Abstract
Shoulder stiffness is a frequent complication after proximal humeral fractures treated with or without surgery. Shoulder stiffness is associated with high rates of absence from work and a significant financial burden for the healthcare system.
Secondary stiffness is characterized by additional extracapsular adhesions, including subacromial, subcoracoid, and subdeltoid spaces, usually derived from post-fracture or post-surgical extraarticular hematomas.
Several secondary causes may coexist with capsular and extracapsular adhesions decreasing the shoulder motion, such as malunion, nonunion, metalwork failure, infection, and osteoarthritis, among others.
Conservative treatment, usually prescribed for primary shoulder stiffness, has shown unfavorable results in secondary stiffness, and surgical intervention may be required.
Surgical interventions need to be patient-specific. Usually, open or arthroscopic fibro-arthrolysis and subacromial release are performed, together with plate removal and biceps tenotomy/tenodesis. In severe osteoarthritis, shoulder replacement may be indicated. Ruling out infection is recommended in every case.
Keywords: shoulder stiffness, arthrofibrosis, proxima humeral fracture, PROMs
Introduction
Proximal humerus fractures (PHFs) have an estimated annual incidence of 25 per 10 000 people in the United States (1). Treatment of these fractures varies depending on patient-related factors and fracture characteristics. For patients <65 years old with 2-, 3-, or 4-part fractures, glenohumeral fracture-dislocations, and displaced intra-articular fractures, treatment may involve open reduction and fixation (ORIF) (2). For patients >65 years old, due to high rates of failure with open reduction and internal fixation, generally either conservative treatment or arthroplasty is preferred.
Stiffness after PHF develops in a significant proportion of patients, even in undisplaced fractures managed conservatively (3). PHFs with secondary stiffness are associated with higher rates of employment absence and higher costs for the healthcare system (4). Before the definite diagnosis of post-traumatic stiffness is made, all other possible causes of functional restriction should be ruled out. These include dislocation, avascular necrosis, osteoarthritis, and metalwork failure. At 6 months, up to 23.6% of patients with complex PHF treated with ORIF will develop secondary shoulder stiffness (5). Of those patients, 75% required revision surgery. Operative treatment for stiffness included isolated or combined procedures such as arthrolysis, subacromial decompression, or osteosynthesis removal (5).
Definition
Stiffness in the shoulder can manifest itself in a variety of conditions. There is no consensus definition for post-traumatic shoulder stiffness (6). Main differences arise between primary idiopathic shoulder stiffness or so-called ‘frozen shoulder’ and various causes of secondary stiffness. Frozen shoulder, or primary idiopathic stiff shoulder, is defined as a global stiffness without any specific identifiable cause (7). Frozen shoulder has a specific pathophysiology and is generally considered to have a self-limiting natural history. The term secondary shoulder stiffness describes the limitation of glenohumeral joint range of motion due to a known cause. This can be further subdivided by category. Stiffness secondary to PHF, managed operatively or conservatively, is usually termed post-traumatic stiffness (7). In post-traumatic stiffness, it is important to differentiate those arising from post-surgical management with those as a result of conservative management. Before determining the cause of stiffness, other causes of functional restriction to the range of motion should be considered. These include dislocation, avascular necrosis, osteoarthritis, and metalwork failure (8).
Pathophysiology
There is a paucity of evidence regarding the pathophysiology of post-traumatic stiffness and the exact mechanism remains unclear. Secondary stiffness, however, does not only involve the glenohumeral joint but is characterized by extracapsular adhesion involving the subacromial, subcoracoid, and subdeltoid space, resulting in a mechanically limited range of motion. This affects mainly abduction and internal rotation/adduction. This might be triggered by an extraarticular hematoma secondary to the fracture or post-surgery (9). Adhesions can be from surfaces that are intended to slide with reference to one another. These are different from other causes of stiffness, which may co-exist. A predisposition to inflammation, pain, prolonged immobilization, and other factors may additionally result in a chronic capsular fibrotic reaction (3). Soft tissue contractures may occur in various tissues including capsular synovial lining, and musculotendinous units. Fibrosis of areolar-fatty packing tissue between muscles, tendons, and nerves may also occur leading to stiffness. Finally, an increased coefficient of friction between two intended articular surfaces secondary to chondrosis and cartilage degradation may further limit the range of motion. Alongside the capsular contracture and extracapsular adhesions, several other secondary causes may coexist. Before determining definitively the source of stiffness all other causes must be ruled out such as dislocation, avascular necrosis, and metalwork failure.
Stiffness due to malunion
Fracture displacement or malreduction can lead to an impingement of the lesser tuberosity (10), limiting internal rotation. Impingement of the greater tuberosity (11) limiting abduction, forward elevation, and possibly external rotation may also occur. Malreduction of the articular humeral head fragment may lead to mechanical limitation or the development of post-traumatic osteoarthritis. Malunion may occur as a result of non-operative management or following open reduction internal rotation. Post-surgical stiffness should therefore be carefully evaluated for malunion using a computed tomography (CT) scan. In cases with metalwork in situ, there is a need to determine whether malunion is primarily the cause vs implant malposition, screw penetration, and secondary collapse due to hardware failure.
Stiffness due to articular degradation
Articular damage can manifest itself as a focal osteochondral lesion or as generalized post-traumatic osteoarthritis. Osteonecrosis, or avascular necrosis, can result from disruption of the blood supply of the humeral head. This may be due to the fracture pattern or as a result of surgical management. Osteonecrosis is more frequent in 3- and 4-part displaced fractures with medial hinge compromise. Osteonecrosis may limit range of motion due to pain or a mechanical block (Fig. 1).
Figure 1.
Post-fracture stiffness in a 63-year-old female patient due to avascular necrosis secondary to proximal humerus fracture treated non-operatively. In this case, due to the destruction of the articular surface, treatment includes open arthrolysis and anatomic total shoulder arthroplasty. (A) True AP radiograph showing right two-part proximal humerus fracture. (B) True AP radiograph at 6 months post-injury demonstrating radiographic union. (C) True AP radiograph 12 months post-injury with visible avascular necrosis. (D) Coronal slice CT-scan at 12 months post-injury demonstrating advanced collapse and glenohumeral joint arthrosis. (E) Postoperative x-ray with total shoulder arthroplasty in situ.
Stiffness related to osteosynthesis
Poor positioning of implants, secondary collapse, and late displacement of fracture fragments can lead to impingement of the implant in the subacromial space producing limitation of range of motion, primarily abduction, due to mechanical effect (12). Screw penetration due to malposition or secondary collapse may lead to secondary damage of the joint and stiffness (13).
Stiffness due to infection
Infection should always be considered. Low-grade infections can be hard to detect as the lab work is often normal and the typical clinical signs are not always encountered (14). Akgün et al. showed a 50% rate of unexpected positive cultures for Propionibacterium acnes in patients undergoing surgery for post-surgical stiffness after ORIF. They suggested routine evaluation in all patients undergoing revision surgery after ORIF (15).
Other pain-related causes
The presence of pain and thus limited motion is associated with low adherence to physiotherapy and persisting stiffness (16). The long head of the biceps is an important structure associated with pain after PHF due to interposition in the fracture, instability in the bicipital groove, and anterior impingement (17). Other possible causes of pain include nerve irritation due to plate proximity, especially during minimally invasive techniques (18), and aggravation of previously asymptomatic acromioclavicular joint arthrosis.
Diagnosis
First, a detailed clinical history, and then a clinical examination are crucial for identifying secondary stiffness and possible causes. Evaluating the severity and confirming secondary causes of range of motion restriction are key to successful management and adherence to the subsequent physio. In the history, careful attention must be placed on the presence of pain, new shoulder injury, specific limitations during daily activities, and any clinical features suggestive of infection. Regarding the fracture itself, it is important to specify the time lapsed since the traumatic event, any treatments undertaken, duration of immobilization, and subsequent physiotherapy rehabilitation.
The physical exam is important. Careful assessment of function including accurate evaluation of range of motion in all planes, preferably using a goniometer, is required. Key aspects of the physical examination are: (i) confirmation of active and/or passive glenohumeral range of motion restriction; (ii) assessment of severity and stiffness pattern, which helps to determine the involved anatomical structures and any hardware-related issues. Generally, rotator interval contracture will limit the external rotation in adduction; antero-inferior capsule contracture will limit the external rotation in abduction; posterior capsule contracture will limit the internal rotation, especially in 90° abduction; (iii) identifying secondary causes of pain or stiffness, such as long biceps pathology or entrapment (classic biceps’ tests), nerve lesions or entrapment (atrophy, numbness, paresis), acromioclavicular joint arthrosis (tenderness over AC joint), rotator cuff tear (weakness during classic rotator cuff tests), and muscle atrophy.
Radiological evaluation
Standardradiographs of the shoulder composed of anterior–posterior (AP), axial, and Neer projections are strongly recommended and aid with the assessment for secondary causes. A CT scan is valuable in determining union, malunion, osteonecrosis, implant positioning, screw penetration, and degenerative arthritic changes. The fracture position, presence of union, and implant positioning are important features to define possible impingement zones and future treatment options. An MRI may show signs of capsular thickness, rotator cuff injury, biceps pathology, AC joint pathology, and extraarticular adhesions. When implants are in situ, artifact degradation is often seen and therefore Metal Artifact Reduction sequences are necessary (19).
Treatment
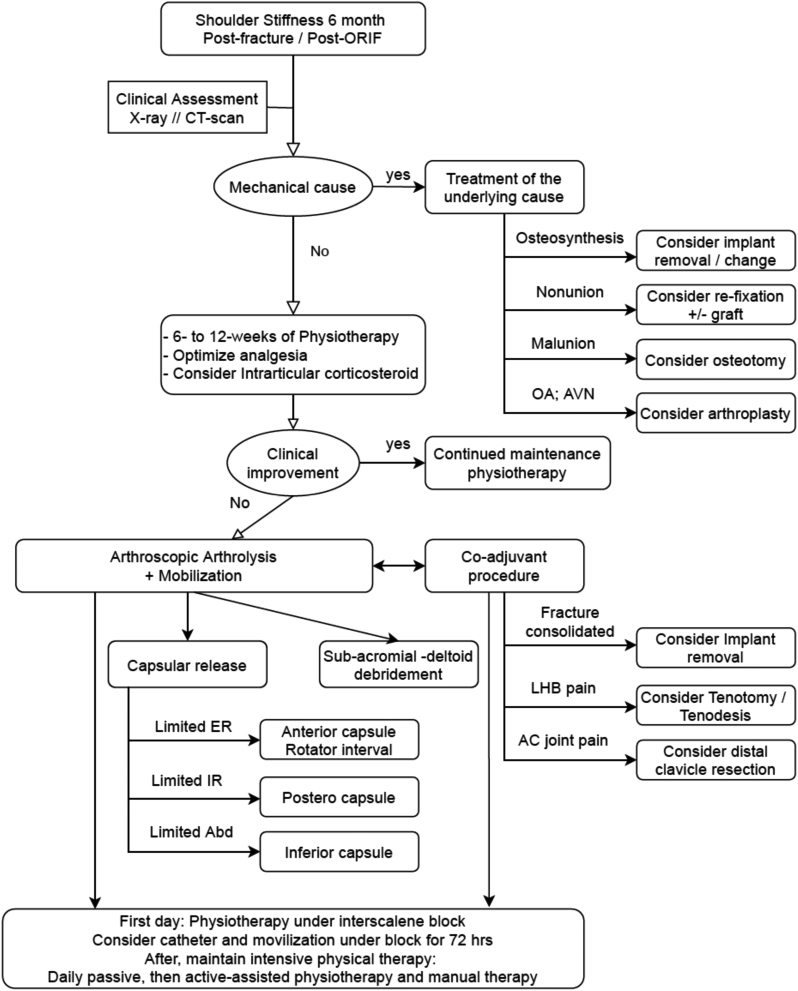
Treatment should be specified according to the cause and patients’ expectations. The goal is to relieve pain, improve range of motion, and restore function. Due to the lack of comparative studies, there is no consensus regarding the optimal treatment of post-fracture stiffness. There is no consensus regarding an optimal algorithm for treatment. We propose a treatment protocol which is summarized in Fig. 2.
Figure 2.
A suggested treatment protocol for post-fracture and post-ORIF stiffness.
Conservative treatment
Physiotherapy remains the first line of treatment. However, the outcomes are poor (8). Before commencing a regime of conservative treatment, it is important to rule out associated reversible causes of stiffness, such as infection, non-union, or implant impingement.
Physiotherapy is usually focused on capsular stretching, passive mobilization, and global functional muscle rehabilitation. It can be used as an isolated treatment or as an adjunct to other treatments (20). Physiotherapy in the context of pain may limit its efficacy, and it is important to control pain in order to allow appropriate rehabilitation to occur. Regular non-steroidal anti-inflammatory drugs are usually indicated and may improve the tolerance to physiotherapy (8).
The use of corticosteroids may be considered as an adjunct to physiotherapy. However, it is unclear how efficacious steroid injections are in isolation. In a recent randomized controlled study of 88 patients undergoing surgical treatment for PHF (21), the use of intraarticular triamcinolone injection improved the range of motion and pain at 3 and 6 months post-operatively. Cortisone injections in this study were given at 8 weeks post-operatively. This effect was not sustained at the 12-month time point. There is no consensus over the optimal timing for cortisone injection for addressing post-surgical shoulder stiffness. On the assumption that the treatment effect of cortisone in these circumstances is to lessen the degree of inflammation, earlier administration in patients identified as developed secondary stiffness may be useful, ideally prior to the switch to fibrotic reaction occurs. The use of triamcinolone injections was not associated with increased infection or non-union rates. Oral corticosteroids have been shown to provide pain relief and range of motion and function in the primary frozen shoulder (22). However, the efficacy of oral steroids in post-traumatic secondary shoulder stiffness has not been demonstrated in the literature. Other drugs have been used as a prophylactic for stiffness in other joints. The use of statins has been tested to prevent post-traumatic stiffness in an animal model showing promising results (23). Nevertheless, no trial has been conducted in humans and no recommendations for its use can be made.
The use of mobilization under anesthesia (MUA) is controversial. A study investigating the outcome of MUA in patients with primary frozen shoulder compared to those with refractory post-traumatic stiffness, including 55% of PHFs treated non-operatively, was reported (3). Both groups benefited from MUA, and no significant differences between the groups were found. To our knowledge, there are no studies evaluating the use of isolated MUA, specifically for operatively managed PHF. Complications including fractures, dislocations, and brachial plexus injury have been reported with the use of MUA (24). Therefore, MUA is not recommended for operated or non-operated PHFs. A controlled surgical release of the capsule and adhesive tissue is preferred in selected patients.
Other treatment options currently in use such as distensionarthrography(25) have not been demonstrated to be an effective treatment for post-traumatic secondary stiffness.
Surgical treatment
Capsular release may be beneficial given the nature and degree of post-traumatic stiffness. There is still no clear ´optimal timing´ for surgery; however, it is generally considered that surgical release may be utilized sooner when compared to a primary frozen shoulder. Consolidation of the fracture should be confirmed before considering any surgical intervention. Some surgeons consider surgery for secondary stiffness at 6 months post-fracture or post-ORIF, which has not improved during a 6- to 12-week trial of physiotherapy (8, 26). Arthrolysis, performed open or arthroscopically, is the most common surgical procedure to improve post-traumatic secondary stiffness. This is the case in both operatively managed and conservatively managed proximal humeral fractures. An á la carte approach dependent on concomitant factors such as impingement, implant malposition, and non-union may be considered. Additional surgical procedures may include implant removal, tenotomy or tenodesis of the long head of the biceps, and samples for microbiological assessment.
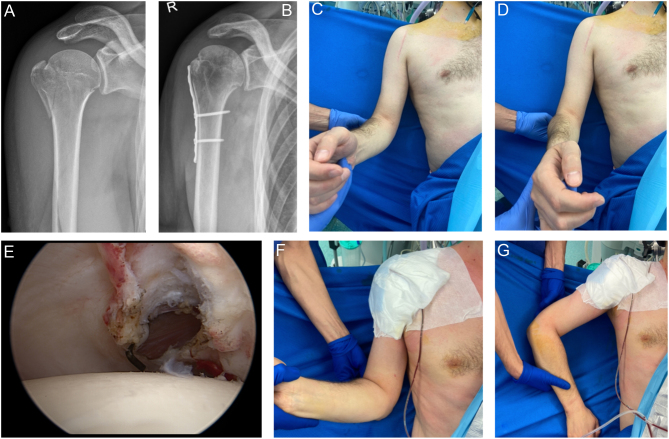
Arthrolysis consists of capsular and rotator interval release in combination with subacromial bursectomy. It is the commonest surgical procedure even if other causes exist, such as bony or implant impingement. This is due to the frequent finding of capsular contracture associated with various extraarticular causes for stiffness (3). Arthrolysis was initially described as an open procedure (9, 27); however recently, arthroscopic arthrolysis is considered the gold standard (9, 12, 26, 28, 29, 30, 31, 32). In comparison to an open procedure, arthroscopic arthrolysis allows the surgeon to conduct a release of the capsule at 270° or 360° under direct visualization, including the resection of the rotator interval and coracohumeral ligament (26, 28) (Fig. 3). One study by Snow et al. demonstrated that release of the posterior capsule is less effective in restoring internal rotation than the release of the anterior and inferior structures for their respective planes of motion (33).
Figure 3.
Post-fracture stiffness in a 37-year-old male patient secondary to proximal humerus fracture treated with ORIF. In this case, due to global limitation in range of motion, arthroscopic arthrolysis and implant removal were performed. (A) Preoperative true AP radiograph showing 3-part PHF. (B) Post-operative true AP radiograph showing fixation with 1/3 tubular plate osteosynthesis. (C–D) Preoperative ROM: 45° abduction, 10° external rotation (at 0° abduction), and 10° internal rotation (at 0° abduction). (E) Arthroscopic view from anterior portal showing complete posteroinferior capsule release (this was extended superiorly to complete the capsular release). (F–G) Postoperative ROM: 95° Abduction, 50° external rotation, and 90° internal rotation.
For this specific procedure, some considerations should be taken into account: (i) Due to excessive thickening of the capsule, the introduction of the scope and various instruments can be challenging and pose a higher risk of chondral damage. (ii) Distortions of the normal anatomy are possible due to mal-union of the greater tuberosity or other aspects of the proximal humerus. To avoid this, a careful preoperative plan should be performed. (iii) The greatest plane of restriction should be clearly defined and the capsule released appropriately. Generally, contracture of the rotator interval will limit external rotation in adduction; contracture of the antero-inferior capsule will limit external rotation in abduction; and contracture of the posterior capsule will limit internal rotation. Greater limitation of rotation in adduction compared to abduction may be due to extraarticular adhesion around the hardware (34).
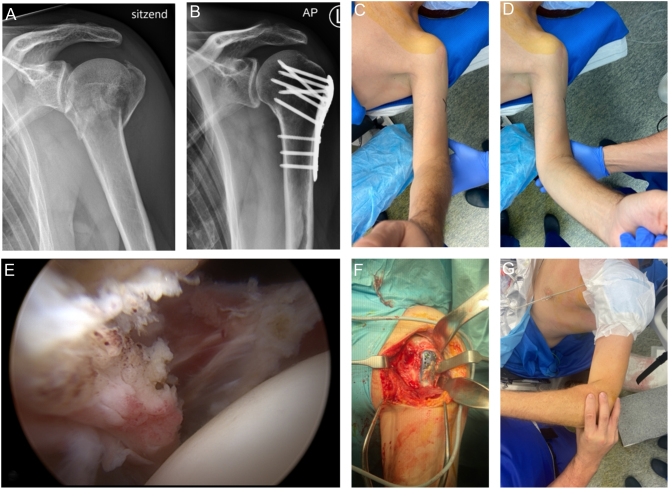
Subacromialandsubdeltoidrelease is appropriate in cases of stiffness secondary to PHF, especially in post-operative cases in which extraarticular adhesions are frequently observed. In cases where the PHF was managed conservatively or where plate removal is not needed, an arthroscopic subacromial and subdeltoid decompression is preferred (10, 18, 25, 26, 28, 29). This typically includes a subacromial and subdeltoid bursectomy, debridement of any adhesions in these spaces, and partial resection of the coracoacromial ligament. In post-operative post-traumatic cases, which require implant removal, an open bursectomy and debridement is also possible (9, 30) (Fig. 4).
Figure 4.
Post-fracture stiffness in a 49-year-old male patient posterior to PHF treated with ORIF. In this case, due to global limitation in ROM, arthroscopic arthrolysis associated with plate removal was performed. (A) Preoperative x-ray showing 3-part PHF. (B) Post-operative x-ray with PHILOS plate osteosynthesis. (C–D) Preoperative ROM: 60° abduction, 10° external rotation, and 0° internal rotation. (E) Arthroscopic view from anterior portal showing complete posterior capsule release. (F) Adhesions in the subdeltoid space and through the plate. (G) Postoperative ROM: 95° Abduction, 60° external rotation, and 80° internal rotation.
After completion of the capsular release and debridement, but prior to any implant removal, controlled mobilization under anesthesia should be performed to release any remaining adhesions. After implant removal, assessment and documentation of the achieved final range of motion are recommended.
For osteosynthesisremoval, preoperative planning should be performed to ensure specific required instrumentation is available. Screw removal sets should always be available. Before removing the screw, careful cleaning of the screw head recess should be performed. An in-line, preferably new screwdriver should be used with gentle impaction on the screwdriver into the screw head prior to attempted removal of the screw. This is especially important in titanium implants. Suture material should be removed prior to removal of the plate. The removed implants should be sent for sonication and microbial cultures (35), independent of whether other microbial cultures were taken.
Osteosynthesis implant removal can be done through an open approach, assisted by an arthroscope or completely arthroscopically. There are several articles demonstrating the feasibility of the removal of a proximal humeral plate arthroscopically (2, 31, 36, 37, 38), showing good results without increased complications (26, 34, 39, 40, 41). Removal of the plate or nail via an open surgical approach has also shown satisfactory results (12, 28, 30). This allows for a careful release of subacromial and subdeltoid adhesions, together with a selective and controlled debridement of the tissue surrounding the plate. After removing the plate, no other mobilization maneuvers should be performed due to the high risk of displacement of the previous fracture or a new fracture through the screw holes.
Other implants have been utilized for PHFs, including nails and external fixators (42). When removing nails, the locking bolts are removed first. Long intramedullary nails with locking bolts in the distal 1/3 of the humerus require an open surgical approach is recommended to avoid iatragenic nerve injury. All locking bolts should be removed prior to nail removal. Confirmation with image intensifier fluoroscopy may be needed. When removing the nail, it is important to note whether an end cap is present. If present, this must be removed prior to guidewire insertion. Bone in-growth into the proximal opening of the nail needs to be identified and removed to allow application of the extraction handle. Techniques for external fixation of PHF have been utilized with increasingly favorable outcomes (43). In a study of 188 patients with PHFs treated with closed or open reduction and a dedicated external fixator, reported mean forward elevation of 137 (95% CI: 130–142°). Four patients (2.1%) developed secondary stiffness, with two of these requiring surgical intervention. The mean time to removal of the fixator was 42 days.
Some additional procedures can be performed with arthrolysis and osteosynthesis removal. Some are frequently indicated, while others depend on the patient’s symptoms and intraoperative findings. A tenotomy or tenodesis of the long head of the biceps is indicated in the presence of biceps pathology. The long head of the biceps may be associated with persistent pain after PHF or ORIF (17, 44). Sometimes, biceps pathology is not clearly identified during clinical evaluation or intraoperatively. Therefore, some authors suggest a long head of biceps tenotomy or tenodesis routinely during arthrolysis, after PHF or revision cases, even in the absence of clear biceps pathology (44). Multiple microbial cultures should be taken to rule out low-grade infection in all cases of operatively treated PHF complaining of pain and stiffness, even in the absence of overt signs of infection. Other additional procedures can be performed depending on the patient’s symptoms. These include distal clavicular resection to treat acromioclavicular joint pathology, acromioplasty in mechanical impingement, and suprascapular nerve release in cases with nerve irritation features. Surgical management of post-traumatic stiffness may only be a part of the overall definitive management, which may also include anatomic or reverse total shoulder arthroplasty (Fig. 1).
Postoperative rehabilitation
Post-operatively, an intensive stretching program is recommended to maintain the functional range of motion achieved. This typically commences immediately, on the same day of the surgery, aided by the effects of regional anesthesia. This allows for a baseline range of motion achieved intraoperatively, uninhibited by pain, to be demonstrated by the therapist to the patient. Some authors suggest the use of a catheter rather than single-dose regional anesthesia (45). This may extend the effect of the pain block, increasing the effect of the passive range of motion physiotherapy during the first days of the postoperative period.
On discharge, the patient is encouraged to perform daily exercises as part of an intensive therapy program. This may include supervised daily therapy sessions. Meticulous pain control, using a variety of modalities, can increase adherence to the therapy regime (16). If available, the use of a continuous passive motion machine may be utilized to augment the early rehabilitation phase and aid maintenance of the achieved intra-operative range of motion.
Outcomes
The results of conservative and surgical treatments for stiffness secondary to PHF remain unclear. This is because most studies are observational, lack a control group, and contain relatively small numbers. The inclusion criteria between studies vary leading to no clear consensus as to the optimal management. In general, most reported series show as follows: (i) worse clinical outcomes with conservative and surgical treatment compared to primary frozen shoulder; (ii) improvement of range of motion and functional outcomes with arthrolysis (open or arthroscopic) with or without implant removal. The summary of results available in the literature is depicted in Table 1. Eight studies reported on the outcomes of 266 patients undergoing arthrolysis (open or arthroscopic) in patients with post-surgical stiffness after PHF treatment. The mean age was 58 years and the mean follow-up of 22 months. Forward elevation improved by a mean of 35°; abduction improved by a mean of 46°; external rotation improved by a mean of 22°. Constant score was reported in five studies and demonstrated a mean improvement of 26 points (MCID: 7.6–9.3) (46, 47).
Table 1.
Outcome reported after arthrolysis in patients with shoulder stiffness after operated proximal humerus fracture.
| Study | OS removal | Patients, n | Age*, years | F-U*, months | Difference | Complications, n (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| FE (°) | Abd (°) | ER (°) | IR (°) | CS | ||||||
| Levy et al. (48) | - | 14 | 54 (26–81) | 33 (13–60) | 76 | - | 57 | - | - | 1 AN |
| Maqdes et al. (41) | Arthroscopic | 11 | 54.6 ± 11 | 17.7 ± 23 | 11.8 | 26.8 | 16.8 | L3–T12 | 17.1 | No |
| Kathagen et al. (26) | Arthroscopic | 45 | 58.5 (30–82) | 24 | 19 | 19.9 | 11.9 | 23 | - | No |
| Acklin et al. (30) | Open | 20 | 56 ± 12 | - | - | - | - | - | 6 | No |
| Maroun et al. (12) | Open | 58 | 58 (24–79) | 23 (6–60) | 37.6 | 39.5 | 24.3 | S1–T12 | 31.7 | No |
| Hagiwara et al. (28) | - | 12 | 65.1 ± 10 | 30.6 ± 12 | 48 | 47 | 21 | 30 | 39.6 | No |
| Waszczykowski et al. (34) | Arthroscopic | 18 | 56 (23–75) | 24 | 34 | 41.2 | 53.2 | L2–T11 | 26.2 | No |
| Chan et al. (40) | Arthroscopic | 88 | 59 ± 14 | 4.7 ± 7 | 37 | 67.8 | 14.9 | 36.2 | - | 2 RF |
| Total† | 266 | 58 | 22 | 35 | 46 | 22 | 31 | 26 | 3 (1%) | |
*Data are presented as mean ± s.d. or mean (range); †mean age, F-U, and complications are presented.
Abd, abduction; AN, avascular necrosis; CS, Constant score; ER, external rotation; FE, forward elevation; F-U, follow-up; IR, internal rotation; OS, osteosynthesis; RF, refractures.
Conclusions
Secondary stiffness following proximal humeral fracture remains a challenge for successful management and return to peak shoulder function. A careful history, clinical examination, and investigations are needed to identify contributing factors for addressing pain and stiffness. Conservative management including physiotherapy and injections form the first line ofn treatment for most with clear cause for surgery. Surgery to address avascular necrosis, secondary arthropathy, and metalwork impingement/failure is often needed to gain significant clinical improvement. Arthrolysis (open or arthroscopic) should address areas of passive restriction identified by clinical examination. Additional procedures such as biceps tenotomy/tenodesis, microscopy culture, acromioplasty for subacromial impingement, and nerve release may be required. This review outlined the limited evidence that may guide management and offered suggestions for successful treatment of post-traumatic shoulder stiffness.
ICMJE conflict of interest statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding statement
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Acknowledgements
The authors are grateful to Trinidad Alliende for proofreading the manuscript and Annabel Hayoz for her help in the submission process.
References
- 1.Maier D Jaeger M Izadpanah K Strohm PC & Suedkamp NP. Proximal humeral fracture treatment in adults. Journal of Bone and Joint Surgery. American Volume 201496251–261. ( 10.2106/JBJS.L.01293) [DOI] [PubMed] [Google Scholar]
- 2.Spross C Meester J Mazzucchelli RA Puskás GJ Zdravkovic V & Jost B. Evidence-based algorithm to treat patients with proximal humerus fractures—a prospective study with early clinical and overall performance results. Journal of Shoulder and Elbow Surgery 2019281022–1032. ( 10.1016/j.jse.2019.02.015) [DOI] [PubMed] [Google Scholar]
- 3.Lancaster ST Grove TN & Woods DA. Management of post-traumatic stiffness of the shoulder following upper limb trauma with manipulation under anaesthetic. Shoulder and Elbow 20179258–265. ( 10.1177/1758573217693974) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouaicha S Wieser K Kriechling P & Scholz-Odermatt SM. A large-scale assessment of the healthcare burden of adhesive capsulitis of the shoulder joint. Swiss Medical Weekly 2020150 w20188. ( 10.4414/smw.2020.20188) [DOI] [PubMed] [Google Scholar]
- 5.Robinson CM Stirling PHC Goudie EB Macdonald DJ & Strelzow JA. Complications and long-term outcomes of open reduction and plate fixation of proximal humeral fractures. Journal of Bone and Joint Surgery. American Volume 20191012129–2139. ( 10.2106/JBJS.19.00595) [DOI] [PubMed] [Google Scholar]
- 6.Audigé L Brorson S Durchholz H Lambert S Moro F & Joeris A. Core set of unfavorable events of proximal humerus fracture treatment defined by an international Delphi consensus process. BMC Musculoskeletal Disorders 2021221002. ( 10.1186/s12891-021-04887-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Itoi E Arce G Bain GI Diercks RL Guttmann D Imhoff AB Mazzocca AD Sugaya H & Yoo YS. Shoulder stiffness: current concepts and concerns. Arthroscopy 2016321402–1414. ( 10.1016/j.arthro.2016.03.024) [DOI] [PubMed] [Google Scholar]
- 8.Robinson CM Seah KTM Chee YH Hindle P & Murray IR. Frozen shoulder. Journal of Bone and Joint Surgery. British Volume 2012941–9. ( 10.1302/0301-620X.94B1.27093) [DOI] [PubMed] [Google Scholar]
- 9.Voigt C Geduhn M Geerling J & Lill H. Arthroscopic and open arthrolysis in secondary shoulder stiffness. Obere Extremität 20094168–177. ( 10.1007/s11678-009-0038-4) [DOI] [Google Scholar]
- 10.Duparc F. Malunion of the proximal humerus. Orthopaedics and Traumatology, Surgery and Research 201399(1) S1–S11. ( 10.1016/j.otsr.2012.11.006) [DOI] [PubMed] [Google Scholar]
- 11.Nyffeler RW Seidel A Werlen S & Bergmann M. Radiological and biomechanical assessment of displaced greater tuberosity fractures. International Orthopaedics 2019431479–1486. ( 10.1007/s00264-018-4170-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maroun C Aliani D Hass A Werthel JD Vidil A & Valenti P. Shoulder arthroscopy combined to hardware removal in proximal humeral fractures: a series of 58 cases with a mean follow-up of 2 years. European Journal of Orthopaedic Surgery and Traumatology: Orthopedie Traumatologie 201727317–321. ( 10.1007/s00590-017-1938-4) [DOI] [PubMed] [Google Scholar]
- 13.Owsley KC & Gorczyca JT. Displacement/screw cutout after open reduction and locked plate fixation of humeral fractures. Journal of Bone and Joint Surgery. American Volume 200890233–240. ( 10.2106/JBJS.F.01351) [DOI] [PubMed] [Google Scholar]
- 14.Ruskin J Seigerman D Sirkin M Reilly M & Adams M. Propionibacterium acnes infection of the shoulder after a manipulation under anesthesia for stiffness status post open reduction and internal fixation proximal humerus: A case report. Journal of Orthopaedic Case Reports 2018819–22. ( 10.13107/jocr.2250-0685.1030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akgün D Peters PM Maziak N Plachel F Minkus M & Moroder P. High rate of unexpected positive cultures in presumed aseptic revision of stiff shoulders after proximal humerus osteosynthesis. BMC Musculoskeletal Disorders 202021393. ( 10.1186/s12891-020-03430-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skedros JG Adondakis MG Knight AN & Pilkington MB. Frequency of shoulder corticosteroid injections for pain and stiffness after shoulder surgery and their potential to enhance outcomes with physiotherapy: A retrospective study. Pain and Therapy 2017645–60. ( 10.1007/s40122-017-0065-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luigi BV Giovanni C & Mauro M. Long head of biceps in proximal fractures of the humerus: an underestimated problem? Critical analysis and review of the literature. Acta Biologicaet Medica 20209169–78. ( 10.23750/abm.v91i4-S.9634) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dang KH Ornell SS Reyes G Hussey M & Dutta AK. A new risk to the axillary nerve during percutaneous proximal humeral plate fixation using the Synthes PHILOS aiming system. Journal of Shoulder and Elbow Surgery 2019281795–1800. ( 10.1016/j.jse.2019.01.019) [DOI] [PubMed] [Google Scholar]
- 19.Branco D Kry S Taylor P Rong J Zhang X Frank S & Followill D. Evaluation of image quality of a novel computed tomography metal artifact management technique on an anthropomorphic head and neck phantom. Physics and Imaging in Radiation Oncology 202117111–116. ( 10.1016/j.phro.2021.01.007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elhassan B Ozbaydar M Massimini D Higgins L & Warner JJP. Arthroscopic capsular release for refractory shoulder stiffness: A critical analysis of effectiveness in specific etiologies. Journal of Shoulder and Elbow Surgery 201019580–587. ( 10.1016/j.jse.2009.08.004) [DOI] [PubMed] [Google Scholar]
- 21.Kim YS Lee KG & Lee HJ. Effect of triamcinolone acetonide on stiffness after surgical treatment of proximal humerus fractures: a randomized controlled study. Archives of Orthopaedic and Trauma Surgery 20201401731–1737. ( 10.1007/s00402-020-03425-3) [DOI] [PubMed] [Google Scholar]
- 22.Buchbinder R Green S Youd JM & Johnston RV. Oral steroids for adhesive capsulitis. Cochrane Database of Systematic Reviews 20062006CD006189. ( 10.1002/14651858.CD006189) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baranowski A, Schlemmer L, Förster K, Slotina E, Mickan T, Truffel S, Klein A, Mattyasovszky SG, Hofmann A, Ritz U, et al. Effects of losartan and atorvastatin on the development of early posttraumatic joint stiffness in a rat model. Drug Design, Development and Therapy 2019132603–2618. ( 10.2147/DDDT.S204135) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang JP Huang TF Hung SC Ma HL Wu JG & Chen TH. Comparison of idiopathic, post-trauma and post-surgery frozen shoulder after manipulation under anesthesia. International Orthopaedics 200731333–337. ( 10.1007/s00264-006-0195-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicholson JA Slader B Martindale A Robinson CM & McKie S. Distension arthrogram in the treatment of adhesive capsulitis has a low rate of repeat intervention: A ten-year review. Bone and Joint Journal 2020B102606–610. ( 10.1302/0301-620X.102B5.BJJ-2020-0082) [DOI] [PubMed] [Google Scholar]
- 26.Katthagen JC Hennecke D Jensen G Ellwein A Voigt C & Lill H. Arthroscopy after locked plating of proximal humeral fractures: implant removal, capsular release, and intra-articular findings. Arthroscopy 2014301061–1067. ( 10.1016/j.arthro.2014.04.092) [DOI] [PubMed] [Google Scholar]
- 27.Omari A & Bunker TD. Open surgical release for frozen shoulder: surgical findings and results of the release. Journal of Shoulder and Elbow Surgery 200110353–357. ( 10.1067/mse.2001.115986) [DOI] [PubMed] [Google Scholar]
- 28.Hagiwara Y Kanazawa K Ando A Sekiguchi T Koide M Yabe Y & Itoi E. Effects of arthroscopic pancapsular release for proximal humeral fractures treated with intramedullary nailing: a retrospective study. JSES International 20204546–550. ( 10.1016/j.jseint.2020.03.013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franceschi F Papalia R Palumbo A Vasta S Maffulli N & Denaro V. Management of postoperative shoulder stiffness. Sports Medicine and Arthroscopy Review 201119420–427. ( 10.1097/JSA.0b013e3182393e06) [DOI] [PubMed] [Google Scholar]
- 30.Acklin YP Michelitsch C & Sommer C. Elective implant removal in symptomatic patients after internal fixation of proximal humerus fractures improves clinical outcome. BMC Musculoskeletal Disorders 201617119. ( 10.1186/s12891-016-0977-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Voigt C Geisler A & Lill H. Arthroscopic locking plate removal after proximal humeral fractures. Archives of Orthopaedic and Trauma Surgery 2010130391–395. ( 10.1007/s00402-009-0882-0) [DOI] [PubMed] [Google Scholar]
- 32.Holloway GB Schenk T Williams GR Ramsey ML & Iannotti JP. Arthroscopic capsular release for the treatment of refractory postoperative or post-fracture shoulder stiffness. Journal of Bone and Joint Surgery. American Volume 2001831682–1687. ( 10.2106/00004623-200111000-00010) [DOI] [PubMed] [Google Scholar]
- 33.Snow M Boutros I & Funk L. Posterior arthroscopic capsular release in frozen shoulder. Arthroscopy 20092519–23. ( 10.1016/j.arthro.2008.08.006) [DOI] [PubMed] [Google Scholar]
- 34.Waszczykowski M & Fabiś J. Selective glenohumeral external rotation deficit - Sequelae of post-ORIF deltoid adhesions after treatment of the proximal humerus fracture. BMC Musculoskeletal Disorders 202021625. ( 10.1186/s12891-020-03634-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dudareva M, Barrett L, Figtree M, Scarborough M, Watanabe M, Newnham R, Wallis R, Oakley S, Kendrick B, Stubbs D, et al. Sonication versus tissue sampling for diagnosis of prosthetic joint and other orthopedic device-related infections. Journal of Clinical Microbiology 201856. ( 10.1128/jcm.00688-18) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Voleti PB Camp CL Sinatro AL & Dines JS. Arthroscopic removal of symptomatic proximal humerus locking plates with bone-void filler augmentation. Arthroscopy Techniques 20165e343–e346. ( 10.1016/j.eats.2016.01.009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bhatia DN. Arthroscopic removal of proximal humerus plates in chronic post-traumatic shoulder stiffness. Arthroscopy Techniques 20176e375–e381. ( 10.1016/j.eats.2016.10.014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dines JS Hettrich CM Kelly BT Savoie FH & Lorich DG. Arthroscopic removal of proximal humerus locking plates. Knee Surgery, Sports Traumatology, Arthroscopy 201018409–411. ( 10.1007/s00167-009-0991-x) [DOI] [PubMed] [Google Scholar]
- 39.Katthagen JC Jensen G Hennecke D Lill H & Voigt C. Arthroskopische materialentfernung nach winkelstabiler plattenosteosynthese am proximalen humerus: Technik und erste Ergebnisse im Vergleich zur offenen materialentfernung. Der Unfallchirurg 201211547–54. ( 10.1007/s00113-011-1953-6) [DOI] [PubMed] [Google Scholar]
- 40.Chan JM Kahlenberg C Gadinsky NE Lorich DG & Dines JS. Arthroscopic-assisted removal of proximal humerus locking plates with capsular release significantly improves range of motion and function. Arthroscopy, Sports Medicine, and Rehabilitation 20213e211–e217. ( 10.1016/j.asmr.2020.09.013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maqdes A Levy B Klouche S & Hardy P. The feasibility and results of an arthroscopic removal of humeral locking plates and glenohumeral arthrolysis after proximal humeral fractures. Knee Surgery, Sports Traumatology, Arthroscopy 201422456–461. ( 10.1007/s00167-013-2437-8) [DOI] [PubMed] [Google Scholar]
- 42.Hohmann E Keough N Glatt V & Tetsworth K. Surgical treatment of proximal humerus fractures: a systematic review and meta-analysis. European Journal of Orthopaedic Surgery and Traumatology: Orthopedie Traumatologie 2022. ( 10.1007/s00590-022-03436-3) [DOI] [PubMed] [Google Scholar]
- 43.Blonna D Assom M Bellato E Pisanu G Greco V Marmotti A & Rossi R. Outcomes of 188 proximal humeral fractures treated with a dedicated external fixator with follow-up ranging from 2 to 12 years. Journal of Bone and Joint Surgery. American Volume 20191011654–1661. ( 10.2106/JBJS.18.00734) [DOI] [PubMed] [Google Scholar]
- 44.Szabó I Boileau P & Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Medicine and Arthroscopy Review 200816180–186. ( 10.1097/JSA.0b013e3181824f1e) [DOI] [PubMed] [Google Scholar]
- 45.Katthagen JC Schliemann B Dyrna F & Raschke MCEJ. Posttraumatic shoulder stiffness. Der Unfallchirurg 2021124241–251. ( 10.1007/s00113-021-00956-1) [DOI] [PubMed] [Google Scholar]
- 46.Ibounig T Juurakko J Lähdeoja T Sumrein BO Järvinen TLN Paavola M Ardern CL Karjalainen T Taimela S & Rämö L. Minimal important difference and patient acceptable symptom state for common outcome instruments in patients with a closed humeral shaft fracture - analysis of the FISH randomised clinical trial data. BMC Medical Research Methodology 202222291. ( 10.1186/s12874-022-01776-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou A Xu S Yew KSA & Lie DTT. Minimal clinically important differences for Oxford, constant, and University of California Los Angeles shoulder scores after reverse shoulder arthroplasty to allow interpretation of patient-reported outcome measures and future statistical power analyses. Arthroscopy 2023391405–1414. ( 10.1016/j.arthro.2022.12.027) [DOI] [PubMed] [Google Scholar]
- 48.Levy O Webb M Even T Venkateswaran B Funk L & Copeland S A.. Arthroscopic capsular release for posttraumatic shoulder stiffness. Journal of Shoulder and Elbow Surgery 200817410–414. ( 10.1016/j.jse.2007.11.014) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a