Abstract
Introduction
Glioblastoma (GBM) is the most common malignant primary central nervous system cancer in adults. The objective of the Multi-Arm GlioblastoMa Australasia (MAGMA) trial is to test hypotheses in real world setting to improve survival of people with GBM. Initial experimental arms are evaluating the effectiveness of interventions in newly diagnosed GBM (ndGBM). This study will compare maximal surgical resection followed by chemoradiotherapy plus adjuvant chemotherapy for 6 months with the addition of (1) ‘neoadjuvant’ chemotherapy beginning as soon as possible after surgery and/or (2) adjuvant chemotherapy continued until progression within the same study platform.
Methods and analysis
MAGMA will establish a platform for open-label, multiarm, multicentre randomised controlled testing of treatments for GBM. The study began recruiting in September 2020 and recruitment to the initial two interventions in MAGMA is expected to continue until September 2023.
Adults aged ≥18 years with ndGBM will be given the option of undergoing randomisation to each study intervention separately, thereby giving rise to a partial factorial design, with two separate randomisation time points, one for neoadjuvant therapy and one for extended therapy. Patients will have the option of being randomised at each time point or continuing on with standard treatment.
The primary outcome for the study is overall survival from the date of initial surgery until death from any cause. Secondary outcomes include progression-free survival, time to first non-temozolomide treatment, overall survival from each treatment randomisation, clinically significant toxicity as measured by grade 3 or 4 adverse events and health-related quality-of-life measures. Tertiary outcomes are predictive/prognostic biomarkers and health utilities and incremental cost-effectiveness ratio.
The primary analysis of overall survival will be performed separately for each study intervention according to the intention to treat principle on all patients randomised to each study intervention.
Ethics and dissemination
The study (Protocol version 2.0 dated 23 November 2020) was approved by a lead Human Research Ethics Committee (Sydney Local Health District: 2019/ETH13297). The study will be conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice.
Trial registration number
ACTRN12620000048987.
Keywords: Adult oncology, Neurological oncology, Magnetic resonance imaging
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Once established, the Multi-Arm GlioblastoMa Australasia platform will enable more rapid and cost effective assessment of new treatments for glioblastoma than stand-alone trials.
Incorporation of a partial factorial clinical trial design will allow several interventions to be examined within a single clinical trial, where it is not feasible to randomise all participants to both interventions.
Pragmatic study design elements such as parsimonious data collection will limit the amount of extraneous information collected, reducing the burden of collecting non-informative information such as previously reported low grade toxicity from temozolomide.
Sharing academic credit and future design opportunities via a consortium model will encourage contributions from early career researchers and clinical neuro-oncologists.
An initial treatment intervention looking at the benefit of extending temozolomide beyond 6 months will address biases in previous studies by mandating randomisation of patients before adjuvant treatment commences.
Introduction
Glioblastoma (GBM) is the most common malignant primary brain cancer in adults. Improving treatment remains elusive, with an overall 1-year survival less than 50% and 5-year survival of less than 5% that has not changed in the past decade.1 Since the introduction of concurrent temozolomide (TMZ) with postsurgical radiation followed by ‘adjuvant’ TMZ chemotherapy in 2005,2 there has been little progress in improving outcomes despite numerous trials proceeding to phase III.3–5 No new drugs have been approved for newly-diagnosed GBM (ndGBM) since TMZ. TMZ is a brain-penetrant alkylating agent that promotes DNA/RNA methylation and ultimately gives rise to cellular apoptosis by inducing G2/M phase cell cycle arrest. DNA repair is controlled in vivo by the O(6)-methylguanine-DNA methyltransferase (MGMT) enzyme. MGMT methylation and silencing is associated with improved sensitivity to TMZ.6 A more recent development is the tumour-treating fields (TTF) device, which showed incremental change in survival in an unblinded phase III trial, but usage in clinical practice has been curtailed due to cost-effectiveness and logistical considerations.7 8 TTF is currently unavailable in Australasia. This underlines the importance of testing treatments for ndGBM which are suitable for rapid and widespread implementation in the community.
The failure of many novel therapies has encouraged attempts to improve existing treatments. Dose-dense or dose-intense TMZ has not demonstrated benefit compared with the EORTC/Stupp regimen, while other efforts to modify MGMT activity to augment TMZ chemotherapy are ongoing.9 10
Treatment sequencing is a potential area for intervention. Standard treatment with surgery is necessary for diagnosis and confers a survival benefit11; however, surgery is associated with systemic immunosuppression,12 local inflammation, angiogenesis and the wound-healing response10 which are associated with rapid growth kinetics and early radiological tumour regrowth prior to commencement of chemoradiotherapy in some ndGBM patients.13 14 Earlier systemic treatment prior to radiotherapy may therefore be useful.
Prolonged additional (5-day schedule every 28 days) cycles of TMZ in the adjuvant setting are also commonly prescribed by clinicians following completion of the planned six cycles of therapy, but with conflicting evidence for this practice.15 Past studies have suggested a possible benefit, but in heavily selected populations.15 16 Testing the hypothesis of prolonged adjuvant TMZ also has high relevance to people with GBM, given the poor overall prognosis with standard approach. Real-world analyses of prescribing patterns indicate that many oncologists continue TMZ beyond six cycles.17
Testing ideas in a rare disease setting can be facilitated by novel trial designs. Multi-Arm GlioblastoMa Australasia (MAGMA) is a multiarm randomised clinical trial incorporating innovations in conduct and design for people affected by ndGBM. The initial two interventions addressed by MAGMA will assess alternative schedules of TMZ dosing. A future transition to a multiarm adaptive trial design is planned. This will permit closure of interventions that do not demonstrate sufficient interim efficacy and addition of new study interventions, thus minimising the number of patients treated on the control regimen. The rationale for this study design will allow rapid testing of new ideas in GBM, a concept that has had success in other tumour types, most notably in the STAMPEDE trial for patients with newly diagnosed metastatic prostate cancer.18
Intervention 1: ‘neoadjuvant’ chemotherapy
Delayed time to initiation of systemic therapy is associated with worse outcome in many cancers.19–21 In ndGBM, delays beyond 6 weeks between primary surgery and starting radiation are associated with inferior survival,22 with another study suggesting the risk of death increases by 2% for each day of waiting for radiotherapy to commence.23 Commencing radiotherapy immediately after surgery may not be feasible for a range of clinical and technical reasons. Several studies have shown evidence for improved outcomes from initiating TMZ chemotherapy before chemoradiotherapy. In a single-arm study, neoadjuvant TMZ (75 mg/m2 daily) started 2–3 weeks after surgery but prior to hypofractionated chemoradiation (n=50) demonstrated median OS of 22.3 months in a single arm compared with the expected 14.6 months with standard regimens,24 25 with no unexpected additional toxicity (table 1). A randomised phase II study (n=99) of neoadjuvant TMZ vs standard TMZ started 2 weeks postoperatively (75 mg/m2 daily) for 2 weeks prior to standard chemoradiation26 showed median OS in the neoadjuvant group of 17.6 months, compared with 13.2 months in the standard TMZ control group (log-rank test p=0.021), with comparable adverse events, though such a study was not powered for survival comparisons. Finally, a small pilot feasibility study showed that a single additional cycle of 5 days of 200 mg/m2 TMZ given in the 4-week interval from surgery to standard chemoradiation was safe, feasible and associated with 71% overall survival rate at 18 months.27 Conversely the clinical efficacy of TMZ administered prior to surgery,28 or prolonged TMZ administered prior to and delaying chemoradiation29 has not demonstrated efficacy. However, there have been no randomised trials demonstrating the efficacy of neoadjuvant chemotherapy compared with the current standard of care, therefore, this experimental arm of MAGMA seeks to answer this question.
Table 1.
Comparison of median OS duration in previous studies of ‘neoadjuvant’ TMZ
| Publication | OS (control)/months | OS (early TMZ) /months | No patients in experimental arm | MGMT methylated (%) | Randomised—R; non-randomised—NR | Study design |
| Shenouda24 25 | 22.3 | 50 | 42 | NR | Start TMZ 3–4 weeks postsurgery for 2 weeks | |
| Chaskis27 | OS 71.3% at 18 months | 12 | 66 | NR | Start TMZ 12 days after surgery for 5 days then 12 days until starting RT | |
| Mao26 | 13.2 | 17.6 | 99 | 39 | R | Start TMZ 2 weeks postsurgery for 2 weeks |
MGMT, O(6)-methylguanine-DNA methyltransferase; OS, overall survival; TMZ, temozolomide.
Intervention 2: prolonged adjuvant chemotherapy
Some oncologists have continued TMZ beyond 6 months in patients with ndGBM where disease is clinically and radiologically stable.16 17 Selection pressures resulting from surgery, radiation and chemotherapy influence cancer cell populations.30 Radiation and TMZ can cause branched evolution of cancer cells because of their mutagenic actions,31 leading to greater genomic diversity on tumour progression. Continuous or prolonged TMZ treatment is hypothesised to suppress this process. However, paradoxically, this might also lead to hypermutation,32 therefore, prospective randomised evaluation of prolonged TMZ is essential.
In a meta-analysis33 of retrospective comparative studies (n=396) from six studies that had met all inclusion and exclusion criteria and showed no significant heterogeneity or publication bias, prolonged adjuvant TMZ (5-day schedule with 5 days treatment followed by 23 days off treatment in a 28-day cycle) was associated with increased OS (HR 2.39 for standard arm relative to prolonged TMZ arm, 95% CI 1.82 to 3.14) and increased progression-free survival (PFS) (HR 2.12, 95% CI 1.56 to 2.89).
Another meta-analysis identified seven studies encompassing 1018 patients.34 OS was higher in patients taking greater than six cycles TMZ compared with the control (six cycles TMZ; p=0.018, 1.0–10.5 months). PFS followed a similar trend (p<0.001, 2.6–7.9 months).
In the first randomised phase II study (n=40), patients with ndGBM were randomised to EORTC/Stupp chemoradiation with either the conventional six (C-TMZ arm) or extended 12 cycles (E-TMZ arm) of adjuvant TMZ.35 The median number of adjuvant treatment cycles was 6 and 12, respectively. Median PFS was 12.8 and 16.8 months respectively (p=0.069), while the median OS was 15.4 vs 23.8 months in the C-TMZ and E-TMZ arms respectively (p=0.044). Five per cent and 15% patients, respectively, experienced haematological toxicity≥G3. Conversely, the recently reported phase II GEINO 14–01 study36 used a randomised non-comparative design to evaluate patients (n=159) with ndGBM who either continued or discontinued TMZ after the first six cycles of standard first-line treatment and found 6-month PFS rates of 61.3% and 55.7%, respectively. There were study limitations including an excess of IDH1 mutant patients randomised to the control arm which the MAGMA study will address by making IDH mutation a stratification factor. The WHO 2016 classification of GBM has been adopted for MAGMA,37 but future protocol updates will address the integration of molecular information into GBM diagnostics.38 A summary of previous studies examining the effect of prolonged TMZ is shown in figure 1.
Figure 1.
Comparison of median OS in retrospective studies of prolonged (>6 months) adjuvant phase temozolomide (adapted from published data33 34). OS, overall survival.
In patients with ndGBM, does the addition of neoadjuvant TMZ (prior to commencement of radiotherapy) or extended TMZ (given for 12 months or until progression/toxicity) improve overall survival compared with concurrent and adjuvant TMZ for 6 months given according to the Stupp/EORTC regimen?
Methods and analysis
Consortium governance
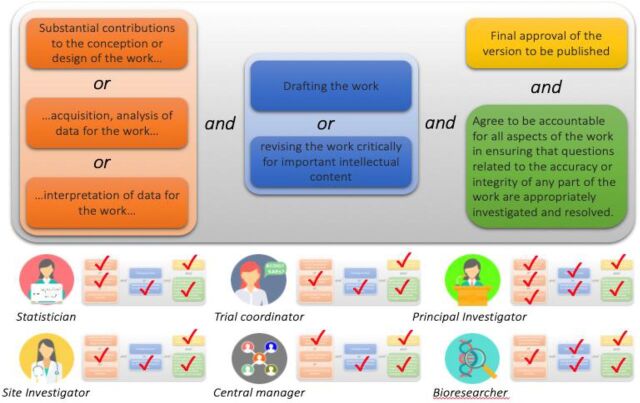
MAGMA is a collaboration between the Cooperative Trials Group for Neuro-Oncology (COGNO) and the National Health and Medical Research Council Clinical Trials Centre, University of Sydney. Funding applications are in process to extend MAGMA to sites in New Zealand. MAGMA will be established with Consortium governance, to respect and recognise the efforts of staff at central and study sites. Consortium social structures are common in other fields of science, and becoming more common in clinical research, as the requirements for teamwork and collaboration lend themselves to this structure, and academic authorship can be justified for all central and site study staff (figure 2).39
Figure 2.
The International Committee of Medical Journal Editors (ICJME) criteria for authorship can be authentically met by most if not all healthcare professionals contributing to clinical trial conduct, as they can be shown to have met the contributions outlined above. An example of a consortium model for research is found in the multiarm, multistage STAMPEDE trial for prostate cancer.47
A part of the Consortium Governance model, regular meetings are scheduled between site investigators and COGNO to facilitate real-time monitoring of trial conduct, thus mitigating the risk of factors that may negatively affect trial recruitment. These include, but are not limited to, the risk that postoperative complications may affect the likelihood of referral within a satisfactory time frame for trial participation.
Study design
The initial two hypotheses in MAGMA will be tested in a factorial design with patients choosing whether to opt-in to being randomised to one or both interventions. This will enable two study interventions to be addressed in a single clinical trial. The design element allowing optional participation in each study intervention (rather than creating a separate clinical trial) is intended to streamline the recruitment process by minimising additional study procedures and allowing patients to participate only in the study interventions they have chosen to participate in, omitting study interventions that may not be feasible for pragmatic reasons such as postoperative recovery. Under this trial design, patients who are randomised to standard-of-care treatment will represent a common control arm and be compared against each intervention separately. Participants randomised to both interventions will be used to check for the interaction between neoadjuvant and extended TMZ in their effects on survival. TMZ is well tolerated; accordingly, there are no interim analyses planned but the study will be overseen by an independent data and safety monitoring committee. Future study interventions may incorporate interim analyses for efficacy and/or futility if required. While serious adverse reactions will be carefully monitored throughout the study, recording and reporting of low-grade toxicity is not requested of sites in order to reduce study costs and site time commitments. In keeping with the pragmatic design elements of MAGMA, the study is designed to reflect real-world practice as closely as possible. An example of this is the planned short course radiotherapy regimen (40 Gy in 15# over 3 weeks), which will be considered at the investigator’s discretion in patients >65 years old or those with a poor performance status. Screening and recruitment for MAGMA commenced in Australia in September 2020. Recruitment to the two initial interventions of MAGMA is expected to continue until September 2023.
In the MAGMA study, randomisation #2 will occur at any time from registration until the start of adjuvant TMZ, in contrast to most of the studies noted above, including the GEINO 14–01 trial,36 in which randomisation occurred only for patients who had not progressed after six cycles of adjuvant treatment. All patients in MAGMA participating in the ‘prolonged’ treatment randomisation will also be stratified both by IDH-mutation status and MGMT methylation status. If treatment delays are encountered due to delayed chemotherapy cycles, then the full planned course of chemotherapy will be administered.
The study philosophy allows future interventions to be incrementally added to the trial platform. New prospective interventions will be developed by the MAGMA Consortium and be implemented as protocol amendments. The current study schema is described in more detail under study interventions and shown in figure 3.
Figure 3.
MAGMA study schema showing randomisation for the initial two interventions: (1) early postoperative temozolomide (TMZ) versus standard chemoradiotherapy (2) extended vs 6 months adjuvant TMZ. Treatment allocation to each intervention will be balanced (1:1) using minimisation over several clinically important stratification factors (listed in box 2). MAGMA, Multi-Arm GlioblastoMa Australasia.
Eligibility
The inclusion and exclusion criteria for the study are listed in box 1. The criteria are pragmatic and reflect the population of patients offered chemoradiotherapy in routine practice including an option for hypofractionated radiotherapy when appropriate. Despite these inclusive criteria, we acknowledge that a proportion of people with ndGBM still may not meet these requirements.40
Box 1. Inclusion and exclusion criteria.
Inclusion criteria
Adults, aged 18 years and older, with newly diagnosed histologically confirmed WHO grade IV glioblastoma (GBM) (as per 2016 Central Nervous System WHO classification) or glioma with molecular features of GBM (as per cIMPACT-NOW Update 3).
Adequate recovery from surgical resection.
Eastern Cooperative Oncology Group (ECOG) performance status of 0–2.
Previous surgery for a low-grade glioma is allowed if there was no radiation or chemotherapy administered at that time.
Adequate bone marrow function (Platelets ≥100 × 109 /L, Absolute neutrophil count ≥1.5 × 109/L).
Adequate liver function (ALT/AST <3 × ULN).
Adequate renal function (creatinine clearance >30 mL/min).
Willing and able to comply with all study requirements, including treatment, timing and nature of required assessments.
Signed, written informed consent.
Exclusion criteria
Recurrence of GBM.
Comorbidities considered to provide a safety concern for use of temozolomide (TMZ).
Other contraindications to TMZ Cranial irradiation within 2 years prior to registration.
Other comorbidities or conditions that may compromise assessment of key outcomes.
History of another malignancy within 2 years prior to registration. Patients with adequately treated carcinoma in situ of the prostate, breast or cervix, melanoma in situ, basal cell carcinoma of the skin, squamous cell carcinoma of the skin, non-muscle invasive transitional cell carcinoma of the bladder or low-grade prostate cancer not requiring treatment (International Society of Urological Pathology 1; Gleason grade ≤6) may be included in this study.
Concurrent illness, including severe or chronic bacterial or viral infection that may jeopardise the ability of the patient to undergo the procedures outlined in this protocol with reasonable safety.
Presence of any psychological, familial, sociological or geographical condition potentially hampering compliance with the study protocol and follow-up schedule.
Pregnancy, lactation or inadequate contraception.
Study interventions
Patients deemed suitable to undergo standard treatment for ndGBM will be offered study participation from up to 30 metropolitan and regional hospitals around Australia. Consenting participants will be randomly allocated to treatment with opt-in randomisation to each study intervention to enable flexibility if they are recruited to the study after randomisation to the first intervention has occurred, or if the participant or their physician specifically choose not to participate in a particular randomisation. The interventions being offered within the MAGMA platform will include neoadjuvant chemotherapy given as soon as possible after surgery prior to the commencement of concurrent chemoradiotherapy (intervention 1; neoadjuvant chemotherapy) and prolonged chemotherapy, given until progression or toxicity during the adjuvant phase of TMZ (intervention 2: prolonged adjuvant chemotherapy). In each case, the randomisation will occur against the standard European Organisation for Research and Treatment of Cancer (EORTC)/Stupp regimen. Randomisation will be performed centrally using a web-based system that communicates with the study database. Allocation will use the method of minimisation separately for each study intervention, and allocation concealment maintained by treatment allocation not being revealed until after patient enrolment and consent details are entered into the study database. Treatment allocation to each intervention will be balanced (1:1) using minimisation over several clinically important stratification factors (listed in box 2). The study is not blinded, so once treatment has been allocated, the treating physician and patient will be informed.
Box 2. Stratification factors for the two initial Multi-Arm GlioblastoMa Australasia treatment interventions.
Stratification factors for first treatment intervention (neoadjuvant chemotherapy):
Duration between surgery and randomisation (≤14 days vs >14 days).
Study site.
Age at registration (<65 years vs ≥65 years).
IDH mutation status (by positive IDH immunohistochemistry) performed at clinical sites in real time according to accepted local methods and pathways.
Extent of surgery (gross macroscopic resection vs subtotal resection or biopsy).
Stratification factors for second treatment intervention (prolonged adjuvant chemotherapy)
As per first treatment intervention (neoadjuvant chemotherapy) PLUS
Treatment arm allocated for first intervention.
MGMT promoter methylation status (not expected to be available prior to randomisation to the first intervention).
Neoadjuvant TMZ will be administered as soon as possible post-operatively at least 1 week or more prior to starting chemoradiotherapy. TMZ will be administered at a dose of 75 mg/m2. Concomitant use of additional cytotoxic chemotherapy, immunotherapy, antiangiogenic agents and other investigational agents is prohibited.
Radiotherapy and concurrent TMZ should commence ideally within 4–6 weeks from the date of surgery up to a maximum of 7 weeks and 3 days. Radiotherapy is standard of care and can consist of a conventionally fractionated approach delivering 60 Gy in 30 fractions (#) over 6 weeks2 or a hypofractionated approach delivering 40 Gy in 15# over 3 weeks. The latter is preferred for elderly patients or those with an ECOG performance status of 2.41 Radiotherapy treatment details are described in online supplemental appendix 1.
bmjopen-2021-058107supp001.pdf (245KB, pdf)
Extended adjuvant TMZ given beyond 6 months will be administered according to the same schedule given during the first six cycles, that is, 150–200 mg/m2 (days 1–5 every 28 days). Guidance for dose modifications due to chemotherapy toxicity will be standardised using published guidelines. MGMT methylation status will be performed on all patients, using the cut-offs of >9% methylated<=9% unmethylated. Prior MGMT methylation results from NATA-accredited laboratories (central or peripheral) will be allowed. Patients will not be randomised onto the second treatment intervention until their MGMT methylation status has been determined, however, it is expected that they will be randomised to the first intervention as early as possible. All patients will be randomised prior to starting the first cycle of adjuvant chemotherapy in order to minimise any selection bias, whereby patients with poorer performance status may be offered only 6 months of therapy. In patients with unknown MGMT status will be stratified as methylated.
The overall study schema is shown in figure 3.
Outcome measures and assessments
Time-to-event measures are defined as the interval between the date of initial surgery and the date of the event, with censoring at last follow-up if the event has not occurred. The date of initial surgery has been chosen as the starting point for time-to-event measures due to the potential difference in timing of randomisation to each of the study interventions, and to facilitate comparisons with published data (Box 3). Radiological response will be defined in the study protocol by investigator-measured modified RANO criteria.42 The time to first treatment for recurrent disease is defined as the interval between the date of initial surgery and the date of first treatment (eg, reresection, reirradiation, second-line chemotherapy or another clinical trial treatment) or death from any cause, whichever occurs first, with censoring at last follow-up if alive with no treatment for recurrent disease.
Toxicity will be defined according to National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events version 5.0. Minor toxicity (grade 1–2) is not recorded for the initial two study interventions as the tolerance of TMZ in routine care is well understood; TMZ has been administered in the GBM setting for over two decades. Grade 3 or 4 adverse events will be recorded, and their relation to treatment will be discussed centrally. Health-related quality of life will be reported by participants using the EORTC QLQ C-30, BN-20 and the EQ-5D-5L (EuroQol 5 dimensions) instruments. Health economic evaluation will be performed through cost–utility analysis with the EQ-5D as the primary analysis, and the EORTC QLU-C10D instrument as a sensitivity analysis. The EQ-5D will calculated using the Australian value set for the EQ-5D. The EORTC QLU-C10D utility scores will be calculated from patients’ responses to the cancer-specific quality-of-life questionnaire, EORTC QLQ-C30 using the Australian value set for the EORTC QLU-C10D.43 44
Assessments will be performed according to the schedule shown in table 2.
Table 2.
Schedule of assessments for the MAGMA trial, showing clinical, radiological, translational research and QOL assessments
| Study treatments and duration | Neoadjuvant treatment (if applicable) 
|
Concurrent treatment
|
Break
|
Adjuvant treatment
|
Follow-up
|
|||
| At least 1 week | 3–6 weeks | About 4 weeks | Min 6 months | |||||
| Timing of randomisation | Randomisation #1 (recommended to be at least 1 week before CRT start) 
|
|||||||
| Randomisation #2 (any time from registration to the start of adjuvant treatment) 
| ||||||||
| Assessment time points | Screening | Optional randomisation to individual treatment interventions (as soon as practical after registration) |
Start of CRT (as soon as practical after registration) |
4 weeks (±7 days) after start of CRT | 4 weeks (±7 days) after completion of CRT | During adjuvant treatment (every 12 weeks±7 days) | Follow-up (every 12 weeks±7 days) |
|
| Clinical assessments | X | X* | X | X | X | |||
| Concomitant medications | X | X* | X | X | X | |||
| Serious adverse Events† | X* | X | X | X | ||||
| Blood tests | X | X* | X | X | X | |||
| MRI brain (or CT brain if unable to undergo MRI) | X‡ | X | X | X | ||||
| HRQoL | X | X | X | X | X | |||
| Blood for translational research | X | |||||||
| Patient survival status | X | |||||||
Randomisation #1 is for neoadjuvant chemotherapy while randomisation #2 is for extended (>6 cycles) chemotherapy.
*If less than 1 week between registration and start of CRT, this does not need to be repeated.
†Adverse events captured until 30 days after completion of all study treatments. Only grade 3–4 events will be recorded.
‡All patients require a postoperative MRI brain (recommended but not mandated <72 hour postoperative) prior to the start of CRT. Study-related procedures/assessments are shown in orange, standard of care assessments in green, demonstrating the pragmatic follow-up schedule for the trial.
CRT, chemoradiotherapy; HRQoL, health-related quality of life; MAGMA, Multi-Arm GlioblastoMa Australasia; QOL, quality of life.
Box 3. Outcome measures, endpoints and other measures.
Primary outcome measure
Overall survival.
Secondary outcome measures
Progression-free survival.
Time to first treatment for recurrent disease.
Serious adverse events (particularly grade 3–4 temozolomide adverse events).
Health-related quality of life.
Tertiary outcome measures
Correlative outcomes: predictive or prognostic biomarkers.
Health economic outcomes: health utilities, incremental cost-effectiveness ratio.
Patient and public involvement
Patients were involved in the design and conduct of this research. In particular, feedback was sought from a panel of consumer representatives during the design of novel video-based patient and information and consent forms to facilitate a patient-centred approach to informed consent. During the trial, a consumer representative joined the trial management committee (TMC). To identify the most relevant research topics for future arms of the study, a formal process for appraisal of scientific concepts by consumers has been developed as concepts are formulated into specific research interventions.
Interim analysis
The treatments for the two initial interventions have been well tolerated in prior studies and no formal interim analyses are planned for treatment interventions 1 and 2, however, the TMC will meet regularly to review safety and efficacy data. For future interventions, interim analyses may be performed using the primary endpoint, or suitable intermediate endpoints to examine early signals of lack of benefit and/or efficacy. Based on consideration of multiple factors, the TMC will formulate recommendations regarding modifications to the study design.
Statistical design
Sample size estimate
The anticipated recruitment for the initial two interventions, with 3 years of accrual and 18 months of follow-up (median follow-up of 3 years), has been calculated as a sample size of at least 125 patients per treatment (250 randomised patients for each intervention, 200 observed events). This will give 80% power at two-sided alpha of 5% to detect a 33% reduction in death rate (HR 0.667), corresponding to an increase in median survival from 12 to 18 months), using the method described in Machin et al.45 The estimated reduction in death rate is based on previously conducted phase II studies.25 26 The study plan is to recruit a total of at least 300 patients, with scope to expand the sample size dependent on budget and additional study interventions being approved by the TMC.
Statistical analysis
All study data will be collected via electronic case report forms with routine and regular review of data entry fields for completeness and accuracy. Every 3 months, the TMC will receive data exports of serious adverse events and recruitment while data exports will occur to the independent safety data monitoring Committee on a regular basis.
A detailed statistical analysis plan will be prepared prior to locking the study database. Participant demographic, clinical and treatment characteristics will be described using frequencies and percentages for categorical variables, mean and range or median and range for continuous variables and the Kaplan-Meier method for time-to-event variables. The primary analysis of overall survival will be performed according to the intention to treat principle on all patients randomised to each study intervention using log-rank tests, and the HR for each intervention described with 95% CI from unadjusted proportional hazards regression models. These analyses will be performed separately for each study intervention. In participants randomised to both study interventions, a proportional hazards regression model will test for interaction between the two randomised treatments in their effects on overall survival. Categorical outcomes will be compared using the χ2 test, continuous outcomes will be compared using the t-test or a non-parametric equivalent while survival outcomes will use the log-rank test. Adjusted analyses and subgroup analyses will use logistic, linear or proportional hazards regression models.
The TMC will assist in developing additional interventions based on the proposed study outcome measurements and types of treatment under consideration (guidance document available on request). The COGNO Scientific Advisory Committee will provide governance and approval of additional interventions. Future treatments may be added to the existing two interventions in a factorial arrangement or be added as separate interventions with a common control arm if comparable outcome measures are proposed. Optional randomisation and interim analyses may be incorporated if appropriate. The MAGMA statistical design uses a partial factorial design for simplicity; adding multiple arms will be enabled by transition to a formal MAMS design.46 Proposed future arms include hypotheses such as drug repurposing or perioperative and radiation dosing questions. A formal statistical analysis plan will be formulated according to the additional proposed future arms.
Ethics and dissemination
The MAGMA study was approved by the lead site, Royal Prince Alfred Hospital Research Ethics and Governance Office Committee. HREA (Version 4, 12 February 2020), Protocol (Version 1.1, 20 November 2019). Protocol No. X19-0419 and 2019/ETH13297. Other clinical sites will provide oversight through local governance processes, including obtaining informed consent from suitable participants. Any substantial amendments to the study protocol will be reported to the lead site ethics committee for approval prior to implementation and updated on the trial registry, with study investigators being advised in writing. The study will be conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice. Results will be disseminated using a range of media channels and peer-reviewed publications.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the contributions of the MAGMA Consortium (online supplemental appendix 2). We acknowledge the assistance of Professor Emerita Madeleine King in refining health economic outcomes for the trial and in review of the protocol manuscript. Icons used in 2 and 3 thanks to https://www.flaticon.com/authors/icon-pond
Footnotes
Collaborators: See online supplemental material.
Contributors: H-WS, BK, EHB, AKN, EJH, RJ, RH, JP, HG, MBP, SY, MH, ET, CC, E-SK, JS and CG conceived the concept. BK and CG wrote drafts of the manuscript. H-WS, EHB, AKN, EJH, RJ, RH, HG, MBP, SY, MH, ET, AD, ZL, E-SK, JS and CG critically reviewed the manuscript.
Funding: This work is supported by the Medical Research Future Fund (MRFF) Rare Cancers Rare Diseases, Unmet Need Grant MRF1170193. Funding for the MAGMA trial is administered by MRFF, from the Australian Brain Cancer Mission of Cancer Australia, co-funded by Carrie’s Beanies for Brain Cancer (https://www.carriesbeanies4braincancer.com/) and the Mark Hughes Foundation (https://markhughesfoundation.com.au/).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Welfare AIfHa . Cancer in Australia 2021 [cited Australian Institute for Health and Welfare. Available: https://www.aihw.gov.au/reports/cancer/cancer-in-australia-2021/summary
- 2. Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005;352:987–96. 10.1056/NEJMoa043330 [DOI] [PubMed] [Google Scholar]
- 3. Stupp R, Wong ET, Kanner AA, et al. NovoTTF-100A versus physician's choice chemotherapy in recurrent glioblastoma: a randomised phase III trial of a novel treatment modality. Eur J Cancer 2012;48:2192–202. 10.1016/j.ejca.2012.04.011 [DOI] [PubMed] [Google Scholar]
- 4. Reardon DA, Lassman AB, van den Bent M, et al. Efficacy and safety results of ABT-414 in combination with radiation and temozolomide in newly diagnosed glioblastoma. Neuro Oncol 2017;19:965–75. 10.1093/neuonc/now257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bristol-Myers. Squibb Announces Phase 3 CheckMate-498 Study Did Not Meet Primary Endpoint of Overall Survival with Opdivo (nivolumab) Plus Radiation in Patients with Newly Diagnosed MGMT-Unmethylated Glioblastoma Multiforme [Press Release]. [press release, 2019. [Google Scholar]
- 6. Lee SY. Temozolomide resistance in glioblastoma multiforme. Genes Dis 2016;3:198–210. 10.1016/j.gendis.2016.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lassman AB, Joanta-Gomez AE, Pan PC, et al. Current usage of tumor treating fields for glioblastoma. Neurooncol Adv 2020;2:vdaa069. 10.1093/noajnl/vdaa069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu Y, Strawderman MS, Warren KT, et al. Clinical efficacy of tumor treating fields for newly diagnosed glioblastoma. Anticancer Res 2020;40:5801–6. 10.21873/anticanres.14597 [DOI] [PubMed] [Google Scholar]
- 9. Strik HM, Marosi C, Kaina B, et al. Temozolomide dosing regimens for glioma patients. Curr Neurol Neurosci Rep 2012;12:286–93. 10.1007/s11910-012-0262-y [DOI] [PubMed] [Google Scholar]
- 10. Fan C-H, Liu W-L, Cao H, et al. O6-Methylguanine DNA methyltransferase as a promising target for the treatment of temozolomide-resistant gliomas. Cell Death Dis 2013;4:e876. 10.1038/cddis.2013.388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sanai N, Polley M-Y, McDermott MW, et al. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 2011;115:3–8. 10.3171/2011.2.JNS10998 [DOI] [PubMed] [Google Scholar]
- 12. Dix AR, Brooks WH, Roszman TL, et al. Immune defects observed in patients with primary malignant brain tumors. J Neuroimmunol 1999;100:216–32. 10.1016/S0165-5728(99)00203-9 [DOI] [PubMed] [Google Scholar]
- 13. Stensjøen AL, Solheim O, Kvistad KA, et al. Growth dynamics of untreated glioblastomas in vivo. Neuro Oncol 2015;17:1402–11. 10.1093/neuonc/nov029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pirzkall A, McGue C, Saraswathy S, et al. Tumor regrowth between surgery and initiation of adjuvant therapy in patients with newly diagnosed glioblastoma. Neuro Oncol 2009;11:842–52. 10.1215/15228517-2009-005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blumenthal DT, Gorlia T, Gilbert MR. Is more better? the impact of extended adjuvant temozolomide in newly diagnosed glioblastoma: a secondary analysis of EORTC and NRG Oncology/RTOG. Neuro Oncol 2017. 10.1093/neuonc/nox025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen S, Visintini S. Extended dosing (12 cycles) of adjuvant temozolomide in adults with newly diagnosed high grade gliomas: a review of clinical effectiveness, cost-effectiveness, and guidelines. CADTH rapid response reports. Ottawa, 2018. [PubMed] [Google Scholar]
- 17. Balañá C, Vaz MA, Lopez D, et al. Should we continue temozolomide beyond six cycles in the adjuvant treatment of glioblastoma without an evidence of clinical benefit? A cost analysis based on prescribing patterns in Spain. Clin Transl Oncol 2014;16:273–9. 10.1007/s12094-013-1068-3 [DOI] [PubMed] [Google Scholar]
- 18. James ND, Sydes MR, Clarke NW, et al. STAMPEDE: systemic therapy for advancing or metastatic prostate cancer — a Multi-Arm multi-stage randomised controlled trial. Clin Oncol 2008;20:577–81. 10.1016/j.clon.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 19. Colleoni M, Gelber RD. Time to initiation of adjuvant chemotherapy for early breast cancer and outcome: the earlier, the better? J Clin Oncol 2014;32:717–9. 10.1200/JCO.2013.54.3942 [DOI] [PubMed] [Google Scholar]
- 20. Kim HW, Lee J-C, Lee J, et al. Early versus delayed initiation of adjuvant treatment for pancreatic cancer. PLoS One 2017;12:e0173960. 10.1371/journal.pone.0173960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mahner S, Eulenburg C, Staehle A, et al. Prognostic impact of the time interval between surgery and chemotherapy in advanced ovarian cancer: analysis of prospective randomised phase III trials. Eur J Cancer 2013;49:142–9. 10.1016/j.ejca.2012.07.023 [DOI] [PubMed] [Google Scholar]
- 22. Spratt DE, Folkert M, Zumsteg ZS, et al. Temporal relationship of post-operative radiotherapy with temozolomide and oncologic outcome for glioblastoma. J Neurooncol 2014;116:357–63. 10.1007/s11060-013-1302-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Do V, Gebski V, Barton MB. The effect of waiting for radiotherapy for grade III/IV gliomas. Radiother Oncol 2000;57:131–6. 10.1016/S0167-8140(00)00257-7 [DOI] [PubMed] [Google Scholar]
- 24. Shenouda G, Souhami L, Petrecca K, et al. A phase 2 trial of neoadjuvant temozolomide followed by Hypofractionated accelerated radiation therapy with concurrent and adjuvant temozolomide for patients with glioblastoma. Int J Radiat Oncol Biol Phys 2017;97:487–94. 10.1016/j.ijrobp.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 25. Shenouda G, Souhami L, Petrecca K, et al. A phase 2 trial of neoadjuvant temozolomide (TMZ) followed by accelerated Hypofractionated radiation therapy (AHRT) and TMZ followed by adjuvant TMZ in patients with newly diagnosed glioblastoma (GBM): long term survival and toxicity analysis. Int J Radiat Oncol Biol Phys 2018;102:S48–9. 10.1016/j.ijrobp.2018.06.096 [DOI] [Google Scholar]
- 26. Mao Y, Yao Y, Zhang L-W, et al. Does early postsurgical temozolomide plus concomitant radiochemotherapy regimen have any benefit in Newly-diagnosed glioblastoma patients? A multi-center, randomized, parallel, open-label, phase II clinical trial. Chin Med J 2015;128:2751–8. 10.4103/0366-6999.167313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chaskis E, Luce S, Goldman S, et al. [Early postsurgical temozolomide treatment in newly diagnosed bad prognosis glioblastoma patients: Feasibility study]. Bull Cancer 2018;105:664–70. 10.1016/j.bulcan.2018.05.006 [DOI] [PubMed] [Google Scholar]
- 28. Jiang H, Zeng W, Ren X, et al. Super-early initiation of temozolomide prolongs the survival of glioblastoma patients without gross-total resection: a retrospective cohort study. J Neurooncol 2019;144:127–35. 10.1007/s11060-019-03211-1 [DOI] [PubMed] [Google Scholar]
- 29. Malmström A, Poulsen HS, Grønberg BH, et al. Postoperative neoadjuvant temozolomide before radiotherapy versus standard radiotherapy in patients 60 years or younger with anaplastic astrocytoma or glioblastoma: a randomized trial. Acta Oncol 2017;56:1776–85. 10.1080/0284186X.2017.1332780 [DOI] [PubMed] [Google Scholar]
- 30. McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell 2017;168:613–28. 10.1016/j.cell.2017.01.018 [DOI] [PubMed] [Google Scholar]
- 31. Orzan F, De Bacco F, Crisafulli G, et al. Genetic evolution of glioblastoma stem-like cells from primary to recurrent tumor. Stem Cells 2017;35:2218–28. 10.1002/stem.2703 [DOI] [PubMed] [Google Scholar]
- 32. Daniel P, Sabri S, Chaddad A, et al. Temozolomide induced hypermutation in glioma: evolutionary mechanisms and therapeutic opportunities. Front Oncol 2019;9:41. 10.3389/fonc.2019.00041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Xu W, Li T, Gao L, et al. Efficacy and safety of long-term therapy for high-grade glioma with temozolomide: a meta-analysis. Oncotarget 2017;8:51758–65. 10.18632/oncotarget.17401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Alimohammadi E, Bagheri SR, Taheri S, et al. The impact of extended adjuvant temozolomide in newly diagnosed glioblastoma multiforme: a meta-analysis and systematic review. Oncol Rev 2020;14:461. 10.4081/oncol.2020.461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bhandari M, Gandhi AK, Devnani B, et al. Comparative study of adjuvant temozolomide six cycles versus extended 12 cycles in newly diagnosed glioblastoma multiforme. J Clin Diagn Res 2017;11:XC04–8. 10.7860/JCDR/2017/27611.9945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Balana C, Vaz MA, Manuel Sepúlveda J, et al. A phase II randomized, multicenter, open-label trial of continuing adjuvant temozolomide beyond 6 cycles in patients with glioblastoma (GEINO 14-01). Neuro Oncol 2020;22:1851–61. 10.1093/neuonc/noaa107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 2016;131:803–20. 10.1007/s00401-016-1545-1 [DOI] [PubMed] [Google Scholar]
- 38. Louis DN, Perry A, Wesseling P, et al. The 2021 who classification of tumors of the central nervous system: a summary. Neuro Oncol 2021;23:1231–51. 10.1093/neuonc/noab106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. ICMJE . Icmje recommendations defining the role of authors and contributors, 2020. Available: http://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html
- 40. Prestwich RJ, Sivapalasunrtharam A, Johnston C, et al. Survival in high-grade glioma: a study of survival in patients unfit for or declining radiotherapy. Clin Oncol 2005;17:133–7. 10.1016/j.clon.2004.08.006 [DOI] [PubMed] [Google Scholar]
- 41. Perry JR, Laperriere N, O'Callaghan CJ, et al. Short-Course radiation plus temozolomide in elderly patients with glioblastoma. N Engl J Med 2017;376:1027–37. 10.1056/NEJMoa1611977 [DOI] [PubMed] [Google Scholar]
- 42. Ellingson BM, Wen PY, Cloughesy TF. Modified criteria for radiographic response assessment in glioblastoma clinical trials. Neurotherapeutics 2017;14:307–20. 10.1007/s13311-016-0507-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. King MT, Viney R, Simon Pickard A, et al. Australian utility weights for the EORTC QLU-C10D, a Multi-Attribute utility instrument derived from the cancer-specific quality of life questionnaire, EORTC QLQ-C30. Pharmacoeconomics 2018;36:225–38. 10.1007/s40273-017-0582-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Viney R, Norman R, Brazier J, et al. An Australian discrete choice experiment to value eq-5d health states. Health Econ 2014;23:729–42. 10.1002/hec.2953 [DOI] [PubMed] [Google Scholar]
- 45. Machin D, Cheung YB, Parmar MKB. Survival Analysis: A Practical Approach. In: Wiley J, Sons L, eds. 2Nd, 2006. [Google Scholar]
- 46. Sydes MR, Parmar MKB, Mason MD, et al. Flexible trial design in practice - stopping arms for lack-of-benefit and adding research arms mid-trial in STAMPEDE: a multi-arm multi-stage randomized controlled trial. Trials 2012;13:168. 10.1186/1745-6215-13-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. James ND, de Bono JS, Spears MR, et al. Abiraterone for prostate cancer not previously treated with hormone therapy. N Engl J Med 2017;377:338–51. 10.1056/NEJMoa1702900 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058107supp001.pdf (245KB, pdf)