Abstract
Objectives
The body mass index (BMI) largely underestimates excess body fat, suggesting that the prevalence of obesity could be underestimated. Biologically, women are known to have higher body fat than men. This study aimed to compare the temporal trends in general obesity by sex, ethnicity and age among adults in the USA using the relative fat mass (RFM), a validated surrogate for whole-body fat percentage and BMI.
Design
Population-based study.
Setting
US National Health and Nutrition Examination Survey, from 1999–2000 to 2017–March 2020.
Participants
A representative sample of adults 20–79 years in the USA.
Main outcome measures
Age-adjusted prevalence of general obesity. RFM-defined obesity was diagnosed using validated cut-offs to predict all-cause mortality: RFM≥40% for women and ≥30% for men. BMI-defined obesity was diagnosed using a cut-off of 30 kg/m2.
Results
Analysis included data from 47 667 adults. Among women, RFM-defined obesity prevalence was 64.7% (95% CI 62.1% to 67.3%) in 2017–2020, a linear increase of 13.9 percentage points (95% CI 9.0% to 18.9%; p<0.001) relative to 1999–2000. In contrast, the prevalence of BMI-defined obesity was 42.2% (95% CI 39.4% to 45.0%) in 2017–2020. Among men, the corresponding RFM-defined obesity prevalence was 45.8% (95% CI 42.0% to 49.7%), a linear increase of 12.0 percentage points (95% CI 6.6% to 17.3%; p<0.001). In contrast, the prevalence of BMI-defined obesity was 42.0 (95% CI 37.8% to 46.3%). The highest prevalence of RFM-defined obesity across years was observed in older adults (60–79 years) and Mexican Americans, in women and men. Conversely, the highest prevalence of BMI-defined obesity across years was observed in middle-age (40–59 years) and older adults, and in African American women.
Conclusions
The use of a surrogate for whole-body fat percentage revealed a much higher prevalence of general obesity in the USA from 1999 to 2020, particularly among women, than that estimated using BMI, and detected a disproportionate higher prevalence of general obesity in older adults and Mexican Americans.
Keywords: epidemiology, public health, general endocrinology, general medicine (see internal medicine), obesity
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Relative fat mass (RFM) is a validated surrogate for whole-body fat percentage that has a high diagnostic accuracy (91%) for dual-energy X-ray absorptiometry-defined obesity.
The diagnosis of obesity was based on measured anthropometrics and validated RFM cut-offs associated with increased risk for all-cause mortality.
RFM requires only waist circumference and height for its calculation.
The proportion of obesity misclassification is not trivial when using RFM.
Estimates of temporal trends in obesity were not possible for Asian Americans.
Introduction
The prevalence of obesity (excess body fat) in the USA has doubled from 15.0% in 1976–1980 to 30.9% in 1999–2000,1 and it continues to increase.2 3 The age-adjusted prevalence of obesity among adults in the USA has been estimated at 41.9% in 2017–March 2020.4 Obesity diagnosis is based on the body mass index (BMI), an indirect measure of body fat.5 6 BMI is calculated as the ratio of body weight in kilograms to the square of the height in metres.7 BMI does not distinguish between fat mass and fat-free mass and does not account for differences in adiposity between women and men. Biologically, women are known to have higher body fat than men.8–12 A meta-analysis of 25 international studies comprising nearly 32 000 adults concluded that BMI underestimates ~50% of all individuals with excess body fat percentage determined by reference techniques,11 suggesting that the prevalence of obesity could be largely underestimated among countries.
There is robust evidence linking high whole-body fat percentage with increased risk of death,13–20 supporting the need for a better assessment of body adiposity. Although the limitations of BMI to assess body adiposity are widely acknowledged,6 8–11 21 22 BMI remains the most widely used anthropometric index in clinical practice, epidemiology and public health, given its simplicity, very low cost, and its association with several clinical conditions and mortality.6 The high cost and time required to assess body adiposity using more accurate techniques such as dual-energy X-ray absorptiometry (DXA), dual-labelled water or MR, prevents their use in large populations or clinical practice as part of routine screening.
The relative fat mass (RFM) is a simple and low-cost anthropometric index developed to estimate whole-body fat percentage.23 RFM is a linear equation based on the ratio of height to waist circumference that has been validated in Mexican, European and African Americans,23 and in other populations.24–26 Compared with BMI, RFM resulted in lower obesity misclassification when DXA was used as the reference method for diagnosing obesity in adults.24 27 The accuracy of RFM in diagnosing high body fat percentage is superior to that of BMI among men and similar to BMI among women.23 In an analysis of a representative sample of the US adult population (National Health and Nutrition Examination Survey, NHANES 1999–2006), RFM had a diagnostic accuracy of 91% (C-statistic=0.91) for DXA-defined obesity in women and men.27
Recent studies have examined the US prevalence trends in obesity using BMI as diagnostic tool.3 28 29 Although data on body fat percentage have also been reported for the US adult population,28 no body fat cut-offs were used to diagnose general obesity, and the analyses were limited to adults 20–59 years only, and for the period 2011–2018. In fact, body composition has been inconsistently assessed across NHANES survey cycles and across age groups. In addition, no study has compared the trends of general obesity in the USA using RFM, a surrogate for body fat percentage and BMI. Furthermore, no study has examined current obesity trends among US adults over a period of nearly 22 years. The aim of this study was to compare the temporal trends in general obesity by sex, ethnicity and age group among adults in the USA from 1999 to 2020 using RFM and BMI.
Material and methods
Study design, data source and participants
In this population-based study, we performed an analysis of cross-sectional individual-level data collected by the NHANES through interviews and physical examination in a subset of a representative sample of the US population from 1999–2000 to 2017–March 2020. Initial complete dataset included 107 622 participants of all ages. NHANES suspended data collection in March 2020 as a consequence of the COVID-19 pandemic. Thus, the most current cycle data available are ‘combined data collected from 2019 to March 2020 with data from the NHANES 2017–2018 cycle to form a nationally representative sample of NHANES 2017–March 2020 prepandemic data’.30 Analysis was restricted to adults 20–79 years of age (n=54 232 potentially eligible) because of three reasons: (1) the diagnosis of obesity in younger adults is based on BMI-for-age percentiles as recommended by the Centers for Disease Control and Prevention7; (2) in NHANES 2007–2008 and subsequent cycles, the upper age limit was 80 years, whereas in earlier cycles the age limit was 85 years and (3) to obtain age-adjusted prevalence estimates using 5-year intervals according to the strata for age and sex available from the 2000 US Census Bureau (20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74 and 75–79).31 Another criterion for inclusion was that individuals had been interviewed and evaluated by physical examination. Women who reported to be pregnant or had a positive urine pregnancy test were excluded from analysis. Observations with missing data on body weight, height or waist circumference were also excluded.
According to the NHANES physical examination protocol, waist circumference was measured just above the uppermost lateral border of the right ilium (hip bone). Weight and height were measured using standard methods.32 Information on ethnicity was collected through a questionnaire. The mean unweighted response rate for the examined sample across survey cycles between 1999–2000 and 2017–March 2020 for individuals 20–79 years was 67.5% (range 50.8%–74.5%).33
Obesity diagnosis
General obesity was diagnosed using RFM, a validated surrogate for whole-body fat percentage23 and validated cut-offs to predict all-cause mortality: RFM≥40% for women and ≥30% for men.27 RFM was calculated as follows: RFM=64−(20×height/waist circumference)+(12×sex); sex equals 0 for men and 1 for women.23 BMI-defined obesity was diagnosed if BMI was 30 kg/m2 or higher.7
Statistical analysis
Data collected during the survey cycles from 1999–2000 to 2017–2020 were analysed using sampling weights following the recommended analytical guidelines, to account for oversampling, non-response rates and subsampling for physical examination.34 The proportion of missing data was 5.2% of all eligible participants. Given this low percentage of missing data, we performed a complete case analysis.35 Since age distribution of study samples may vary across survey cycles, all prevalence estimates were adjusted for age to make the estimates more comparable throughout the study period.31 Estimates across the age categories 20–39, 40–59 and 60–79 years were also adjusted for age using 5-year intervals according to corresponding 2000 US Census Bureau age categories by sex.31 The changes in obesity prevalence from 1999–2000 to 2017–March 2020 were assessed using the Wald test. For multiple comparisons of prevalence across ethnic groups and age groups, we applied the Bonferroni correction. Because Asian Americans were not oversampled before NHANES 2011, our analyses by ethnicity were restricted to Mexican, European and African Americans.
To determine the possible role of menopause in the high prevalence of RFM-defined obesity in women, we performed a post hoc analysis. Data related to menopause were self-reported. We defined postmenopausal women as those with natural menopause and no missing information on age at menopause. For this analysis, women were excluded if menopause occurred before age 40 or after age 62,36 or if they reported oophorectomy (surgical removal of one or two ovaries), treatment with oestrogen/progesterone for hysterectomy/oophorectomy, breast feeding, pregnancy in past year of the interview, or irregular period due to medical conditions or treatment.
Temporal trends in prevalence of obesity were tested for the assumption of linearity using logistic regression models, comparing linear and non-linear regression models using the likelihood-ratio test.37 For the non-linear models, restricted cubic splines with three knots were used at years 2001–2002, 2009–2010 and 2017–2020, based on the quantiles recommended by Harrel.38 Survey cycles were analysed as a continuous variable. For visualisation purposes, trend lines were smoothed using the locally weighted scatterplot smoothing (LOWESS) method.39 Statistical significance was set to an alpha level of 0.05. All statistical analyses were performed using Stata V.14 for Windows (StataCorp). Prevalence estimates and standard errors were obtained using the survey ‘svy’ command with Taylor linearisation.
Patient and public involvement
Patients and the public were not involved in this study. This study will be available to the public once it is published in the scientific literature.
Results
Clinical characteristics
After applying the inclusion and exclusion criteria, the final sample for analysis comprised 47 667 adults (online supplemental figure 1). The median age of the study population was 45 years (IQR 33–58); 50.6% were women; 67.2% were European Americans, 11.2% were African Americans and 8.3% were Mexican Americans (table 1).
Table 1.
Characteristics of study participants*
| Characteristic | All 47 667 |
Women 23 931 (50.6%) |
Men 23 736 (49.4%) |
| Median age (IQR), years | 45 (33–58) | 46 (33–59) | 44 (32–57) |
| Ethnicity, n (%) | |||
| Mexican American | 8416 (8.3) | 4204 (7.7) | 4212 (9.0) |
| European American | 19 691 (67.2) | 9710 (67.0) | 9981 (67.5) |
| African American | 10 673 (11.2) | 5417 (12.0) | 5256 (10.4) |
| Other/multi-racial | 8887 (13.3) | 4600 (13.4) | 3928 (13.1) |
| Body weight (SD), kg | 82.6 (21.3) | 76.3 (20.5) | 89.0 (20.1) |
| Mean height (SD), cm | 168.9 (10.0) | 162.1 (6.9) | 175.9 (7.5) |
| Mean waist circumference (SD), cm | 98.5 (16.5) | 95.9 (16.9) | 101.2 (15.6) |
| Mean BMI (SD), kg/m2 | 28.9 (6.8) | 29.0 (7.5) | 28.7 (5.9) |
| Mean RFM (SD), % | 34.9 (8.5) | 41.2 (6.0) | 28.4 (5.3) |
| RFM-defined obesity, % (95% CI)† | 50.1 (48.9 to 50.8) | 59.4 (58.4 to 60.5) | 40.6 (39.4 to 41.8) |
| BMI-defined obesity, % (95% CI)‡ | 36.2 (35.4 to 37.1) | 37.8 (36.8 to 38.7) | 34.6 (33.5 to 35.8) |
| Abdominal obesity, % (95% CI)§ | 54.0 (53.0 to 55.0) | 63.8 (62.8 to 64.9) | 43.9 (42.7 to 45.1) |
*Sample size represents unweighted data. Estimates represent weighted data.
†Defined as having an RFM of 40% or higher for women and an RFM of 30% or higher for men. RFM was calculated as follows: 64−(20×height/waist circumference)+(12×sex); sex equals 0 for men and 1 for women; height and waist circumference were measured in the same units. Estimates were not adjusted for age.
‡Defined as having a BMI of 30 kg/m2 or higher. BMI was calculated as the body weight in kilograms divided by the square of the height in metres. Estimates were not adjusted for age.
§Defined as having a waist circumference of more than 88 cm for women and more than 102 cm for men, according to the recommendations of the National Cholesterol Education Programme Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Estimates were not adjusted for age.
BMI, body mass index; RFM, relative fat mass.
bmjopen-2022-071295supp001.pdf (302.5KB, pdf)
The overall prevalence of obesity by ethnicity in the study participants is shown in online supplemental table 1. The characteristics of the population with missing data are shown in online supplemental table 2.
Obesity prevalence and temporal trends
Our findings indicate a higher proportion of individuals with obesity when RFM was used instead of BMI. The overall age-adjusted prevalence of RFM-defined obesity increased from 42.4% (95% CI 38.3% to 46.4%) in 1999–2000 to 55.4% (95% CI 53.0% to 57.9%) in 2017–March 2020. The corresponding BMI-defined obesity prevalence increased from 30.4% (95% CI 26.7% to 34.0%) to 42.1% (95% CI 39.4% to 44.8%). We found a linear increase in the overall prevalence of obesity during the study period using either RFM (p<0.001; p=0.38 for non-linearity) or BMI (p<0.001; p=0.55 for non-linearity).
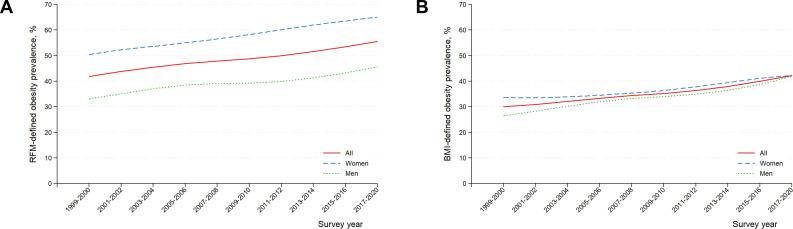
Obesity prevalence and temporal trends by sex
We observed a consistently higher prevalence of RFM-defined obesity in women compared with men across years. In contrast, this difference was not consistent for BMI-defined obesity (figure 1). In 2017–March 2020, the prevalence of RFM-defined obesity was significantly higher in women than in men (p<0.001). In contrast, the prevalence of BMI-defined obesity was similar in women and men (p=0.97). Among women, the prevalence of RFM-defined obesity increased from 50.8% (95% CI 46.2% to 55.3%) in 1999–2000 to 64.7% (95% CI 62.1% to 67.3%) in 2017–March 2020, a linear increase of 13.9 percentage points (95% CI 9.0% to 18.9%; p<0.001). For comparison, the prevalence of BMI-defined obesity in women was 42.2% (95% CI 39.4% to 45.0%) in 2017–March 2020, a linear increase of 8.3 percentage points (95% CI 3.5% to 13.2%; p<0.001) (table 2).
Figure 1.
Age-adjusted US adult prevalence temporal trends in RFM-defined obesity by sex: 1999–2000 to 2017–March 2020. Trend lines were smoothed using the LOWESS method on weighted prevalence estimates. Body fat-defined obesity was determined using the RFM (A). RFM was calculated as follows: RFM=64−(20×height/waist circumference)+ (12×sex); sex equals 0 for men and 1 for women. RFM-defined obesity was diagnosed if RFM was 40% or higher for women and RFM was 30% or higher for men. BMI-defined obesity was diagnosed using a cutoff of 30 kg/m2 (B). BMI, body mass index; LOWESS, locally weighted scatterplot smoothing; RFM, relative fat mass.
Table 2.
Age-adjusted US adult prevalence temporal trends in RFM-defined obesity by sex: 1999–2000 to 2017–Mach 2020*
| RFM-defined obesity | BMI-defined obesity | |
| All participants (n=47 667) | ||
| Prevalence, % (95% CI) | ||
| 1999–2000 | 42.4 (38.3 to 46.4) | 30.4 (26.7 to 34) |
| 2001–2002 | 42.5 (41.1 to 43.9) | 30.0 (27.6 to 32.4) |
| 2003–2004 | 46.9 (44.7 to 49.2) | 32.1 (29.3 to 34.9) |
| 2005–2006 | 47.1 (43.7 to 50.5) | 34.3 (31.1 to 37.4) |
| 2007–2008 | 47.7 (45.0 to 50.5) | 33.7 (31.5 to 36.0) |
| 2009–2010 | 48.5 (46.1 to 50.8) | 35.7 (33.6 to 37.8) |
| 2011–2012 | 49.8 (46.6 to 53.0) | 35.4 (32.5 to 38.3) |
| 2013–2014 | 51.3 (48.7 to 53.8) | 37.8 (35.6 to 40) |
| 2015–2016 | 53.7 (49.3 to 58.0) | 40.0 (36.4 to 43.6) |
| 2017–2020 | 55.4 (53.0 to 57.9) | 42.1 (39.4 to 44.8) |
| Prevalence change† | 13.0 (8.5 to 17.5) | 11.8 (7.4 to 16.1) |
| P for non-linearity‡ | 0.38 | 0.55 |
| P value for trend‡ | <0.001 | <0.001 |
| Women (n=23 931) | ||
| Prevalence, % (95% CI) | ||
| 1999–2000 | 50.8 (46.2 to 55.3) | 33.9 (29.6 to 38.1) |
| 2001–2002 | 51.6 (49.2 to 53.9) | 32.9 (29.7 to 36.0) |
| 2003–2004 | 55.3 (51.2 to 59.3) | 33.5 (29.7 to 37.2) |
| 2005–2006 | 53.9 (50.4 to 57.4) | 34.8 (31.5 to 38.1) |
| 2007–2008 | 56.4 (53.5 to 59.3) | 35.4 (32.7 to 38.0) |
| 2009–2010 | 58.1 (55.3 to 60.8) | 36.0 (34.0 to 37.9) |
| 2011–2012 | 60.8 (56.8 to 63.6) | 36.9 (33.4 to 40.5) |
| 2013–2014 | 61.3 (57.9 to 64.7) | 40.0 (36.8 to 43.2) |
| 2015–2016 | 64.4 (60.2 to 68.6) | 41.7 (38.1 to 45.3) |
| 2017–2020 | 64.7 (62.1 to 67.3) | 42.2 (39.4 to 45.0) |
| Prevalence change† | 13.9 (9.0 to 18.9) | 8.3 (3.5 to 13.2) |
| P for non-linearity§ | 0.10 | 0.39 |
| P value for trend§ | <0.001 | <0.001 |
| Men (n=23 736) | ||
| Prevalence, % (95% CI) | ||
| 1999–2000 | 33.9 (29.9 to 37.8) | 27.0 (23.5 to 30.4) |
| 2001–2002 | 33.1 (30.6 to 35.5) | 27.0 (24.8 to 29.2) |
| 2003–2004 | 38.4 (35.9 to 40.8) | 30.7 (27.6 to 33.9) |
| 2005–2006 | 40.2 (35.9 to 44.4) | 33.5 (29.3 to 37.8) |
| 2007–2008 | 38.8 (35.6 to 42.0) | 32.1 (29.3 to 34.8) |
| 2009–2010 | 38.7 (35.2 to 42.2) | 35.3 (31.4 to 39.2) |
| 2011–2012 | 39.2 (35.9 to 42.5) | 33.8 (30.7 to 36.9) |
| 2013–2014 | 41.2 (38.7 to 43.7) | 35.6 (33.2 to 38.1) |
| 2015–2016 | 42.7 (37.7 to 47.7) | 38.2 (33.3 to 43.2) |
| 2017–2020 | 45.8 (42.0 to 49.7) | 42.0 (37.8 to 46.3) |
| Prevalence change† | 12.0 (6.6 to 17.3) | 15.1 (9.8 to 20.4) |
| P for non-linearity§ | 0.82 | 0.84 |
| P value for trend§ | <0.001 | <0.001 |
*Prevalence estimates represent weighted data. RFM-defined obesity was diagnosed as having an RFM of 40% or higher for women and having an RFM of 30% or higher for men. RFM was calculated as follows: 64−(20×height/waist circumference)+(12×sex); sex equals 0 for men and 1 for women. Height and waist circumference were measured in the same units. BMI-defined obesity was diagnosed as having a BMI of 30 kg/m2 or higher. BMI was calculated as the body weight in kilograms divided by the square of the height in metres. Estimates were not adjusted for age.
†Absolute difference (prevalence in 2017–2020 minus the prevalence in 1999–2000).
‡Adjusted for age, sex and ethinicity.
§Adjusted for age and ethnicity.
BMI, body mass index; RFM, relative fat mass.
Among men, the prevalence of RFM-defined obesity increased from 33.9% (95% CI 29.9% to 37.8%) in 1999–2000 to 45.8% (95% CI 42.0% to 49.7%) in 2017–March 2020, a linear increase of 12.0 percentage points (95% CI 6.6% to 17.3%; p<0.001). The prevalence of BMI-defined obesity in men was 42.0% (95% CI 37.8% to 46.3%) in 2017–March 2020, a linear increase of 15.1 percentage points (95% CI 9.8% to 20.4%).
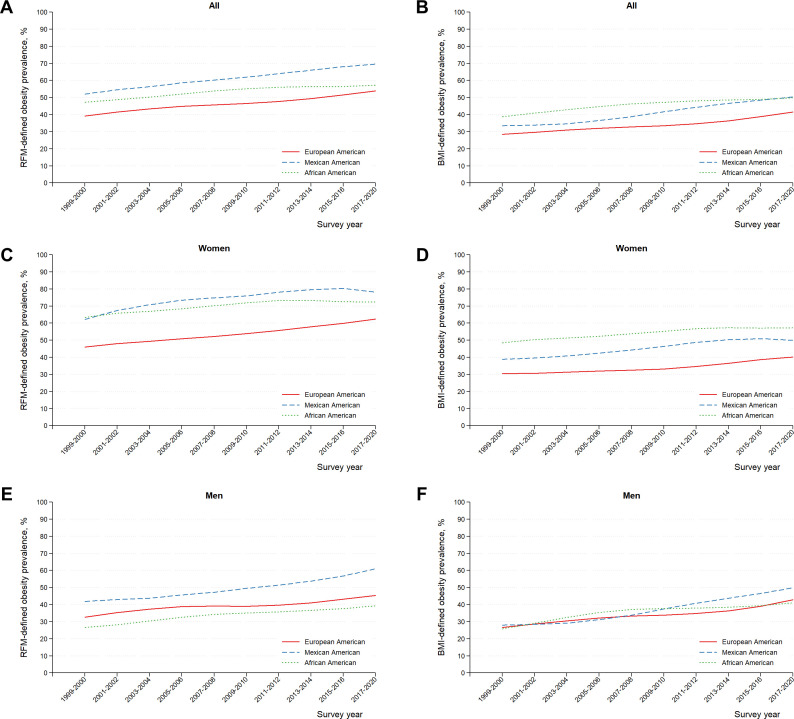
Obesity prevalence and temporal trends by ethnicity
The highest prevalence of RFM-defined obesity across years was observed among Mexican Americans. In contrast, the highest prevalence of BMI-defined obesity was observed among African American women but not men (figure 2). In 2017–March 2020, the prevalence of RFM-defined obesity was significantly higher in Mexican Americans compared with African Americans (Bonferroni corrected p<0.001) or European Americans (p<0.001). BMI-defined obesity prevalence was similar in Mexican and African Americans (p=0.99) and both groups had a higher prevalence than European Americans (p=0.003 and p=0.001, respectively).
Figure 2.
Age-adjusted US adult prevalence temporal trends in RFM-defined obesity by ethnicity: 1999–2000 to 2017–March 2020. Trend lines were smoothed using the LOWESS method on weighted prevalence estimates. The RFM was calculated as follows: RFM=64−(20×height/waist circumference)+(12×sex); sex equals 0 for men and one for women. Obesity was diagnosed if RFM was 40% or higher for women and RFM was 30% or higher for men. LOWESS, locally weighted scatterplot smoothing; RFM, relative fat mass.
The largest increase in the prevalence of RFM-defined obesity from 1999–2000 to 2017–March 2020 occurred in Mexican American men, with a linear increase of 18.3 percentage points (95% CI 12.0% to 24.5%; p<0.001) (online supplemental table 3 and figure 2). The highest increase in the prevalence of BMI-defined obesity also occurred in Mexican American men, with a linear increase of 21.2 percentage points (95% CI 15.3% to 27.1%; p<0.001) (online supplemental table 3 and figure 2).
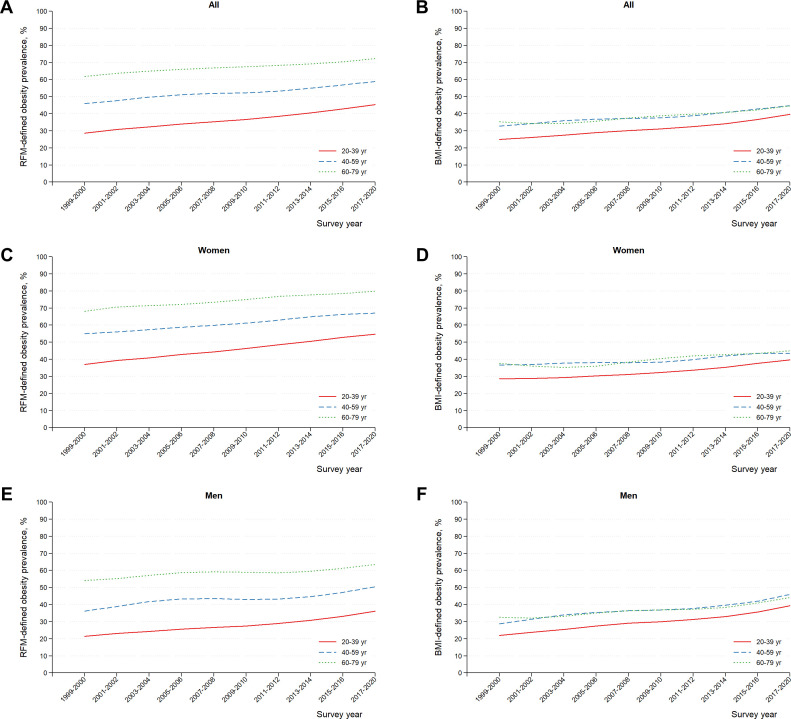
Obesity prevalence and temporal trends by age group
In women and men, the highest prevalence of RFM-defined obesity across years was observed in older adults (60–79 years) (figure 3 and online supplemental table 4).
Figure 3.
Age-adjusted US adult prevalence temporal trends in RFM-defined obesity by age group: 1999–2000 to 2017–March 2020. Trend lines were smoothed using the LOWESS method on weighted prevalence estimates. The RFM was calculated as follows: RFM=64−(20×height/waist circumference)+(12×sex); sex equals 0 for men and 1 for women. Obesity was diagnosed if RFM was 40% or higher for women and RFM was 30% or higher for men. LOWESS, locally weighted scatterplot smoothing; RFM, relative fat mass.
In contrast, no differences were observed in the prevalence of obesity between individuals 60–79 years and 40–59 years when using BMI for the diagnosis of obesity (figure 3). In 2017–March 2020, the prevalence of RFM-defined obesity was significantly higher in individuals 60–79 years compared with those 40–59 years (Bonferroni corrected p<0.001) or 20–39 years (p<0.001). We found no statistically significant differences in the prevalence of BMI-defined obesity across age groups (p>0.17 for all comparisons).
Although our analysis by age showed an increased prevalence of obesity in older women and men (figure 3), we performed a sensitivity analysis to specifically explore the possible role of menopause. Our findings from this post hoc analysis revealed that the crude prevalence of RFM-defined obesity in 2017–2020 was 56.4% (95% CI 53.5% to 59.3%) among premenopausal women (n=1935) and 76.4% (95% CI 71.0% to 81.8%) among postmenopausal women (n=1406). The mean age at last menstrual period was 49 years in this population. For comparison, among men, the corresponding prevalence of obesity was 39.7% (95% CI 34.9% to 44.6%) in those younger than 50 years (n=1790) and 56.2% (95% CI 52.9% to 59.5%) in men 50 years of age and older (n=1886).
Discussion
Our study shows that, compared with BMI, the use of a surrogate for whole-body fat percentage revealed a much higher prevalence of general obesity among adults in the USA, particularly among women, affecting nearly two-thirds of all women and nearly half of all men in 2017–2020, with an overall prevalence of 55.4%. This is an additional 22.5% of women and 3.8% of men 20–79 years being defined as having obesity compared with a BMI-based definition with the current criteria.
The use of RFM also revealed that the highest prevalence of general obesity over the study period from 1999 to 2020 occurred among Mexican Americans and not among African Americans, as was observed when BMI was used to diagnose obesity. Likewise, the use of RFM showed that the highest prevalence of general obesity over this study period occurred among older adults (60–79 years) and not among adults 40–59 years, as was observed when BMI was used. The higher prevalence of obesity in older individuals does not appear to be fully explained by a loss of skeletal muscle with age, since absolute fat mass also increases with age, although mainly visceral fat.40 41 However, it is difficult to draw a firm conclusion from cross-sectional data. Our findings are consistent with those from other studies also showing a higher body fat percentage in older individuals.12 23 40 42–45
Overall, women had a markedly higher prevalence of RFM-defined obesity across years than men, a difference that was less evident when using BMI. Previous studies have shown no differences in the prevalence of BMI-defined obesity between women and men.3 4 46 In this study, the difference in the prevalence of RFM-defined obesity for 2017–2020 between women and men was nearly 20 percentage points.
The highest prevalence of RFM-defined obesity was observed in Mexican Americans, and the increase was linear over the study period, although this linear increase was largely driven by a steady increase among men. Among Mexican American women, a decrease was observed since 2015. A previous study reported that, between 2003 and 2006, the prevalence of BMI-defined obesity was higher among African Americans compared with Mexican Americans, but between 2015 and 2018, Mexican American men had a higher prevalence than African American men.29 In contrast, RFM revealed a consistently higher prevalence of general obesity among Mexican Americans over the observed time, in both women and men. Socioeconomic characteristics are probably the main determinants of differences in the prevalence of general obesity between ethnic groups.47
It has been argued that the fat mass index (FMI, body fat mass adjusted for the square of the height, expressed in kg/m2) should be used as a reference of fat mass instead of body fat percentage (body fat mass adjusted for body weight) to avoid including fat mass both in the numerator and the denominator, as this is not mathematically advisable.48 However, the concept of obesity (excess body fat) and all different forms to express it, for example BMI,6 49 50 FMI,51 52 fat mass/fat-free-mass,53 54 body fat percentage,12 55 to cite a few, should not be seen only as mathematical constructs but also as biological variables with important implications as risk factors for disease and mortality. In this study, we chose body fat percentage as the reference because numerous studies have shown that body fat percentage is associated with mortality.13–20 56 What is also important to note is that FMI does not appear to be superior to body fat percentage or BMI as a predictor of cardiovascular mortality,14 all-cause mortality57 58 or cardiovascular risk factors.59 Because of its association with mortality, body fat percentage is of great clinical relevance. Recent studies support the utility of RFM to predict type 2 diabetes60 and heart failure.61
Further research is needed to better understand the clinical implications of our study findings: (1) the much higher prevalence of general obesity among women when RFM is used as opposed to BMI; (2) the higher burden of general obesity on Mexican Americans compared with African and European Americans and (3) the higher prevalence of general obesity in older individuals.
It is difficult to establish whether the higher prevalence of general obesity estimated using RFM would translate into a higher risk of cardiovascular disease (CVD). The association between obesity and CVD is very complex and several factors may mediate this association.62 Although subcutaneous fat appears to have a relative protective effect against CVD,63 others have shown that subcutaneous fat is also associated with cardiovascular risk factors, although less strongly than visceral fat.64 A major limitation of these studies, however, is that the analyses involved a small region of the abdominal trunk.
In women, who biologically have a higher body adiposity than men, the possible protective effect of estrogens on metabolism could be attenuated by the high prevalence of RFM-defined obesity. This could help explain, for example, the similar relative increase in the US prevalence of diabetes in women and men from 1999 to 2019 (by ~74%) (www.healthdata.org) or the similar prevalence of diabetes in women (14.1% (95% CI 11.8% to 16.7%)) and men (15.4% (95% CI 13.5% to 17.5%)) in 2017–2020.65 Our findings, although cross-sectional, do not appear to support a protective role of estrogens against obesity per se.
The temporal trends in RFM-defined and BMI-defined obesity in both women and men follow a parallel pattern. However, stratified analysis by ethnicity showed some differences. RFM revealed that Mexican Americans have a higher prevalence of obesity than European or African Americans. Although we cannot establish causality, this finding coincides with the higher absolute increase in the prevalence of diabetes and liver disease observed in Mexican Americans from 1999 to 2018 compared with European and African Americans.66
Whether the increased whole-body fat percentage in older individuals confers a higher risk on mortality also requires further investigation as age per se is a strong risk factor for mortality,67 and the relationship between obesity and mortality could be mediated by age.68 In addition, this can be confounded by concomitant severe disease. For instance, several studies have shown an inverse association between body fat percentage (but also BMI and FMI) and mortality in older patients.58 69 70 Conversely, the high body fat percentage in older individuals could explain the association of BMI-defined obesity with diabetes and CVD in older individuals.71–74 The increase in body adiposity with ageing coincides with the high prevalence of many cardiometabolic alterations occurring more often in older individuals, such as glucose intolerance, insulin resistance, dyslipidaemia and hypertension.68 BMI did not detect a higher prevalence of general obesity in individuals aged 60 years and older compared with younger adults, unlike when RFM was used. These findings further support that notion that BMI is a poor predictor of morbidity and mortality in older individuals.45 75
Abdominal obesity and general obesity are overall underestimated when using BMI (table 1 and online supplemental table 1). It is also important to mention that the prevalence of abdominal obesity is overall higher compared with the prevalence of RFM-defined obesity, except among Mexican Americans (online supplemental table 1). However, the closer proportions of abdominal obesity and RFM-defined general obesity is expected. Since RFM is based on waist circumference, and waist circumference is a surrogate for intra-abdominal fat,76 77 RFM could be a surrogate for both general obesity and abdominal obesity. Although RFM has been shown to predict trunk fat percentage, the prediction error is greater for trunk fat percentage than for whole-body fat percentage.23
It is plausible that the association of fat mass with mortality is, at least partly, reflecting the effect of fat-free mass on mortality. Although body fat percentage is associated with mortality, the implications of fat-free mass percentage, as opposed to body fat percentage, as a predictor of mortality require careful examination. Although the proportion of body FFM is the numeric complement of the proportion of body fat mass (%FM=100%−%FFM), this does not take into account the fact that FFM is not exclusively muscle mass. Unless muscle mass and fat mass are measured accurately, it will be difficult to distinguish the overall contribution of fat mass from the largest metabolically tissue in the body, the skeletal muscle, to predict mortality. The problem is that accurate estimates of skeletal muscle mass remain a challenge.78 The current evidence suggests that increased fat mass is associated with higher mortality whereas increased fat-free mass is associated with lower mortality.13 79 80
The opposite relationship of fat mass and fat-free mass with mortality could be altered due to weight loss interventions (which induce more fat mass loss than muscle mass loss) or because of loss of muscle mass due to age.81 In older individuals, increased fat-free mass has been associated with lower mortality, whereas lower fat mass has also been associated with increased risk of mortality,82 suggesting frailty could be a more important factor for mortality risk than body composition. Future studies should focus on comparing the association of fat mass and the metabolic components of fat-free mass with mortality. The muscle-mass centric view of health or disease,83 84 rather than focusing on BMI or body fat percentage, is interesting but requires further research due to the complex interrelationship between fat mass and fat-free mass (and muscle mass).
Our study has strengths. First, we used a previously validated surrogate for whole-body fat percentage in adults in the USA,23 which has a high diagnostic accuracy (91%) for DXA-defined obesity27 and has been shown to result in lower total misclassification of DXA-defined high body adiposity compared with BMI among women (RFM: 12.7%; BMI: 56.5%) and men (RFM: 9.4% BMI: 13.0%).23 Second, to define general obesity, we used previously validated RFM cut-offs to predict all-cause mortality in a large US adult population.27 Previously proposed cut-offs for fat-defined obesity have been based on arbitrary values85 86 or on corresponding BMI cut-offs.12 Third, we used measured anthropometrics. RFM requires only waist circumference and height for its calculation, which allowed us to estimate the prevalence of general obesity in a large adult population of the USA (n=44 754) with a wide age range, over a period of nearly 22 years. Fourth, NHANES has used a consistent methodology across survey cycles to measure anthropometrics, reducing the risk of measurement error that could affect our results.
Our study also has limitations. First, RFM was developed and validated using DXA as the reference method. However, DXA is an indirect method to assess body fatness and is susceptible to bias introduced mainly by age, degree of fatness and disease.87 88 Thus, there are limitations to the level of accuracy and precision that RFM can perform. Nevertheless, RFM is an attempt to provide a relatively easy and affordable alternative method to BMI to better assess body fatness. Second, although the overall obesity misclassification has been reported to be lower with RFM than with BMI in American (21) and Korean individuals (20), another limitation is that the proportion of obesity misclassification is not trivial when using RFM. Third, our analysis was performed using data from a representative sample of the non-institutionalised US population only. Fourth, our estimates of prevalence trends could have been affected by some variability in sampling across NHANES survey cycles.34 Finally, we did not analyse the prevalence trends for Asian Americans during the period studied because NHANES began oversampling Asian Americans only from 2011 to 2012 onwards and RFM cut-offs used to diagnose general obesity have not been validated among Asian populations.
From a public health perspective, we argue that due to the underdiagnosis of obesity when using BMI, the most affected populations are not receiving adequate medical care that they require. Aspects that will need further research are the implications of some possible overdiagnosis of obesity89 and the stigma that would be associated with it.90
In conclusion, the use of RFM, a surrogate for whole-body fat percentage, revealed a much higher prevalence of general obesity in the USA from 1999 to 2020, particularly among women, than that estimated by BMI. RFM, but not BMI, also revealed a disproportionate higher prevalence of general obesity in adults aged 60 years and older and Mexican Americans. Using BMI as the lone measure to define obesity may lead to significant misclassification of large obese subpopulations as non-obese, particularly among women. Our findings may have implications for the use of resources in public health to tackle obesity-related health problems in the most affected populations.
Supplementary Material
Acknowledgments
We thank the Centres for Disease Control and Prevention (CDC) and the National Centre for Health Statistics (NCHS) for providing access to the NHANES datasets. We also thank all subjects who participated in the surveys from 1999 to 2020.
Footnotes
Contributors: OOW was responsible for the conception and design of the study. OOW contributed to the statistical analysis. OOW and TS contributed to the interpretation of data and critical revision of the manuscript. OOW and TS drafted the final version of the manuscript and agreed to the submitted version of the manuscript. OOW is the manuscript’s guarantor. OOW accepts full responsibility for the work and the conduct of the study, had access to the data and controlled the decision to submit for publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: OOW is the lead author of the original article describing the development and validation of RFM. OOW currently works as an editor for The Lancet group.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. All data used are publicly and freely available from the NHANES website at https://wwwn.cdc.gov/nchs/nhanes/.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Since this study used publicly available de-identified data, approval from an Institutional Review Board was not required, as indicated in the Federal Policy for the Protection of Human Subjects (detailed in 45 CFR part 46), https://www.hhs.gov/ohrp/regulations-and-policy/regulations/common-rule/index.html
References
- 1.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999-2000. JAMA 2002;288:1723–7. 10.1001/jama.288.14.1723 [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States. JAMA 2016;315:2284. 10.1001/jama.2016.6458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief 2020;2020:1–8. [PubMed] [Google Scholar]
- 4.Stierman B, Afful J, Carroll MD, et al. National health and nutrition examination survey 2017–march 2020 prepandemic data files - development of files and prevalence estimates for selected health outcomes. Natl Health Stat Report 2021:1–20. [Google Scholar]
- 5.Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes (Lond) 2008;32 Suppl 3:S56–9. 10.1038/ijo.2008.87 [DOI] [PubMed] [Google Scholar]
- 6.WHO . Physical status: the use and interpretation of anthropometry. WHO technical report series. Geneva, 1995. [PubMed] [Google Scholar]
- 7.CDC . Defining adult overweight & obesity. Available: https://www.cdc.gov/obesity/basics/adult-defining.html [Accessed 18 Apr 2022].
- 8.Garn SM, Leonard WR, Hawthorne VM. Three limitations of the body mass index. Am J Clin Nutr 1986;44:996–7. 10.1093/ajcn/44.6.996 [DOI] [PubMed] [Google Scholar]
- 9.Gallagher D, Visser M, Sepúlveda D, et al. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups Am J Epidemiol 1996;143:228–39. 10.1093/oxfordjournals.aje.a008733 [DOI] [PubMed] [Google Scholar]
- 10.Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet 2006;368:666–78. 10.1016/S0140-6736(06)69251-9 [DOI] [PubMed] [Google Scholar]
- 11.Okorodudu DO, Jumean MF, Montori VM, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes (Lond) 2010;34:791–9. 10.1038/ijo.2010.5 [DOI] [PubMed] [Google Scholar]
- 12.Gallagher D, Heymsfield SB, Heo M, et al. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 2000;72:694–701. 10.1093/ajcn/72.3.694 [DOI] [PubMed] [Google Scholar]
- 13.Heitmann BL, Erikson H, Ellsinger BM, et al. Mortality associated with body fat, fat-free mass and body mass index among 60-year-old Swedish men-a 22-year follow-up. The study of men born in 1913. Int J Obes Relat Metab Disord 2000;24:33–7. 10.1038/sj.ijo.0801082 [DOI] [PubMed] [Google Scholar]
- 14.Ortega FB, Sui X, Lavie CJ, et al. Body mass index, the most widely used but also widely criticized index: would a criterion standard measure of total body fat be a better predictor of cardiovascular disease mortality? Mayo Clin Proc 2016;91:443–55. 10.1016/j.mayocp.2016.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Padwal R, Majumdar SR, Leslie WD. Relationship among body fat percentage, body mass index, and all-cause mortality. Ann Intern Med 2016;165:604. 10.7326/L16-0334 [DOI] [PubMed] [Google Scholar]
- 16.Zong G, Zhang Z, Yang Q, et al. Total and regional adiposity measured by dual-energy X-ray absorptiometry and mortality in NHANES 1999-2006. Obesity (Silver Spring) 2016;24:2414–21. 10.1002/oby.21659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dong B, Peng Y, Wang Z, et al. Joint association between body fat and its distribution with all-cause mortality: a data linkage cohort study based on NHANES (1988-2011). PLoS One 2018;13:e0193368. 10.1371/journal.pone.0193368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lahmann PH, Lissner L, Gullberg B, et al. A prospective study of adiposity and all-cause mortality: the malmo diet and cancer study. Obes Res 2002;10:361–9. 10.1038/oby.2002.50 [DOI] [PubMed] [Google Scholar]
- 19.Jenkins DA, Bowden J, Robinson HA, et al. Adiposity-mortality relationships in type 2 diabetes, coronary heart disease, and cancer subgroups in the UK biobank, and their modification by smoking. Diabetes Care 2018;41:1878–86. 10.2337/dc17-2508 [DOI] [PubMed] [Google Scholar]
- 20.Jayedi A, Khan TA, Aune D, et al. Body fat and risk of all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Int J Obes (Lond) 2022;46:1573–81. 10.1038/s41366-022-01165-5 [DOI] [PubMed] [Google Scholar]
- 21.Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today 2015;50:117–28. 10.1097/NT.0000000000000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CDC . Body mass index: considerations for practitioners. Available: https://stacks.cdc.gov/view/cdc/25368 [Accessed 8 Dec 2021].
- 23.Woolcott OO, Bergman RN. Relative Fat Mass (RFM) as a new estimator of whole-body fat percentage ─ a cross-sectional study in American adult individuals. Sci Rep 2018;8:10980. 10.1038/s41598-018-29362-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paek JK, Kim J, Kim K, et al. Usefulness of relative fat mass in estimating body adiposity in Korean adult population. Endocr J 2019;66:723–9. 10.1507/endocrj.EJ19-0064 [DOI] [PubMed] [Google Scholar]
- 25.Guzmán-León AE, Velarde AG, Vidal-Salas M, et al. External validation of the relative fat mass (RFM) index in adults from north-west Mexico using different reference methods. PLoS One 2019;14:e0226767. 10.1371/journal.pone.0226767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corrêa CR, Formolo NPS, Dezanetti T, et al. Relative fat mass is a better tool to diagnose high adiposity when compared to body mass index in young male adults: a cross-section study. Clin Nutr ESPEN 2021;41:225–33. 10.1016/j.clnesp.2020.12.009 [DOI] [PubMed] [Google Scholar]
- 27.Woolcott OO, Bergman RN. Defining cutoffs to diagnose obesity using the relative fat mass (RFM): association with mortality in NHANES 1999-2014. Int J Obes (Lond) 2020;44:1301–10. 10.1038/s41366-019-0516-8 [DOI] [PubMed] [Google Scholar]
- 28.Liu B, Du Y, Wu Y, et al. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011-18: population based study. BMJ 2021;372:n365. 10.1136/bmj.n365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gupta RD, Chakraborty PA, Al Kibria GM. Racial/ethnic disparities in prevalence and trends of obesity, grade 3 obesity, and abdominal obesity among US adults, 2003-18. Obesity Medicine 2021;28:100372. 10.1016/j.obmed.2021.100372 [DOI] [Google Scholar]
- 30.CDC . NHANES 2017-march 2020 pre-pandemic data release notes. Available: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/releasenotes.aspx?Cycle=2017-2020 [Accessed 10 Oct 2022].
- 31.Day JC. Population projections of the United States by age, sex, race, and hispanic origin: 1995 to 2050. Washington, DC: U. S Bureau of the Census, Current Population Reports. Reports, P25-1130, U.S, 1996. [Google Scholar]
- 32.National Health and Nutrition Examination Survey (NHANES) . Anthropometry procedures manual. Available: http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf [Accessed 16 May 2016].
- 33.CDC . NHANES response rates and population totals. 2022. Available: https://wwwn.cdc.gov/nchs/nhanes/responserates.aspx [Accessed 19 Jul 2022].
- 34.Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: analytic guidelines, 1999-2010. Vital Health Stat 2 2013:1–24. [PubMed] [Google Scholar]
- 35.CDC . National health and nutrition examination survey. Module 1: datasets and documentation. Available: https://wwwn.cdc.gov/nchs/nhanes/tutorials/module1.aspx [Accessed 18 Jul 2022].
- 36.Appiah D, Nwabuo CC, Ebong IA, et al. Trends in age at natural menopause and reproductive life span among US women, 1959-2018. JAMA 2021;325:1328–30. 10.1001/jama.2021.0278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med 1989;8:551–61. 10.1002/sim.4780080504 [DOI] [PubMed] [Google Scholar]
- 38.Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. New York, NY: Springer, 2001. 10.1007/978-1-4757-3462-1 [DOI] [Google Scholar]
- 39.Cox NJ. Speaking STATA: smoothing in various directions. The Stata Journal 2005;5:574–93. 10.1177/1536867X0500500408 [DOI] [Google Scholar]
- 40.Novak LP. Aging, total body potassium, fat-free mass, and cell mass in males and females between ages 18 and 85 years. J Gerontol 1972;27:438–43. 10.1093/geronj/27.4.438 [DOI] [PubMed] [Google Scholar]
- 41.Song M-Y, Ruts E, Kim J, et al. Sarcopenia and increased adipose tissue infiltration of muscle in elderly African American women. Am J Clin Nutr 2004;79:874–80. 10.1093/ajcn/79.5.874 [DOI] [PubMed] [Google Scholar]
- 42.Deurenberg P, Weststrate JA, Seidell JC. Body mass index as a measure of body fatness: age- and sex-specific prediction formulas. Br J Nutr 1991;65:105–14. 10.1079/bjn19910073 [DOI] [PubMed] [Google Scholar]
- 43.Noppa H, Andersson M, Bengtsson C, et al. Body composition in middle-aged women with special reference to the correlation between body fat mass and anthropometric data. Am J Clin Nutr 1979;32:1388–95. 10.1093/ajcn/32.7.1388 [DOI] [PubMed] [Google Scholar]
- 44.Jensky-Squires NE, Dieli-Conwright CM, Rossuello A, et al. Validity and reliability of body composition analysers in children and adults. Br J Nutr 2008;100:859–65. 10.1017/S0007114508925460 [DOI] [PubMed] [Google Scholar]
- 45.Kuk JL, Saunders TJ, Davidson LE, et al. Age-related changes in total and regional fat distribution. Ageing Res Rev 2009;8:339–48. 10.1016/j.arr.2009.06.001 [DOI] [PubMed] [Google Scholar]
- 46.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–7. 10.1001/jama.2012.39 [DOI] [PubMed] [Google Scholar]
- 47.Lakerveld J, Mackenbach J. The upstream determinants of adult obesity. Obes Facts 2017;10:216–22. 10.1159/000471489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wells JCK. Toward body composition reference data for infants, children, and adolescents. Adv Nutr 2014;5:320S–9S. 10.3945/an.113.005371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation 2021;143:e984–1010. 10.1161/CIR.0000000000000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Quetelet LAJ, Knox R, Smibert T. A treatise on man and the development of his faculties. Cambridge: Cambridge University Press, 2013. 10.1017/CBO9781139864909 [DOI] [Google Scholar]
- 51.VanItallie TB, Yang MU, Heymsfield SB, et al. Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am J Clin Nutr 1990;52:953–9. 10.1093/ajcn/52.6.953 [DOI] [PubMed] [Google Scholar]
- 52.Kyle UG, Schutz Y, Dupertuis YM, et al. Body composition interpretation. Contributions of the fat-free mass index and the body fat mass index. Nutrition 2003;19:597–604. 10.1016/s0899-9007(03)00061-3 [DOI] [PubMed] [Google Scholar]
- 53.Goran MI, Allison DB, Poehlman ET. Issues relating to normalization of body fat content in men and women. Int J Obes Relat Metab Disord 1995;19:638–43. [PubMed] [Google Scholar]
- 54.Prado CMM, Wells JCK, Smith SR, et al. Sarcopenic obesity: a critical appraisal of the current evidence. Clinical Nutrition 2012;31:583–601. 10.1016/j.clnu.2012.06.010 [DOI] [PubMed] [Google Scholar]
- 55.Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord 1998;22:1164–71. 10.1038/sj.ijo.0800741 [DOI] [PubMed] [Google Scholar]
- 56.Parra-Soto S, Cowley ES, Rezende LFM, et al. Associations of six adiposity-related markers with incidence and mortality from 24 cancers-findings from the UK biobank prospective cohort study. BMC Med 2021;19:7. 10.1186/s12916-020-01848-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Auyeung TW, Lee JSW, Leung J, et al. Survival in older men may benefit from being slightly overweight and centrally obese--a 5-year follow-up study in 4,000 older adults using DXA. J Gerontol A Biol Sci Med Sci 2010;65:99–104. 10.1093/gerona/glp099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rolland Y, Gallini A, Cristini C, et al. Body-composition predictors of mortality in women aged >/= 75 Y: data from a large population-based cohort study with a 17-Y follow-up. Am J Clin Nutr 2014;100:1352–60. 10.3945/ajcn.114.086728 [DOI] [PubMed] [Google Scholar]
- 59.Jeong S-M, Lee DH, Rezende LFM, et al. Different correlation of body mass index with body fatness and obesity-related biomarker according to age, sex and race-ethnicity. Sci Rep 2023;13:3472. 10.1038/s41598-023-30527-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Suthahar N, Wang K, Zwartkruis VW, et al. Associations of relative fat mass, a new index of adiposity, with type-2 diabetes in the general population. Eur J Intern Med 2023;109:73–8. 10.1016/j.ejim.2022.12.024 [DOI] [PubMed] [Google Scholar]
- 61.Suthahar N, Meems LMG, Withaar C, et al. Relative fat mass, a new index of adiposity, is strongly associated with incident heart failure: data from PREVEND. Sci Rep 2022;12:147. 10.1038/s41598-021-02409-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tutor AW, Lavie CJ, Kachur S, et al. Updates on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis 2023;78:2–10. 10.1016/j.pcad.2022.11.013 [DOI] [PubMed] [Google Scholar]
- 63.Porter SA, Massaro JM, Hoffmann U, et al. Abdominal subcutaneous adipose tissue: a protective fat depot Diabetes Care 2009;32:1068–75. 10.2337/dc08-2280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fox CS, Massaro JM, Hoffmann U, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the framingham heart study. Circulation 2007;116:39–48. 10.1161/CIRCULATIONAHA.106.675355 [DOI] [PubMed] [Google Scholar]
- 65.CDC . National diabetes statistics report. Estimates of diabetes and its burden in the United States. Available: https://www.cdc.gov/diabetes/data/statistics-report/index.html [Accessed 2 Apr 2023].
- 66.Caraballo C, Herrin J, Mahajan S, et al. Temporal trends in racial and ethnic disparities in multimorbidity prevalence in the United States, 1999-2018. Am J Med 2022;135:1083–92. 10.1016/j.amjmed.2022.04.010 [DOI] [PubMed] [Google Scholar]
- 67.Tian YE, Cropley V, Maier AB, et al. Heterogeneous aging across multiple organ systems and prediction of chronic disease and mortality. Nat Med 2023;29:1221–31. 10.1038/s41591-023-02296-6 [DOI] [PubMed] [Google Scholar]
- 68.Schwartz RS. Obesity in the elderly: prevalence, consequences, and treatment. In: Bray GA, Bouchard C, eds. Handbook of obesity etiology and pathophysiology. Second edition ed. New York: Marcel Dekker, Inc, 2004: 135–48. [Google Scholar]
- 69.de Santana FM, Domiciano DS, Gonçalves MA, et al. Association of appendicular lean mass, and subcutaneous and visceral adipose tissue with mortality in older Brazilians: the Sao Paulo ageing & health study. J Bone Miner Res 2019;34:1264–74. 10.1002/jbmr.3710 [DOI] [PubMed] [Google Scholar]
- 70.Lee JSW, Auyeung TW, Kwok T, et al. Survival benefit of abdominal adiposity: a 6-year follow-up study with dual X-ray absorptiometry in 3,978 older adults. Age (Dordr) 2012;34:597–608. 10.1007/s11357-011-9272-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen Y, Zhang X-P, Yuan J, et al. Association of body mass index and age with incident diabetes in Chinese adults: a population-based cohort study. BMJ Open 2018;8:e021768. 10.1136/bmjopen-2018-021768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lind L, Sundström J, Ärnlöv J, et al. Impact of aging on the strength of cardiovascular risk factors: a longitudinal study over 40 years. J Am Heart Assoc 2018;7:e007061. 10.1161/JAHA.117.007061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Masaki KH, Curb JD, Chiu D, et al. Association of body mass index with blood pressure in elderly Japanese American men. The honolulu heart program. Hypertension 1997;29:673–7. 10.1161/01.hyp.29.2.673 [DOI] [PubMed] [Google Scholar]
- 74.Tromp J, Paniagua SMA, Lau ES, et al. Age dependent associations of risk factors with heart failure: pooled population based cohort study. BMJ 2021;372:n461. 10.1136/bmj.n461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chang S-H, Beason TS, Hunleth JM, et al. A systematic review of body fat distribution and mortality in older people. Maturitas 2012;72:175–91. 10.1016/j.maturitas.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Edston E. A correlation between the weight of visceral adipose tissue and selected anthropometric indices: an autopsy study. Clin Obes 2013;3:84–9. 10.1111/cob.12021 [DOI] [PubMed] [Google Scholar]
- 77.Conway JM, Chanetsa FF, Wang P. Intraabdominal adipose tissue and anthropometric surrogates in African American women with upper- and lower-body obesity. Am J Clin Nutr 1997;66:1345–51. 10.1093/ajcn/66.6.1345 [DOI] [PubMed] [Google Scholar]
- 78.Bosy-Westphal A, Müller MJ. Identification of skeletal muscle mass depletion across age and BMI groups in health and disease--there is need for a unified definition. Int J Obes (Lond) 2015;39:379–86. 10.1038/ijo.2014.161 [DOI] [PubMed] [Google Scholar]
- 79.Allison DB, Zhu SK, Plankey M, et al. Differential associations of body mass index and adiposity with all-cause mortality among men in the first and second national health and nutrition examination surveys (NHANES I and NHANES II) follow-up studies. Int J Obes Relat Metab Disord 2002;26:410–6. 10.1038/sj.ijo.0801925 [DOI] [PubMed] [Google Scholar]
- 80.Zhu S, Heo M, Plankey M, et al. Associations of body mass index and anthropometric indicators of fat mass and fat free mass with all-cause mortality among women in the first and second national health and nutrition examination surveys follow-up studies. Ann Epidemiol 2003;13:286–93. 10.1016/s1047-2797(02)00417-9 [DOI] [PubMed] [Google Scholar]
- 81.Heymsfield SB, Gonzalez MCC, Shen W, et al. Weight loss composition is one-fourth fat-free mass: a critical review and critique of this widely cited rule. Obes Rev 2014;15:310–21. 10.1111/obr.12143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Spahillari A, Mukamal KJ, DeFilippi C, et al. The Association of lean and fat mass with all-cause mortality in older adults: the cardiovascular health study. Nutr Metab Cardiovasc Dis 2016;26:1039–47. 10.1016/j.numecd.2016.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bosy-Westphal A, Müller MJ. Diagnosis of obesity based on body composition-associated health risks-time for a change in paradigm. Obes Rev 2021;22 Suppl 2:e13190. 10.1111/obr.13190 [DOI] [PubMed] [Google Scholar]
- 84.Flegal KM. Use and misuse of BMI categories. AMA J Ethics 2023;25:E550–558. 10.1001/amajethics.2023.550 [DOI] [PubMed] [Google Scholar]
- 85.Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am J Clin Nutr 1999;69:373–80. 10.1093/ajcn/69.3.373 [DOI] [PubMed] [Google Scholar]
- 86.Lobman TG, Houtkooper L, Going SB. Body fat measurement goes high-tech: not all are created equal. ACSM’s Health & Fitness Journal 1997;1:30–5. [Google Scholar]
- 87.Wells JCK, Fewtrell MS. Measuring body composition. Arch Dis Child 2006;91:612–7. 10.1136/adc.2005.085522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Clasey JL, Kanaley JA, Wideman L, et al. Validity of methods of body composition assessment in young and older men and women. J Appl Physiol (1985) 1999;86:1728–38. 10.1152/jappl.1999.86.5.1728 [DOI] [PubMed] [Google Scholar]
- 89.Brodersen J, Schwartz LM, Heneghan C, et al. Overdiagnosis: what it is and what it isn't. BMJ EBM 2018;23:1–3. 10.1136/ebmed-2017-110886 [DOI] [PubMed] [Google Scholar]
- 90.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health 2010;100:1019–28. 10.2105/AJPH.2009.159491 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-071295supp001.pdf (302.5KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. All data used are publicly and freely available from the NHANES website at https://wwwn.cdc.gov/nchs/nhanes/.