Key Clinical Message
A middle‐aged female veteran artistic gymnast sustained an avulsion injury of the latissimus dorsi and teres major. The case reveals possible pitfalls in the current classification system and illustrates how a nonoperative approach, in contrast to recommended guidelines, was adequate for an excellent clinical outcome.
Keywords: acute tendon tear, artistic gymnastics, classification system, latissimus dorsi, MRI, nonoperative treatment, teres major
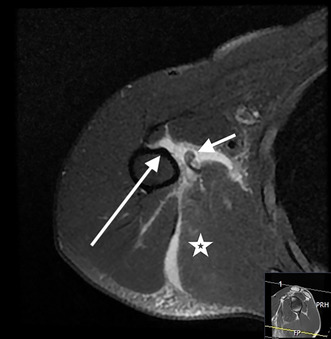
Magnetic resonance imaging (MRI) shows a total rupture of the latissimus dorsi with retraction, muscle edema, and a large hematoma between the tendon stump and the humerus.
1. INTRODUCTION
Acute shoulder injuries are common in female gymnasts, and uneven bars are the dominating mechanism of injury. 1 We present a case report of a conjoined tendon avulsion of both the latissimus dorsi (LD) and teres major (TM) muscles in a high‐performance, middle‐aged, veteran artistic gymnast. The challenges associated with these types of injuries are related to the complex anatomy, a potentially low degree of clinical suspicion because of unfamiliarity with the diagnosis among clinicians, and the fact that these injuries are not well visualized at standard shoulder imaging.
Due to the rarity of injury to the LD and/or the TM, the literature mainly consists of case reports and case series of high‐level athletes, initially reported in baseball pitchers, but also in several other sports. 2 However, reports of a combined tear to both the LD and the TM tendons are, to the best of our knowledge, restricted to baseball, golf, and water‐skiing. 3 , 4 , 5 , 6 The incidence of LD tear seems to be increasing. 1 Because baseball is a sport with variable popularity around the world, injury to the LD/TM may be unfamiliar for physicians and physiotherapists in health care systems outside the Americas and South Asia. Consequently, the diagnosis may be overlooked, even in high quality health care countries. A clear classification system would be helpful when orthopedic surgeons with limited knowledge of these injuries are consulted for treatment recommendations. 7
1.1. Case history
The patient is a 45‐year‐old female gymnast, active and participating in national and international competitions for veterans. As a child and youth, she was actively competing on national level, outside the national team. Around her 30, the gymnastics were resumed for 4 years before paused due to pregnancies, and again resumed at the age of 40, but on a veteran level with approximately 5 h weekly training. She is a medical doctor, healthy with no relevant prior injuries, nonsmoker, and does not use medication. Before the injury, she exercised two or three times a week with gymnastics and sometimes with running or cross‐country skiing. Two years prior to the injury, she had chronic right shoulder pain radiating along the proximal dorsal part of the right upper arm which worsened after training sessions. However, on clinical examination, there was full passive and active range of motion, and strength testing was normal including adduction, internal rotation, and extension.
The patient was injured in September 2020 while doing subsequent glide kips in the uneven bars. She experienced a snap in the right shoulder area after the third repetition of sudden pull of the shoulder when hanging by her arms. She initially felt no pain but had a sense that something was missing in the dorsal musculature and the feeling of reduced function and swelling (Figure 1). She did not cool down the area with ice, nor did she need analgesics. On physical examination, an asymmetry could be seen as the axillary fold on the affected right side was swollen, tender, and painful on palpation. Clinical testing was difficult to perform in the sub‐acute setting because of pain evolving in the area but reduced strength when trying to adduct and extend the shoulder was noted. She was referred to MRI with the question of a possible tear of a tendon in the right shoulder area. The referrer suggested a tear of the triceps, TM, or subscapularis muscles.
FIGURE 1.

Day of injury. The arrow indicates the area of swelling, tenderness, and pain.
Imaging was performed as described below, but no specific therapy, like guided physiotherapy, was performed, and no surgical attempts were made.
After the injury, the patient continued to exercise twice a week but avoided sudden movements, the uneven bars, climbing the ropes, and pull‐ups.
After 2 weeks, an apparent abnormal contour of the right posterior axillary fold was visible (Figure 2A). However, she could do push‐ups and “cross handstand – roll forward” on the balance beam. When hanging by her arms, she was hanging obliquely “like a banana” with her legs deviating to the left in the coronal plane, probably due to compensation for reduced strength on her injured right side (Figure 3A).
FIGURE 2.

Two weeks post‐injury. Arrow indicates abnormal contour of the posterior axillary fold on the right side caused by retraction of the teres major and latissimus dorsi muscles from the humeral insertion.
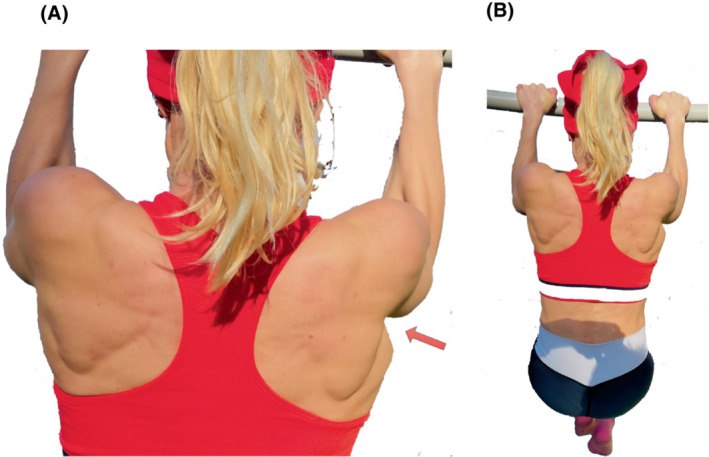
FIGURE 3.

(A) Three weeks post‐injury. The image shows the patient hanging from the upper bar of the uneven bars device where she inferred her injury 3 weeks previously. Note the involuntary compensatory deviation of the legs toward the left, uninjured side—like a “banana.” (B) Three weeks post‐injury performing handstand on the balance beam.
She continued exercising mainly by doing cross‐country skiing 3 h a week and some basic strength exercises at home. She experienced reduced strength in the right upper arm when poling during the diagonal stride in cross‐country skiing (i.e., extending the right shoulder against resistance). The pain subsided a few weeks after the injury, but she experienced a stretching sensation in the area, for instance, when doing pull‐ups.
After 3 weeks, she could do a handspring entry onto the vault board and handstand on the balance beam (Figure 3B).
After 3 months, she was able to walk on her hands, as she could before the injury.
After 6 months of nonoperative treatment with continuous but self‐guided tailored exercises, she had no pain, nor did she experience any asymmetric strength, and she could climb the ropes all the way to the ceiling (>10 m above the floor) (Figure 4). The shoulder range of motion was completely normal and pain‐free. However, the stretching sensations in the injured area persisted, and a contour change was visible when doing pull‐ups, but otherwise, no noticeable sequelae (Figure 5A,B).
FIGURE 4.

Six months post‐injury the patient demonstrates “climbing the ropes.” Arrow indicates injured right side.
FIGURE 5.
(A) Six months post‐injury. The patient reports to have regained her pre‐injury strength and performs the same number of pull‐ups as before the injury. The arrow indicates the abnormal contour of the posterior axillary fold. (B) Shows negligible cosmetic sequela 6 months post‐injury.
1.2. Imaging
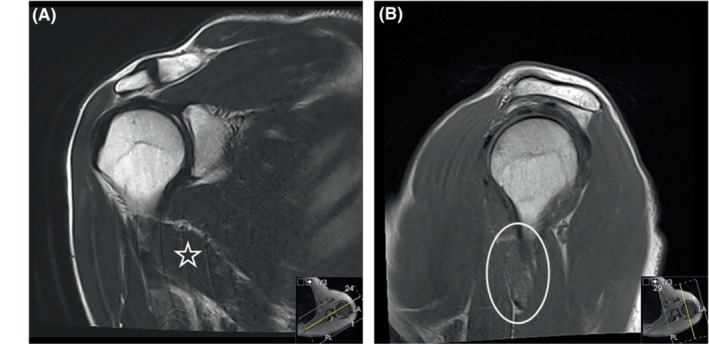
The patient's right shoulder was scanned with magnetic resonance imaging (MRI) 10 months prior to the injury because of chronic shoulder pain lasting for 2 years. At that point, the range of motion was normal. The MRI study showed intact rotator cuff, but degenerative cystic changes and bone marrow edema at the supraspinatus insertion were believed to result of chronic tractional forces. In addition, there were edematous changes at the posteroinferior part of the glenoid joint and the inferior glenohumeral ligament, probably due to a soft‐tissue injury to the capsule. The protocol covered the right proximal LD and the TM in the coronal and sagittal planes, but there were no pathological changes in that area.
The patient was scanned again 10 months later, 1 week post‐injury. The MRI was performed as a standard shoulder protocol with a proton density fat‐saturated sequence (PD fat sat) in all three planes, coronal T2 and sagittal T1. However, the technician added 10 more axial slices because of soft‐tissue edema seen below the shoulder joint, covering 12 cm in the craniocaudal direction (standard coverage in the current shoulder MRI protocol is 9 cm) (Figure 6A,B).
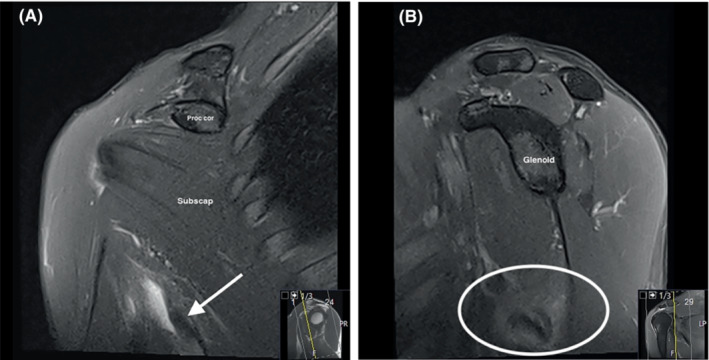
FIGURE 6.
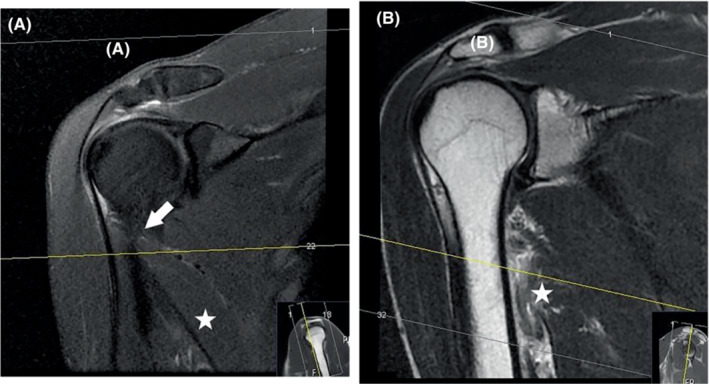
Coronal proton density fatsat in a study (A) performed before the injury, showing a common placement of transverse slices in a regular shoulder MRI exam. The latissimus dorsi (star) and its proximal insertion (arrow) are not covered sufficiently by the axial slices (lines 1–22). Coronal T2 1 week post‐injury (B) was performed by an experienced radiographer who extended the imaging of axial slices to cover the injured area along the humerus.
The scanner used for these two first MRI scans was an older model (1.5T GE Optima MR 360).
Despite some movement artifacts, the MRI showed extensive hematoma and edema in the soft‐tissues medial and anterior to the right proximal humerus, below the level of the subscapularis muscle and the axillary neurovascular bundle. The hematoma continued dorsally between the muscle belly of the proximal triceps laterally and the LD medially. The hematoma along the humerus measured 5 × 3 × 1.5 cm, and in this area a completely ruptured and avulsed tendon of the LD was identified, retracted 1.5–2.5 cm from its original attachment. The TM, normally having a shorter tendinous attachment than the LD, was partially torn at its insertion at the proximal humerus. There was extensive edema in the bellies of both muscles near the musculotendinous junction, particularly in the LD, which had extensive muscle fiber defects and intramuscular hematoma (Figure 7A–D).
FIGURE 7.
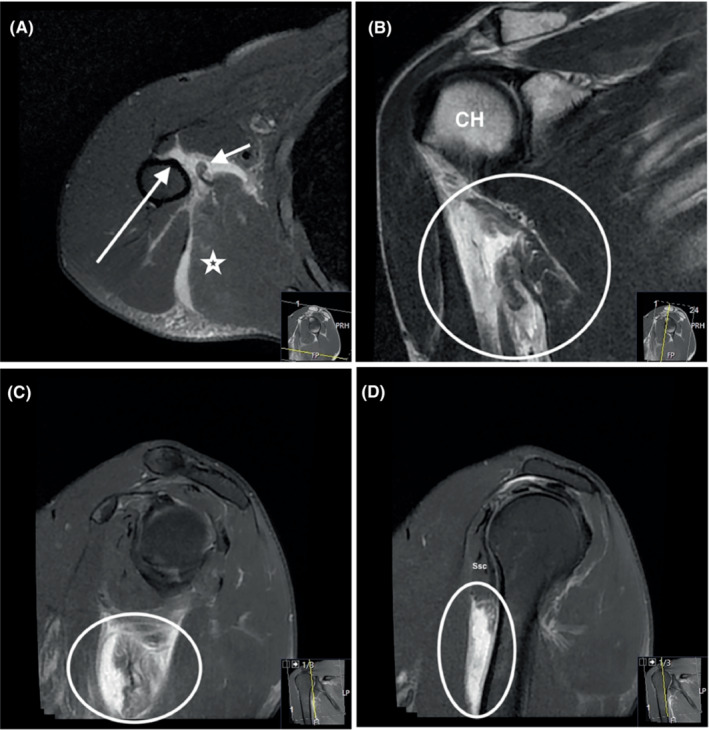
Axial proton density (PD) fatsat (A), coronal T2 (B), sagittal PD fatsat in a medial position (C) and a more lateral position along the humerus (D) show a total rupture of the latissimus dorsi with retraction, muscle edema, and a large hematoma between the tendon stump and the humerus. It is difficult to identify the teres major tendon, and a total rupture of this tendon cannot be verified.
The right shoulder was imaged again on three additional occasions with a 1.5T Siemens Aera MRI scanner:
Seven weeks post‐injury, the hematoma was largely resorbed, but a small amount of fluid along the now 4 cm retracted tendon of the LD remained. The attachment of the muscles to the humerus was not possible to identify, apart from probably a small remaining TM component. (Figure 8A,B)
Eleven weeks post‐injury, some edema along the course of the TM and LD was seen, but no hematoma. The ruptured end of the LD was, in both this and the previous scan, somewhat thickened and maybe scarred, and there was slight edema in the myotendinous junction (Figure 9A–C). In contrast to the initial post‐traumatic MRI, a subdeltoid bursitis and a partial rupture of the infraspinatus tendon attachment were visible.
Thirty‐eight weeks post‐injury, the hematoma and edema were completely resorbed. Some scar tissue had formed at the musculotendinous junction. Even though parts of the muscle could now be seen connecting to the humerus, the tendon and the distal muscle fibers were thin and slender compared to the left side and the imaging before the injury (Figures 10A–D and 11A,B [left side]).
FIGURE 8.
Seven weeks post‐injury. The hematoma is largely absorbed, but a small amount of fluid along the retracted tendon is seen. (A) Coronal proton density (PD) fatsat. Arrow points to the retracted tendon, and lateral to the tendon a small amount of fluid/hematoma is seen. Coracoid process (proc cor); subscapularis muscle belly (subscap). (B): Sagittal PD fatsat. The circle captures the retracted tendon with surrounding soft‐tissue edema.
FIGURE 9.
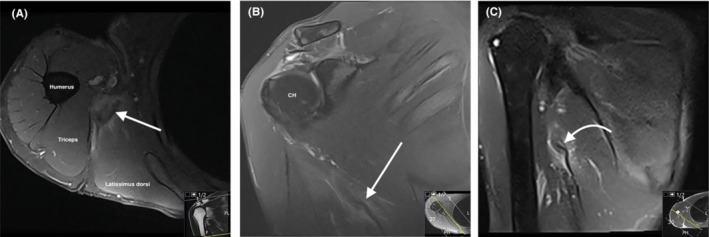
Eleven weeks post‐injury. (A) Axial proton density (PD) fatsat shows the still thickened proximal end of the latissimus dorsi and slight surrounding edema (arrow). (B) Coronal PD fatsat also shows the proximal tendon of the latissimus dorsi, retracted and with some surrounding edema (arrow). (C) Coronal STIR with extended field of view shows the proximal end of the latissimus dorsi.
FIGURE 10.
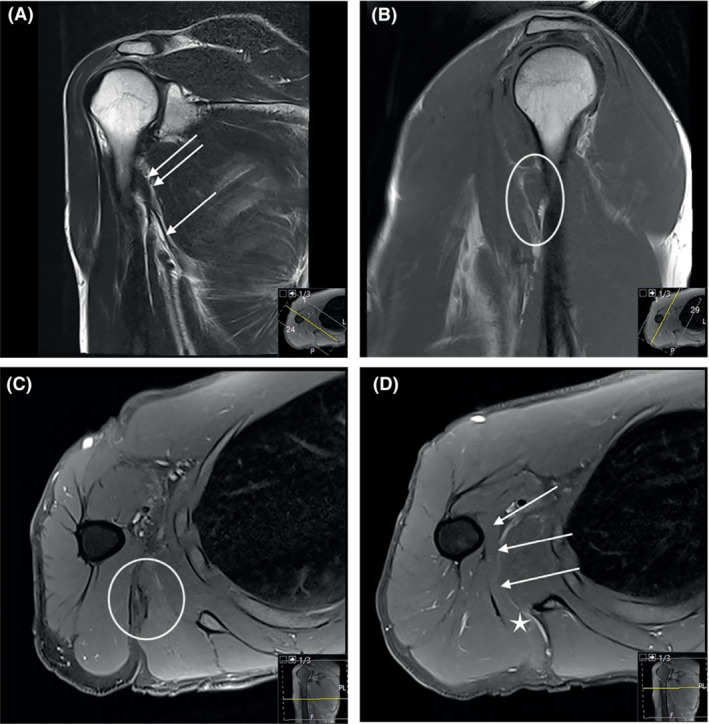
Thirty‐eight weeks post‐injury. The hematoma and edema are completely absorbed. The muscle seems to have reattached to the humerus, and there is some residual scar tissue at the musculotendinous junction. (A) Coronal T2. The tendon can be seen as a slender structure all the way to its former insertion (arrows). (B) Sagittal T1. Part of the muscle is close to its humeral insertion indicated by the circle. Compare with previous Figure 7D. (C) Axial proton density (PD) fatsat. Scar tissue at the musculotendinous junction indicated by the circle. (D) Axial PD fatsat. The latissimus dorsi indicated by the star is reconnected to the humerus by reattachment of muscle tissue as indicated by the arrows.
FIGURE 11.
Normal left side. (A) Coronal T2. Compare latissimus dorsi indicated by the star, with Figure 10A. (B) Sagittal T1. Compare latissimus dorsi indicated by the circle, with Figure 10B.
2. DISCUSSION
The LD and TM muscles act as one muscle unit in a wide variety of movements. The large LD muscle originates from the iliac crest's posterior third, the sacrum, all lumbar vertebrae, the spinous processes of vertebrae T7‐T12, and sometimes from the 9th to the 12th rib and the inferior angle of the scapula. It is oriented in a craniocaudal direction, dorso‐laterally along the torso. The TM muscle originates from the scapular inferior angle. It follows the LD laterally, and both muscles merge together to form a conjoined tendon and insert into the bicipital groove at the proximal humerus (Figure 12A–C). The LD/TM muscle unit adducts, extends, and rotates the humerus internally when the shoulder is abducted. An intact LD muscle is mandatory for shoulder stability and plays a crucial role in stabilizing the lower back and the sacroiliac joint together with the contralateral gluteus maximus muscle during bodily motions like walking and running. 8 , 9 Together with the pectoralis major, the LD and TM are the main adductors of the shoulder. 10 A sudden contraction, against resistance, from a hyper‐abducted position of the shoulder with the arm externally rotated and/or hyperextended can cause injury to the LD/TM muscle bellies, avulsion from their origins, or avulsion of the conjoined tendon insertion from the proximal humerus.
FIGURE 12.
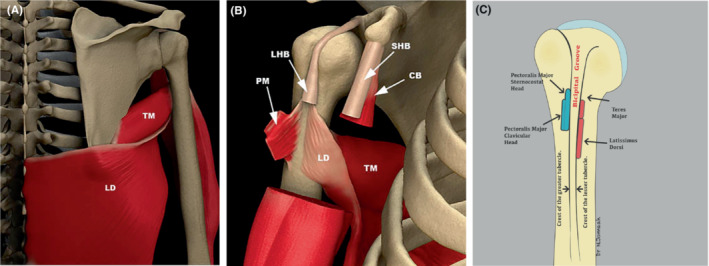
Schematic drawings of the shoulder region in a posterior (A) and anterior (B) view show the latissimus dorsi (LD) muscle curving along the thoracic wall and inserting on to the humerus together with the teres major (TM). Partially resected views of the following structures: pectoralis major (PM); long head of the biceps (LHB); short head of the biceps (SHB); coracobrachialis (CB). Images by Michael Stadnick, courtesy of Radsource (www.radsource.us). (C) Schematic drawing of the tendon attachments on the proximal humerus. Courtesy of Dr Nabil Jomaah.
Injury to the LD muscle is rare in nonbaseball‐athletes and most often occurs after an acute traumatic event, typically as an avulsion of the tendon rather than injury to the myotendinous junction. 11
Standard imaging studies of the shoulder may not visualize injuries to the LD, as its attachment could be in the periphery of the chosen field of view. The referral should clearly state clinical suspicion of LD injury to ensure that the correct area is covered. In our case, there were both clinical suspicion and an alert radiographer who added extra slices to the axial series to cover an area of suspected soft‐tissue edema. The oblique course of the LD along the thoracic cage makes it often difficult, even with adequate MRI imaging, to visualize a traumatized muscle and tendon. 12
In the subsequent follow‐up imaging examinations, we attempted to cover more of the muscle belly, but at the price of somewhat reduced image quality.
In the literature, treatment recommendations for LD/TM injuries are predominantly based on younger male baseball pitchers treated nonoperatively or surgically.
Erickson et al. reported a return to sport rate of 75% among 120 baseball pitchers from 2006 to 2011 with a LD/TM regardless of treatment (nonoperative or surgical treatment). 13 Interestingly, they found a shorter recovery time to the same competition level in the nonoperatively treated pitchers compared to those who underwent surgery, which can be explained by a more extensive injury in those receiving surgical treatment. A grading system based on MRI is proposed by Erickson et al. 7 :
Grade I: Fluid tracking along LD/TM.
Grade II: Partial‐thickness tear.
- Grade III: Full‐thickness tear, < 2 cm of retraction.
- A: Muscle is torn off the humerus.
- B: Tear is at the musculotendinous junction.
- Grade IV: Full‐thickness tear, > 2 cm of retraction.
- A: Muscle is torn off the humerus.
- B: Tear is at the musculotendinous junction.
Nonoperative management of Grade I and II injuries and surgical repair in avulsion injuries in Grade III and IV tears were recommended. In the present case report, the injury was an avulsion of both LD and the TM, and the retraction of the LD tendon was >2 cm. According to the suggested treatment algorithm by Erickson et al. our patient's injury may be classified as Grade IV‐A which implies recommendation for surgical intervention. However, the patient's choice of nonoperative management with self‐administered early accelerated functional rehabilitation guided by the gradual reveal of symptoms and limitations led to a full functional recovery with only a negligible cosmetic sequel. The MRI findings of reduced thickness of the muscle fibers on the right side compared to the uninjured left side 38 weeks post‐injury and the fact that other glenohumeral extensors, adductors, and internal rotators (such as the deltoid, subscapularis, and pectoralis major muscles) were uninjured, suggest that the potential injury‐related reduction in strength of the TM and LD muscles has been compensated by biomechanical adjustments of motion pattern and/or increased contribution from accessory muscles around the shoulder.
The classification system by Erickson et al. does not distinguish between isolated tears to either the LD or the TM, and the conjoined tendon as a whole. The current case demonstrates the need for a clarification of the MRI classification system. A full‐thickness tear of the LD with a retraction of more than 2 cm may be classified as a severe (Grade IV) injury which should be treated surgically according to recommended guidelines. 7 The successful nonoperative treatment of the patient in the current case may be explained by the fact that a small string of the TM tendon remained in contact with its bony attachment on the humerus despite the tear of the rest of the TM and the whole LD with large retractions of more than 2 cm. Importantly, there were no other injuries to the other shoulder muscles allowing for accessory muscle adaptation.
We propose that tears to the LD and TM tendons are graded as one conjoined tendon tear and that a complete rupture of both the LD and the TM must be present to classify the injury as a Grade III or IV according to Erickson et al. As exemplified by the injury in our female middle‐aged gymnast, this additional specification would have led to nonoperative treatment recommendations similar to the Grade II injuries.
In the shared decision‐making process of whether undergo surgery in a subtotal avulsion of the TM/LD conjoined tendon, accompanying accessory muscle injury and function, patient age, comorbidities and activity level, expectations and type of sport should also be taken into consideration in addition to the classification system by Erickson et al.
3. CONCLUSION
Injuries to the LD and TM are increasingly reported in baseball pitchers. However, in most countries, baseball is an uncommon sport, and the diagnosis may be challenging because of unfamiliarity with the injury among patients and health care providers. Because regular shoulder MRI examination does not cover the insertion of the conjoined tendon of TM and LD at its insertion on the humerus the diagnosis can be missed. Our case illustrates that classification of these injuries should be clarified to avoid unnecessary surgical treatment recommendations. Several centimeters of retraction of the LD part of the conjoined tendon combined with a subtotal avulsion of the TM part with no other muscle injuries as in the present case report may be successively treated nonoperatively with excellent functional results and return to the same level of gymnastic performance in less than 6 months post‐injury.
AUTHOR CONTRIBUTIONS
Roar Pedersen: Resources; software; writing – original draft; writing – review and editing. Kerstin Anine Johnsen Myhrvold: Software; writing – original draft; writing – review and editing. Ståle Bergman Myhrvold: Supervision; writing – original draft; writing – review and editing.
FUNDING INFORMATION
The authors did not receive any funding in the production of this article.
ETHICS STATEMENT
This manuscript was completed in accordance with the ethical standards of the institutional research committee, and the patient signed consent for publication.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Pedersen R, Johnsen Myhrvold KA, Myhrvold SB. Nonoperative treatment of a conjoined tendon avulsion tear of latissimus dorsi and teres major in a high performing, middle‐aged, artistic gymnast: Diagnostic and classificational challenges, and clinical result. Clin Case Rep. 2023;11:e7790. doi: 10.1002/ccr3.7790
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- 1. Hinds N, Angioi M, Birn‐Jeffery A, Twycross‐Lewis R. A systematic review of shoulder injury prevalence, proportion, rate, type, onset, severity, mechanism and risk factors in female artistic gymnasts. Phys Ther Sport. 2019;35:106‐115. [DOI] [PubMed] [Google Scholar]
- 2. Pardiwala DN, Subbiah K, Rao N, Modi R. Latissimus dorsi tear in an Olympics‐level tennis player: case report and review of literature. Indian J Orthop. 2020;54(3):332‐338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schickendantz MS, Kaar SG, Meister K, Lund P, Beverley L. Latissimus dorsi and Teres major tears in professional baseball pitchers: a case series. Am J Sports Med. 2009;37(10):2016‐2020. [DOI] [PubMed] [Google Scholar]
- 4. Nagda SH, Cohen SB, Noonan TJ, Raasch WG, Ciccotti MG, Yocum LA. Management and outcomes of latissimus dorsi and teres major injuries in professional baseball pitchers. Am J Sports Med. 2011;39(10):2181‐2186. [DOI] [PubMed] [Google Scholar]
- 5. Spinner RJ, Speer KP, Mallon WJ. Avulsion injury to the conjoined tendons of the latissimus dorsi and teres major muscles. Am J Sports Med. 1998;26(6):847‐849. [DOI] [PubMed] [Google Scholar]
- 6. Ahmad AN, Hankins DA, Wascher DC. Simultaneous bilateral latissimus dorsi tendon ruptures: a case report. JBJS Case Connect. 2021;11(4). [DOI] [PubMed] [Google Scholar]
- 7. Erickson BJ, Chalmers PN, Potter HG, Altchek DW, Romeo AA. Magnetic resonance imaging grading system for tears of the latissimus dorsi and Teres major. Orthop J Sports Med. 2019;7(3):2325967119826548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Feeney DF, Capobianco RA, Montgomery JR, Morreale J, Grabowski AM, Enoka RM. Individuals with sacroiliac joint dysfunction display asymmetrical gait and a depressed synergy between muscles providing sacroiliac joint force closure when walking. J Electromyogr Kinesiol. 2018;43:95‐103. [DOI] [PubMed] [Google Scholar]
- 9. Hawkes DH, Khaiyat OA, Howard AJ, Kemp GJ, Frostick SP. Patterns of muscle coordination during dynamic glenohumeral joint elevation: an EMG study. PloS One. 2019;14(2):e0211800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marchetti PH, Uchida MC. Effects of the pullover exercise on the pectoralis major and latissimus dorsi muscles as evaluated by EMG. J Appl Biomech. 2011;27(4):380‐384. [DOI] [PubMed] [Google Scholar]
- 11. Friedman MV, Stensby JD, Hillen TJ, Demertzis JL, Keener JD. Traumatic tear of the latissimus dorsi myotendinous junction: case report of a CrossFit‐related injury. Sports Health. 2015;7(6):548‐552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burdett PH. Acute musculotendinous tears of the latissimus dorsi and teres major. 2011. Accessed June 29, 2023. https://radsource.us/acute‐musculotendinous‐tears/
- 13. Erickson BJ, Chalmers PN, D'Angelo J, Ma K, Romeo AA. Performance and return to sport after latissimus dorsi and Teres major tears among professional baseball pitchers. Am J Sports Med. 2019;47(5):1090‐1095. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


