Abstract
Progressive external ophthalmoplegia (PEO), characterized by ptosis and impaired eye movements, is a clinical syndrome with an expanding number of etiologically distinct subtypes. Advances in molecular genetics have revealed numerous pathogenic causes of PEO, originally heralded in 1988 by the detection of single large-scale deletions of mitochondrial DNA (mtDNA) in skeletal muscle of people with PEO and Kearns–Sayre syndrome. Since then, multiple point variants of mtDNA and nuclear genes have been identified to cause mitochondrial PEO and PEO-plus syndromes, including mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) and sensory ataxic neuropathy dysarthria ophthalmoplegia (SANDO). Intriguingly, many of those nuclear DNA pathogenic variants impair maintenance of the mitochondrial genome causing downstream mtDNA multiple deletions and depletion. In addition, numerous genetic causes of nonmitochondrial PEO have been identified.
DEFINITION OF PROGRESSIVE EXTERNAL OPHTHALMOPLEGIA
Progressive external ophthalmoplegia (PEO, also known as chronic progressive external ophthalmoplegia [CPEO]) is a clinical syndrome that was defined by Lewis P. Rowland in the 1992 Handbook of Clinical Neurology by the following features: (1) progressive ptosis and impaired mobility of the eyes; (2) bilaterality; (3) affected muscles are innervated by more than one nerve; (4) pupils are spared; (5) gradual progression over months or years; and (6) there are no remissions or exacerbations (Rowland, 1992). In addition, “no evidence of a specific disorder” (e.g., myasthenia gravis, thyroid disorder, or myotonic dystrophy) was an exclusionary criterion. However, in the thirty-plus years since Rowland’s original definition, scientific advances—particularly in molecular genetics—have defined multiple etiologically distinct forms of PEO. Accordingly, exclusion of specific disorders has become less relevant to diagnosing PEO, while inclusion of genetically defined disorders has gained importance in delineating subtypes of this syndrome. Thus, this chapter focuses on molecular advances in our understanding of the causes and reclassification of subtypes of PEO that have been reported since the previous Handbook chapter on this subject. Because many of the PEO variants have been linked to pathogenic variants of mitochondrial or nuclear DNA that are critical for mitochondrial functions, it is appropriate to feature PEO in this Handbook of Clinical Neurology focused on mitochondrial diseases.
HISTORICAL BACKGROUND
The first case of PEO was described 1868 by Dr. Albrech von Gräefe, who reported a woman of unspecified age with partial ptosis and complete rigidity of both eyes, with preservation of pupillary muscles that appeared static over 6 years (Von Gräefe, 1868). The striking isolated symmetric extraocular muscle weakness was associated with absent to mild strabismus, without other systemic clinical manifestations. Dr. von Gräefe attributed the syndrome to defects in the ocular nerves, given muscle from a prior case with diplopia showed no macro- or microscopic abnormalities and because eye movements require little force from muscle. As well-documented in Dr. Rowland’s previous chapter (Rowland, 1992), subsequent reports of progressive ophthalmoplegia primarily attributed the condition to neuronal degeneration (Hutchinson, 1879; Beaumont, 1890; Wilbrand and Saenger, 1900; Langdon and Cadwalader, 1928; Marburg, 1936; Hassler, 1953); however, Dr. Ernst Fuchs suggested that the weakness was due to isolated muscular dystrophy based upon findings in a superior levator biopsy (Fuchs, 1890).
In the 1930s, reports of ophthalmoplegia in association with muscular dystrophy-like limb weakness (Martin, 1936; Elliott, 1939), followed by reports of histological evidence of myopathy (Sandifer, 1946; Kiloh and Nevin, 1951) with absence of pathology in oculomotor nuclei (Beckett and Netsky, 1953; Schwarz and Liu, 1954), indicated myopathic etiologies for PEO. Further complexity of PEO became evident with cases of ocular myopathy with neural involvement, including peripheral neuropathy, ataxia, or spinal cord involvement (Rosenberg et al., 1968), which Dr. David Drachman described as “ophthalmoplegia-plus” (Drachman, 1968). A clinically distinct form of ophthalmoplegia-plus, Kearns–Sayre syndrome, was characterized by the triad of external ophthalmoplegia, retinitis pigmentosa, and heart block (Kearns and Sayre, 1958).
The application of a modified-Gomori trichrome histochemical stain to skeletal muscle revealed ragged-red fibers (RRFs), a sign of abnormal proliferation of mitochondria in subsarcolemmal regions of the skeletal muscle of patients with progressive ophthalmoplegia (Olson et al., 1972), a seminal observation that indicated mitochondrial pathology as a key factor in many cases of PEO.
MITOCHONDRIAL PROGRESSIVE EXTERNAL OPHTHALMOPLEGIA (PEO)
After Dr. William Olson’s initial report of seven individuals with RRFs in “oculocraniosomatic neuromuscular disease,” multiple other case series reinforced the association of PEO with RRFs (DiMauro et al., 1973; Pongratz et al., 1979; Mussini et al., 1984; Petty et al., 1986; Rowland et al., 1991; Serratrice, 1991). The application of cytochrome c oxidase (COX, mitochondrial complex IV) and succinate dehydrogenase (SDH, mitochondrial complex II) histochemical stains revealed that many of the RRFs were COX-deficient and SDH-positive or had excessive SDH activity, so-called ragged-blue fibers (Olson et al., 1972; Muller-Hocker et al., 1983; Yamamoto and Nonaka, 1988; Mita et al., 1989; Reichmann et al., 1991).
PEO is one of the most common clinical manifestations of mitochondrial disease; in the Nation-wide Italian Collaborative Network of Mitochondrial Disease, more than half of the genetically confirmed mitochondrial disease subjects had ocular myopathy (399/722, 55.3%), while in the North American Mitochondrial Disease Consortium (NAMDC) Registry, over 20% of genetically diagnosed participants had ptosis (196/666, 29.4%) or PEO (137/666, 20.6%) (Orsucci et al., 2017; Barca et al., 2020).
Mitochondrial PEO begins insidiously and progresses slowly and symmetrically such that many patients are initially unaware of the problem, in part because many do not develop diplopia; one study reported that 8 of 52 patients (15%) with mitochondrial PEO were aware of abnormal extraocular motility, and only 5 of 49 (10%) with ophthalmoplegia had diplopia (Petty et al., 1986).
The seemingly straightforward task of defining PEO has dissenting opinions. While there is consensus that mitochondrial PEO is defined by the presence of ptosis, progressive external ophthalmoplegia, or, as in most cases, both (Moraes et al., 1989; Rowland et al., 1991; Rowland, 1992; Van Goethem et al., 2003b; Aure et al., 2007; Goldstein and Falk, 2013 [Updated 2019 Jan 31]), some clinicians view this syndrome as a pure extraocular myopathy (Mancuso et al., 2015; Orsucci et al., 2017). Others consider PEO to be a generalized myopathy with extraocular, oropharyngeal, and skeletal muscle involvement (Aure et al., 2007; Barca et al., 2020; Emmanuele et al., 2022). In the majority of mitochondrial PEO, skeletal muscles demonstrate some clinical weakness, mitochondrial histological abnormalities (RRF and COX-deficient myofibers), or genetic defects (e.g., single or multiple deletions or depletion of mtDNA) (Aure et al., 2007). Consequently, consensus criteria for mitochondrial syndromes defined mitochondrial PEO clinically by ptosis, PEO, or both, but noted limb myopathy, exercise intolerance, and dysphagia may also be present (Emmanuele et al., 2022).
In 1988, the ground-breaking identification of single large-scale deletions of mitochondrial DNA (mtDNA) by Drs. Ian Holt, Anita Harding, and John Morgan-Hughes heralded the molecular genetic era of mitochondrial disease research (Holt et al., 1988). Later that year, Drs. Massimo Zeviani, Salvatore DiMauro, Rowland, and colleagues as well as other groups reported the association of mtDNA single deletions with Kearns–Sayre syndrome and with PEO (Fig. 2.1) (Lestienne and Ponsot, 1988; Ozawa et al., 1988; Zeviani et al., 1988; Holt et al., 1989; Johns et al., 1989; Moraes et al., 1989). Subsequently, the phenotypic spectrum of mtDNA single deletions was expanded by the identification of these mutations in infants with Pearson syndrome, a severe, typically infantile onset sideroblastic anemia that is often fatal (Rötig et al., 1990; McShane et al., 1991). Follow-up of long-term survivors of Pearson syndrome developed PEO or KSS further broadening the clinical spectrum of mtDNA single deletions not only across affected individuals but within single patients.
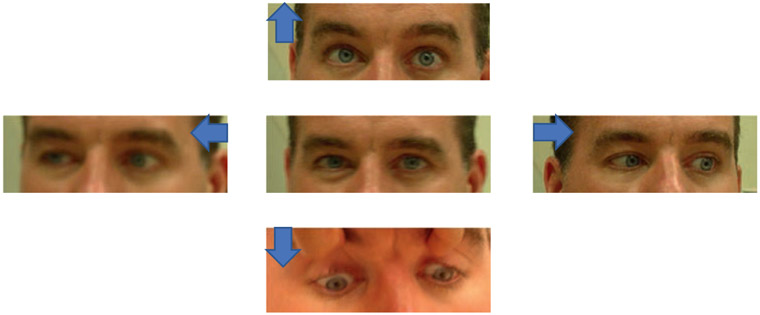
Fig. 2.1.
Ophthalmoparesis in a patient with mitochondrial progressive external ophthalmoplegia due to a single mitochondrial DNA large-scale deletion. The patient has severely impaired upgaze and partially impaired lateral gaze most evident on left lateral gaze with sclera visible on abducting left eye. Mild right ptosis is accentuated on right lateral gaze. Blue arrows denote direction of eye movement.
While it is clear that mtDNA single deletions exhibit phenotypic diversity ranging from Pearson syndrome to isolated PEO and multisystemic KSS, this heterogeneity spans a spectrum rather than discrete entities with overlap cases with PEO-plus manifestations beyond myopathy, albeit not fulfilling criteria for KSS (Berenberg et al., 1977; Rowland et al., 1991; Rowland, 1992; Mancuso et al., 2015; Orsucci et al., 2017; Carelli and La Morgia, 2018).
Although the natural history of mitochondrial PEO has not been prospectively characterized, a retrospective analysis of 69 patients with PEO and mtDNA single large-scale deletions noted that 40 patients with PEO without neurological involvement had later onset (median: 17.5 years-old vs. 12 years-old with neurological manifestations) and slower progression (Aure et al., 2007). Most patients had initial onset of PEO with subsequent development of limb myopathy, dysphagia, and heart involvement, supporting the notion that mitochondrial pure PEO is less common than PEO with myopathy.
MRI scans of extraocular muscle have revealed that increased T1-weighted hyperintensity and T2 prolongation correlated severity of ophthalmoparesis indicating MRI biomarkers may be useful in assessing PEO progression in natural history studies and therapeutic clinical trials (Pitceathly et al., 2016). In a detailed study of 87 patients with single large-scale mtDNA deletions, Drs. John Grady, Robert McFarland and colleagues noted correlations between clinical and histological outcome measures with the size of the deletion, deletion heteroplasmy level, and location of the deletion (Grady et al., 2014); however, application of the mtDNA single-deletion features to predict outcome in individual patient is not yet feasible.
While mtDNA single deletions comprise the most frequent cause of PEO (Moraes et al., 1989; Rodriguez-Lopez et al., 2020), at least 35 distinct mtDNA point mutations as well as pathogenic variants in at least 12 nDNA genes can present with isolated PEO (Table 2.1) (Moraes et al., 1993; Hattori et al., 1994; Seibel et al., 1994; Laforet et al., 1995; Silvestri et al., 1996; Santorelli et al., 1997; Franceschina et al., 1998; Taylor et al., 1998; Tiranti et al., 1999; Kaukonen et al., 2000; Campos et al., 2001; Sahashi et al., 2001; Seneca et al., 2001; Spagnolo et al., 2001; Spelbrink et al., 2001; Van Goethem et al., 2001; Karadimas et al., 2002; Spinazzola et al., 2004; Zsurka et al., 2004; Smits et al., 2007; Sotiriou et al., 2009; Alston et al., 2010; Berardo et al., 2010; Souilem et al., 2010, 2011; Liu et al., 2011; Pinos et al., 2011; Gamba et al., 2012; Wolf et al., 2012; Blakely et al., 2013; Jackson et al., 2014; Hellebrekers et al., 2019; Schlapakow et al., 2019; Tarnopolsky et al., 2019; Joshi et al., 2020; O’Donnell et al., 2020; Rodriguez-Lopez et al., 2020; Visuttijai et al., 2021).
Table 2.1.
Differential diagnosis of mitochondrial progressive external ophthalmoplegia
| Ocular myopathies |
| Mitochondrial progressive external ophthalmoplegia (PEO) |
| Single mitochondrial DNA deletion |
| Mitochondrial DNA depletion deletions syndrome (MDDS) |
| Polymerase gamma (POLG) disease |
| Thymidine kinase 2 deficiency |
| Mitochondrial DNA point mutations |
| Mitochondrial progressive external ophthalmoplegia plus (PEO-plus) |
| Kearns–Sayre syndrome (KSS) |
| Mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) |
| Sensory ataxic neuropathy dysarthria ophthalmoplegia (SANDO) |
| PEO, optic atrophy, and deafness |
| Other PEO-plus |
| Myotonic dystrophy types 1 and 2 |
| Oculopharyngeal muscular dystrophy (OPMD) |
| Oculopharyngodistal myopathy (OPDM) |
| Congenital myopathies |
| Limb-girdle muscular dystrophy (LGMD) with ophthalmoplegia |
| Graves’ disease |
| Orbital myositis (orbital pseudotumor) |
| Neuromuscular Junction Disorders |
| Myasthenia gravis |
| Congenital myasthenia gravis |
| Lambert–Eaton myasthenic syndrome (LEMS) |
| Neurogenic ophthalmoplegia |
| Multiple sclerosis |
| Anti-GQ1b syndrome |
| Miller–Fisher syndrome |
| Congenital with facial diplegia (Moebius syndrome) |
| A-beta lipoproteinemia |
| Supranuclear ophthalmoplegia |
| Progressive supranuclear palsy (PSP) |
| Hereditary ataxias |
| Hereditary spastic paraplegia (HSP) |
| Spastic paraplegia 7 (SPG7) and rarely spastic paraplegia 35 (SPG35) |
| Spinocerebellar ataxia (SCA) |
| SCA 1, 2, 3, 7, 9, 11, 28 |
Most of the nuclear genes presenting with PEO are required for mtDNA maintenance as evident by the presence of mtDNA multiple deletions, depletion, or both in muscle and other postmitotic tissues (Lopez-Gomez et al., 2022). Pathogenic variants in POLG are the most frequent nDNA cause of PEO, which may be inherited in an autosomal dominant or recessive manner (Cohen et al., 1993; Van Goethem et al., 2001). While PEO due to POLG pathogenic variants may be the only manifestation, most individuals develop a generalized myopathy with proximal limb weakness, fatigue, and exercise intolerance. Furthermore, after initially presenting with PEO, people with autosomal POLG pathogenic variants often progress to develop PEO-plus with extra-muscular manifestations, such as peripheral neuropathy, ataxia, encephalopathy, and seizures (Van Goethem et al., 2001, 2003a; Lamantea et al., 2002; Horvath et al., 2006). Similarly, some individuals with autosomal dominant POLG pathogenic variants have PEO-plus with variable combinations and severity of sensorineural hearing loss, peripheral neuropathy, ataxia, depression, parkinsonism, hypogonadism, and cataracts (Luoma et al., 2004; Pagnamenta et al., 2006). One recurrent form of PEO-plus due to recessive POLG pathogenic variants is sensory ataxic neuropathy, dysarthria, and ophthalmoplegia (SANDO) (Fadic et al., 1997).
Other nDNA genes that cause PEO include SLC25A4, TWNK, POLG2, SPG7, DNA2, RNASEH1, TOP3A, TK2, DGUOK, RRM2B, and GMPR (Table 2.2) (Kaukonen et al., 2000; Saada et al., 2001; Spelbrink et al., 2001; Longley et al., 2006; Bourdon et al., 2007; Tyynismaa et al., 2009, 2012; Fratter et al., 2011; Ronchi et al., 2012, 2013; Paradas et al., 2013; Pfeffer et al., 2014; Wedding et al., 2014; Reyes et al., 2015; Feichtinger et al., 2017; Martin et al., 2018; Sommerville et al., 2020; Primiano et al., 2022).
Table 2.2.
Nuclear genes with pathogenic variants that cause mitochondrial progressive external ophthalmoplegia
| Gene | Protein | PEO Phenotype | Inheritance | Reference |
|---|---|---|---|---|
| TYMP | Thymidine phosphorylase | MNGIE | AR | Nishino et al. (2000) |
| SLC25A4 | Adenine nucleotide translocator 1 | PEO | AD/AR | Kaukonen et al. (2000) |
| TK2 | Thymidine kinase 2 | PEO/PEO-plus | AR | Saada et al. (2001) and Garone et al. (2018) |
| DGUOK | Deoxyguanosine kinase | PEO | AR | Mandel et al. (2001) and Ronchi et al. (2012) |
| POLG | Polymerase gamma catalytic subunit | PEO/PEO-plus/SANDO/MNGIE-like | AD/AR | Van Goethem et al. (2001) and Van Goethem et al. (2003a) |
| TWNK | Twinkle | PEO | AD/AR | Spelbrink et al. (2001) |
| POLG2 | Polymerase gamma subunit 2 | PEO | AD/AR | Longley et al. (2006) |
| RRM2B | P53-subunit of ribonucleotide reductase | PEO/KSS/MNGIE-like | AD/AR | Bourdon et al. (2007) and Pitceathly et al. (2012) |
| OPA1 | GTPase mitochondrial fusion | PEO-plus | AD | Hudson et al. (2008) |
| MGME1 | Mitochondrial genome maintenance exonuclease 1 | PEO/KSS | AR | Kornblum et al. (2013) |
| DNA2 | DNA replication ATP-dependent | PEO | AD | Ronchi et al. (2013) |
| SPG7 | Paraplegin | PEO-plus | AR | Wedding et al. (2014) |
| AFGL2 | AFG3-like protein 2 | PEO-plus | AD | Gorman et al. (2015) |
| RNASEH1 | Ribonuclease H1 | PEO/PEO-plus | AR | Reyes et al. (2015) and Bugiardini et al. (2017) |
| C1QBP | Complement component C1q binding protein | PEO | AR | Feichtinger et al. (2017) |
| TOP3A | DNA topoisomerase 3 alpha | PEO-plus | AR | Nicholls et al. (2018) |
| GMPR | GMP reductase 1 | PEO | AD | Sommerville et al. (2020) |
| LIG3 | Ligase III | MNGIE-like | AR | Bonora et al. (2021) |
| RRM1 | Ribonucleotide reductase catalytic subunit | PEO/MNGIE-like | AD/AR | Shintaku et al. (2022) |
Abbreviations: AD, autosomal dominant; AR, autosomal recessive; KSS, Kearns–Sayre syndrome; MNGIE, mitochondrial neurogastrointestinal encephalomyopathy; PEO, progressive external ophthalmoplegia; SANDO, sensory ataxic neuropathy dysarthria ophthalmoplegia.
Thymidine kinase 2 deficiency (TK2d), due to autosomal recessive TK2 pathogenic variants, presents as a clinical spectrum from early onset (beginning in the 1–4th year of life), rapidly progressive and fatal myopathy to a late-onset (after age 12 years) PEO, which often resembles PEO due to POLG pathogenic variants or single mtDNA deletions (Garone et al., 2018; Wang et al., 2018). However, early respiratory muscle involvement causing severe restrictive lung disease is characteristic of TK2d. Compassionate use of deoxynucleoside in TK2d patients suggests this may be an effective therapy (Dominguez-Gonzalez et al., 2019; Berardo et al., 2022).
KEARNS–SAYRE SYNDROME
The frequently cited historical criteria for KSS are an obligate triad of CPEO, pigmentary retinopathy, and onset before age 20 years plus at least one of the following three manifestations: cardiac conduction block, cerebellar ataxia, and elevated cerebrospinal fluid protein (>100 mg/dL) (Rowland et al., 1983, 1991). Shortcomings of this definition include the age-at-onset requirement, as some cases have had onset after age 20 (Hirano and DiMauro, 1996), and elevated CSF protein, which is rarely performed because molecular genetic testing provides definitive diagnosis is many cases via noninvasive testing (Emmanuele et al., 2022). Thus, a North American consensus paper has reverted to the original definition of KSS composed of the clinical tetrad: 1) PEO; 2) pigmentary retinopathy; 3) cardiac conduction block; and 4) skeletal muscle involvement (Kearns and Sayre, 1958; Emmanuele et al., 2022). While as many as 90% of KSS cases are due to mtDNA single deletions (Moraes et al., 1989), pathogenic variants in nDNA genes or mtDNA point mutations may present as KSS (Wilichowski et al., 1998; Seneca et al., 2001; Nishigaki et al., 2003; Pitceathly et al., 2011; Kornblum et al., 2013).
PEO-PLUS
In addition to the distinct cases of PEO and KSS, there are patients with mtDNA single deletions that have manifestations beyond PEO, but do not fulfill criteria for KSS and are therefore classified as PEO-plus (previously described as ophthalmoplegia-plus) (Table 2.2). Some individuals are transiently PEO-plus until they develop the full KSS phenotype (Aure et al., 2007). Furthermore, it has become clear that distinct PEO-plus syndromes are clinically recognizable and often linked to pathogenic variants in specific nuclear DNA (nDNA) genes, such as mitochondrial neurogastrointestinal encephalomyopathy (MNGIE), which is typically due to TYMP pathogenic variants, while sensory ataxic neuropathy dysarthria ophthalmoplegia (SANDO) has been linked primarily to POLG pathogenic variants (Table 2.2) (Drachman, 1968; Rosenberg et al., 1968; Rowland et al., 1991, 1997; Rowland, 1992; Fadic et al., 1997; Nishino et al., 1999; Hirano et al., 2001; McClelland et al., 2016; Viscomi and Zeviani, 2017; Lopez-Gomez et al., 2022). Pathogenic variants in OPA1 typically cause autosomal dominant optic atrophy; however, a subset of patients develop PEO and other neurological features in addition to optic neuropathy (Ferraris et al., 2008; Hudson et al., 2008; Yu-Wai-Man et al., 2010).
MITOCHONDRIAL NEUROGASTROINTESTINAL ENCEPHALOMYOPATHY (MNGIE)
MNGIE is clinically defined by PEO, gastrointestinal dysmotility, cachexia, peripheral neuropathy, and leukoencephalopathy, and supported by laboratory tests indicating mitochondrial dysfunction (elevated lactate in blood, cerebrospinal fluid, or both; mtDNA multiple deletions, deletions, or somatic point mutations; and RRF, COX-deficient fibers, or both in muscle) (Hirano et al., 2021). Autosomal recessive TYMP pathogenic variants cause loss of thymidine phosphorylase activity leading to accumulation of thymidine and deoxyuridine and mitochondrial deoxynucleoside triphosphate pool imbalances that cause mtDNA instability (Nishino et al., 1999; Spinazzola et al., 2002). Typically, the disease onset is in the late teens and progresses to fatality in the late-30s (Garone et al., 2011). Allogeneic hematopoietic stem cell transplantation (AHSCT) and liver transplantation decrease levels of the toxic nucleosides, thymidine and deoxyuridine, and may lead to stabilization or mild clinical improvements; however, due to high morbidity and mortality after AHSCT, liver transplantation is the more suitable option for most MNGIE patients (Halter et al., 2011; D’Angelo et al., 2020; Hirano et al., 2021). Patients with MNGIE or MNGIE-like phenotypes have been linked to pathogenic variants in POLG, RRM2B, and LIG3 (Van Goethem et al., 2003c; Shaibani et al., 2009; Bonora et al., 2021) as well as mtDNA point mutations (Gamez and Garces-Garmendia, 2005; Keilland et al., 2016).
SENSORY ATAXIC NEUROPATHY DYSARTHRIA OPHTHALMOPLEGIA (SANDO)
Originally reported as a distinct mitochondrial disease phenotype, Sensory Ataxic Neuropathy Dysarthria Ophthalmoplegia (SANDO) was initially linked to autosomal recessive pathogenic variants in POLG (Fadic et al., 1997; Van Goethem et al., 2003a). Rare subsequent cases of SANDO have been identified to be caused by pathogenic variants in C10orf2 and RNASEH1 (Hudson et al., 2005; Hanisch et al., 2015; Bugiardini et al., 2017).
NONMITOCHONDRIAL FORMS OF PEO
In addition to mitochondrial diseases, other neuromuscular disorders manifest PEO and need to be considered in the differential diagnosis of mitochondrial PEO (Table 2.1). Nonmitochondrial ocular myopathies include myotonic dystrophy, oculopharyngeal muscular dystrophy (OPMD), oculopharyngodistal myopathy (OPDM), congenital myopathies, limb-girdle muscular dystrophy, Graves’ ophthalmopathy, and orbital myositis (Rowland, 1992; Rowland et al., 1997). Myotonic dystrophy type 1 characteristically presents as a multisystemic disorder with distal limb weakness, myotonia, early cataracts, cardiac arrhythmias, endocrinopathies, daytime sleepiness, balding, and intellectual disabilities (Bird, 1993). Myotonic dystrophy type 1 is due to autosomal dominant expansions of a CTG trinucleotide repeat in DMPK. In contrast to type 1, type 2 myotonic dystrophy typically affects proximal and axial muscles, and less frequently affects nonmuscle tissues, and is caused by autosomal dominant expansions of a CCTG repeat in CNBP (Schoser, 1993). Oculopharyngeal muscular dystrophy (OPMD) is a late-onset disorder with ptosis, dysphagia, and proximal limb weakness with relatively mild ophthalmoparesis (Brais, 2011; Yamashita, 2021). OPMD is usually inherited in an autosomal pattern due to expansions of a GCN trinucleotide repeat in PABP1 (biallelic 11 repeats cause autosomal recessive OPMD, while heterozygous 12–18 repeats cause autosomal dominant OPMD). Oculopharyngodistal myopathy (OPDM) is an adolescent or adult-onset disorder with extraocular, facial, pharyngeal, and distal limb weakness due to expansions in CGG trinucleotide repeats in four genes: LRP12, GIPC1, NOTCH2NLC, and RIPL1 (Yu et al., 2022). Thus, expansions of tri- or tetra-nucleotide repeats in noncoding regions of genes are emerging as a recurrent cause of myopathies with PEO.
Inherited congenital myopathies that often manifest PEO in addition to limb and axial weakness include central core myopathy due to recessive RYR1 pathogenic variants, centronuclear myopathy due to X-linked recessive variants in MTM1, and autosomal dominant pathogenic variants in DNM2 (Claeys, 2020). Genetic congenital myasthenic syndromes with defects at the neuromuscular junction typically present with generalized weakness with prominent ptosis and ophthalmoparesis, and some forms present with isolated extraocular weakness (Estephan et al., 2022). Congenital fibrosis of extraocular muscles (CFEOM), Duane retraction syndrome, and Mobius syndrome are congenital cranial dysinnervation disorders presenting with ptosis at birth with variable restrictive and paretic strabismus due to genetic defects of embryological development of cranial neuromuscular units (Vivian, 2020).
Among the nongenetic causes of PEO, autoimmune ocular and generalized myasthenia gravis are the most frequent and can be clinically distinguished from genetic forms by acute to subacute onset and prominent fluctuation of symptoms, in contrast to the gradual onset and chronic slow progression of most genetic forms of PEO (Gilhus, 2016; Farmakidis et al., 2018; Pasnoor et al., 2018). The diagnosis can be confirmed in most cases by detection of autoantibodies against the acetylcholine receptor, muscle specific kinase, or lipoprotein-related protein 4 (LRP4), as well as electrophysiological studies. Thyroid-associated ophthalmopathy can present with ophthalmoparesis; however, most cases manifest eyelid retraction with signs of orbital inflammation, such as conjunctival erythema and swelling, periocular edema, and proptosis (Bahn, 2010; Liu et al., 2010).
CONCLUSIONS
In the three decades since the last Handbook of Clinical Neurology chapter on PEO (Rowland, 1992), there has been remarkable progress in delineating multiple genetic causes of this condition. In particular, pathogenic variants in mtDNA and nDNA that impair mitochondrial functions have emerged as frequent causes of isolated PEO, PEO-plus, and specific PEO-plus syndromes such as KSS, MNGIE, and SANDO. Several conclusions can be drawn from the genetic knowledge. Single large-scale deletions of mtDNA are the most frequent causes of sporadic mitochondrial PEO and KSS, while nDNA defects causing secondary defects of mtDNA maintenance are the most frequent causes of autosomal mitochondrial PEO and PEO-plus syndromes. Additional nonmitochondrial forms of PEO have also been genetically linked to expansions of tri- and tetra-nucleotide DNA repeats, as well as defects in genes required for development of the neuromuscular junction or cranial neuromuscular units. Further advances to develop therapies for PEO are needed.
FUNDING INFORMATION
MH is supported by research grants from the National Institutes of Health (North American Mitochondrial Disease Consortium [NAMDC] U54 NS078059 from NINDS, NICHD, and ODS), Department of Defense (W81XWH2010807), Muscular Dystrophy Association, the Arturo Estopinan TK2 Research Fund, Nicholas Nunno Foundation, JDM Fund for Mitochondrial Research, Shuman Mitochondrial Disease Fund, and the Marriott Mitochondrial Disease Clinic Research Fund (MMDCRF) from the J. Willard and Alice S. Marriott Foundation. NAMDC is part of Rare Diseases Clinical Research Network (RDCRN), an initiative of the Office of Rare Diseases Research (ORDR), National Center for Advancing Translational Sciences (NCATS). R.D.S.P. is supported by a Medical Research Council (UK) Clinician Scientist Fellowship (MR/S002065/1), a Medical Research Council (UK) award MC_PC_21046 to establish a National Mouse Genetics Network Cluster in Mitochondria (MitoCluster), and a Medical Research Council (UK) strategic award MR/S005021/1 to establish an International Centre for Genomic Medicine in Neuromuscular Diseases (ICGNMD).
Footnotes
DECLARATION OF INTERESTS
MH is a paid consultant to Modis Therapeutics, a wholly owned subsidiary of Zogenix/UCB, and Entrada Therapeutics. These relationships are de minimus for Columbia University Medical Center. Columbia University has patents for deoxynucleotide and deoxynucleoside therapies for mitochondrial DNA depletion syndrome, which is licensed by Modis Therapeutics; this relationship is monitored by an unconflicted external academic researcher. Received honoraria from the AAN and PlatformQ for speaking activities and research support from Modis Therapeutics and Entrada Therapeutics.
References
- Alston CL, Lowe J, Turnbull DM et al. (2010). A novel mitochondrial tRNAGlu (MTTE) gene mutation causing chronic progressive external ophthalmoplegia at low levels of heteroplasmy in muscle. J Neurol Sci 298: 140–144. 10.1016/j.jns.2010.08.014. [DOI] [PubMed] [Google Scholar]
- Aure K, Ogier de Baulny H, Laforet P et al. (2007). Chronic progressive ophthalmoplegia with large-scale mtDNA rearrangement: can we predict progression? Brain 130: 1516–1524. 10.1093/brain/awm067. [DOI] [PubMed] [Google Scholar]
- Bahn RS (2010). Graves’ ophthalmopathy. N Engl J Med 362: 726–738. 10.1056/NEJMra0905750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barca E, Long Y, Cooley V et al. (2020). Mitochondrial diseases in North America: an analysis of the NAMDC Registry. Neurol Genet 6: e402. 10.1212/NXG.0000000000000402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaumont WM (1890). Notes of a case of progressive nuclear ophthalmoplegia. Brain 13: 386–387. [Google Scholar]
- Beckett RS, Netsky MG (1953). Familial ocular myopathy and external ophthalmoplegia. AMA Arch Neurol Psychiatry 69: 64–72. 10.1001/archneurpsyc.1953.02320250070007. [DOI] [PubMed] [Google Scholar]
- Berardo A, Coku J, Kurt B et al. (2010). A novel mutation in the tRNAIle gene (MTTI) affecting the variable loop in a patient with chronic progressive external ophthalmoplegia (CPEO). Neuromuscul Disord 20: 204–206. 10.1016/j.nmd.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berardo A, Dominguez-Gonzalez C, Engelstad K et al. (2022). Advances in thymidine kinase 2 deficiency: clinical aspects, translational progress, and emerging therapies. J Neuromuscul Dis 9: 225–235. 10.3233/JND-210786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenberg RA, Pellock JM, DiMauro S et al. (1977). Lumping or splitting? “Ophthalmoplegia-plus” or Kearns-Sayre syndrome? Ann Neurol 1: 37–54. 10.1002/ana.410010104. [DOI] [PubMed] [Google Scholar]
- Bird TD (1993). Myotonic dystrophy type 1. In: Adam MP et al. (Eds.)., GeneReviews((R)). Seattle (WA). [Google Scholar]
- Blakely EL, Yarham JW, Alston CL et al. (2013). Pathogenic mitochondrial tRNA point mutations: nine novel mutations affirm their importance as a cause of mitochondrial disease. Hum Mutat 34: 1260–1268. 10.1002/humu.22358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonora E, Chakrabarty S, Kellaris G et al. (2021). Biallelic variants in LIG3 cause a novel mitochondrial neurogastrointestinal encephalomyopathy. Brain 144: 1451–1466. 10.1093/brain/awab056. [DOI] [PubMed] [Google Scholar]
- Bourdon A, Minai L, Serre V et al. (2007). Mutation of RRM2B, encoding p53-controlled ribonucleotide reductase (p53R2), causes severe mitochondrial DNA depletion. Nat Genet 39: 776–780. 10.1038/ng2040. [DOI] [PubMed] [Google Scholar]
- Brais B (2011). Oculopharyngeal muscular dystrophy. Handb Clin Neurol 101: 181–192. 10.1016/B978-0-08-045031-5.00014-1. [DOI] [PubMed] [Google Scholar]
- Bugiardini E, Poole OV, Manole A et al. (2017). Clinicopathologic and molecular spectrum of RNASEH1-related mitochondrial disease. Neurol Genet 3: e149. 10.1212/NXG.0000000000000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos Y, Gamez J, Garcia A et al. (2001). A new mtDNA mutation in the tRNA(Leu(UUR)) gene associated with ocular myopathy. Neuromuscul Disord 11: 477–480. 10.1016/s0960-8966(00)00223-6. [DOI] [PubMed] [Google Scholar]
- Carelli V, La Morgia C (2018). Clinical syndromes associated with mtDNA mutations: where we stand after 30 years. Essays Biochem 62: 235–254. 10.1042/EBC20170097. [DOI] [PubMed] [Google Scholar]
- Claeys KG (2020). Congenital myopathies: an update. Dev Med Child Neurol 62: 297–302. 10.1111/dmcn.14365. [DOI] [PubMed] [Google Scholar]
- Cohen BH, Chinnery PF, Copeland WC (1993). POLG-related disorders. In: Adam MP et al. (Eds.)., GeneReviews((R)). Seattle (WA). [Google Scholar]
- D’Angelo R, Boschetti E, Amore G et al. (2020). Liver transplantation in mitochondrial neurogastrointestinal encephalomyopathy (MNGIE): clinical long-term follow-up and pathogenic implications. J Neurol 267: 3702–3710. 10.1007/s00415-020-10051-x. [DOI] [PubMed] [Google Scholar]
- DiMauro S, Schotland DL, Bonilla E et al. (1973). Progressive ophthalmoplegia, glycogen storage, and abnormal mitochondria. Arch Neurol 29: 170–179. 10.1001/archneur.1973.00490270052008. [DOI] [PubMed] [Google Scholar]
- Dominguez-Gonzalez C, Madruga-Garrido M, Mavillard F et al. (2019). Deoxynucleoside therapy for thymidine kinase 2-deficient myopathy. Ann Neurol 86: 293–303. 10.1002/ana.25506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drachman DA (1968). Ophthalmoplegia plus. The neurodegenerative disorders associated with progressive external ophthalmoplegia. Arch Neurol 18: 654–674. 10.1001/archneur.1968.00470360076008. [DOI] [PubMed] [Google Scholar]
- Elliott FA (1939). Myopathic wasting associated with ptosis and external ophthalmoplegia. Proc R Soc Med 32: 876. 10.1177/003591573903200811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmanuele V, Ganesh J, Vladutiu G et al. (2022). Time to harmonize mitochondrial syndrome nomenclature and classification: a consensus from the North American Mitochondrial Disease Consortium (NAMDC). Mol Genet Metab 136: 125–131. 10.1016/j.ymgme.2022.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estephan EP, Zambon AA, Thompson R et al. (2022). Congenital myasthenic syndrome: correlation between clinical features and molecular diagnosis. Eur J Neurol 29: 833–842. 10.1111/ene.15173. [DOI] [PubMed] [Google Scholar]
- Fadic R, Russell JA, Vedanarayanan VV et al. (1997). Sensory ataxic neuropathy as the presenting feature of a novel mitochondrial disease. Neurology 49: 239–245. 10.1212/wnl.49.1.239. [DOI] [PubMed] [Google Scholar]
- Farmakidis C, Pasnoor M, Dimachkie MM et al. (2018). Treatment of myasthenia gravis. Neurol Clin 36: 311–337. 10.1016/j.ncl.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feichtinger RG, Olahova M, Kishita Y et al. (2017). Biallelic C1QBP mutations cause severe neonatal-, childhood-, or later-onset cardiomyopathy associated with combined respiratory-chain deficiencies. Am J Hum Genet 101: 525–538. 10.1016/j.ajhg.2017.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraris S, Clark S, Garelli E et al. (2008). Progressive external ophthalmoplegia and vision and hearing loss in a patient with mutations in POLG2 and OPA1. Arch Neurol 65: 125–131. 10.1001/archneurol.2007.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franceschina L, Salani S, Bordoni A et al. (1998). A novel mitochondrial tRNA(Ile) point mutation in chronic progressive external ophthalmoplegia. J Neurol 245: 755–758. 10.1007/s004150050283. [DOI] [PubMed] [Google Scholar]
- Fratter C, Raman P, Alston CL et al. (2011). RRM2B mutations are frequent in familial PEO with multiple mtDNA deletions. Neurology 76: 2032–2034. 10.1212/WNL.0b013e31821e558b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs E (1890). Ueber isolierte doppelseitige ptosis. Graefe Arch Ophthalmol 36: 234–259. [Google Scholar]
- Gamba J, Kiyomoto BH, de Oliveira AS et al. (2012). The mutations m.5628T>C and m.8348A>G in single muscle fibers of a patient with chronic progressive external ophthalmoplegia. J Neurol Sci 320: 131–135. 10.1016/j.jns.2012.05.037. [DOI] [PubMed] [Google Scholar]
- Gamez J, Garces-Garmendia MA (2005). Paralytic ileus in a MELAS patient mimicking MNGIE. Pediatr Neurol 33: 151. 10.1016/j.pediatrneurol.2005.05.023. [DOI] [PubMed] [Google Scholar]
- Garone C, Tadesse S, Hirano M (2011). Clinical and genetic spectrum of mitochondrial neurogastrointestinal encephalomyopathy. Brain 134: 3326–3332. 10.1093/brain/awr245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garone C, Taylor RW, Nascimento A et al. (2018). Retrospective natural history of thymidine kinase 2 deficiency. J Med Genet 55: 515–521. 10.1136/jmedgenet-2017-105012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilhus NE (2016). Myasthenia Gravis. N Engl J Med 375: 2570–2581. 10.1056/NEJMra1602678. [DOI] [PubMed] [Google Scholar]
- Goldstein A, Falk MJ (2013). Mitochondrial DNA Deletion Syndromes. In: GeneReviews((R)) [Internet], University of Washington, Seattle, Seattle (WA). [Updated 2019 Jan 31]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20301382. [Google Scholar]
- Gorman GS, Pfeffer G, Griffin H et al. (2015). Clonal expansion of secondary mitochondrial DNA deletions associated with spinocerebellar ataxia type 28. JAMA Neurol 72: 106–111. 10.1001/jamaneurol.2014.1753. [DOI] [PubMed] [Google Scholar]
- Grady JP, Campbell G, Ratnaike T et al. (2014). Disease progression in patients with single, large-scale mitochondrial DNA deletions. Brain 137: 323–334. 10.1093/brain/awt321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halter J, Schupbach W, Casali C et al. (2011). Allogeneic hematopoietic SCT as treatment option for patients with mitochondrial neurogastrointestinal encephalomyopathy (MNGIE): a consensus conference proposal for a standardized approach. Bone Marrow Transplant 46: 330–337. 10.1038/bmt.2010.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanisch F, Kornhuber M, Alston CL et al. (2015). SANDO syndrome in a cohort of 107 patients with CPEO and mitochondrial DNA deletions. J Neurol Neurosurg Psychiatry 86: 630–634. 10.1136/jnnp-2013-306748. [DOI] [PubMed] [Google Scholar]
- Hassler R (1953). Erkrankungen der Oblongata, der Brücke und des Mittelhirns. In: von Bergmann F, Frey W, Schwiegk H (Eds.), Handbuch der inneren Medizin. Springer, Berlin, pp. 552–619. [Google Scholar]
- Hattori Y, Goto Y, Sakuta R et al. (1994). Point mutations in mitochondrial tRNA genes: sequence analysis of chronic progressive external ophthalmoplegia (CPEO). J Neurol Sci 125: 50–55. 10.1016/0022-510x(94)90241-0. [DOI] [PubMed] [Google Scholar]
- Hellebrekers D, Blakely EL, Hendrickx ATM et al. (2019). A novel mitochondrial m.4414T>C MT-TM gene variant causing progressive external ophthalmoplegia and myopathy. Neuromuscul Disord 29: 693–697. 10.1016/j.nmd.2019.08.005. [DOI] [PubMed] [Google Scholar]
- Hirano M, DiMauro S (1996). Clinical features of mitochondrial myopathies and encephalomyopathies. In: Lane R (Ed.), Handbook of muscle disease. Marcel Dekker Inc. USA, New York, pp. 479–504. [Google Scholar]
- Hirano M, Marti R, Ferreiro-Barros C et al. (2001). Defects of intergenomic communication: autosomal disorders that cause multiple deletions and depletion of mitochondrial DNA. Semin Cell Dev Biol 12: 417–427. [DOI] [PubMed] [Google Scholar]
- Hirano M, Carelli V, De Giorgio R et al. (2021). Mitochondrial neurogastrointestinal encephalomyopathy (MNGIE): position paper on diagnosis, prognosis, and treatment by the MNGIE International Network. J Inherit Metab Dis 44: 376–387. 10.1002/jimd.12300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt IJ, Harding AE, Morgan-Hughes JA (1988). Mitochondrial DNA polymorphism in mitochondrial myopathy. Hum Genet 79: 53–57. 10.1007/BF00291710. [DOI] [PubMed] [Google Scholar]
- Holt IJ, Harding AE, Cooper JM et al. (1989). Mitochondrial myopathies: clinical and biochemical features of 30 patients with major deletions of muscle mitochondrial DNA. Ann Neurol 26: 699–708. 10.1002/ana.410260603. [DOI] [PubMed] [Google Scholar]
- Horvath R, Hudson G, Ferrari G et al. (2006). Phenotypic spectrum associated with mutations of the mitochondrial polymerase gamma gene. Brain 129: 1674–1684. 10.1093/brain/awl088. [DOI] [PubMed] [Google Scholar]
- Hudson G, Deschauer M, Busse K et al. (2005). Sensory ataxic neuropathy due to a novel C10Orf2 mutation with probable germline mosaicism. Neurology 64: 371–373. 10.1212/01.WNL.0000149767.51152.83. [DOI] [PubMed] [Google Scholar]
- Hudson G, Amati-Bonneau P, Blakely EL et al. (2008). Mutation of OPA1 causes dominant optic atrophy with external ophthalmoplegia, ataxia, deafness and multiple mitochondrial DNA deletions: a novel disorder of mtDNA maintenance. Brain 131: 329–337. 10.1093/brain/awm272. [DOI] [PubMed] [Google Scholar]
- Hutchinson J (1879). On ophthalmoplegia externa, or symmetrical immobility (partial) of the eyes, with ptosis. Med Chir Trans 62: 307–329. 10.1177/095952877906200120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson CB, Neuwirth C, Hahn D et al. (2014). Novel mitochondrial tRNA(Ile) m.4282A>G gene mutation leads to chronic progressive external ophthalmoplegia plus phenotype. Br J Ophthalmol 98: 1453–1459. 10.1136/bjophthalmol-2014-305300. [DOI] [PubMed] [Google Scholar]
- Johns DR, Drachman DB, Hurko O (1989). Identical mitochondrial DNA deletion in blood and muscle. Lancet 1: 393–394. 10.1016/s0140-6736(89)91779-0. [DOI] [PubMed] [Google Scholar]
- Joshi PR, Baty K, Hopton S et al. (2020). Progressive external ophthalmoplegia due to a recurrent de novo m.15990C>T MT-TP (mt-tRNA(Pro)) gene variant. Neuromuscul Disord 30: 346–350. 10.1016/j.nmd.2020.02.020. [DOI] [PubMed] [Google Scholar]
- Karadimas CL, Salviati L, Sacconi S et al. (2002). Mitochondrial myopathy and ophthalmoplegia in a sporadic patient with the G12315A mutation in mitochondrial DNA. Neuromuscul Disord 12: 865–868. 10.1016/s0960-8966(02)00072-x. [DOI] [PubMed] [Google Scholar]
- Kaukonen J, Juselius JK, Tiranti V et al. (2000). Role of adenine nucleotide translocator 1 in mtDNA maintenance. Science 289: 782–785. 10.1126/science.289.5480.782. [DOI] [PubMed] [Google Scholar]
- Kearns TP, Sayre GP (1958). Retinitis pigmentosa, external ophthalmophegia, and complete heart block: unusual syndrome with histologic study in one of two cases. AMA Arch Ophthalmol 60: 280–289. [PubMed] [Google Scholar]
- Keilland E, Rupar CA, Prasad AN et al. (2016). The expanding phenotype of MELAS caused by the m.3291T > C mutation in the MT-TL1 gene. Mol Genet Metab Rep 6: 64–69. 10.1016/j.ymgmr.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiloh LG, Nevin S (1951). Progressive dystrophy of the external ocular muscles (ocular myopathy). Brain 74: 115–143. 10.1093/brain/74.2.115. [DOI] [PubMed] [Google Scholar]
- Kornblum C, Nicholls TJ, Haack TB et al. (2013). Loss-of-function mutations in MGME1 impair mtDNA replication and cause multisystemic mitochondrial disease. Nat Genet 45: 214–219. 10.1038/ng.2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laforet P, Lombes A, Eymard B et al. (1995). Chronic progressive external ophthalmoplegia with ragged-red fibers: clinical, morphological and genetic investigations in 43 patients. Neuromuscul Disord 5: 399–413. 10.1016/0960-8966(94)00080-s. [DOI] [PubMed] [Google Scholar]
- Lamantea E, Tiranti V, Bordoni A et al. (2002). Mutations of mitochondrial DNA polymerase gammaA are a frequent cause of autosomal dominant or recessive progressive external ophthalmoplegia. Ann Neurol 52: 211–219. 10.1002/ana.10278. [DOI] [PubMed] [Google Scholar]
- Langdon HM, Cadwalader WB (1928). Chronic progressive external ophthalmoplegia: report of a case with necropsy. Trans Am Ophthalmol Soc 26: 247–260. [PMC free article] [PubMed] [Google Scholar]
- Lestienne P, Ponsot G (1988). Kearns-Sayre syndrome with muscle mitochondrial DNA deletion. Lancet 1: 885. 10.1016/s0140-6736(88)91632-7. [DOI] [PubMed] [Google Scholar]
- Liu GT, Volpe JJ, Galetta SL (2010). Neuro-ophthalmology: diagnosis and management, 2nd ed.Saunders Elsevier, Philadelphia. [Google Scholar]
- Liu CH, Liou CW, Liu CH et al. (2011). Chronic progressive external ophthalmoplegia with T9957C mitochondrial DNA mutation in a Taiwanese patient. Acta Neurol Taiwanica 20: 53–58. [PubMed] [Google Scholar]
- Longley MJ, Clark S, Yu Wai Man C et al. (2006). Mutant POLG2 disrupts DNA polymerase gamma subunits and causes progressive external ophthalmoplegia. Am J Hum Genet 78: 1026–1034. 10.1086/504303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Gomez C, Camara Y, Hirano M et al. (2022). 232nd ENMC international workshop: recommendations for treatment of mitochondrial DNA maintenance disorders, 16–18 June 2017, Heemskerk, The Netherlands. Neuromuscul Disord 32: 609–620. 10.1016/j.nmd.2022.05.008. [DOI] [PubMed] [Google Scholar]
- Luoma P, Melberg A, Rinne JO et al. (2004). Parkinsonism, premature menopause, and mitochondrial DNA polymerase gamma mutations: clinical and molecular genetic study. Lancet 364: 875–882. 10.1016/S0140-6736(04)16983-3. [DOI] [PubMed] [Google Scholar]
- Mancuso M, Orsucci D, Angelini C et al. (2015). Redefining phenotypes associated with mitochondrial DNA single deletion. J Neurol 262: 1301–1309. 10.1007/s00415-015-7710-y. [DOI] [PubMed] [Google Scholar]
- Mandel H, Szargel R, Labay V et al. (2001). The deoxyguanosine kinase gene is mutated in individuals with depleted hepatocerebral mitochondrial DNA. Nat Genet 29: 337–341. 10.1038/ng746. [DOI] [PubMed] [Google Scholar]
- Marburg O (1936). Die chronisch-progressiven nuclearen Amyotrophien. In: Bumke O, Foerster O (Eds.), Handbuch der Neurologie. Springer, Berlin, pp. 524–663. [Google Scholar]
- Martin JP (1936). Progressive external ophthalmoplegia. Proc R Soc Med 29: 965. 10.1177/003591573602900842. [DOI] [Google Scholar]
- Martin CA, Sarlos K, Logan CV et al. (2018). Mutations in TOP3A cause a bloom syndrome-like disorder. Am J Hum Genet 103: 221–231. 10.1016/j.ajhg.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland C, Manousakis G, Lee MS (2016). Progressive external ophthalmoplegia. Curr Neurol Neurosci Rep 16: 53. 10.1007/s11910-016-0652-7. [DOI] [PubMed] [Google Scholar]
- McShane MA, Hammans SR, Sweeney M et al. (1991). Pearson syndrome and mitochondrial encephalomyopathy in a patient with a deletion of mtDNA. Am J Hum Genet 48: 39–42. [PMC free article] [PubMed] [Google Scholar]
- Mita S, Schmidt B, Schon EA et al. (1989). Detection of “deleted” mitochondrial genomes in cytochrome-c oxidase-deficient muscle fibers of a patient with Kearns-Sayre syndrome. Proc Natl Acad Sci U S A 86: 9509–9513. 10.1073/pnas.86.23.9509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moraes CT, DiMauro S, Zeviani M et al. (1989). Mitochondrial DNA deletions in progressive external ophthalmoplegia and Kearns-Sayre syndrome. N Engl J Med 320: 1293–1299. 10.1056/NEJM198905183202001. [DOI] [PubMed] [Google Scholar]
- Moraes CT, Ciacci F, Silvestri G et al. (1993). Atypical clinical presentations associated with the MELAS mutation at position 3243 of human mitochondrial DNA. Neuromuscul Disord 3: 43–50. 10.1016/0960-8966(93)90040-q. [DOI] [PubMed] [Google Scholar]
- Muller-Hocker J, Pongratz D, Hubner G (1983). Focal deficiency of cytochrome-c-oxidase in skeletal muscle of patients with progressive external ophthalmoplegia. Cytochemical-fine-structural study. Virchows Arch A Pathol Anat Histopathol 402: 61–71. 10.1007/BF00695049. [DOI] [PubMed] [Google Scholar]
- Mussini JM, Friol-Vercelletto M, Forgeau Y et al. (1984). Role of muscle biopsy in the diagnosis of ocular myopathies. Rev Otoneuroophtalmol 56: 203–208. [PubMed] [Google Scholar]
- Nicholls TJ, Nadalutti CA, Motori E et al. (2018). Topoisomerase 3alpha is required for decatenation and segregation of human mtDNA. Mol Cell 69: 9–23. e6. 10.1016/j.molcel.2017.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishigaki Y, Tadesse S, Bonilla E et al. (2003). A novel mitochondrial tRNA(Leu(UUR)) mutation in a patient with features of MERRF and Kearns-Sayre syndrome. Neuromuscul Disord 13: 334–340. 10.1016/s0960-8966(02)00283-3. [DOI] [PubMed] [Google Scholar]
- Nishino I, Spinazzola A, Hirano M (1999). Thymidine phosphorylase gene mutations in MNGIE, a human mitochondrial disorder. Science 283: 689–692. 10.1126/science.283.5402.689. [DOI] [PubMed] [Google Scholar]
- Nishino I, Spinazzola A, Papadimitriou A et al. (2000). Mitochondrial neurogastrointestinal encephalomyopathy: an autosomal recessive disorder due to thymidine phosphorylase mutations. Ann Neurol 47: 792–800. [PubMed] [Google Scholar]
- O’Donnell L, Blakely EL, Baty K et al. (2020). Chronic progressive external ophthalmoplegia due to a rare de novo m.12334G>A MT-TL2 mitochondrial DNA variant 1. J Neuromuscul Dis 7: 355–360. 10.3233/JND-200486. [DOI] [PubMed] [Google Scholar]
- Olson W, Engel WK, Walsh GO et al. (1972). Oculocraniosomatic neuromuscular disease with “ragged-red” fibers. Arch Neurol 26: 193–211. 10.1001/archneur.1972.00490090019001. [DOI] [PubMed] [Google Scholar]
- Orsucci D, Angelini C, Bertini E et al. (2017). Revisiting mitochondrial ocular myopathies: a study from the Italian Network. J Neurol 264: 1777–1784. 10.1007/s00415-017-8567-z. [DOI] [PubMed] [Google Scholar]
- Ozawa T, Yoneda M, Tanaka M et al. (1988). Maternal inheritance of deleted mitochondrial DNA in a family with mitochondrial myopathy. Biochem Biophys Res Commun 154: 1240–1247. 10.1016/0006-291x(88)90272-0. [DOI] [PubMed] [Google Scholar]
- Pagnamenta AT, Taanman JW, Wilson CJ et al. (2006). Dominant inheritance of premature ovarian failure associated with mutant mitochondrial DNA polymerase gamma. Hum Reprod 21: 2467–2473. 10.1093/humrep/del076. [DOI] [PubMed] [Google Scholar]
- Paradas C, Gutierrez Rios P, Rivas E et al. (2013). TK2 mutation presenting as indolent myopathy. Neurology 80: 504–506. 10.1212/WNL.0b013e31827f0ff7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasnoor M, Dimachkie MM, Farmakidis C et al. (2018). Diagnosis of myasthenia gravis. Neurol Clin 36: 261–274. 10.1016/j.ncl.2018.01.010. [DOI] [PubMed] [Google Scholar]
- Petty RK, Harding AE, Morgan-Hughes JA (1986). The clinical features of mitochondrial myopathy. Brain 109: 915–938. 10.1093/brain/109.5.915. [DOI] [PubMed] [Google Scholar]
- Pfeffer G, Gorman GS, Griffin H et al. (2014). Mutations in the SPG7 gene cause chronic progressive external ophthalmoplegia through disordered mitochondrial DNA maintenance. Brain 137: 1323–1336. 10.1093/brain/awu060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinos T, Marotta M, Gallardo E et al. (2011). A novel mutation in the mitochondrial tRNA(Ala) gene (m.5636T>C) in a patient with progressive external ophthalmoplegia. Mitochondrion 11: 228–233. 10.1016/j.mito.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Pitceathly RD, Fassone E, Taanman JW et al. (2011). Kearns-Sayre syndrome caused by defective R1/p53R2 assembly. J Med Genet 48: 610–617. 10.1136/jmg.2010.088328. [DOI] [PubMed] [Google Scholar]
- Pitceathly RD, Smith C, Fratter C et al. (2012). Adults with RRM2B-related mitochondrial disease have distinct clinical and molecular characteristics. Brain 135: 3392–3403. 10.1093/brain/aws231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitceathly RD, Morrow JM, Sinclair CD et al. (2016). Extraocular muscle MRI in genetically-defined mitochondrial disease. Eur Radiol 26: 130–137. 10.1007/s00330-015-3801-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pongratz D, Perwein J, Hubner G et al. (1979). Muscle biopsy in progressive external ophthalmoplegia (author’s transl). Klin Wochenschr 57: 779–788. 10.1007/BF01478036. [DOI] [PubMed] [Google Scholar]
- Primiano G, Torraco A, Verrigni D et al. (2022). Novel TOP3A variant associated with mitochondrial disease: expanding the clinical spectrum of topoisomerase iii alpha-related diseases. Neurol Genet 8: e200007. 10.1212/NXG.0000000000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichmann H, Degoul F, Gold R et al. (1991). Histological, enzymatic and mitochondrial DNA studies in patients with Kearns-Sayre syndrome and chronic progressive external ophthalmoplegia. Eur Neurol 31: 108–113. 10.1159/000116656. [DOI] [PubMed] [Google Scholar]
- Reyes A, Melchionda L, Nasca A et al. (2015). RNASEH1 mutations impair mtDNA replication and cause adult-onset mitochondrial encephalomyopathy. Am J Hum Genet 97: 186–193. 10.1016/j.ajhg.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Lopez C, Garcia-Cardaba LM, Blazquez A et al. (2020). Clinical, pathological and genetic spectrum in 89 cases of mitochondrial progressive external ophthalmoplegia. J Med Genet 57: 643–646. 10.1136/jmedgenet-2019-106649. [DOI] [PubMed] [Google Scholar]
- Ronchi D, Garone C, Bordoni A et al. (2012). Next-generation sequencing reveals DGUOK mutations in adult patients with mitochondrial DNA multiple deletions. Brain 135: 3404–3415. 10.1093/brain/aws258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronchi D, Di Fonzo A, Lin W et al. (2013). Mutations in DNA2 link progressive myopathy to mitochondrial DNA instability. Am J Hum Genet 92: 293–300. 10.1016/j.ajhg.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg RN, Schotland DL, Lovelace RE et al. (1968). Progressive ophthalmoplegia. Report of cases. Arch Neurol 19: 362–376. 10.1001/archneur.1968.00480040028002. [DOI] [PubMed] [Google Scholar]
- Rötig A, Cormier V, Blanche S et al. (1990). A multisystem mitochondrial disorder in infancy. J Clin Invest 86: 1601–1608. 10.1172/JCI114881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland LP (1992). Progressive external ophthalmoplegia. Handb Clin Neurol 287–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland LP, Hays AP, DiMauro S et al. (1983). Diverse clinical disorders associated with morphological abnormalities of mitochondria. In: Cerri C, Scarlato G (Eds.), Mitochondrial pathology in muscle diseases. Piccin Editore, Padua, pp. 141–158. [Google Scholar]
- Rowland LP, Blake DM, Hirano M et al. (1991). Clinical syndromes associated with ragged red fibers. Rev Neurol 147: 467–473. [PubMed] [Google Scholar]
- Rowland LP, Hirano M, DiMauro S et al. (1997). Oculopharyngeal muscular dystrophy, other ocular myopathies, and progressive external ophthalmoplegia. Neuromuscul Disord 7: S15–S21. 10.1016/s0960-8966(97)00076-x. [DOI] [PubMed] [Google Scholar]
- Saada A, Shaag A, Mandel H et al. (2001). Mutant mitochondrial thymidine kinase in mitochondrial DNA depletion myopathy. Nat Genet 29: 342–344. 10.1038/ng751. [DOI] [PubMed] [Google Scholar]
- Sahashi K, Yoneda M, Ohno K et al. (2001). Functional characterisation of mitochondrial tRNA(Tyr) mutation (5877–>GA) associated with familial chronic progressive external ophthalmoplegia. J Med Genet 38: 703–705. 10.1136/jmg.38.10.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandifer PH (1946). Chronic progressive ophthalmoplegia of myopathic origin. J Neurol Neurosurg Psychiatry 9: 81–83. 10.1136/jnnp.9.3.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santorelli FM, Siciliano G, Casali C et al. (1997). Mitochondrial tRNA(Cys) gene mutation (A5814G): a second family with mitochondrial encephalopathy. Neuromuscul Disord 7: 156–159. 10.1016/s0960-8966(97)00444-6. [DOI] [PubMed] [Google Scholar]
- Schlapakow E, Peeva V, Zsurka G et al. (2019). Distinct segregation of the pathogenic m.5667G>A mitochondrial tRNA(Asn) mutation in extraocular and skeletal muscle in chronic progressive external ophthalmoplegia. Neuromuscul Disord 29: 358–367. 10.1016/j.nmd.2019.02.009. [DOI] [PubMed] [Google Scholar]
- Schoser B (1993). Myotonic dystrophy type 2. In: Adam MP et al. (Eds.)., GeneReviews((R)). Seattle (WA). [Google Scholar]
- Schwarz GA, Liu CN (1954). Chronic progressive external ophthalmoplegia. AMA Arch Neurol Psychiatry 71: 31–53. 10.1001/archneurpsyc.1954.02320370033003. [DOI] [PubMed] [Google Scholar]
- Seibel P, Lauber J, Klopstock T et al. (1994). Chronic progressive external ophthalmoplegia is associated with a novel mutation in the mitochondrial tRNA(Asn) gene. Biochem Biophys Res Commun 204: 482–489. 10.1006/bbrc.1994.2485. [DOI] [PubMed] [Google Scholar]
- Seneca S, Verhelst H, De Meirleir L et al. (2001). A new mitochondrial point mutation in the transfer RNA(Leu) gene in a patient with a clinical phenotype resembling Kearns-Sayre syndrome. Arch Neurol 58: 1113–1118. 10.1001/archneur.58.7.1113. [DOI] [PubMed] [Google Scholar]
- Serratrice G (1991). The history of mitochondrial encephalomyopathies. Bull Acad Natl Med 175: 631–639. discussion 40-1. [PubMed] [Google Scholar]
- Shaibani A, Shchelochkov OA, Zhang S et al. (2009). Mitochondrial neurogastrointestinal encephalopathy due to mutations in RRM2B. Arch Neurol 66: 1028–1032. 10.1001/archneurol.2009.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shintaku J, Pernice WM, Eyaid W et al. (2022). RRM1 variants cause a mitochondrial DNA maintenance disorder via impaired de novo nucleotide synthesis. J Clin Invest 132. 10.1172/JCI145660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvestri G, Servidei S, Rana M et al. (1996). A novel mitochondrial DNA point mutation in the tRNA(Ile) gene is associated with progressive external ophtalmoplegia. Biochem Biophys Res Commun 220: 623–627. 10.1006/bbrc.1996.0453. [DOI] [PubMed] [Google Scholar]
- Smits BW, Hol FA, van den Heuvel LP et al. (2007). Chronic progressive external ophthalmoplegia caused by an m.4267A > G mutation in the mitochondrial tRNAIle. J Neurol 254: 1614–1615. 10.1007/s00415-007-0608-6. [DOI] [PubMed] [Google Scholar]
- Sommerville EW, Dalla Rosa I, Rosenberg MM et al. (2020). Identification of a novel heterozygous guanosine mono-phosphate reductase (GMPR) variant in a patient with a late-onset disorder of mitochondrial DNA maintenance. Clin Genet 97: 276–286. 10.1111/cge.13652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotiriou E, Coku J, Tanji K et al. (2009). The m.3244G>A mutation in mtDNA is another cause of progressive external ophthalmoplegia. Neuromuscul Disord 19: 297–299. 10.1016/j.nmd.2009.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souilem S, Kefi M, Mancuso M et al. (2010). A novel hetero-plasmic tRNA Ser(UCN) mtDNA point mutation associated with progressive ophthalmoplegia and dysphagia. Diagn Mol Pathol 19: 28–32. 10.1097/PDM.0b013e3181b00f02. [DOI] [PubMed] [Google Scholar]
- Souilem S, Chebel S, Mancuso M et al. (2011). A novel mitochondrial tRNA(Ile) point mutation associated with chronic progressive external ophthalmoplegia and hyperCKemia. J Neurol Sci 300: 187–190. 10.1016/j.jns.2010.08.065. [DOI] [PubMed] [Google Scholar]
- Spagnolo M, Tomelleri G, Vattemi G et al. (2001). A new mutation in the mitochondrial tRNA(Ala) gene in a patient with ophthalmoplegia and dysphagia. Neuromuscul Disord 11: 481–484. 10.1016/s0960-8966(01)00195-x. [DOI] [PubMed] [Google Scholar]
- Spelbrink JN, Li FY, Tiranti V et al. (2001). Human mitochondrial DNA deletions associated with mutations in the gene encoding Twinkle, a phage T7 gene 4-like protein localized in mitochondria. Nat Genet 28: 223–231. 10.1038/90058. [DOI] [PubMed] [Google Scholar]
- Spinazzola A, Marti R, Nishino I et al. (2002). Altered thymidine metabolism due to defects of thymidine phosphorylase. J Biol Chem 277: 4128–4133. 10.1074/jbc.M111028200. [DOI] [PubMed] [Google Scholar]
- Spinazzola A, Carrara F, Mora M et al. (2004). Mitochondrial myopathy and ophthalmoplegia in a sporadic patient with the 5698G–>A mitochondrial DNA mutation. Neuromuscul Disord 14: 815–817. 10.1016/j.nmd.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Tarnopolsky MA, Sundaram ANE, Provias J et al. (2019). CPEO-like mitochondrial myopathy associated with m.8340G>A mutation. Mitochondrion 46: 69–72. 10.1016/j.mito.2018.02.008. [DOI] [PubMed] [Google Scholar]
- Taylor RW, Chinnery PF, Bates MJ et al. (1998). A novel mitochondrial DNA point mutation in the tRNA(Ile) gene: studies in a patient presenting with chronic progressive external ophthalmoplegia and multiple sclerosis. Biochem Biophys Res Commun 243: 47–51. 10.1006/bbrc.1997.8055. [DOI] [PubMed] [Google Scholar]
- Tiranti V, Carrara F, Confalonieri P et al. (1999). A novel mutation (8342G–>A) in the mitochondrial tRNA(Lys) gene associated with progressive external ophthalmoplegia and myoclonus. Neuromuscul Disord 9: 66–71. 10.1016/s0960-8966(98)00103-5. [DOI] [PubMed] [Google Scholar]
- Tyynismaa H, Ylikallio E, Patel M et al. (2009). A heterozygous truncating mutation in RRM2B causes autosomal-dominant progressive external ophthalmoplegia with multiple mtDNA deletions. Am J Hum Genet 85: 290–295. 10.1016/j.ajhg.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyynismaa H, Sun R, Ahola-Erkkila S et al. (2012). Thymidine kinase 2 mutations in autosomal recessive progressive external ophthalmoplegia with multiple mitochondrial DNA deletions. Hum Mol Genet 21: 66–75. 10.1093/hmg/ddr438. [DOI] [PubMed] [Google Scholar]
- Van Goethem G, Dermaut B, Lofgren A et al. (2001). Mutation of POLG is associated with progressive external ophthalmoplegia characterized by mtDNA deletions. Nat Genet 28: 211–212. 10.1038/90034. [DOI] [PubMed] [Google Scholar]
- Van Goethem G, Martin JJ, Dermaut B et al. (2003a). Recessive POLG mutations presenting with sensory and ataxic neuropathy in compound heterozygote patients with progressive external ophthalmoplegia. Neuromuscul Disord 13: 133–142. 10.1016/s0960-8966(02)00216-x. [DOI] [PubMed] [Google Scholar]
- Van Goethem G, Martin JJ, Van Broeckhoven C (2003b). Progressive external ophthalmoplegia characterized by multiple deletions of mitochondrial DNA: unraveling the pathogenesis of human mitochondrial DNA instability and the initiation of a genetic classification. NeuroMolecular Med 3: 129–146. 10.1385/NMM:3:3:129. [DOI] [PubMed] [Google Scholar]
- Van Goethem G, Schwartz M, Lofgren A et al. (2003c). Novel POLG mutations in progressive external ophthalmoplegia mimicking mitochondrial neurogastrointestinal encephalomyopathy. Eur J Hum Genet 11: 547–549. 10.1038/sj.ejhg.5201002. [DOI] [PubMed] [Google Scholar]
- Viscomi C, Zeviani M (2017). MtDNA-maintenance defects: syndromes and genes. J Inherit Metab Dis 40: 587–599. 10.1007/s10545-017-0027-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visuttijai K, Hedberg-Oldfors C, Lindgren U et al. (2021). Progressive external ophthalmoplegia associated with novel MT-TN mutations. Acta Neurol Scand 143: 103–108. 10.1111/ane.13339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vivian AJ (2020). Congenital fibrosis of the extra-ocular muscles (CFEOM) and the cranial dysinnervation disorders. Eye (Lond) 34: 251–255. 10.1038/s41433-019-0700-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Gräefe A (1868). Verhandlungen ärztlicher Gesellschaften. Berl Klin Wochenschr 5: 125–127. [Google Scholar]
- Wang J, Kim E, Dai H et al. (2018). Clinical and molecular spectrum of thymidine kinase 2-related mtDNA maintenance defect. Mol Genet Metab 124: 124–130. 10.1016/j.ymgme.2018.04.012. [DOI] [PubMed] [Google Scholar]
- Wedding IM, Koht J, Tran GT et al. (2014). Spastic paraplegia type 7 is associated with multiple mitochondrial DNA deletions. PLoS One 9: e86340. 10.1371/journal.pone.0086340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilbrand H, Saenger. (1900). Die ptosis bei der chronischen, progressiven aber isoliert bleibenden ophthalmoplegia exterior. Die Neurologie des Auges: Ein Handbuch für Nerven- und Augenärzte, Bergmann JF, Münich, Wiesbaden, pp. 117–133. [Google Scholar]
- Wilichowski E, Korenke GC, Ruitenbeek W et al. (1998). Pyruvate dehydrogenase complex deficiency and altered respiratory chain function in a patient with Kearns-Sayre/MELAS overlap syndrome and A3243G mtDNA mutation. J Neurol Sci 157: 206–213. 10.1016/s0022-510x(98)00068-9. [DOI] [PubMed] [Google Scholar]
- Wolf J, Obermaier-Kusser B, Jacobs M et al. (2012). A new mitochondrial point mutation in the transfer RNA(Lys) gene associated with progressive external ophthalmoplegia with impaired respiratory regulation. J Neurol Sci 316: 108–111. 10.1016/j.jns.2012.01.013. [DOI] [PubMed] [Google Scholar]
- Yamamoto M, Nonaka I (1988). Skeletal muscle pathology in chronic progressive external ophthalmoplegia with ragged-red fibers. Acta Neuropathol 76: 558–563. 10.1007/BF00689593. [DOI] [PubMed] [Google Scholar]
- Yamashita S (2021). Recent progress in oculopharyngeal muscular dystrophy. J Clin Med 10. 10.3390/jcm10071375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J, Deng J, Wang Z (2022). Oculopharyngodistal myopathy. Curr Opin Neurol 35: 637–644. 10.1097/WCO.0000000000001089. [DOI] [PubMed] [Google Scholar]
- Yu-Wai-Man P, Griffiths PG, Gorman GS et al. (2010). Multi-system neurological disease is common in patients with OPA1 mutations. Brain 133: 771–786. 10.1093/brain/awq007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeviani M, Moraes CT, DiMauro S et al. (1988). Deletions of mitochondrial DNA in Kearns-Sayre syndrome. Neurology 38: 1339–1346. 10.1212/wnl.38.9.1339. [DOI] [PubMed] [Google Scholar]
- Zsurka G, Schroder R, Kornblum C et al. (2004). Tissue dependent co-segregation of the novel pathogenic G12276A mitochondrial tRNALeu(CUN) mutation with the A185G D-loop polymorphism. J Med Genet 41: e124. 10.1136/jmg.2004.022566. [DOI] [PMC free article] [PubMed] [Google Scholar]