Abstract
Aims
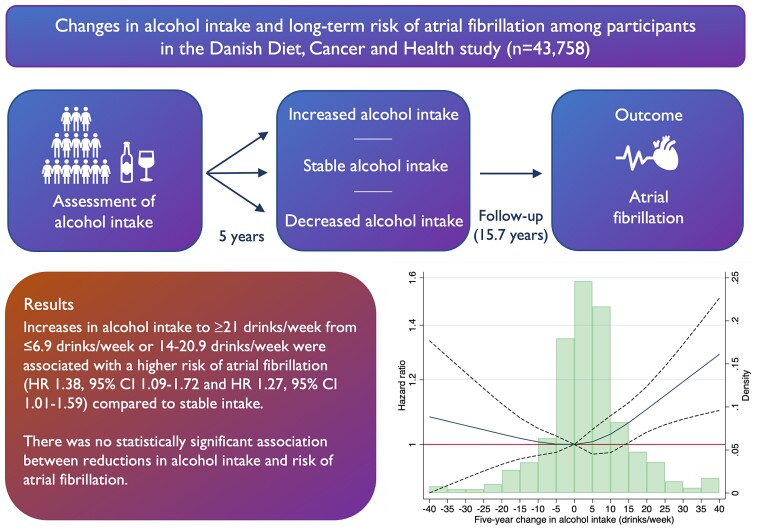
Alcohol intake is a well-established risk factor for atrial fibrillation (AF). However, evidence on the effects of changes in alcohol intake to primary AF prevention is sparse. The aim of this study was to examine the association between 5-year changes in alcohol intake and the risk of incident AF.
Methods and results
This study was based on the Danish cohort study Diet, Cancer and Health. Lifestyle factors were assessed using questionnaires at a recruitment research examination and a second examination 5 years later. Diagnoses of AF and comorbidities were retrieved from the Danish National Patient Registry. 43 758 participants without prior AF were included. The median age was 61 (25th–75th percentile 58–66) years and 54% were female. Over a median follow-up time of 15.7 years, 5312 participants had incident AF (incidence rate 8.6/1000 person-years). Compared with stable intake, increases in alcohol intake to ≥21 drinks/week from ≤6.9 drinks/week (HR: 1.38, 95% CI: 1.09–1.72) or 14–20.9 drinks/week (HR: 1.27, 95% CI: 1.01–1.59) at baseline were associated with a higher risk of AF. In contrast, we did not observe a statistically significant association between reductions in alcohol intake and the risk of AF.
Conclusion
A 5-year increase in alcohol intake was associated with a greater risk of AF compared with a stable low/moderate intake.
Keywords: Alcohol, Atrial Fibrillation, Lifestyle, Prevention, cohort
Graphical Abstract
Graphical Abstract.
Lay Summary.
In this study of 43 758 people, we studied whether a reduction or increase in alcohol intake over a 5-year period was linked to an either higher or lower risk of a common cardiac rhythm disturbance, atrial fibrillation, compared with a stable intake.
A high alcohol intake of more than 21 drinks per week was related to a higher risk of atrial fibrillation
People who increased their alcohol intake had a higher risk of atrial fibrillation compared with individuals who maintained a low or moderate alcohol intake
Introduction
It is well-established that habitual alcohol consumption is a risk factor for incident atrial fibrillation (AF).1 In large observational studies, the relationship between alcohol intake and risk of incident AF was dose-dependent and even at moderate intakes, alcohol consumption was associated with a higher risk of AF.2 The association between alcohol intake and risk of AF has been confirmed in a Mendelian randomization study showing that genetically predicted heavy alcohol consumption was associated with an increased risk of AF.3 Recently, a randomized controlled trial showed that alcohol abstinence in patients with previous habitual alcohol intake reduced AF recurrences,4 pointing to the benefits of reducing alcohol intake for secondary AF prevention. In addition, a large observational study reported that alcohol abstinence after AF diagnosis was associated with a lower risk of stroke compared with continued use of alcohol.5 European guidelines suggest modification of an unhealthy lifestyle to reduce the AF burden, including avoidance of excess alcohol intake for AF prevention,6 however the evidence for changes in alcohol intake for primary prevention of AF is sparse. We hypothesized that compared with stable intake, a decrease in alcohol intake is associated with a lower risk of AF, whereas an increase is associated with a higher risk of AF. Thus, we set out to examine the association between 5-year changes in self-reported alcohol intake and long-term risk of AF in a large Danish cohort.
Methods
Study population
The study was based on the Danish cohort study Diet, Cancer and Health, which has previously been described in detail.7 Briefly, between 1993 and 1997, a total of 160 725 men and women born in Denmark and living in the greater Copenhagen or Aarhus areas, with no diagnosis of cancer, aged 50–64 years, were invited and 57 053 individuals accepted to participate in a research examination. A flowchart of participation is found in supplementary material online, Figure S1. Of the 57 053 individuals who accepted participation, 585 were later excluded because of a cancer diagnosis prior to enrolment, which had not been registered in the Danish Cancer Registry at the time of invitation because of processing delay. Three withdrew their consent leaving 56 465 participants. Approximately 5 years after the first examination, the participants were invited to participate in a follow-up research examination. From the individuals who participated in the first examination, 11 592 did not attend the second examination. For this study, we excluded participants with a diagnosis of AF before the second examination (n = 901) and participants with missing data (n = 214).
The Diet, Cancer and Health cohort was approved by the relevant scientific Ethic Committees and the Data Protection Agency, and all participants gave written informed consent at enrolment.
Assessment of changes in alcohol intake
At the first and second examinations, a detailed food frequency questionnaire consisting of 192 and 211 food items, respectively, was sent by mail to the participants and filled in. In the food frequency questionnaire, alcohol intake was reported as the average units of beer, wine, and spirits consumed over the preceding year and converted into grams of alcohol per day in total. The number of units per week was calculated with a definition of a standard unit containing 10 g of alcohol. Change in alcohol intake was assessed by subtracting alcohol intake (drinks/week) at the first examination from alcohol intake at the second examination (drinks/week). Hence a negative value represented a decrease in alcohol intake and a positive value an increase. Based on a previous study from the Diet, Cancer and Health cohort,8 we categorized participants by alcohol intake at the second examination in the following four groups: ≤ 6.9 drinks/week, 7–13.9 drinks/week, 14–20.9 drinks/week, and ≥21 drinks/week for the main analysis.
Covariates and outcomes
At the first examination height and weight were measured, whereas weight was self-reported at the second examination. Body mass index (BMI) was calculated as [weight (kg)]/[height (m2)]. At the first and the second examination, participants were asked about smoking status (never, prior, or current), and the participants filled in questionnaires regarding comorbidities, including hypertension, diabetes, and hypercholesterolaemia, and educational level.
Using the civil registration number, assigned to all individuals living in Denmark,9 we linked the cohort database to the Danish National Patient Register, which includes discharge diagnoses from in-hospital patients, emergency departments, and outpatient visits.10 The ICD-10 codes for the outcome and each covariate can be seen in supplementary material online, TableS1. The outcome of the analyses was AF (including atrial flutter) thus we identified all participants with a diagnosis of AF and/or atrial flutter in the register. In a previous validation study, the positive predictive value of AF and/or atrial flutter in the Danish National Patient Register was 92%.11 For covariates we identified all patients with a diagnosis of heart failure, ischaemic stroke, diabetes mellitus, myocardial infarction, and hypertension before the second examination in the Danish National Patient Register. Overall, the validity of cardiovascular diagnoses in the register has been reported to be high.11 For hypertension and diabetes mellitus, we combined information from the Danish National Patient Register and self-reported information regarding treatment for hypertension and diabetes mellitus since these conditions are often diagnosed and managed by a general practitioner and thus not registered in the Danish National Patient Register. Information on vital status was obtained from the National Central Person Register.
Statistical analyses
Baseline characteristics were compared between participants according to change in alcohol intake from the first to the second examination in the following groups: stable intake [change in the number of drinks/week between −0.9 and 0.9, decreased intake (−6.9 to −1 drinks/week and ≤ −7 drinks/week)] and participants who increased their alcohol intake (1–6.9 and ≥7 drinks/week).8
We assessed risk estimates using Cox proportional hazards models. Assumptions of independent entry were checked and found valid. For each model, the proportional hazards assumption was checked by plotting the observed and fitted curves and by log-log curves and was found to be valid in all cases.
To verify the underlying assumption of an association between alcohol intake and risk of AF, we first performed an analysis of alcohol intake at the second examination and risk of AF based on the categories: ≤ 6.9 drinks/week, 7–13.9 drinks/week, 14–20.9 drinks/week and ≥21 drinks/week. The group drinking ≤6.9 drinks/week was used as a reference. The risk of AF was assessed from the time of the second examination until the date of AF diagnosis, death, immigration, or end of follow-up in September 2017, whichever came first. The model was adjusted for age, sex, educational level, BMI, smoking status, hypertension, heart failure, stroke, diabetes mellitus, and myocardial infarction at the time of the second examination.
By combining alcohol intake at the first and the second examination, we defined 16 categories of alcohol intake for the main analyses of associations between changes in alcohol intake and AF risk. The risk of AF was assessed from the time of second examination until the date of AF diagnosis, death, immigration, or end of follow-up in September 2017, whichever came first. The risk of AF was assessed with a stable intake in each category, defined by the alcohol intake category at the first examination, as the reference. The models were adjusted for age, sex, educational level, and the following variables assessed at the second examination: BMI, smoking status, heart failure, hypertension, diabetes mellitus, stroke, and myocardial infarction. For the main analysis of the association between changes in alcohol intake and the risk of AF, we performed several sensitivity analyses. First, to ensure that a possible association between change in alcohol intake was not confounded by a change in BMI, we adjusted for a change in BMI from the first to the second examination. In addition, to reduce bias from individuals who abstained from alcohol use due to illness, we omitted all participants who were diagnosed with AF within the first year of follow-up. We also conducted the analyses after omitting participants who abstained from alcohol intake at both examinations. We conducted an analysis adjusting for death as a competing risk using the Fine and Gray model. In addition, we explored the association between changes in drinks/week and AF risk for different types of alcoholic beverages including beer, wine, and spirits and liqueur. Finally, we restricted follow-up to 5 years in sensitivity analyses.
The absolute 5-year change in alcohol intake and risk of AF was assessed in a model adjusted for the abovementioned variables and alcohol intake at the first examination as a continuous measure (drinks/week). Absolute change in alcohol intake was visualized using a restricted cubic spline and tested for non-linearity. We performed all analyses in sex-pooled and sex-stratified analyses.
For all analyses, two-sided P-values below 0.05 were considered statistically significant. Analyses were performed using the Stata program software version 17.0.
Results
For the analyses, 43 758 participants were included. The median time of follow-up was 15.7 years. During this follow-up period, 5312 individuals were diagnosed with incident AF, 156 migrated and 9017 individuals died. The overall incidence rate of AF was 8.6 per 1000 person-years.
Study population characteristics
The median (interquartile range) alcohol intake was nine drinks/week (25th-75th percentile, 4-22) at the first examination and 10 drinks/week (25th-75th percentile, 4-22) at second examination (the median difference from the first to the second examination 0.5 drinks/week). The number of participants who abstained from alcohol was 825 (1.8%) at the first examination and 1662 (3.8%) at the second examination.
Characteristics at the second examination according to change in alcohol intake are shown in Table 1. In the total population, the median age was 61 (25th–75th percentile, 58–66) years and 54% were female. The proportion of participants with a school education <8 years was 31.1%. The median BMI was 25.4 kg/m2 (25th-75th percentile 23.1-28.0), 28% smoked and the median alcohol intake was 10 drinks/week (25th-75th percentile, 4-22). Generally, the prevalence of comorbidities was low with hypertension being the most prevalent comorbidity (17.2%).
Table 1.
Study population characteristics at the second examination according to change in alcohol intake in the Danish Diet, Cancer, and Health study (n = 43 758)
| Total | Change in alcohol intake (drinks/week) | |||||
|---|---|---|---|---|---|---|
| Decreased intake (n = 14 577, 33%) | Stable intake (n = 10 779, 25%) | Increased intake (n = 18 402, 42%) | ||||
| ≤−7 | −6.9 to −1.0 | −0.9–0.9 | 1.0–6.9 | ≥7 | ||
| Number | 43 758 | 5193 (12%) | 9384 (21%) | 10 779 (25%) | 11 502 (26%) | 6900 (16%) |
| Age, years | 61 (58–66) | 61 (58–65) | 61 (58–65) | 62 (58–66) | 62 (58–66) | 62 (58–65) |
| Females | 23 397 (54%) | 1840 (35%) | 4969 (53%) | 7226 (67%) | 6530 (57%) | 2832 (41%) |
| School education <8 years | 13 625 (31.1%) | 1679 (32.3%) | 2933 (31.3%) | 3726 (34.6%) | 3368 (29.3%) | 1919 (27.8%) |
| Currently smoking | 12 228 (28.0%) | 1888 (36.4%) | 2537 (27.0%) | 2918 (27.1%) | 2788 (24.2%) | 2097 (30.4%) |
| Alcohol intake (drinks/week) | 10 (4-22) | 12.3 (7.1–22.9) | 6.7 (3.1–12.5) | 3.9 (1.1–9.8) | 9.9 (6.2–15.4) | 28.7 (22.2–42.9) |
| Body mass index (kg/m2) | 25.4 (23.1–28.0) | 25.6 (23.4–28.3) | 25.4 (23.2–28.0) | 25.4 (23.0–28.2) | 25.2 (23.0–27.7) | 25.5 (23.3–27.7) |
| Hypertension | 7504 (17.2%) | 994 (19.1%) | 1557 (16.6%) | 1932 (18.0%) | 1855 (16.1%) | 1166 (16.9%) |
| Diabetes mellitus | 1245 (2.9%) | 191 (3.7%) | 249 (2.7%) | 344 (3.2%) | 283 (2.5%) | 178 (2.6%) |
| Heart failure | 302 (0.7%) | 49 (1%) | 57 (0.6%) | 84 (0.8%) | 72 (0.6%) | 40 (0.6%) |
| Myocardial infarction | 1336 (3.1%) | 161 (3.1%) | 278 (3.0%) | 321 (3.0%) | 349 (3.0%) | 227 (3.3%) |
| Stroke | 761 (1.7%) | 132 (2.5%) | 167 (1.8%) | 175 (1.6%) | 163 (1.4%) | 124 (1.8%) |
Change in alcohol intake (drinks/week) was assessed by subtracting alcohol intake at the first examination from alcohol intake at the second examination. Data are presented as mean ± SD, median (25th–75th percentiles) or number (percentage).
Between the first and the second examination, 14 577 (33%) reported a decrease in alcohol intake, 10 779 (25%) reported a stable intake and 18 402 (42%) reported an increase in alcohol intake (Table 1). The proportion of females was lowest among those who reported a decrease or increase in alcohol intake ≥7 drinks/week (35% and 41%, respectively) compared with stable intake (67% females). The proportion of individuals who smoked at follow-up was highest among those who reported decreasing their alcohol intake by seven or more drinks/week (36.4% currently smoking). Among those reporting a decrease of seven or more drinks/week, the prevalence of comorbidities was slightly higher compared with all the other groups, except for myocardial infarction (Table 1). Characteristics at the second examination according to changes in alcohol intake in females and males are shown in supplementary material online, TableS2. The 11 592 individuals who did not attend the second examination were less frequently females, had lower level of education, were more frequently smoking, and had higher prevalence of comorbidities, at the first examination, compared with those who participated in the second examination. However, alcohol intake at the first examination did not differ between participants and non-participants (supplementary material online, Table S3).
Alcohol intake at second examination and risk of atrial fibrillation
supplementary material online, Table S4 shows the number of AF cases per 1000 person-years and hazard ratios for AF according to alcohol intake at the second examination. With participants drinking ≤6.9 drinks/week as a reference, the risk of AF was higher for participants drinking ≥21 drinks/week (HR: 1.19, 95% CI: 1.11–1.28), while there was no statistically significant difference in risk of AF for participants drinking 7–13.9 drinks/week and 14–20.9 drinks per week, respectively. The association between alcohol intake ≥21 drinks/week and risk of AF was observed for both females and males (supplementary material online, Table S4).
Five-year changes in alcohol intake and risk of atrial fibrillation
Absolute and relative risks of AF according to changes in alcohol intake from the first to the second examination are shown in Table 2. The rate of AF was 10.9 per 1000 person-years (95% CI: 8.7–13.5) among participants who reported an increase in alcohol intake from ≤6.9 at the first examination to ≥21 drinks/week at the second examination. For participants with a stable intake of ≤6.9 drinks/week at both examinations, the rate was 7.7 per 1000 person-years (95% CI: 7.3–8.1). Compared with participants with a stable alcohol intake of ≤6.9 drinks/week, the risk of AF was higher among participants who increased their alcohol intake from ≤6.9 drinks/week at the first examination to ≥21 drinks/week at the second examination (HR: 1.38, 95% CI: 1.09–1.72) (Table 2). A higher risk of AF was also noted in participants who increased their alcohol intake from 14–20.9 drinks/week at the first examination to ≥21 drinks/week at the second examination (rate 11.1 per 1000 person-years, 95% CI: 9.6–12.8) compared with those with a stable intake of 14–20.9 drinks/week at both examinations (rate 8.9 per 1000 person-years, 95% CI: 7.4–10.6) (HR: 1.27, 95% CI: 1.01–1.59). However, there was no statistically significant difference in risk of AF for participants who increased their alcohol intake from 7–13.9 to ≥21 drinks/week compared with those with a stable intake of 7–13.9 drinks/week (HR: 1.11, 95% CI: 0.96–1.29). For all categories of alcohol intake at the first examination, there was no significant difference in risk of AF for participants who reported a decrease in alcohol intake from the first to the second examination compared to stable intake in each category (Table 2).
Table 2.
Absolute and relative risk of atrial fibrillation by 5-year changes in alcohol intake (drinks/week) in the Danish Diet, Cancer, and Health study
| First examination (drinks/week) | Second examination (drinks/week) | |||
|---|---|---|---|---|
| ≤6.9 | 7–13.9 | 14–20.9 | ≥21 | |
| Number of cases/1000 person-years (95% CI) | ||||
| ≤6.9 | 7.7 (7.3–8.1) | 7.7 (6.9–8.5) | 7.1 (5.0–10.1) | 10.9 (8.7–13.5) |
| 7–13.9 | 7.5 (6.7–8.4) | 7.5 (6.9–8.1) | 7.6 (6.5–8.8) | 8.6 (7.6–9.7) |
| 14–20.9 | 11.4 (8.1–16.0) | 9.1 (7.7–10.8) | 8.9 (7.4–10.6) | 11.1 (9.6–12.8) |
| ≥21 | 11.2 (9.0–13.9) | 10.6 (9.2–12.1) | 10.2 (8.6–12.1) | 10.5 (9.9–11.1) |
| Hazard ratio (95% CI) | ||||
| ≤6.9 | Reference | 1.02 (0.90–1.14) | 0.82 (0.57–1.16) | 1.38 (1.09–1.72) |
| 7–13.9 | 0.99 (0.86–1.14) | Reference | 0.93 (0.78–1.11) | 1.11 (0.96–1.29) |
| 14–20.9 | 1.40 (0.95–2.06) | 1.08 (0.85–1.38) | Reference | 1.27 (1.01–1.59) |
| ≥21 | 1.01 (0.81–1.27) | 1.08 (0.93–1.26) | 0.97 (0.81–1.16) | Reference |
We performed these analyses on individuals who attended first and second examination and who did not have a diagnosis of AF before time of second examination (n = 43 758). Hazard ratios are adjusted for sex, educational level and age, body mass index, smoking status, hypertension, heart failure, stroke, diabetes mellitus and myocardial infarction at time of second examination.
Table 3 shows absolute and relative risks of AF by 5-year changes in alcohol intake (drinks/week) stratified by sex. The rate of AF was 6.8 per 1000 person-years (95% CI: 6.4–7.3) for females with a stable intake of ≤6.9 drinks/week at both examinations. In comparison, the rate of AF was 9.4 per 1000 person-years (95% CI: 6.9–12.6) for females with an alcohol intake ≤6.9 drinks/week at the first examination but ≥21 drinks/week at the second examination. In the adjusted model, the HR was 1.45, 95% CI: 1.07–1.98 for females who reported an increase in alcohol intake from ≤6.9 drinks/week at the first examination to ≥21 drinks/week at the second examination compared with females with a stable intake ≤6.9 drinks/week at both examinations. For females who increased their alcohol intake to ≥21 weeks/drink at the second examination from 7–13.9 drinks/week at the first examination (rate 6.9 per 1000 person-years, 95% CI: 5.7–8.4), the risk of AF was also higher compared with females with a stable intake of 7–13.9 drinks/week at both examinations (rate 5.4 per 1000 person-years, 95% CI: 4.7–6.1) (HR: 1.30, 95% CI: 1.04–1.64). For females with an alcohol intake of 14–20.9 drinks/week and ≥21 drinks/week, respectively, at the first examination, there was no statistically significant association between reported changes in alcohol intake and AF risk (Table 3). For males, changes in alcohol intake from the first to the second examination were not statistically significantly associated with the risk of AF, except for males who decreased their alcohol intake from 14–20.9 drinks/week at the first examination to ≤6.9 drinks/week at the second examination (HR: 1.69, 95% CI: 1.09–2.63) (Table 3).
Table 3.
Absolute and relative risks of atrial fibrillation by 5-year changes in alcohol intake (drinks/week) for females (n = 23 397) and males (n = 20 361) in the Danish Diet, Cancer, and Health study
| Females | ||||
|---|---|---|---|---|
| First examination (drinks/week) | Second examination (drinks/week) | |||
| ≤6.9 | 7–13.9 | 14–20.9 | ≥21 | |
| Number of cases/1000 person-years (95% CI) | ||||
| ≤6.9 | 6.8 (6.4–7.3) | 5.9 (5.1–6.8) | 7.5 (4.8–11.8) | 9.4 (6.9–12.6) |
| 7–13.9 | 5.9 (5.0–6.9) | 5.4 (4.7–6.1) | 5.3 (3.9–7.1) | 6.9 (5.7–8.4) |
| 14–20.9 | 5.9 (3.0–11.9) | 6.4 (4.6–8.9) | 6.3 (4.2–9.4) | 7.3 (5.2–10.1) |
| ≥21 | 6.4 (4.2–9.8) | 7.1 (5.5–9.1) | 6.5 (4.6–9.3) | 6.6 (5.8–7.5) |
| Hazard ratio (95% CI) | ||||
| ≤6.9 | Reference | 0.93 (0.80–1.09) | 1.11 (0.70–1.74) | 1.45 (1.07–1.98) |
| 7–13.9 | 1.03 (0.84–1.27) | Reference | 0.91 (0.66–1.24) | 1.30 (1.04–1.64) |
| 14–20.9 | 0.80 (0.35–1.82) | 1.02 (0.60–1.73) | Reference | 1.22 (0.72–1.08) |
| ≥21 | 0.85 (0.54–1.34) | 1.04 (0.79–1.37) | 0.89 (0.61–1.31) | Reference |
| Males | ||||
|---|---|---|---|---|
| First examination (drinks/week) | Second examination (drinks/week) | |||
| ≤6.9 | 7–13.9 | 14–20.9 | ≥21 | |
| Number of cases/1000 person-years (95% CI) | ||||
| ≤6.9 | 10.4 (9.5–11.4) | 11.3 (9.7–13.1) | 6.6 (3.8–11.4) | 13.4 (9.7–18.4) |
| 7–13.9 | 10.1 (8.7–11.8) | 10.2 (9.2–11.3) | 9.1 (7.6–11.0) | 10.3 (8.7–12.0) |
| 14–20.9 | 16.1 (10.9–23.8) | 10.8 (8.8–13.1) | 9.9 (8.1–12.0) | 12.6 (10.8–14.8) |
| ≥21 | 15.1 (11.7–19.3) | 13.7 (11.6–16.2) | 12.1 (10.0–14.7) | 12.4 (11.6–13.2) |
| Hazard ratio (95% CI) | ||||
| ≤6.9 | Reference | 1.12 (0.94–1.33) | 0.60 (0.35–1.05) | 1.29 (0.92–1.80) |
| 7–13.9 | 0.96 (0.80–1.16) | Reference | 0.92 (0.74–1.14) | 1.01 (0.83–1.22) |
| 14–20.9 | 1.69 (1.09–2.63) | 1.09 (0.82–1.44) | Reference | 1.27 (0.99–1.64) |
| ≥21 | 1.09 (0.84–1.41) | 1.10 (0.92–1.32) | 0.99 (0.81–1.21) | Reference |
We performed these analyses on individuals who attended the first and the second examination and who did not have a diagnosis of AF before time of the second examination (n = 43 758). Hazard ratios are adjusted for educational level and age, body mass index, smoking status, hypertension, heart failure, stroke, diabetes mellitus and myocardial infarction at the time of second examination.
In sensitivity analyses, in which we adjusted for changes in BMI, omitted participants with AF within the first year of follow-up, omitted participants who abstained from alcohol intake, and adjusted for competing risk of death, respectively, the associations were not qualitatively different from the results obtained in the main analyses (supplementary material online, TableS5). There were no statistically significant associations between changes in alcohol intake and risk of AF when restricting to 5 years of follow-up in sensitivity analyses (supplementary material online, Table S5). When assessing the associations between changes in alcohol intake and risk of AF stratified by the type of alcoholic beverages, there was a statistically significant signal in individuals who increased their intake of wine from ≤6.9 drinks/week to 14–20.9 drinks/week (supplementary material online, TableS6). There were no other statistically significant associations when stratifying by the type of alcoholic beverages.
Figure 1 shows hazard ratio estimates by absolute change in alcohol intake with no change as a reference. An increase in alcohol intake was associated with a higher risk of AF compared with no changes, whereas there was no statistically significant association between decreases in alcohol intake and risk of AF. The test for non-linearity was statistically significant (P = 0.01). In sex-stratified analyses, the association between an increase in alcohol intake and the risk of AF was statistically significant for females but not for males (supplementary material online, Figure S2).
Figure 1.
Restricted cubic spline showing hazard ratios of atrial fibrillation by absolute change in alcohol intake (drinks/week). The curved solid line represents hazard ratio estimates by absolute change in alcohol intake with a change of 0 drinks/week as a reference in the Danish Diet, Cancer, and Health study (n = 43 758). The dotted lines represent the 95% CI. The bars show the density distribution of alcohol changes. The model was adjusted for sex, educational level and age, body mass index, smoking status, hypertension, heart failure, stroke, diabetes mellitus and myocardial infarction at time of second examination and alcohol intake at first examination. Test for non-linearity, P = 0.01.
Discussion
In this cohort study, we observed that individuals who reported an increase in alcohol intake over a 5-year period had a higher risk of AF compared with those with a stable low or moderate intake. We did not find statistically significant associations between reductions in alcohol intake and the risk of AF.
The positive association between alcohol consumption and risk of incident AF has been demonstrated in numerous studies1 and was confirmed in our analysis. A recent study from the Korean National Health Insurance Service database found that heavy alcohol intake was a risk factor for AF from the age of 30 years, while mild to moderate alcohol intake was associated with an increased risk of AF from the age of 60.12 The evidence regarding changes in alcohol intake and risk of incident AF, however, is sparse. Recently, another study from the Korean National Health Insurance Service database demonstrated that in 175 100 patients with type 2 diabetes mellitus (T2DM), abstaining from alcohol after T2DM diagnosis was associated with a lower risk of AF compared with continued heavy alcohol consumption (≥20 g of alcohol/day).13 Surprisingly, we did not observe a statistically significant association between a reduction in alcohol intake and the risk of AF. We even observed that males who decreased their alcohol intake from 14–20.9 drinks/week to <6.9 drinks/week had a significantly higher risk of AF. There may be several potential explanations for these findings. First, participants who decreased their alcohol intake by more than seven drinks/week had a higher prevalence of cardiovascular comorbidities including stroke, myocardial infarction, diabetes mellitus, and hypertension. They were also more frequent smoking. Thus, these participants may have decreased their alcohol intake due to illnesses associated with a higher risk of AF, possibly leading to confounding by indication. A paper from the Atherosclerosis Risk in Communities Study reported that individuals with former alcohol use had higher risk of AF compared with individuals who never consumed alcohol and that longer duration and greater previous quantity of alcohol were predictors of AF risk.14 Since studies have reported that alcohol consumption is associated with atrial electrical, structural, and functional changes,15–17 the higher risk of AF in individuals who previously consumed alcohol may be explained by irreversible changes. Finally, there might lack of statistical power to detect differences in AF risk in participants reducing their alcohol intake in our study.
A large study from the UK Biobank found differences in associations between alcohol intake and risk of AF when stratifying according to the type of alcoholic beverage.18 In exploratory analyses, we did not find clear associations between changes in alcohol intake and risk of AF when stratifying by beverage type. Most likely, there was a lack of statistical power in these analyses.
In sex-stratified analyses, the association between a high alcohol intake at the second examination and the risk of AF was present in both males and females. This corresponds to previous studies, in which the authors did not find sex to be a modifier of the association between alcohol intake and AF risk.2,18,19 However, in the Norwegian Tromsø study, there was an increase in AF incidence in men from 1994 to 2016, partly attributable to an increase in alcohol intake, while the incidence of AF decreased in women.20 Nevertheless, we observed that the association between increases in alcohol intake and risk of AF was only statistically significant for females. The direction of association was, however, also present for males. A potential reason for a statistically significant association in females could be that female participants had a lower median alcohol intake at baseline compared to males. Thus, an increase of one drink/week would proportionally be a larger increase for participants with lower baseline alcohol intake.
The results of our study should be interpreted in light of its limitations, one being that alcohol intake was assessed by questionnaires, which may lead to an underestimation of the true alcohol intake and thus cause an overestimation of the effects of alcohol. However, other studies have validated the assessment of alcohol intake from questionnaires against detailed diet records and found that self-reporting correlated with detailed reports.21,22 In addition, the semiquantitative food frequency questionnaire developed for and used in this study was validated against detailed diet records and found valid.23 Another common limitation in cohort studies is generalizability. In this study, participants may have healthier lifestyles compared with non-participants and thus alcohol intake may differ from the general population. Possibly due to a healthier lifestyle and low comorbidity, the incidence rates of AF found in this study were somewhat lower than other findings,24,25 however this would presumably not bias the association between alcohol changes and the risk of AF. Also, individuals who attended the second examination were healthier than those who did not attend the second examination. However, since baseline alcohol intake did not differ and we adjusted for a number of relevant comorbidities, we do not expect this selection to cause a bias in the association between changes in alcohol intake and risk of AF. In addition, the participants were White and at baseline middle-aged; the generalizability to other races/ethnicities or ages remains to be determined. Since we assessed alcohol intake at two timepoints only, we could not consider alcohol intake in the period between the two timepoints or the duration of changes in alcohol intake. Alcohol intake may vary substantially during a lifetime. A decrease or cessation in alcohol intake may be provoked by illness, including AF or diseases that predispose to AF, resulting in a bias from alcohol abstinence due to illness and thus an overestimation of AF risk in participants who decrease their alcohol intake. However, in sensitivity analyses, we omitted participants with a diagnosis of AF within 1 year after the second examination which did not considerably alter the results. This exclusion of potentially more susceptible participants may possibly introduce selection bias in the sensitivity analysis, but the results were largely similar. We also adjusted for changes in BMI, as a marker of changes in subclinical predisposition to AF and observed no substantial differences in our main results. Also, drinking pattern was not considered. A previous study showed that binge drinking in individuals with moderate habitual consumption was associated with a higher risk of AF compared with non-binge moderate drinking.26 Assuming that individuals with a high alcohol intake more frequently binge drink compared with individuals with a lower alcohol intake, binge drinking episodes, which were not assessed in this cohort, may be a confounder of the relationship between alcohol intake and risk of AF. Another possible confounder of the relationship between alcohol intake and AF is sleep apnoea. Alcohol intake is associated with a higher risk of sleep apnoea,27 which is a risk factor for AF.28 However, information on sleep apnoea was not available in this cohort. Our data are observational, and many of the confounders such as hypertension and weight at the second examination were based on self-report. We cannot exclude residual confounding and cannot establish causal relations. In addition, AF assessment was based on diagnosis codes and not systematic ECG monitoring, which could potentially lead to an underestimation of AF incidence. Finally, in most cases, the type of AF was not specified in the Danish National Patient Registry. Thus, we were not able to assess the association between changes in alcohol intake and the risk of different types of AF.
Conclusions
A 5-year increase to a high alcohol intake was associated with a greater risk of AF compared with a stable low or moderate alcohol intake in the Danish Diet, Cancer and Health cohort, whereas decreases in alcohol intake were not statistically significantly associated with differences in AF risk compared with stable intake. These results suggest that an increase in alcohol intake should be avoided for the primary prevention of AF.
Author’s contribution
T.C.F., C.C.D., M.K.C., K.O., and H.K.J. contributed to the conception or design of the work. T.C.F., K.O., A.O., and C.C.D. contributed to the acquisition, analysis, or interpretation of data for the work. T.C.F. drafted the manuscript. C.C.D., M.K.C., A.O., K.O., E.J.B., and H.K.J. critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Supplementary material
Supplementary material is available at European Journal of Preventive Cardiology online.
Supplementary Material
Acknowledgements
We thank the participants of the Danish Diet, Cancer and Health Study for their time and cooperation.
Contributor Information
Tanja Charlotte Frederiksen, Department of Cardiology, Aarhus University Hospital, Palle Juul-Jensens Blvd 99, 8200 Aarhus N, Denmark; Department of Clinical Medicine, Health, Aarhus University, Palle Juul-Jensens Blvd 99, 8200 Aarhus N, Denmark.
Morten Krogh Christiansen, Department of Cardiology, Aarhus University Hospital, Palle Juul-Jensens Blvd 99, 8200 Aarhus N, Denmark.
Emelia J Benjamin, Sections of Cardiovascular Medicine, Boston Medical Center, Boston University Chobanian and Avedisian School of Medicine, Boston, 725 Albany Street, MA 02118, USA.
Kim Overvad, Research Unit for Epidemiology, Department of Public Health, Aarhus University, Bartholins Allé 2, 8000 Aarhus C, Denmark.
Anja Olsen, Research Unit for Epidemiology, Department of Public Health, Aarhus University, Bartholins Allé 2, 8000 Aarhus C, Denmark; Danish Cancer Society Research Center, Strandboulevarden 49, 2100 Copenhagen, Denmark.
Christina Catherine Dahm, Research Unit for Epidemiology, Department of Public Health, Aarhus University, Bartholins Allé 2, 8000 Aarhus C, Denmark.
Henrik Kjærulf Jensen, Department of Cardiology, Aarhus University Hospital, Palle Juul-Jensens Blvd 99, 8200 Aarhus N, Denmark; Department of Clinical Medicine, Health, Aarhus University, Palle Juul-Jensens Blvd 99, 8200 Aarhus N, Denmark.
Funding
Aarhus University; Helsefonden (R01HL092577); Sundhed, Region Midt (R01HL092577) to T.C.F. National Heart, Lung, and Blood Institute (R01HL092577); American Heart Association (AHA_18SFRN34110082) to E.J.B. Novo Nordisk Foundation (NNF18OC0031258, NNF20OC0065151) to H.K.J.
Data availability
The data are available from Diet, Cancer and Health Steering Committee at the Danish Cancer Society (dchdata@cancer.dk).
References
- 1. Voskoboinik A, Prabhu S, Ling LH, Kalman JM, Kistler PM. Alcohol and Atrial Fibrillation: A Sobering Review. Journal of the American College of Cardiology 2016;68:2567–2576. [DOI] [PubMed] [Google Scholar]
- 2. Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol 2014;64:281–289. [DOI] [PubMed] [Google Scholar]
- 3. Lu Y, Guo Y, Lin H, Wang Z, Zheng L. Genetically determined tobacco and alcohol use and risk of atrial fibrillation. BMC Med Genomics 2021;14:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Voskoboinik A, Kalman JM, De Silva A, Nicholls T, Costello B, Nanayakkara S, Prabhu S, Stub, Azzopardi S, Vizi D, Wong G, Nalliah C, Sugumar H, Wong M, Kotschet E, Kaye D, Taylor AJ, Kistler OM, Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med 2020;382:20–28. [DOI] [PubMed] [Google Scholar]
- 5. Lee SR, Choi EK, Jung JH, Han KD, Oh S, Lip GYH. Lower risk of stroke after alcohol abstinence in patients with incident atrial fibrillation: a nationwide population-based cohort study. Eur Heart J 2021;42:4759–4768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J 2021;42:373–498. [DOI] [PubMed] [Google Scholar]
- 7. Tjonneland A, Olsen A, Boll K, Stripp C, Christensen J, Engholm G, Overvad K. Study design, exposure variables, and socioeconomic determinants of participation in diet, cancer and health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health 2007;35:432–441. [DOI] [PubMed] [Google Scholar]
- 8. Dam MK, Hvidtfeldt UA, Tjønneland A, Overvad K, Grønbæk M, Tolstrup JS. Five year change in alcohol intake and risk of breast cancer and coronary heart disease among postmenopausal women: prospective cohort study. BMJ 2016;353:i2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pedersen CB. The Danish civil registration system. Scand J Public Health 2011;39:22–25. [DOI] [PubMed] [Google Scholar]
- 10. Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health 2011;39:30–33. [DOI] [PubMed] [Google Scholar]
- 11. Sundbøll J, Adelborg K, Munch T, Frøslev T, Sørensen HT, Bøtker HE, Schmidt M. Positive predictive value of cardiovascular diagnoses in the Danish national patient registry: a validation study. BMJ Open 2016;6:e012832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kim YG, Han KD, Choi JI, Choi YY, Choi HY, Boo KY, Kim DY, Lee KN, Shim J, Kim JS, Park YG, Kim YH, et al. Non-genetic risk factors for atrial fibrillation are equally important in both young and old age: a nationwide population-based study. Eur J Prev Cardiol 2021;28:666–676. [DOI] [PubMed] [Google Scholar]
- 13. Choi YJ, Han KD, Choi EK, Jung JH, Lee SR, Oh S, Lip GYH. Alcohol abstinence and the risk of atrial fibrillation in patients with newly diagnosed type 2 diabetes Mellitus: a nationwide population-based study. Diabetes Care 2021;44:1393–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dixit S, Alonso A, Vittinghoff E, Soliman EZ, Chen LY, Marcus GM. Past alcohol consumption and incident atrial fibrillation: the atherosclerosis risk in communities (ARIC) study. PLoS One 2017;12:e0185228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Voskoboinik A, Wong G, Lee G, Nalliah C, Hawson J, Prabhu S, Sugumar H, Ling LH, McLellan A, Morton J, Kalman JM, Kistler PM. Moderate alcohol consumption is associated with atrial electrical and structural changes: insights from high-density left atrial electroanatomic mapping. Heart Rhythm 2019;16:251–259. [DOI] [PubMed] [Google Scholar]
- 16. McManus DD, Yin X, Gladstone R, Vittinghoff E, Vasan RS, Larson MG, Benjamin EJ, Marcus GM. Alcohol consumption, left atrial diameter, and atrial fibrillation. J Am Heart Assoc 2016;5:e004060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Voskoboinik A, Costello BT, Kalman E, Prabhu S, Sugumar H, Wong G, Nalliah C, Ling LH, McLellan A, Hettige T, Springer F, La Gerche A, Kalman JM, Taylor AJ, Kistler PM. Regular alcohol consumption is associated with impaired atrial mechanical function in the atrial fibrillation population: a cross-sectional MRI-based study. JACC Clin Electrophysiol 2018;4:1451–1459. [DOI] [PubMed] [Google Scholar]
- 18. Tu SJ, Gallagher C, Elliott AD, Linz D, Pitman BM, Hendriks JML, Lau DH, Sanders P, Wong CX. Risk thresholds for total and beverage-specific alcohol consumption and incident atrial fibrillation. JACC Clin Electrophysiol 2021;7:1561–1569. [DOI] [PubMed] [Google Scholar]
- 19. Csengeri D, Sprünker NA, Di Castelnuovo A, Niiranen T, Vishram-Nielsen JK, Costanzo S, Söderberg S, Jensen SM, Vartiainen E, Donati MB, Magnussen C, Camen S, Gianfagna F, Løchen ML, Kee F, Kontto J, Mathiesen EB, Koenig W, Stefan B, de Gaetano G, Jørgensen T, Kuulasmaa K, Zeller T, Salomaa V, Iacoviello L, Schnabel RB. Alcohol consumption, cardiac biomarkers, and risk of atrial fibrillation and adverse outcomes. Eur Heart J 2021;42:1170–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sharashova E, Gerdts E, Ball J, Espnes H, Jacobsen BK, Kildal S, Mathiesen EB, Njølstad I, Rosengren A, Schirmer H, Wilsgaard T, Løchen ML. Sex-specific time trends in incident atrial fibrillation and the contribution of risk factors: the tromsø study 1994-2016. Eur J Prev Cardiol 2023;30:72–81. [DOI] [PubMed] [Google Scholar]
- 21. Giovannucci E, Colditz G, Stampfer MJ, Rimm EB, Litin L, Sampson L, Willett WC. The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol 1991;133:810–817. [DOI] [PubMed] [Google Scholar]
- 22. Grønbaek M, Heitmann BL. Validity of self-reported intakes of wine, beer and spirits in population studies. Eur J Clin Nutr 1996;50:487–490. [PubMed] [Google Scholar]
- 23. Tjønneland A, Overvad K, Haraldsdóttir J, Bang S, Ewertz M, Jensen OM. Validation of a semiquantitative food frequency questionnaire developed in Denmark. Int J Epidemiol 1991;20:906–912. [DOI] [PubMed] [Google Scholar]
- 24. Stefansdottir H, Aspelund T, Gudnason V, Arnar DO. Trends in the incidence and prevalence of atrial fibrillation in Iceland and future projections. Europace 2011;13:1110–1117. [DOI] [PubMed] [Google Scholar]
- 25. Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, Stijnen T, Lip GY, Witteman JC. Prevalence, incidence and lifetime risk of atrial fibrillation: the rotterdam study. Eur Heart J 2006;27:949–953. [DOI] [PubMed] [Google Scholar]
- 26. Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, Fagard R, Lonn E, Teo KK. Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ 2012;184:E857–EE66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Simou E, Britton J, Leonardi-Bee J. Alcohol and the risk of sleep apnoea: a systematic review and meta-analysis. Sleep Med 2018;42:38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen W, Cai X, Yan H, Pan Y. Causal effect of obstructive sleep apnea on atrial fibrillation: a Mendelian randomization study. J Am Heart Assoc 2021;10:e022560. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are available from Diet, Cancer and Health Steering Committee at the Danish Cancer Society (dchdata@cancer.dk).