Abstract
Age-related distance esotropia (ARDET) is characterized by an esodeviation greater at distance than near in older aged patients and generally managed with prism spectacles or surgery. The purpose of this study is to describe the prevalence, clinical characteristics, and natural history of age-related distance esotropia in a defined population. The medical records of all adult (≥19 years of age) residents of Olmsted County, Minnesota, diagnosed with an esodeviation at least 2 prism diopters (PD) greater at distance than near, from January 1, 1985, through December 31, 2004, were retrospectively reviewed. Seventy-three (9.7%) of 751 new cases of adult-onset strabismus were diagnosed with age-related distance esotropia during the 20-year period. The mean age of onset was 70 years (range, 19 to 93 years) and 48 (65.8%) were female (p=0.007). The mean angle of esodeviation was 7.6 (range, 2 to 20) prism diopters (PD) at distance and 0.4 (range, 10 PD of XT to 12 PD of ET) PD at near. The Kaplan-Meier rate of progression, as defined by a ≥ 6 prism diopter (PD) increase in esotropia, was 50% by 15 years after diagnosis. Half of the patients had hypertension while one-third had coronary artery disease or other cardiac co-morbidities. Age-related distance esotropia comprised 1 in 10 adults with new-onset strabismus in this population and was significantly more common among women. Hypertension and cardiovascular disease may be risk factors for this form of strabismus and approximately half of the patients worsened over a 15-year period.
Keywords: Esotropia, Strabismus, Adult, Distance Esotropia, Divergence Insufficiency
Age-related distance esotropia (ARDET) is an acquired disorder of ocular alignment characterized by an esodeviation greater at distance than near with relatively normal versions and comitant horizontal measurements.1 Patients typically complain of a gradual onset of horizontal diplopia for distance viewing and are often asymptomatic at near. The previous terminology for this disorder has included divergence insufficiency,2,3 primary divergence insufficiency,4,5 divergence weakness,6 adult-onset divergence insufficiency esotropia,7 and adult onset age-related distance esotropia.8 Although a number of etiologic causes have been suggested,1,6,9–12 the underlying abnormality in this disease is unknown and may include more than one mechanism. Patients are generally managed with prism glasses or strabismus surgery.7–9,13–16
Although there exist a number of studies on ARDET, 1,5–9,13,14,16–18 most are small case series focused on surgical outcomes with limited clinical data. There are currently no published population-based studies describing the clinical characteristics and natural history of ARDET. The primary objective of this study is to describe the clinical characteristics and early natural history of age-related distance esotropia diagnosed among a population-based cohort of adults over a 20-year period.
Materials and methods
The medical records of all patients 19 years of age and older who were residing in Olmsted County, Minnesota, and diagnosed with distance esotropia from January 1, 1985, through December 31, 2004, were retrospectively reviewed. Potential cases of ARDET were identified using the resources of the Rochester Epidemiology Project, a regional collaboration of medical data designed to capture all patient-physician encounters in Olmstead County, Minnesota.19 The racial distribution of Olmsted County, Minnesota in 2000 was 90.3% white, 4.2% Asian, 2.7% African American, 2.4% Hispanic or Latino, 2.4% other or multiracial, and 0.2% American Indian. The county population (124,277 in 2000) is relatively isolated from other urban areas and essentially all medical care is provided to residents by Mayo Clinic or Olmsted Medical Group and affiliated hospitals.
This study was approved by the Institutional Review Board at Mayo Clinic and Olmsted Medical Group and was compliant with the Health Insurance Portability and Accountability Act (HIPAA). The medical records of all patients aged ≥ 19 years who were diagnosed from January 1, 1985, through December 31, 2004, as having an esotropia measuring at least 2 prism diopters (PD) greater at distance than near were reviewed. Patients with a paralytic or restrictive cause of their deviation were excluded. The medical record of each patient was reviewed, and all systemic and ocular co-morbidities present at the time of diagnosis were identified. The deviations were generally measured by prism and alternate cover test (PACT) at distance and near. Disease progression was defined by an increase in the distance deviation of 6 or more prism diopters based on a previous study of test-retest variability of distance esotropia measurements using prism and alternate cover measurements.20
The overall incidence was estimated using age- and sex-specific population figures from Olmsted County, with inter-census years estimated by linear interpolation. Incidence rates were age- and/or sex-adjusted to the 2010 census figures for the U.S. white population to allow data to be compared to the national population estimate from the census figures. The percentage of females was tested against the expectation of 50% using a one sample binomial test. The probability of progression was estimated using the Kaplan-Meier method.21 Data analysis was performed using SAS Version 9.4 (SAS Institute; Cary, North Carolina).
Results
Seventy-three (9.7%) of 751 patients with adult-onset strabismus were diagnosed with distance esotropia during the 20-year study period. The age- and gender-adjusted annual incidence rate for age-related distance esotropia was 5.8 (95% confidence interval 4.4–7.1) per 100,000 residents per year for those 19 years of age or older. Table 1 shows the historical and initial clinical characteristics of the study cohort. ARDET presented at a mean age of 70 years (range, 19 to 93 years), was more common among women (p=0.007), and 60 (82.2%) had symptoms of diplopia. The mean initial deviation was 7.6 PD (range, 2 to 20 PD ET) at distance and 0.4 PD (range, −10 PD exophoria to 12 esotropia) at near. Among the 9 (12.3%) patients aged < 40 years, the mean initial deviation at distance was 10 PD (range, 4 to 20 PD ET) and at near was 5.4 PD of esodeviation (range, 0 to 12 PD ET). While 18 (24.7%) patients had an initial exodeviation at near, none of the patients less than 40 years had an exodeviation at near. Forty-four (60.2%) of the patients had 6 PD or more of esodeviation at distance, while 23 (31.5%) patients had less than 6 PD and 6 (8.2%) had less than 4 PD at the initial presentation. Of the 6 patients with less than 4 PD of esodeviation at the time of presentation, all were noted to be symptomatic with diplopia at distance. A number of ocular and systemic comorbidities were observed among the 73 patients at the time of their diagnosis of distance esotropia as shown in Table 2. The most common ocular co-morbidity was macular degeneration, reported in 17 (23.3%), while arterial hypertension was observed in 37 (50.7%) and heart disease in 26 (35.6%).
Table 1.
Historical and initial clinical characteristics of 73 patients diagnosed with age-related distance esotropia in Olmsted County, MN from 1985 through 2004
| Patient Characteristic | Number |
|---|---|
| Mean age at onset of symptoms (range) | 70 years (19 to 93 years) |
| Median age (standard deviation) | 74 years (± 18 years) |
| Age 19 through 39 years (%) | 9 (12.3) |
| Age 40 through 59 years (%) | 6 (8.2) |
| Age 60 years and older (%) | 58 (79.5) |
| Gender (%) | 48 females (65.8) |
| Diplopia at presentation (%) | 60 (82.2) |
| Mean strabismic deviation at distance (Range) | 7.5 PD ET (2 to20) |
| Mean strabismic deviation at near (Range) | 0.5 PD ET (10PD XT to 12PD ET) |
| Difference between distance and near deviation (Range) | 6.9 PD ET (1 to 16) |
XT = exotropia, ET = esotropia
Table 2.
Observed ocular and systemic comorbidities among 73 adults with age-related distance esotropia
| Ocular diagnoses | Number of patients (%) |
|---|---|
| Age related macular degeneration | 17 (23.3) |
| High myopia | 6 (8.2) |
| Corneal dystrophy | 6 (8) |
| Glaucoma | 5 (6.9) |
| Retinal detachment | 2 (2.7) |
| Epiretinal membrane | 2 (2.7) |
| Retinal detachment with scleral buckle | 2 (2.7) |
| Systemic Diseases | |
| Hypertension | 37 (50.7) |
| Coronary/heart disease | 26 (35.6) |
| Hyperlipidemia | 9 (12.3) |
| Thyroid disease | 7 (9.6) |
| Diabetes mellitus | 6 (8.2) |
| History of stroke | 6 (8.2) |
| History of radiation | 2 (2.7) |
Fifty-four patients (74.0%) were initially treated with prism glasses while the remaining 19 (26.0%) were observed without treatment. During a mean follow-up of 99 months (range, 0 to 312 months), 17 (23.2%) patients had an increase in their distance esotropia by 6 or more prism diopters. The Kaplan-Meier rate of increasing by 6 or more PD occurred in 4.4% (95% CI 0–10.3 %) by 5 years after diagnosis, 24.9% (95% CI 10.5–39.3%) by 10 years, and 50.2% (95% CI 30.9–69.6%) by 15 years, as shown in the Figure. Seven patients (9.6%) clinically resolved and no longer complained of diplopia or required prism correction. Among these seven patients, the mean age at onset was 58 (range, 19 to 83 years) and the mean initial deviation at distance was 5.4 PD (range 4 to 7 PD ET) and 0.3 PD (range, −5 PD exophoria to 5 esotropia) at near. Ten (13.7%) patients eventually underwent a variety of extraocular muscle surgeries at an average age of 61.8 years (range, 25 to 92). Among these, 5 (6.9%) patients had bilateral medial rectus recessions, 2 (2.7%) had unilateral recession/resection, 2 (2.7%) had single lateral rectus resections, and the remaining patient had a bilateral lateral rectus resection (n=1). Following surgery, 5 patients had a recurrence of esotropia managed with prism glasses, 3 remained stable, 1 developed convergence insufficiency and hypertropia, and 1 developed a skew deviation following brain radiotherapy.
Figure.
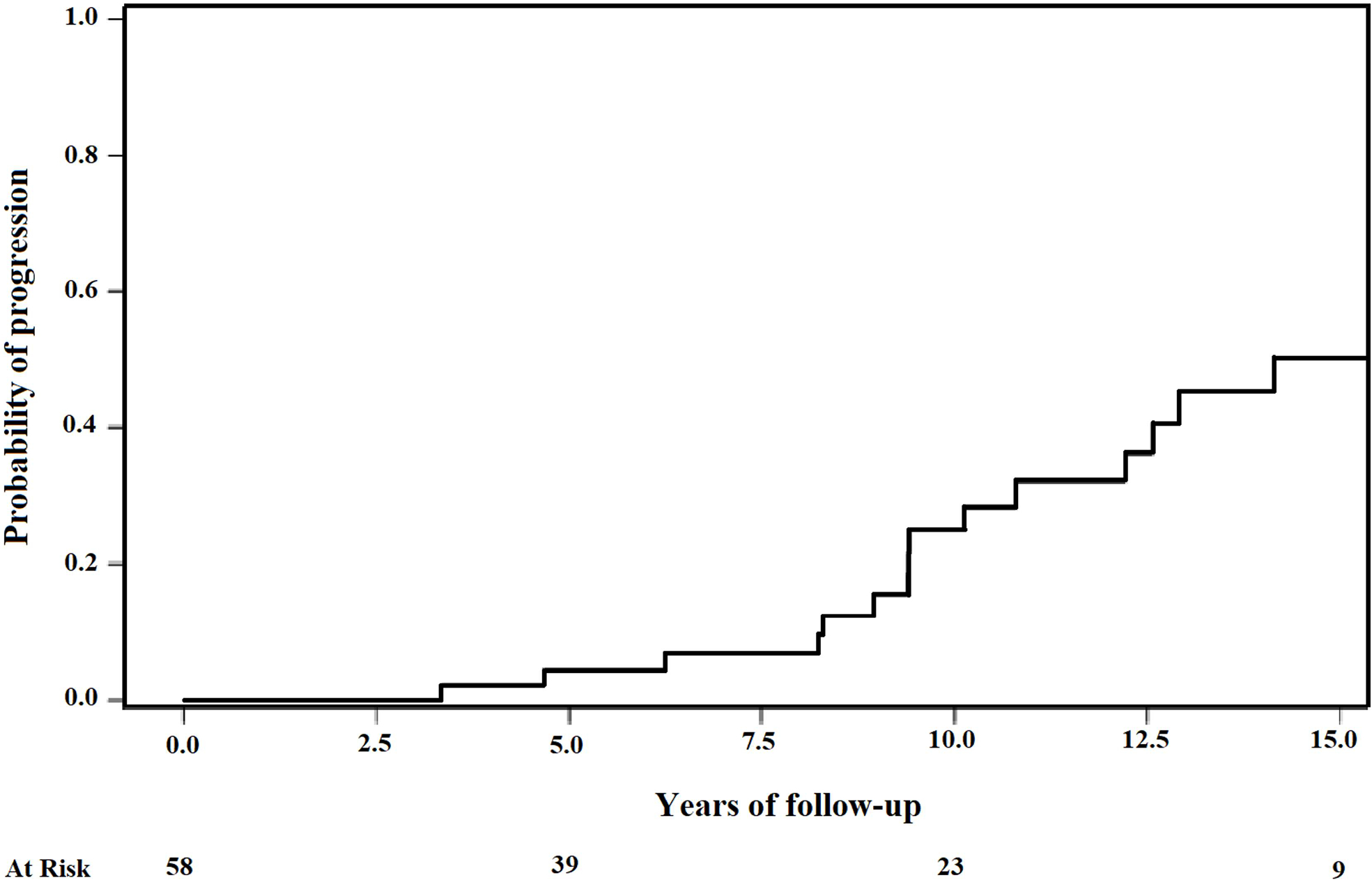
Kaplan-Meier rate of 73 adults with age-related distance esotropia increasing by 6 prism diopters or more over time (years)
Discussion
In this population-based cohort of adults diagnosed with new-onset strabismus over a 20-year period, age-related distance esotropia comprised approximately 1 in 10 new diagnoses. The patients were predominantly female in the seventh decade of life and half had an increase of their distance esotropia after 15 years of observation.
Comparable studies on the clinical characteristics and natural history of ARDET are essentially non-existent, with no known prior population-based studies. In a retrospective review from a single institution, El-Sahn22 and colleagues reported a 21.6% prevalence of esotropia among adults over age 60 with strabismus. Similarly, Repka and Coleman23 reported a 22% prevalence of esotropia among Medicare beneficiaries with strabismus. However, neither of these studies provided information on the prevalence or characteristics of specific sub-types of esotropia, including ARDET.
The clinical features of patients with ARDET in this report are similar to prior studies. An older age at presentation observed in this cohort has been previously reported1,5–8,14,18 and, while some small case series have observed equal gender ratios,2,5,6,13 larger studies have found a greater proportion of females affected by ARDET,1,14,18,24 including Repka and Downing7 who reported a 61% female predominance in a series of 85 patients. Although an association between increased axial length in myopic patients and ARDET has been proposed,25 prior series have been comprised of mostly myopes,24 mostly hyperopes,2 or a similar proportion of both.18 Among the phakic patients in this study, 48.0% were hyperopic, 31.5% were myopic, and the remainder had mixed astigmatism or emmetropia. Although six of the patients in this study had high myopia (>6.00 D), none were believed to have progressive esotropia due to high myopia,26 an entity with different clinical findings and surgical implications.27–29
Multiple hypotheses have been proposed to explain the etiology of ARDET. Lyle has suggested that a microvascular compromise affecting the ‘divergence center’ in the midbrain as the etiology.12 Many patients in this cohort had medical co-morbidities associated with microvascular compromise, including hypertension and diabetes mellitus; however, without a control group it is not possible to establish such an association. The theory of microvascular compromise as an etiology of ARDET lacks evidence in the literature and warrants further study. Progressive addition lenses were recently reported to be associated with this condition, with improper use suggested to cause medial rectus muscle shortening as a mechanism for divergence insufficiency.30 Age-related changes and mechanical perturbations such as a decrease in fusional divergence amplitudes,6,31 loss of medial rectus elasticity,9 and peripheral muscle abnormalities,10,11 have also been proposed as causes of ARDET. Demer and colleagues have suggested that age-related laxity of the band between the superior rectus and lateral rectus muscle pulleys are implicated in the development of ARDET.10 Should age-related orbital changes be the exclusive etiology of ARDET, one would not expect patients to have clinical improvement over time. While uncommon, nearly 10% of this study cohort experienced clinical resolution.
The natural course of this form of adult strabismus has been reported to be variable. Some investigators have suggested that the disease remains stable,6 while others have reported spontaneous resolution.5 Recently, Godts et al18 reported an increase in the distance esodeviation of 2 PD by 5-years of follow-up. Our data indicate that half the patients progressed within 15 years of diagnosis. Although this population-based cohort had 7 patients (9.6%) who clinically resolved and no longer complained of diplopia or required prism correction, the majority of patients remained stable or demonstrated an increase in their angle of deviation. Age-related distance esotropia has generally been treated conservatively, most often with prism management.1–3,7,18 Patients in this study were managed similarly with 54 (74.0%) treated initially with prisms and 19 (26.0%) with simple observation. Ten patients eventually underwent extraocular muscle surgery, of which approximately half developed recurrent esotropia.
There are several limitations to the findings of this study. Its retrospective design is limited by non-standardized and incomplete data collection. Second, this investigation was performed in a racially homogenous population in a single geographic area. Extrapolating the findings from this study to groups not represented within our community is problematic. Finally, the angle of deviation in some patients was measured using maddox-rod measurements which may differ from prism and alternate cover testing, and may adversely affect the assessment of progression over time. Nevertheless, their use did not affect the accuracy of the diagnosis, which was confirmed over multiple visits for most patients.
The findings from this population-based cohort suggest that age-related distance esotropia is relatively common, occurring in approximately 1 in 10 adults with new-onset strabismus. Most patients were females in the seventh decade of life. Hypertension and cardiovascular disease were relatively common in these patients and one half demonstrated an increase in their angle of deviation after 15 years of observation.
Acknowledgments
Supported in part by the National Institute on Aging of the National Institutes of Health (NAI; 15 AG058738)
Footnotes
No authors have any financial/conflicting interest to disclose.
Disclosure of Interest
This study was supported in part by the National Institute on Aging of the National Institutes of Health (NAI;15 AG058738). No authors have any financial or conflicting interest to disclose.
References
- 1.Mittelman D Age-related distance esotropia. JAAPOS. 2006;10(3):212–213. doi: 10.1016/j.jaapos.2006.01.217. [DOI] [PubMed] [Google Scholar]
- 2.Prangen Ade H, Koch FL. Divergence Insufficiency: A Clinical Study. Trans Am Ophthalmol Soc. 1937;35:136–148. [PMC free article] [PubMed] [Google Scholar]
- 3.Scheiman M, Gallaway M, Ciner E. Divergence insufficiency: characteristics, diagnosis, and treatment. Am J Optom Physiol Opt. 1986;63(6):425–431. [PubMed] [Google Scholar]
- 4.Simpson GV. Primary divergence insufficiency. Trans Am Ophthalmol Soc. 1973;71:152–161; discussions 161–152. [PMC free article] [PubMed] [Google Scholar]
- 5.Jacobson DM. Divergence insufficiency revisited: natural history of idiopathic cases and neurologic associations. Arch Ophthalmol. 2000;118(9):1237–1241. doi: 10.1001/archopht.118.9.1237. [DOI] [PubMed] [Google Scholar]
- 6.Wiggins RE Jr., Baumgartner S Diagnosis and management of divergence weakness in adults. Ophthalmology. 1999;106(7):1353–1356. doi: 10.1016/S0161-6420(99)00724-1. [DOI] [PubMed] [Google Scholar]
- 7.Repka MX, Downing E. Characteristics and surgical results in patients with age-related divergence insufficiency esotropia. JAAPOS. 2014;18(4):370–373. doi: 10.1016/j.jaapos.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Mittelman D Surgical management of adult onset age-related distance esotropia. J Pediatr Ophthalmol Strabismus. 2011;48(4):214–216; quiz 217. doi: 10.3928/01913913-20100818-04. [DOI] [PubMed] [Google Scholar]
- 9.Bothun ED, Archer SM. Bilateral medial rectus muscle recession for divergence insufficiency pattern esotropia. JAAPOS. 2005;9(1):3–6. doi: 10.1016/j.jaapos.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhuri Z, Demer JL. Sagging eye syndrome: connective tissue involution as a cause of horizontal and vertical strabismus in older patients. JAMA Ophthalmol. 2013;131(5):619–625. doi: 10.1001/jamaophthalmol.2013.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawai M, Goseki T, Ishikawa H, et al. Characterization of the position of the extraocular muscles and orbit in acquired esotropia both at distance and near using orbital magnetic resonance imaging. PLoS One. 2021;16(3):e0248497. doi: 10.1371/journal.pone.0248497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyle DJ. Divergence insufficiency. AMA Arch Ophthalmol. 1954;52(6):858–864. [DOI] [PubMed] [Google Scholar]
- 13.Thomas AH. Divergence insufficiency. JAAPOS. 2000;4(6):359–361. doi: 10.1067/mpa.2000.111783. [DOI] [PubMed] [Google Scholar]
- 14.Ridley-Lane M, Lane E, Yeager LB, Brooks SE. Adult-onset chronic divergence insufficiency esotropia: clinical features and response to surgery. JAAPOS. 2016;20(2):117–120. doi: 10.1016/j.jaapos.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Chaudhuri Z, Demer JL. Divergence insufficiency esotropia is a misnomer-reply. JAMA Ophthalmol. 2013;131(4):547–548. doi: 10.1001/jamaophthalmol.2013.2412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breidenstein BG, Robbins SL, Granet DB, Acera EC. Comparison of the Efficacy of Medial Rectus Recession and Lateral Rectus Resection for Treatment of Divergence Insufficiency. J Pediatr Ophthalmol Strabismus. 2015;52(3):173–176. doi: 10.3928/01913913-20150427-07. [DOI] [PubMed] [Google Scholar]
- 17.Berscheid C Divergence insufficiency. Am Orthopt J. 2005;55:106–111. doi: 10.3368/aoj.55.1.106. [DOI] [PubMed] [Google Scholar]
- 18.Godts D, Deboutte I, Mathysen DGP. Long-term evolution of age-related distance esotropia. JAAPOS. 2018;22(2):97–101. doi: 10.1016/j.jaapos.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Melton LJ 3rd. History of the Rochester Epidemiology Project. Mayo Clinic proceedings. 1996;71(3):266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 20.PEDIG. Interobserver reliability of the prism and alternate cover test in children with esotropia. Arch Ophthalmol. 2009;127(1):59–65. Pediatric Eye Disease Investigator Group. doi: 10.1001/archophthalmol.2008.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaplan ELM, Paul. Nonparametric Estimation from Incomplete Observations. Journal of the American Statistical Association. 1958;53(282):457–481. [Google Scholar]
- 22.El-Sahn MF, Granet DB, Marvasti A, Roa A, Kinori M. Strabismus in Adults Older Than 60 Years. J Pediatr Ophthalmol Strabismus 2016;53(6):365–368. doi: 10.3928/01913913-20160722-02. [DOI] [PubMed] [Google Scholar]
- 23.Repka MX, Yu F, Coleman A. Strabismus among aged fee-for-service Medicare beneficiaries. JAAPOS s. 2012;16(6):495–500. doi: 10.1016/j.jaapos.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Moore S, Harbison JW, Stockbridge L. Divergence insufficiency. Am Orthopt J. 1971;21:59–63. [PubMed] [Google Scholar]
- 25.Kohmoto H, Inoue K, Wakakura M. Divergence insufficiency associated with high myopia. Clin Ophthalmol. 2010;5:11–16. doi: 10.2147/OPTH.S14759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hayashi T, Iwashige H, Maruo T. Clinical features and surgery for acquired progressive esotropia associated with severe myopia. Acta Ophthalmol Scand. 1999;77(1):66–71. doi: 10.1034/j.1600-0420.1999.770115.x. [DOI] [PubMed] [Google Scholar]
- 27.Yokoyama T, Ataka S, Tabuchi H, Shiraki K, Miki T. Treatment of progressive esotropia caused by high myopia—a new surgical procedure based on its pathogenesis. Paper presented at: Transactions: 27th Meeting, European Strabismological Association, Florence, Italy2001. [Google Scholar]
- 28.Shenoy BH, Sachdeva V, Kekunnaya R. Silicone band loop myopexy in the treatment of myopic strabismus fixus: surgical outcome of a novel modification. Br J Ophthalmol. 2015;99(1):36–40. doi: 10.1136/bjophthalmol-2014-305166. [DOI] [PubMed] [Google Scholar]
- 29.Farid MF, Elbarky AM, Saeed AM. Superior rectus and lateral rectus muscle union surgery in the treatment of myopic strabismus fixus: three sutures versus a single suture. JAAPOS. 2016;20(2):100–105. doi: 10.1016/j.jaapos.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 30.Chen X, Marsh JD, Zafar S, Gerber EE, Guyton DL. Increasing incidence and risk factors for divergence insufficiency esotropia. J AAPOS. 2021. Oct;25(5):278.e1–278.e6. doi: 10.1016/j.jaapos.2021.05.013. Epub 2021 Sep 25. [DOI] [PubMed] [Google Scholar]
- 31.Oatts JT, Salchow DJ. Age-related distance esotropia--fusional amplitudes and clinical course. Strabismus. 2014. Jun;22(2):52–7. doi: 10.3109/09273972.2014.904895. Epub 2021 Sep 25. [DOI] [PubMed] [Google Scholar]


