, gastric bypass, sleeve gastrectomy, veterans, suicidal ideation, suicide attempts
Mini Abstract
Bariatric surgery has significant health benefits but little is known about long-term risk of suicidal ideation or attempts. Bariatric surgery appears to be associated with a greater risk of suicidal ideation and attempts than non-surgical treatment of patients with severe obesity, suggesting that patients need careful monitoring for suicidal ideation and additional psychological support after bariatric surgery.
Introduction
Adults with mental health conditions are more likely to have severe obesity than adults without these conditions.1–4 The relationship between obesity and many mental health conditions is both convergent and bidirectional, and they are linked through clinical, neurobiological, genetic, and environmental factors.5–10 Over 50% of bariatric patients have current or past history of mental illness at the time of their surgery.11
There is also emerging evidence that bariatric surgery may increase the risk of suicide.12–17 Suicide ranks 10th among all causes of mortality in the US population, accounting for nearly 38,000 deaths in 2010.18 For every death by suicide, there are approximately 25 suicide attempts.19 One million U.S. adults make a suicide attempt each year, resulting in over 600,000 emergency room visits20 and nearly 200,000 hospitalizations each year.19 Bariatric surgery is also associated with alcohol use disorders and long-term opiate use, both of which can further increase the risk of suicide attempt and death. 12–17
Suicide death rates after bariatric surgery have been estimated to range from 2–6.6 per 10,000 people annually21,22, and 30-to-1800% higher than expected among patients with obesity managed non-surgically in cohort studies21,23–26 and systematic reviews.27,28 Peterhansel and colleagues27 identified 28 studies involving a total of 23,885 bariatric cases (their primary analysis excluded the Tindle study21), of which 15 did not describe timing or patient age about the suicide event (e.g., the timing of the event, the age of the patient) and the remainder provided some information. These prior studies have several limitations, including lack of a control group22,29–31, being limited to a single site or state21,23,24 or exclusion of currently performed procedures.25,31 Further, few studies have examined the antecedents of suicide death in terms of suicidal ideation or suicide attempts.
To address these major gaps, we conducted an analysis of a nationwide, retrospective cohort study among U.S. Veterans to examine post-surgical trends in suicidal ideation and attempts among veterans who underwent bariatric surgery in Veterans Administration (VA) bariatric centers from FY 2000–2016 compared to matched non-surgical controls. We hypothesized that suicidal ideation and suicide attempts would be higher in surgical patients due to several factors.12 These factors include the persistence or recurrence of medical comorbidities after surgery, inadequate weight loss and/or weight regain, variable effects of surgery on depressive symptoms and psychosocial functioning, disinhibition/impulsivity secondary to changes in pharmacokinetics of alcohol, increased drinking and alcohol use disorders after some bariatric procedures,17 persistent opioid use possibly associated with opioid use disorders,16 and decreases in antidepressant absorption after surgery.
Methods
Study Design and Study Population
We conducted a retrospective cohort study of VA patients who underwent bariatric surgery that were matched to a cohort of severely obese Veterans who did not undergo bariatric surgery. This study was approved by the Institutional Review Boards of the Durham VAMC and Kaiser Permanente Washington Health Research Institute. We identified 10,653 Veterans with procedure codes for any of three bariatric surgical procedures (open or laparoscopic Roux-en-Y gastric bypass (RYGB), laparoscopic sleeve gastrectomy (LSG)) in any VA bariatric center between 10/1/2000 and 9/30/2016. We excluded adjustable gastric banding procedures because they were rarely performed in the cohort and their use has recently declined rapidly worldwide. After applying additional standard exclusions that we have applied in prior analyses,16,17 the surgical cohort included 3,940 patients who underwent RYGB or LSG.
Since clinical eligibility criteria for surgery change over time, a sequential stratification matching approach was used to identify all potential non-surgical control patients for each bariatric surgery patient at their surgery index date using VA electronic health records (EHR).32–34 For each surgical patient, the identified set of eligible potential matches were clinically and demographically similar to the surgical patient but had not yet undergone bariatric surgery. Specifically, we required that potential matches exactly match their surgical patient in terms of sex, race (white/non-white), diabetes diagnosis, VA regional network, and a history of chronic prescription opioid use, depression treatment, or unhealthy alcohol use in the last two years. Additionally, we required that the potential matches be within 5 years of age from that of their surgical patients and have a similar BMI measurement within the 6 months before the surgery index date. Up to 10 matches with the closest BMI measurements to those of the surgical patient were selected among the potential matches.
Non-surgical control patients were allowed to match to more than one surgical patient at any time during the study period so long as they had an eligible BMI measurement. Non-surgical control patients could also receive bariatric surgery at a later point and contributed person-time to the control group until they received bariatric surgery. If non-surgical control patients later received bariatric surgery, their follow-up time was censored at the date of their surgery. The non-surgical control cohort consisted of 32,015 individual patients representing 35,995 matches.
Surgical patients and matched controls were excluded if they had an index date prior to October 1, 2001 (due to having less than one-year lookback for covariate construction). Patients were excluded if they had a prior year suicide attempt (for the suicide attempt analysis) or prior year ideation or attempt (for the suicidal ideation analysis) since post-surgical diagnoses of these events might be related to ongoing treatment for prior year attempt or ideation. Finally, patients were excluded if after the above exclusions, no matched case or control remained in a given risk set (eFigure 1).
Suicide Outcomes
Three diagnosis-based outcomes were compared between surgical and non-surgical cohorts: 1) suicidal ideation, 2) suicide attempt and 3) death from suicide up to 5 years after surgery. The first two outcomes were identified from inpatient and outpatient VA claims and death from suicide was identified from the cause of death field in the National Death Index (ICD-10 codes X60-84 or Y87). Suicidal ideation was identified based on ICD-9 code V62.84 and ICD-10 code R45.851. Suicide attempt was identified from ICD-9 codes E950-959 and ICD-10 codes X71-83, T14.91, T36-65 with a sixth character of 2 (with some exceptions) and T71 with a sixth character of 2. All outcomes were constructed as time to the first documented occurrence to enable assessment of differences in time until incident documentation of each of these three events. For the time to suicidal ideation outcome, time to first ideation, attempt, or death from suicide was included. For the time to suicide attempt outcome, time to attempt or death from suicide was included. Across all three outcomes, death for reasons other than suicide was considered a competing risk.
Statistical Analysis
Covariate balance between the surgical patients and non-surgical matches was evaluated using standardized differences.35 Unadjusted differences in the incidence of the three outcomes between surgical (LSG and RYGB pooled) and matched control cohorts was assessed via cumulative incidence functions using the Fine and Gray method36 to account for competing risks.
Adjusted differences in suicidal ideation and suicide attempts between surgical and non-surgical patients were estimated using a Cox regression with a robust sandwich variance estimator37 to account for the fact that the same individual could have been matched to multiple surgical patients. Covariate adjustment for the suicidal ideation analysis included demographics (age, sex, race), marital status, individual comorbidity indicators (alcohol use disorder, anxiety, bipolar disorder, cannabis use disorder, depression treatment, non-recent depression, eating disorder, opioid use disorder, other drug use disorder, psychosis, post-traumatic stress disorder, schizophrenia, tobacco use disorder) measured in the two years prior to index date, quartile indicators for diagnosed comorbidity index, past suicidal ideation or suicide attempt more than one year prior to index, and quartile indicators for counts of VA outpatient visits and VA outpatient mental health visits. Covariate adjustment in the suicide attempt analysis included the same variables, except past suicidal attempt more than one year prior to index was adjusted instead of past suicidal ideation or attempt. The proportional hazards assumption was satisfied after assessing via inspection of log(-log[survival]) curves, Schoenfeld residuals, and martingale residuals.38
There were too few suicidal deaths to examine the association between surgery and suicide death in regression analysis, so we conducted descriptive analyses only. The a priori level of statistical significance was 0.05 for all analyses and all were conducted with PROC PHREG and PROC LIFETEST using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Suicidal Ideation by Surgical and Non-surgical Patients
The final cohort for the suicidal ideation analysis consisted of 38,199, including 3,813 surgical patients and 34,386 matched non-surgical controls. The mean age was 53.51 years and the majority were males (78.8%) and white (77.7%; Table 1), with an average of 8 mental health outpatient visits in the prior year. Over 40% were treated for depression (41.2%), had a non-recent depression diagnosis (40.5%) and 4.1% had past suicidal ideation or suicide attempts more than one year prior to index. The surgical patients were more likely to be married (51.4% versus 43.6%, standardized mean difference [SMD] = 0.281) and had more outpatient visits than the matched non-surgical controls (mean of 20.78 versus 16.08 visits, SMD = 0.307). Mean follow-up was 4.6 and 4.5 years in the surgical patients and the matched non-surgical controls, respectively (median of 5.0 years in both arms).
Table 1.
Descriptive Statistics of Surgical and Non-surgical Cohorts in Ideation Analysis
| Total (n=38,199) | Received surgery (n=3,813) | Did not receive surgery (n=34,386) | SMD | |
|---|---|---|---|---|
| Age, mean (SD) | 53.51 (9.40) | 52.83 (9.52) | 53.59 (9.39) | 0.08 |
| Male, n (%) | 30103 (78.8%) | 2907 (76.2%) | 27196 (79.1%) | 0.068 |
| Race, n (%) | 0.036 | |||
| Black or African American | 6035 (15.8%) | 627 (16.4%) | 5408 (15.7%) | |
| Other/Unknown | 2483 (6.5%) | 272 (7.1%) | 2211 (6.4%) | |
| White | 29681 (77.7%) | 2914 (76.4%) | 26767 (77.8%) | |
| Marital status, n (%) | 0.281 | |||
| Married | 16962 (44.4%) | 1959 (51.4%) | 15003 (43.6%) | |
| Unmarried or unknown | 9801 (25.7%) | 590 (15.5%) | 9211 (26.8%) | |
| Previously married | 11436 (29.9%) | 1264 (33.1%) | 10172 (29.6%) | |
| Region, n (%) | 0.063 | |||
| Midwest | 6357 (16.6%) | 629 (16.5%) | 5728 (16.7%) | |
| Northeast | 7243 (19.0%) | 753 (19.7%) | 6490 (18.9%) | |
| Other | 201 (0.5%) | 8 (0.2%) | 193 (0.6%) | |
| South | 15399 (40.3%) | 1504 (39.4%) | 13895 (40.4%) | |
| West | 8999 (23.6%) | 919 (24.1%) | 8080 (23.5%) | |
| Risk Scorea, mean (SD) | 1.37 (1.05) | 1.43 (0.96) | 1.37 (1.05) | 0.062 |
| Comorbidities in prior year, n (%) | ||||
| Anxiety | 5342 (14.0%) | 556 (14.6%) | 4786 (13.9%) | 0.019 |
| Depression (treatment) | 15729 (41.2%) | 1649 (43.2%) | 14080 (40.9%) | 0.047 |
| Non-recent depression (7–24 months prior to index) | 15485 (40.5%) | 1685 (44.2%) | 13800 (40.1%) | 0.082 |
| Bipolar | 1803 (4.7%) | 204 (5.4%) | 1599 (4.7%) | 0.032 |
| Psychosis | 432 (1.1%) | 21 (0.6%) | 411 (1.2%) | 0.069 |
| Schizophrenia | 1189 (3.1%) | 47 (1.2%) | 1142 (3.3%) | 0.14 |
| Eating disorder | 194 (0.5%) | 61 (1.6%) | 133 (0.4%) | 0.123 |
| Alcohol use disorder | 1741 (4.6%) | 226 (5.9%) | 1515 (4.4%) | 0.069 |
| Opioid use disorder | 58 (0.2%) | 16 (0.4%) | 42 (0.1%) | 0.057 |
| Post-traumatic stress disorder | 7309 (19.1%) | 788 (20.7%) | 6521 (19.0%) | 0.043 |
| Cannabis use disorder | 376 (1.0%) | 28 (0.7%) | 348 (1.0%) | 0.03 |
| Tobacco use disorder | 5109 (13.4%) | 310 (8.1%) | 4799 (14.0%) | 0.187 |
| Other drug use disorder | 976 (2.6%) | 95 (2.5%) | 881 (2.6%) | 0.004 |
| Past suicide attempt everb, n (%) | 438 (1.1%) | 42 (1.1%) | 396 (1.2%) | 0.005 |
| Past suicidal ideation or suicide attempt everb, n (%) | 1207 (3.2%) | 114 (3.0%) | 1093 (3.2%) | 0.011 |
| Number of mental health-related outpatient visits in past year, mean (SD) | 8.08 (19.61) | 9.27 (17.72) | 7.94 (19.80) | 0.071 |
| Number of outpatient visits in past year, mean (SD) | 16.54 (15.75) | 20.78 (14.86) | 16.08 (15.78) | 0.307 |
Risk score was based on either Nosos or Diagnostic Cost Group (DCG) depending on year available (DCG was used by VA through 2006 then Nosos after)
More than 1 year prior to index date (individuals with suicidal ideation or suicide attempt within 1 year before index date were excluded from this cohort)
SD = standard deviation; SMD = standardized mean difference
Longer-term risk of incident suicidal ideation was greater for surgical patients than matched non-surgical controls (Figure 1). The 5-year incidence rates of suicidal ideation were 11.6 per 1,000 person-years for surgical patients and 9.0 per 1,000 person-years for matched controls. Results from the Cox regression found that risk of suicidal ideation was significantly greater for surgical patients (adjusted hazard ratio (aHR) = 1.21, 95% confidence interval: 1.03–1.41; Figure 2 and eTable 2) than matched controls.
Figure 1: Five-year, matched, unadjusted cumulative incidence of suicidal ideation and attempt among bariatric surgery cases and matched non-surgical controls.
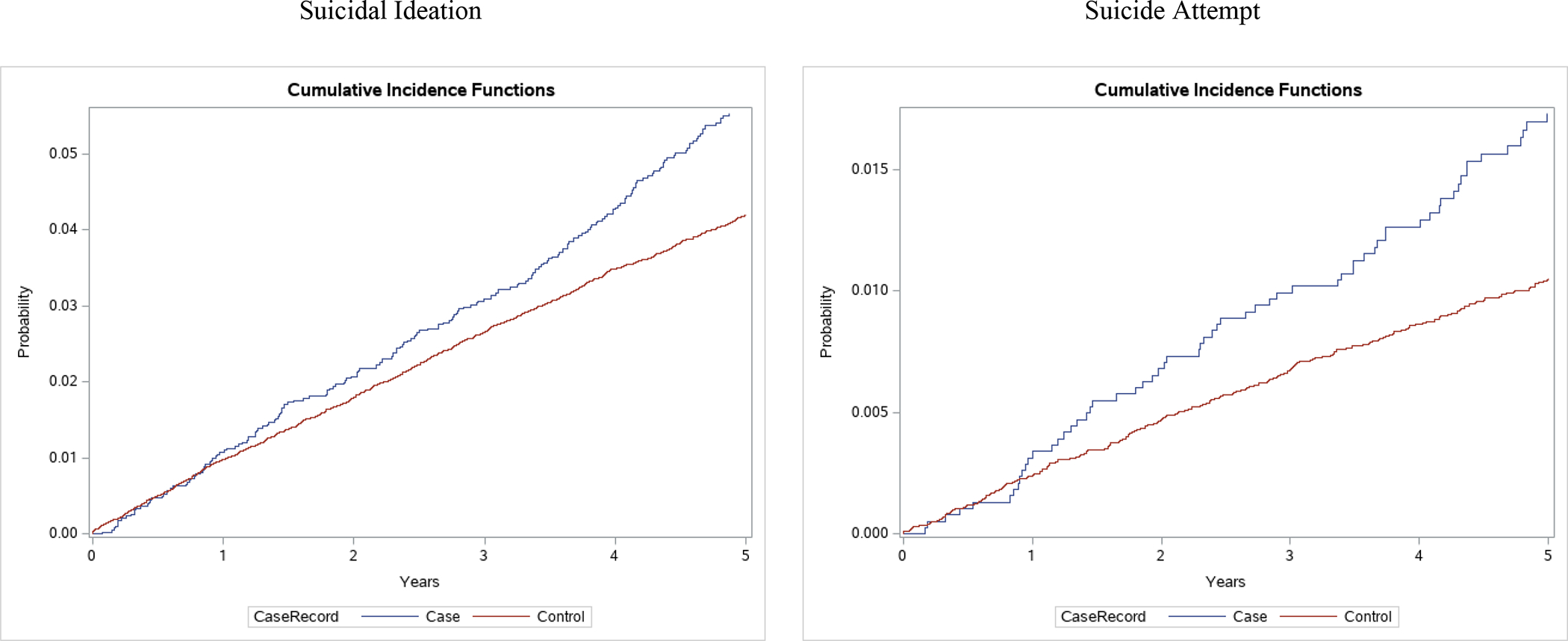
Figure 2: Multivariable adjusted Cox proportional hazard ratio estimates for risk of suicidal ideation and attempt comparing surgical cases vs. matched non-surgical controls, with 95% confidence intervals.
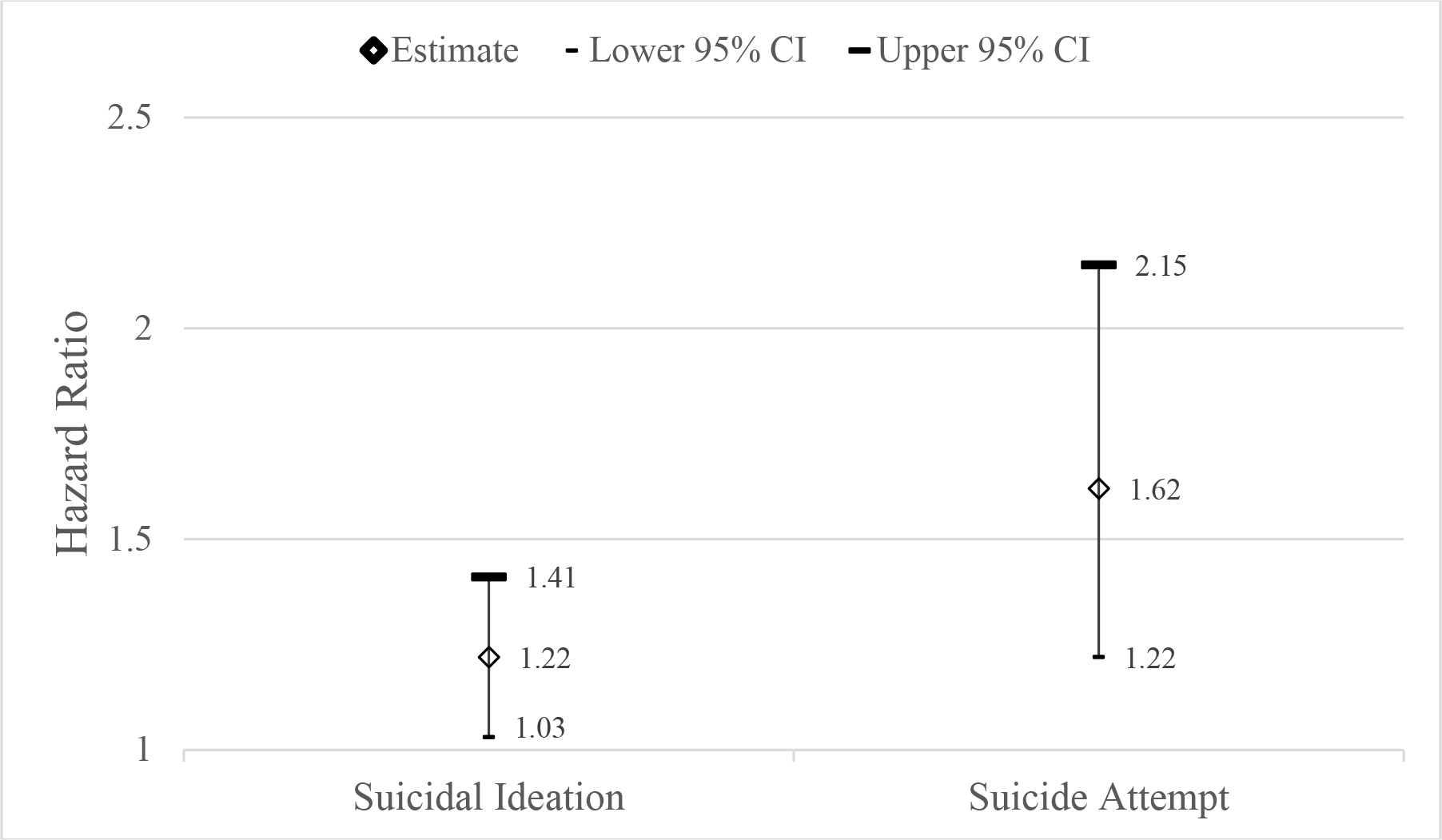
Note: adjusted for demographics (age, sex, race), marital status, quartile indicators for diagnosed comorbidity index, individual comorbidity indicators (alcohol use disorder, anxiety, bipolar disorder, cannabis use disorder, depression treatment, non-recent depression, eating disorder, opioid use disorder, other drug use disorder, psychosis, post-traumatic stress disorder, schizophrenia, tobacco use disorder), past suicidal ideation or suicide attempt more than one year prior to index in the ideation analysis (or past suicide attempt more than one year prior to index in the attempt analysis), and quartile indicators for counts of VA outpatient visits and VA outpatient mental health visits
Evaluation of patient characteristics associated with increased risk of suicidal ideation revealed that prior suicidal ideation or suicide attempt (aHR=2.73, 95% CI: 2.32–3.21; eTable 2) was associated with greater risk of a new suicidal ideation event, as was having more mental health-related outpatient visits in the year prior to index (compared to those with no visits, those with 2–7 visits had an aHR=1.63, 95% CI: 1.35–1.98 and those with 8+ visits had an aHR=2.07, 95% CI: 1.69–2.55). Older age was associated with a lower risk of a new suicidal ideation event (aHR=0.98 for an increase of one year, 95% CI: 0.97–0.98).
Suicide Attempt and Death by Surgical and Non-surgical Patients
The final cohort for the suicide attempt analysis consisted of 38,661, including 3,825 surgical patients and 34,836 matched non-surgical controls. While the suicide attempt cohort was slightly larger than the suicidal ideation cohort (eFigure 1), they had similar characteristics (eTable 1). Five-year risk of incident suicide attempt from the cumulative incidence function (Figure 1) was greater for surgical patients than matched non-surgical controls (Figure 1, right column). The 5-year incidence rates of suicide attempt were 3.6 per 1,000 person-years for surgical patients and 2.2 per 1,000 person-years for matched controls. Results from the Cox regression found that risk of suicide attempt was significantly higher for surgical patients (aHR=1.62, 95% confidence interval: 1.22–2.15; Figure 2 and eTable 2) than matched controls.
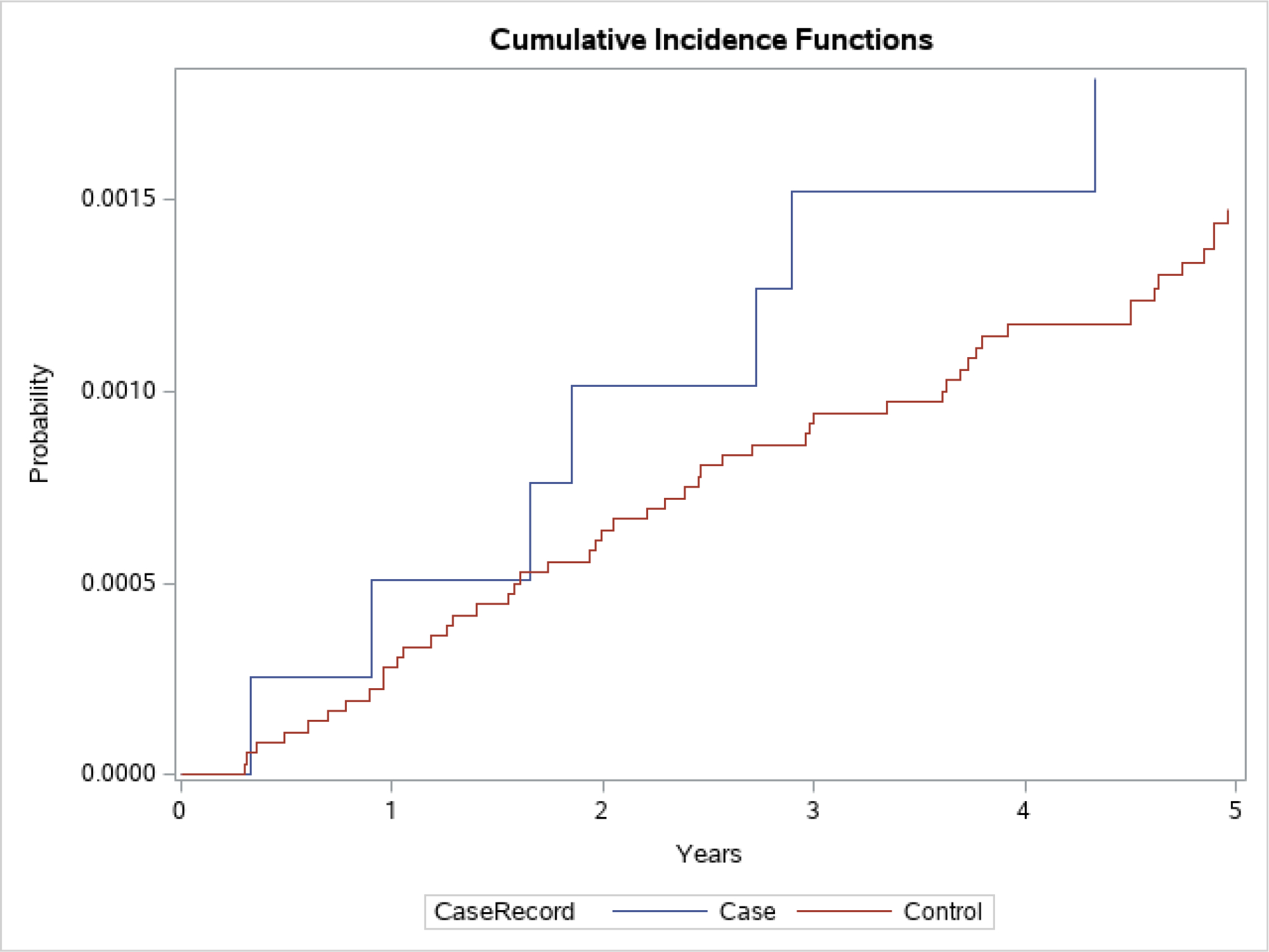
Patient characteristics associated with increased risk of a new suicide attempt included prior suicide attempt more than one year prior to index date (aHR=3.85, 95% CI: 2.63–5.63) and age (aHR=0.97 for an increase of one year, 95% CI: 0.96–0.98). Finally, the 5-year incidence of suicide death was 3.8 per 10,000 person-years for surgical patients and 3.1 per 10,000 person-years for matched controls (Figure 3).
Figure 3: Matched, unadjusted, cumulative incidence of suicide death among bariatric surgical cases and non-surgical controls.
Discussion
In this nationwide, retrospective cohort study of Veterans undergoing bariatric surgery from FY 2000–2016 and matched to non-surgical patients with severe obesity, bariatric surgery was associated with greater risk of suicidal ideation, attempt and death. This greater risk after surgery was affirmed in fully-adjusted analyses, suggesting that bariatric surgery may significantly increase the risk of suicidal ideation and attempts. These patients merit long-term monitoring to identify and ensure appropriate treatment of any emerging suicidal ideation or other changes in mental health symptoms.
To our knowledge, no prior study has compared incident suicidal ideation between surgical and non-surgical patients, so our finding of a modestly higher risk (aHR=1.21) is novel. Our results for suicide attempt (aHR=1.62) is similar to two prior analyses of the risk of non-fatal self-harm (aHR=1.74 from Neovius25; aHR=1.98 from Konttinen26) from the Swedish Obese Subjects study that did not include the sleeve gastrectomy procedure. We lacked the statistical power to conduct regression comparing suicide death, but our unadjusted results showing higher matched, unadjusted rates of suicide death in surgical patients is consistent with prior studies of cohorts in Utah23,24, Pennsylvania21 and two systematic reviews.27,28
Prior studies have also demonstrated that prior/pre-operative history of suicidal ideation and self-harm were associated with greater risk of new suicidal ideation or suicide attempt,22,29–31 which was also the most significant risk factor in this Veteran cohort. Prior studies have also demonstrated that older age was negatively associated with new suicidal ideation,30,31 consistent with our results. Given the significantly increased risk of recurrence of suicidal ideation and attempts in patients with a past history of these events, patients with this mental health history should be carefully screened pre-operatively and counseled regarding their possible greater post-surgical risk. Well-informed patients with a history of suicidal ideation or attempts may still wish to proceed with bariatric surgery, but these individuals deserve careful long-term post-operative follow-up.
Our research extends prior work by carefully matching surgical patients to non-surgical controls based on their pre-operative mental health characteristics, including demographics, diabetes diagnosis, BMI, VA regional network, and a history of chronic prescription opioid use, depression treatment, or unhealthy alcohol use. Additional research is also needed to identify whether clinical prediction models could help identify patients who are at the highest risk of suicidal ideation, attempt, and death after bariatric surgery. It is possible that prior clinical prediction tools may work well for this purpose, but these have not been validated in bariatric cohorts.
As noted previously, there are several possible mechanisms that could explain the consistent findings across studies of greater risk of suicide after bariatric surgery.12 These include the stress caused by either the persistence or recurrence of medical comorbidities after surgery (e.g., diabetes), inadequate weight loss and/or weight regain, possible negative effects of surgery on depressive symptoms and psychosocial functioning, disinhibition/impulsivity secondary to increased drinking, alcohol use disorders, or changes in pharmacokinetics of alcohol after some bariatric procedures, and decreases in antidepressant absorption after surgery. We have previously reported that this same cohort of veterans had a greater risk of incidence of chronic prescription opioid use16 and unhealthy alcohol use.17 Future research should examine potential mechanisms by which bariatric surgery may be associated with suicide risk, including the role of patient-perceived inadequacy of weight loss or subsequent weight regain. These findings are consistent with the overall pattern that bariatric surgery may worsen the overall mental health of a small, but not insignificant subset of patients, and may increase several risk factors for suicide. Thus, careful screening at baseline and follow-up using validated measures such as the Alcohol Use Disorders Identification Test (AUDIT-c) for alcohol problems and the Patient Health Questionnaire-9 (PHQ-9) for depression would be merited. In addition, consideration of a consent form that states risks clearly to patients, post-surgical monitoring for depression (with the PHQ-9) as well as for changes in alcohol use, opiate use (and other substances), and anxiety, and referral of patients with new or worsening symptoms or endorsement of suicidal ideation are warranted. These changes could afford patients the greatest possible chance for early detection and treatment of mental health issues.
This study has several limitations that should be acknowledged. First, this study of Veterans may not generalize to non-Veterans undergoing bariatric surgery. Veterans obtaining VA care are predominantly men, so bariatric surgery patients in VA are mostly men (76%), whereas women are a vast majority of non-VA bariatric surgery cohorts. Thus, these results may not generalize to non-Veteran cohorts. Second, confounding in this retrospective cohort study was reduced via sequential stratification matching but residual unobserved confounding may persist after matching.39 Third, given sample size and statistical constraints related to the number of variables that could be accommodated in the matching process, we could not match on every available characteristic and BMI imbalances in two cohorts were statistically but likely not clinically significant. The estimated effect estimates represent associations and not necessarily the causal effect of bariatric surgery on suicide risk. Fourth, all treatment and visit data were identified from VA EHR data only, so treatments obtained outside VA were not ascertained. Finally, as mentioned previously, we did not have access to data on self-reported depression symptoms, so we cannot ascertain differences in depression symptom severity across groups. Patients who receive bariatric surgery may be more engaged in VA care, so outcome ascertainment of outcomes may be biased if they are more likely to seek care in VA.
Conclusion
Compared with matched non-surgical patients with severe obesity, bariatric surgery was associated greater risk of suicidal ideation and attempts, suggesting that patients need carefully monitoring for suicidal ideation and additional psychological support after bariatric surgery.
Supplementary Material
ACKNOWLEDGEMENTS
Funding/Support:
Dr. Maciejewski was also supported by a Research Career Scientist award from the Department of Veterans Affairs (RCS 10-391) and by the Center of Innovation to Accelerate Discovery and Practice Transformation (CIN 13-410) at the Durham VA Health Care System.
Role of the Sponsor:
The opinions expressed are those of the authors and not necessarily those of the Department of Veterans Affairs, the United States Government, Duke University, the Kaiser Permanente Washington Health Research Institute, or the University of Washington.
Footnotes
Conflict of Interest Disclosures: Dr. Maciejewski reports research grants for National Institutes of Health (NIH) and Veterans Affairs Health Services Research and Development Service outside of the submitted work, and ownership of Amgen stock due to his spouse’s employment. Dr. Arterburn reports research grants from NIH and PCORI outside of the submitted work. Dr. Bradley reports research grants from NIH, Agency for Healthcare Research and Quality (AHRQ) and work for NCQA outside of the submitted work. All other authors have no conflicts of interest to disclose.
REFERENCES
- 1.McIntyre RS, Konarski JZ, Wilkins K, Soczynska JK, Kennedy SH. Obesity in bipolar disorder and major depressive disorder: results from a national community health survey on mental health and well-being. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2006;51(5):274–280. [DOI] [PubMed] [Google Scholar]
- 2.Simon GE, Ludman EJ, Linde JA, et al. Association between obesity and depression in middle-aged women. General hospital psychiatry. 2008;30(1):32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simon GE, Von Korff M, Saunders K, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63(7):824–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.M DEH, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World psychiatry : official journal of the World Psychiatric Association. 2011;10(1):52–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu CS, Carvalho AF, Mansur RB, McIntyre RS. Obesity and bipolar disorder: synergistic neurotoxic effects? Advances in therapy. 2013;30(11):987–1006. [DOI] [PubMed] [Google Scholar]
- 6.Taylor VH, McIntyre RS, Remington G, Levitan RD, Stonehocker B, Sharma AM. Beyond pharmacotherapy: understanding the links between obesity and chronic mental illness. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2012;57(1):5–12. [DOI] [PubMed] [Google Scholar]
- 7.Hryhorczuk C, Sharma S, Fulton SE. Metabolic disturbances connecting obesity and depression. Frontiers in neuroscience. 2013;7:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schur E, Godfrey KM, Dansie E, Buchwald D, Pagoto S, Afari N. Can familial factors account for the association of body mass index with poor mental health in men or women? General hospital psychiatry. 2013;35(5):502–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kao AC, Muller DJ. Genetics of antipsychotic-induced weight gain: update and current perspectives. Pharmacogenomics. 2013;14(16):2067–2083. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz TL, Nihalani N, Virk S, Jindal S, Chilton M. Psychiatric medication-induced obesity: treatment options. Obes Rev. 2004;5(4):233–238. [DOI] [PubMed] [Google Scholar]
- 11.Fisher D, Coleman KJ, Arterburn DE, et al. Mental illness in bariatric surgery: A cohort study from the PORTAL network. Obesity (Silver Spring). 2017;25(5):850–856. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell JE, Crosby R, de Zwaan M, et al. Possible risk factors for increased suicide following bariatric surgery. Obesity (Silver Spring). 2013;21(4):665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ertelt TW, Mitchell JE, Lancaster K, Crosby RD, Steffen KJ, Marino JM. Alcohol abuse and dependence before and after bariatric surgery: a review of the literature and report of a new data set. Surg Obes Relat Dis. 2008;4(5):647–650. [DOI] [PubMed] [Google Scholar]
- 14.King WC, Chen JY, Mitchell JE, et al. Prevalence of alcohol use disorders before and after bariatric surgery. Jama. 2012;307(23):2516–2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raebel MA, Newcomer SR, Reifler LM, et al. Chronic use of opioid medications before and after bariatric surgery. Jama. 2013;310(13):1369–1376. [DOI] [PubMed] [Google Scholar]
- 16.Maciejewski ML, Smith VA, Berkowitz TSZ, et al. Long-term opioid use after bariatric surgery. Surg Obes Relat Dis. 2020;16(8):1100–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maciejewski ML, Smith VA, Berkowitz TSZ, et al. Association of Bariatric Surgical Procedures With Changes in Unhealthy Alcohol Use Among US Veterans. JAMA Netw Open. 2020;3(12):e2028117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murphy SL, Xu JX, Kochanek KD. Deaths: Preliminary data for 2010. National Vital Statistics Reports. 2012;60(4):1–31. [PubMed] [Google Scholar]
- 19.Crosby AE, Han B, Ortega LA, et al. Suicidal thoughts and behaviors among adults aged >/=18 years--United States, 2008–2009. Morbidity and mortality weekly report Surveillance summaries. 2011;60(13):1–22. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2008 Emergency Department Summary Tables Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/nhamcsed2008.pdf. Published 2012. Updated January 6, 2012. Accessed February 22, 2012, 2012.
- 21.Tindle HA, Omalu B, Courcoulas A, Marcus M, Hammers J, Kuller LH. Risk of suicide after long-term follow-up from bariatric surgery. The American journal of medicine. 2010;123(11):1036–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kauppila JH, Santoni G, Tao W, et al. Risk Factors for Suicide After Bariatric Surgery in a Population-based Nationwide Study in Five Nordic Countries. Ann Surg. 2022;275(2):e410–e414. [DOI] [PubMed] [Google Scholar]
- 23.Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–761. [DOI] [PubMed] [Google Scholar]
- 24.Adams TD, Davidson LE, Litwin SE, et al. Health benefits of gastric bypass surgery after 6 years. Jama. 2012;308(11):1122–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neovius M, Bruze G, Jacobson P, et al. Risk of suicide and non-fatal self-harm after bariatric surgery: results from two matched cohort studies. The lancet Diabetes & endocrinology. 2018;6(3):197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Konttinen H, Sjoholm K, Jacobson P, Svensson PA, Carlsson LMS, Peltonen M. Prediction of Suicide and Nonfatal Self-harm After Bariatric Surgery: A Risk Score Based on Sociodemographic Factors, Lifestyle Behavior, and Mental Health: A Nonrandomized Controlled Trial. Ann Surg. 2021;274(2):339–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peterhansel C, Petroff D, Klinitzke G, Kersting A, Wagner B. Risk of completed suicide after bariatric surgery: a systematic review. Obes Rev. 2013;14(5):369–382. [DOI] [PubMed] [Google Scholar]
- 28.Castaneda D, Popov VB, Wander P, Thompson CC. Risk of Suicide and Self-harm Is Increased After Bariatric Surgery-a Systematic Review and Meta-analysis. Obes Surg. 2019;29(1):322–333. [DOI] [PubMed] [Google Scholar]
- 29.Gordon KH, King WC, White GE, et al. A longitudinal examination of suicide-related thoughts and behaviors among bariatric surgery patients. Surg Obes Relat Dis. 2019;15(2):269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wnuk S, Parvez N, Hawa R, Sockalingam S. Predictors of suicidal ideation one-year post-bariatric surgery: Results from the Toronto Bari-Psych Cohort Study. Gen Hosp Psychiatry. 2020;63:39–45. [DOI] [PubMed] [Google Scholar]
- 31.Morgan DJR, Ho KM, Platell C. Incidence and Determinants of Mental Health Service Use After Bariatric Surgery. JAMA Psychiatry. 2020;77(1):60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kennedy EH, Taylor JM, Schaubel DE, Williams S. The effect of salvage therapy on survival in a longitudinal study with treatment by indication. Statistics in medicine. 2010;29(25):2569–2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li YP, Propert KJ, Rosenbaum PR. Balanced Risk Set Matching. Journal of the American Statistical Association. 2001;96(455):870–882. [Google Scholar]
- 34.Lu B Propensity Score Matching with Time-Dependent Covariates. Biometrics. 2005;61(3):721–728. [DOI] [PubMed] [Google Scholar]
- 35.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fine JP, Gray RJ. A Proportional Hazards Model for the Subdistribution of a Competing Risk. Journal of the American Statistical Association. 1999;94:496–509. [Google Scholar]
- 37.Lin DY, Wei LJ. The Robust Inference for the Proportional Hazards Model. Journal of the American Statistical Association. 1989;84(408):1074–1078. [Google Scholar]
- 38.Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. 2000. [Google Scholar]
- 39.Flum DR. Administrative data analyses in bariatric surgery--limits of the technique. Surg Obes Relat Dis. 2006;2(2):78–81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


