Abstract
Background and Aims:
Fatty liver disease is highly prevalent, resulting in overarching wellbeing and economic costs. Addressing it requires comprehensive and coordinated multisectoral action. We developed a fatty liver disease Sustainable Development Goal (SDG) country score to provide insights into country-level preparedness to address fatty liver disease through a whole-of-society lens.
Approach and Results:
We developed 2 fatty liver disease–SDG score sets. The first included 6 indicators (child wasting, child overweight, noncommunicable disease mortality, a universal health coverage service coverage index, health worker density, and education attainment), covering 195 countries and territories between 1990 and 2017. The second included the aforementioned indicators plus an urban green space indicator, covering 60 countries and territories for which 2017 data were available. To develop the fatty liver disease–SDG score, indicators were categorized as “positive” or “negative” and scaled from 0 to 100. Higher scores indicate better preparedness levels. Fatty liver disease–SDG scores varied between countries and territories (n = 195), from 14.6 (95% uncertainty interval: 8.9 to 19.4) in Niger to 93.5 (91.6 to 95.3) in Japan; 18 countries and territories scored > 85. Regionally, the high-income super-region had the highest score at 88.8 (87.3 to 90.1) in 2017, whereas south Asia had the lowest score at 44.1 (42.4 to 45.8). Between 1990 and 2017, the fatty liver disease–SDG score increased in all super-regions, with the greatest increase in south Asia, but decreased in 8 countries and territories.
Conclusions:
The fatty liver disease–SDG score provides a strategic advocacy tool at the national and global levels for the liver health field and noncommunicable disease advocates, highlighting the multisectoral collaborations needed to address fatty liver disease, and noncommunicable diseases overall.
INTRODUCTION
Fatty liver disease refers to a range of conditions in which excess fat builds up in the liver and is largely unknown among the general population,1 health policy makers, and the global public health community.2 This potentially serious condition is estimated to affect about one in 3 adults globally3 and is increasingly problematic in children and adolescents.4–6 Disease severity is measured through the degree of fibrosis; however, population-based estimates of advanced fibrosis associated with fatty liver disease are limited. Data from Germany have shown it to be around 1%,7 whereas a Korean study estimated it at 2.6%.8 A review of studies in patients at risk of clinically significant liver disease in a general population setting found that the prevalence of advanced liver fibrosis ranged between 0.9% and 2.0%, and cirrhosis between 0.1% and 1.7%.9 Fatty liver disease, and particularly the more aggressive condition NASH, have a substantial impact on individual health,10 burdening health systems, causing substantial economic encumbrance, and increasing wellbeing costs.11
Beyond being a leading cause of cirrhosis12 and liver cancer,13,14 fatty liver disease shares a close bidirectional relationship with other highly prevalent noncommunicable diseases (NCDs), most notably cardiovascular disease, type 2 diabetes mellitus, obesity, and nonhepatic cancers.15–17 In the majority of patients, fatty liver disease emerges in the context of metabolic syndrome.17 Although fatty liver disease is strongly associated with obesity,18 it is still prevalent in nonobese individuals, especially those of Asian descent.19 As a consequence of the lack of overall awareness about the condition, fatty liver disease continues to go largely undiagnosed among the general population,20 even among some high-risk populations, like people diagnosed with type 2 diabetes mellitus.21 Furthermore, fatty liver disease is asymptomatic until the occurrence of severe complications, making it difficult to identify the disease20 and implement treatment and care interventions, such as lifestyle modification.
Much like the other major public health challenges of the 21st century, fatty liver disease requires systems thinking alongside multidisciplinary and multisectoral responses22 that address the immediate and underlying determinants of the disease. Yet, despite the scale of the challenge posed by fatty liver disease, health system and public health responses have generally been weak and fragmented.2,23,24 A 2020 study captured data on NAFLD-related policies and guidelines in 102 countries, creating a NAFLD preparedness index that characterized the health system and public health responses in the participating countries. The study found that no country had a written strategy to address the disease and, in most countries, NAFLD was absent within strategies and guidelines for related conditions, including obesity and diabetes.2 To fill the dearth of strategic guidance, a consortium of 218 experts from 91 countries recently developed NAFLD consensus statements and recommendations to advance public health and policy agendas.25
Although health systems sit at the center of efforts to address the burden of fatty liver disease, tackling this public health challenge will require action well beyond the health sector. To help the public health community and those across other sectors to conceptualize the design of whole-of-society responses to fatty liver disease, we published a NAFLD–Sustainable Development Goal (SDG) framework.26 The SDGs serve as the mainstay of the 2030 Agenda for Sustainable Development, with clear priorities, from reducing social and economic inequalities to improving nutrition, health, and education, and were adopted by all United Nations member states in 2015. Using the SDGs as a multisectoral framework for action,27 a multidisciplinary group followed a standard Delphi process to identify the targets and indicators that are most relevant to NAFLD, with the final framework including 7 indicators. The framework is intended as a strategic advocacy tool to build the case for closer collaboration within and between sectors, to address fatty liver disease and other NCDs. Similar work has been undertaken to develop a framework to inform policy approaches on sustainable development and urban health28 and to highlight the importance of addressing obesity for achieving the SDG agenda.29
Here, we present the development of the first fatty liver disease–SDG score, covering 195 countries and territories from 1990 to 2017. The fatty liver disease–SDG score builds on the earlier framework to provide a multisectoral lens through which to view country-level preparedness to address the challenge of fatty liver disease, and to guide future health and development sector collaboration and action on this issue.
METHODS
NAFLD Sustainable Development Goal framework
The NAFLD–SDG framework underpinning the fatty liver disease–SDG score was developed through a Delphi process. First, a core team of researchers reviewed the SDG targets and indicators,30 identifying those directly or indirectly associated with NAFLD. Subsequently, a multidisciplinary group of experts (n = 15) was invited to select which of the shortlisted targets and indicators to include in the NAFLD–SDG framework. Targets and indicators with 75% or greater agreement were included in the final NAFLD–SDG framework, with this framework comprising 16 targets and 7 indicators (Figure 1). The detailed methodology has been published.26
FIGURE 1.
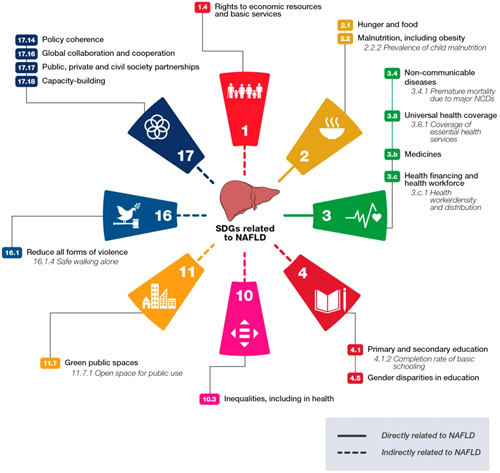
NAFLD–SDG framework. The NAFLD–SDG framework shows the SDG targets and indicators that are most relevant to NAFLD. The 8 colored segments indicate the selected targets and the 7 selected indicators are nested within 5 of these targets. Solid lines indicate targets with a direct link to NAFLD and dashed lines show those indirectly related to NAFLD. Abbreviations: NCD, noncommunicable disease; SDG, Sustainable Development Goal.
Development of the fatty liver disease Sustainable Development Goal score
The indicators included in the fatty liver disease–SDG score are shown in Table 1. We developed 2 sets of fatty liver disease–SDG scores. The first set was developed using 6 indicators [child wasting, child overweight, NCD mortality, a universal health coverage (UHC) service coverage index, health worker density, and education attainment] and excluded the urban green space (UGS) score as it was not available for all countries and territories. It covers 195 countries and territories between 1990 and 2017. The second set was constructed using all 7 indicators and includes only the 60 countries for which the UGS data were available in 2017.
TABLE 1.
List of indicators used to develop the fatty liver disease–SDG score
| Indicator | Indicator description | Source | Related SDG indicator | Group category |
|---|---|---|---|---|
| Child overweight | Prevalence of overweight in children aged 2–4 y (%) | GBD 2017 | 2.2.2 | Negative |
| Child wasting | Prevalence of wasting in children younger than 5 y (%) | GBD 2017 | 2.2.2 | Negative |
| NCD mortality | Age-standardized death rate due to cardiovascular disease, cancer, type 2 diabetes, and chronic respiratory disease in populations aged 30–70 y, per 100,000 population | GBD 2017 | 3.4.1 | Negative |
| UHC service coverage index | Coverage of essential health services, as defined by the UHC service coverage index of 9 tracer interventions and risk-standardized death rates or mortality-to-incidence ratios from 32 causes amenable to personal health carea | GBD 2017 | 3.8.1 | Positive |
| Health worker density | Health worker density per 1000 population, by cadre and summed across cadresb | GBD 2017 | 3.c.1 | Positive |
| Education | Age-standardized level of educational attainment for all ages 15–99 | GBD 2020 preliminary analysis | 4.1.2 | Positive |
| UGS score | Logarithm of total vegetation index per capitac | Kwon et al | 11.7.1 | Positive |
Thirty-two causes amenable to personal health care included tuberculosis, diarrheal diseases, lower respiratory infections, upper respiratory infections, chronic respiratory diseases, diphtheria, whooping cough, tetanus, measles, maternal disorders, neonatal disorders, colon and rectum cancer, nonmelanoma skin cancer, breast cancer, cervical cancer, uterine cancer, testicular cancer, Hodgkin lymphoma, leukemia, rheumatic heart disease, ischemic heart disease, cerebrovascular disease, hypertensive heart disease, peptic ulcer disease, appendicitis, hernia, gallbladder and biliary diseases, epilepsy, diabetes, chronic kidney disease, congenital heart anomalies, and adverse effects of medical treatment.
Cadres included physicians, nurses, midwives, and pharmacists.
Used the normalized difference vegetation index as a basis for the UGS indicator.
Abbreviations: GBD, Global Burden of Disease; NCD, noncommunicable disease; SDG, Sustainable Development Goal; UGS, urban green space; UHC, universal health coverage.
The estimates for child wasting, child overweight, NCD mortality, the UHC service coverage index, health worker density, and education attainment came from the “Global Burden of Disease (GBD), Injuries, and Risk Factors Study.”31–33 Details of the input data and modeling procedures for estimating these indicators have been published.34 The data for UGS were extracted from a published study conducted by Kwon et al.35 UGS is a globally comparable metric computed using Sentinel-2 satellite imagery data.36
We took an analytical approach similar to the GBD’s health-related SDG index to develop the fatty liver disease–SDG score. First, indicators were grouped into either a “positive” or “negative” category. The “positive” category consisted of indicators where higher estimates were associated with better health outcomes (eg, UHC service coverage index). The “negative” category consisted of indicators where lower estimates were associated with better health outcomes (eg, child wasting).
Then, all indicators were scaled from 0 to 100, with 0 denoting the worst observed performance and 100 reflecting the best performance, to make them comparable. To reduce the sensitivity of extreme outliers in a given location-year, we set the lower bound at the 2.5th percentile and the upper bound at the 97.5th percentile of the distribution for a given indicator. For “positive” indicators, any value below the 2.5th percentile was assigned a value of 0 and any value exceeding the 97.5th percentile was assigned a value of 100. The “negative” indicators were scaled and adjusted for outliers similarly but with 0 assigned to any value exceeding the 97.5th percentile and 100 assigned to any value below the 2.5th percentile, over the same study period. A modified scaling approach was applied to 2 indicators: NCD mortality and health worker density. Specifically, NCD mortality was scaled in log-space. Health worker density was scaled to reflect the density of each health worker cadre (ie, physicians, nurses, midwives, and pharmacists). The details of the modified scaling approach for health worker density have been published.34
The final fatty liver disease–SDG score was calculated in 2 steps. First, we computed the geometric mean of child wasting and child overweight, 2 indicators that fall under the same SDG target.34 Then, we computed the geometric mean of the remaining indicators, including the aggregate child wasting and child overweight score. In both steps, we restricted draws of each indicator score to a minimum value of 1 before computing the geometric mean to mitigate issues with values close to 0. To generate the fatty liver disease–SDG score for the 7 standard GBD super-regions,37 we aggregated the national-level, unscaled estimates of each indicator for each super-region, using population weights. Then, the national-level 2.5th and 97.5th percentile values for each indicator were applied to scale the indicators for each super-region location, before taking the geometric mean of the indicators, to produce the final fatty liver disease–SDG scores.
Every analytic step was carried out for 1000 draws from the posterior distribution of the previous step, to ensure uncertainty from all inputs, and analyses were propagated through to the final scores. Uncertainty intervals (UIs) were obtained by taking the 2.5th and 97.5th percentiles of the 1000 draw values.
Combining the fatty liver disease Sustainable Development Goal scores with the NAFLD preparedness index
In contrast to our fatty liver disease–SDG score, which aims to measure preparedness to address fatty liver disease from a multisectoral, whole-of-society perspective, the described NAFLD preparedness index2 reports on country preparedness to address NAFLD specifically from a health system and public health policy perspective. After the development of the fatty liver disease–SDG scores, we combined them with the NAFLD preparedness index for a more comprehensive assessment of countries’ fatty liver disease preparedness. Fatty liver disease–SDG scores for 100 countries included in the NAFLD preparedness index were extracted and then ranked. Two countries/territories included in the NAFLD preparedness index (Aruba and Hong Kong) were not included in the fatty liver disease–SDG score and, hence, were excluded. For these 100 countries, we summed the country rankings for the fatty liver disease–SDG score with the rankings of the NAFLD preparedness index.
Comparing the fatty liver disease Sustainable Development Goal scores to the NAFLD preparedness index and the Human Development Index
We separately compared the 2017 estimates of fatty liver disease–SDG scores to the NAFLD preparedness index2 and the Human Development Index (HDI).38 The HDI is a composite index of life expectancy, level of education attainment, and gross national income per capita that measures the overall human development of a country. It covers some of the themes also captured in the fatty liver disease–SDG score, namely, education; however, it does not incorporate key issues for fatty liver disease, such as UHC service coverage or access to UGSs, which are included in the fatty liver disease–SDG score. Two countries/territories (Aruba and Hong Kong) were excluded from the comparison analysis between fatty liver disease–SDG scores and the NAFLD preparedness index, whereas 7 countries/territories (Hong Kong, Liechtenstein, Palau, Saint Kitts and Nevis, San Marino, Eswatini, and Tuvalu) were excluded for the fatty liver disease–SDG score and HDI comparison.
RESULTS
The fatty liver disease–SDG scores for the 195 countries and territories vary substantially, from 14.6 (95% UI: 8.92 to 19.4) in Niger to 93.5 (91.6 to 95.3) in Japan, with 18 countries scoring > 85 on the 0 to100 scale (Figure 2A; Supplemental Table S1 and S2 http://links.lww.com/HEP/F1000 for country and territory scores from 1990 to 2017). The SD of the fatty liver disease–SDG score across all 195 countries and territories in 2017 is 18.58 and the interquartile range is 26.81. The SD and interquartile range of the fatty liver disease–SDG score by GBD super-region can be found in Supplemental Table S3 (http://links.lww.com/HEP/F1000).
FIGURE 2.
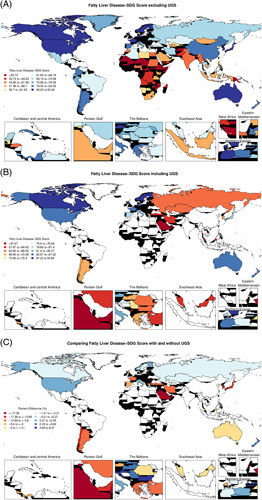
Geographical distribution of the fatty liver disease–SDG score, 2017. (A) Fatty liver disease SDG score in 195 countries and territories developed by using 6 indicators (child wasting, child overweight, NCD mortality, a UHC service coverage index, health worker density, and education attainment). (B) Fatty liver disease–SDG score in 60 countries and territories developed by using the 6 aforementioned indicators plus the UGS indicator. Countries and territories with no color indicate that they do not have UGS data. (C) Percentage change (%) of the fatty liver disease–SDG score with and without the UGS indicator in 60 countries that have UGS data. Percent change was calculated by first subtracting the fatty liver disease–SDG score developed without UGS data from the fatty liver disease–SDG score developed with UGS data and then dividing the difference by the fatty liver disease–SDG score without UGS data. Countries and territories with no color indicate that they do not have UGS data. Abbreviations: NCD, noncommunicable disease; SDG, Sustainable Development Goal; UGS, urban green space; UHC, universal health coverage.
Regionally, the high-income super-region had the highest score at 88.8 (95% UI: 87.3 to 90.1) in 2017, and south Asia had the lowest score at 44.1 (42.4 to 45.8). Between 1990 and 2017, the fatty liver disease–SDG score improved in all 7 super-regions, with the percentage increase ranging from 13.3% to 181.2% (Figure 3). The greatest improvement was in south Asia, despite its poor performance in absolute terms.
FIGURE 3.
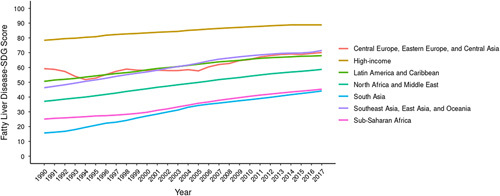
Temporal trend of the fatty liver disease–SDG score by GBD super-region, 1990 to 2017. Fatty liver disease–SDG score ranges from 0 to 100. The lines represent the population-weighted average of scores for countries and territories within each super-region. Abbreviations: GBD, Global Burden of Disease; SDG, Sustainable Development Goal.
Across the 195 countries and territories, the fatty liver disease–SDG score decreased (worsened) in 8 countries and territories during the study period, with the largest decrease in Guam [–27.9% (95% UI: –32.8 to –20.2)] (Supplemental Table S4 http://links.lww.com/HEP/F1000). In contrast, the biggest fatty liver disease–SDG score increase (improvement) was observed in Eritrea [1116.1% (531.3 to 1913.1)], followed by Ethiopia [645.9% (382.6 to 764.9)] and Laos [628.3% (324.0 to 1292.3)].
Of the 6 indicators that were used to develop the fatty liver disease–SDG score, the UHC service coverage index had the lowest average scaled value across all 195 countries and territories. This was consistent when restricted to the countries and territories with the bottom 20% of the fatty liver disease–SDG scores. The second lowest indicator, however, differed in those 2 groups. When compared across all 195 countries and territories, the indicator with the second lowest scaled value was NCD mortality, whereas, when restricted to the bottom 20%, the second lowest was education attainment.
For the 60 countries and territories where UGS data were available (Figure 2B, Supplemental Table S5 http://links.lww.com/HEP/F1000), the inclusion of the indicators had variable impacts on the fatty liver disease–SDG scores (Figure 2C). In 21 countries and territories (35%), the inclusion of UGS data improved the score, whereas in 39 countries and territories (65%), the score worsened with the inclusion of this indicator. The average percentage improvement in the score including UGS data was 2.62% (95% UI: 0.83 to 3.82), whereas the average decrease was 9.29% (7.04 to 11.92) (Figure 2C). Montenegro had the biggest improvement in score with the inclusion of UGS data (8.37%), whereas Bahrain had the largest decrease (51.4%).
Sweden had the highest overall combined rank when comparing the fatty liver disease–SDG score and NAFLD preparedness index (ranked fourth for the fatty liver disease–SDG score and third on the NAFLD preparedness index), whereas Central African Republic had the lowest (ranked 96th for the fatty liver disease–SDG score and joint 71st on the NAFLD preparedness index). Sweden, the UK, Belgium, Germany, and Israel ranked in the top 15 on both indices. The largest difference between the fatty liver disease–SDG score and the NAFLD preparedness index was seen in India, which ranked 88th on the former and first on the latter (Supplemental Table S6 http://links.lww.com/HEP/F1000).
The comparisons of the national fatty liver disease–SDG scores to the NALFD preparedness index and HDI are shown in Figure 4 (Supplemental Tables S7 and S8 http://links.lww.com/HEP/F1000). Although many countries across all 7 GBD super-regions had near zero NAFLD preparedness index values, countries with higher fatty liver disease–SDG scores were more likely to score higher on the NAFLD preparedness index. A few notable exceptions were found. India and Bulgaria, 2 countries with suboptimal fatty liver disease–SDG scores, had some of the highest NAFLD preparedness index values. The correlation was higher, but not 100%, between the fatty liver disease–SDG score and the HDI.
FIGURE 4.
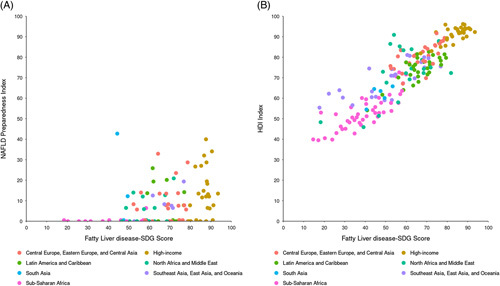
Comparisons of the fatty liver disease–SDG score to the (A) NAFLD preparedness index and (B) HDI by GBD super-region. The fatty liver disease–SDG score, NAFLD preparedness index, and HDI range from 0 to 100. The dots represent the population-weighted average of scores for countries and territories within each super-region. Abbreviations: GBD, Global Burden of Disease; HDI, Human Development Index; SDG, Sustainable Development Goal.
DISCUSSION
There have been increasingly frequent calls to focus on systems thinking and to develop new tools to conceptualize and implement the complex responses needed to address today’s major health challenges,22 including the partnerships and collaborations that sit at the center of systems responses. In this study, we present a score for 195 countries and territories (1990–2017), which uses the SDG framework as a lens through which to assess countries’ preparedness to tackle fatty liver disease. The burden of fatty liver disease is high3 and rapidly increasing,39 and it is already the fastest growing cause of HCC in France, the UK, and the USA. The incidence of NAFLD-related HCC is projected to increase dramatically by 2030, with increases of 82%, 117%, and 122% from 2016 in China, France, and the USA, respectively.40 Fatty liver disease is an archetypical public health issue of the 21st century, requiring action across a wide range of sectors and disciplines. Although the focus of this study was fatty liver disease, the findings have broader relevance to NCDs, especially to closely related conditions, such as type 2 diabetes mellitus, cardiovascular disease, and obesity.
We suggest the fatty liver disease–SDG score for 3 primary uses. Given the lack of awareness about fatty liver disease and the importance of a multisectoral approach in tackling this public health challenge, the score can help to create awareness among key stakeholder groups, within and beyond the health sector. Second, the score can be an advocacy tool for public health professionals, civil society, and patient groups to advocate for greater action across sectors on this neglected public health challenge, at national and global levels. Finally, the score can inform the strategic decision-making within the national, regional, and global liver and other NCD organizations about the types of cross-sectoral actors that they should be engaging and collaborating with. While there is some correlation between the fatty liver disease–SDG score and existing scores, such as the HDI, the new score provides a more granular focus on the key issues impacting fatty liver disease and will support more nuanced discussions at a strategic and policy level. If the score is updated periodically (eg, every 3–5 years), advocates can also use it to scrutinize success and challenges over time, including policy changes. The fatty liver disease–SDG score provides a holistic multisectoral lens, through which to view efforts to address fatty liver disease, complementing existing efforts, such as the NAFLD preparedness index, which takes a focused look at health system and public health responses within countries. Furthermore, the data used to calculate the score are regularly and consistently collected for 195 countries and territories, while the preparedness index had data from only 102 countries.2
As expected, high-income countries generally had higher fatty liver disease–SDG scores than low-income and lower middle-income countries. There were some notable exceptions, including Uruguay, Brunei, and Qatar, none of which scored in the top quartile. This highlights that advanced economic development is not a guarantee of a higher fatty liver disease–SDG score, emphasizing the importance of focused policy interventions aimed at addressing the underlying and direct drivers of public health. These may, for example, target inadequate nutrition and sedentary lifestyles at the population level.41 Although fatty liver disease is a pressing public health problem, no country is yet fully prepared to address it.25 Geographically, sub-Saharan Africa and south Asia were the GDB super-regions with the lowest scores; however, some countries in these regions performed well overall, such as Cabo Verde and Botswana, which both ranked higher than other more economically advanced countries, highlighting that low- and middle-income countries can take strides in preparing to address conditions such as fatty liver disease.
For the 60 countries where UGS data were available, the inclusion of this indicator had varying impacts on the overall score, improving it in just over one-third of countries and reducing it in the remainder, in the case of Bahrain by over 50%. Although we were unable to include UGS data in the score for all countries and territories, we believe that this indicator captures critical information on the environment in which people live. Importantly, the availability of UGS does not guarantee access and utilization, 2 points that are not reflected in our score. The use of UGS is impacted by socioeconomic and sociocultural factors,42,43 and efforts to increase its availability need to be accompanied by interventions to increase access and use, such as improved security and lighting. This is especially important among those who can benefit the most from using such space, including people at a higher risk of fatty liver disease and other NCDs, considering that UGS has effects on both physical and mental health.
Whole-of-society and health system responses
We combined the ranking of countries and territories on the fatty liver disease–SDG score with a published NAFLD preparedness index.2 While the fatty liver disease–SDG score provides a multisectoral perspective that speaks to a country’s action on fatty liver disease and NCDs more broadly, the NAFLD preparedness index gives insights into the relevant health system policy, guidelines, and strategies that are in place to address NAFLD. By comparing how well countries performed across both indices, we aimed to provide a holistic view of a country’s preparedness to address this public health challenge. Countries that rank highly on both the fatty liver disease–SDG and NAFLD preparedness indices are best prepared to address the challenge of fatty liver disease. The NAFLD preparedness index found substantial variation between countries’ readiness to address NAFLD. Notably, even those countries that score relatively highly exhibit deficiencies in key domains, suggesting that structural changes are needed to optimize NAFLD management and ensure that effective public health approaches are in place.42 Further detailed analysis at the regional level of countries and territories ranking highly on both indices could provide useful case studies to understand the policy measures that have been implemented and how these could be implemented in other national or subnational contexts.
Informing national responses to fatty liver disease
While national development priorities vary, fatty liver disease and NCDs—more broadly—are important considerations for decision-makers in all countries. For example, in low-income and lower middle–income countries, where public health issues have traditionally focused on communicable diseases, NCDs are becoming a major cause of morbidity and mortality,44,45 with important implications for individual health, health systems, and economic development.46,47
Fatty liver disease, to date, is not addressed in global health policy or technical guidance. Improving public health is a central pillar of the SDG agenda48 and should be a primary goal in all countries as a means of driving economic and social progress. While health system preparedness, underpinned by achieving UHC and health equity, is crucial, the underlying causes of fatty liver disease and other highly prevalent diseases cannot be addressed in the health sector alone. Our findings re-emphasize the longstanding calls for health in all policies’ approaches.
Several indicators in this fatty liver disease–SDG score, namely, education attainment and UGS, fall beyond the direct scope of the public health community, pointing to the need to engage across various sectors, and for the public health community to support and champion the work of other sectors. Successful multisectoral action requires strong governance mechanisms that enable different stakeholders to collaborate around shared goals. Such governance structures are frequently missing or insufficient, especially in low- and middle-income countries, where institutions are commonly weak and fragmentation is common.49 More detailed analysis is still needed to understand how multisectoral action can best work in practice.
Limitations
This study has several limitations. There is variation in the clinical definition of fatty liver disease and countries may monitor the disease using different methods. Hence, the full burden and impact of the disease are unknown, precluding the potential to externally validate the fatty liver disease–SDG score using the estimated disease burden of fatty liver disease and NASH in each country. While such a validation would theoretically show if high-scoring countries have a lower disease burden and vice versa, interpretation of such an analysis is challenging, in part because primary data on fatty liver disease prevalence are scant and heterogeneous. Changes in fatty liver disease epidemiology occur slowly over time; in theory, the fatty liver disease–SDG scores for 1990, 2000, and 2010 will provide useful insights into the disease burden today, yet the myriad of confounding factors and data quality over this time makes such comparisons fraught.
Furthermore, we recognize that our combination of the fatty liver disease–SDG score with the NAFLD preparedness index uses data from different timepoints, with the former using data from 2017—the latest available data—and the latter from 2020. However, we suggest that it is unlikely that the fatty liver disease–SDG score will have changed substantially between these timepoints and find value in the aggregate score.
One SDG indicator (16.1.4: proportion of population that feel safe walking alone around the area they live after dark) was included in the NAFLD–SDG framework;26 however, data for this indicator were unavailable to include in the fatty liver disease–SDG score.30 We note that the metric for UGS was developed using data from only 90 cities within the 60 countries and territories included and may, thus, not be an accurate representation of UGS throughout each country and territory. We also had no information available regarding the quality of UGS scores. For example, there is uncertainty as to whether UGS practically relates to better walkability and ability to perform outdoor exercise, as UGS has different factors for usability not captured in a single metric, including safety and environmental health risks.50,51
We present a fatty liver disease–SDG score for 195 countries and territories over 3 decades, with the aim of supporting efforts to address the public health challenge of fatty liver disease through a whole-of-society approach. Fatty liver disease remains a high-prevalence, largely unknown, and underaddressed disease, yet one that will have an increasing impact on health, health systems, and economies in the years ahead. The fatty liver disease–SDG score can help support efforts to raise awareness about fatty liver disease and ultimately assist all levels of policy-making processes to address it.
AUTHOR CONTRIBUTIONS
Jeffrey V. Lazarus: conceived the idea for this study and prepared a proposal to IHME with Henry E. Mark. They also prepared the first draft of the manuscript. Hannah Han and M. Ashworth Dirac: led the data collection. Manik Aggarwal, Ali Ahmadi, Fares Alahdab, Motasem Alkhayyat, Sami Almustanyir, Hubert Amu, Tahira Ashraf, Bantalem Tilaye Tilaye Atinafu, Sara Bagherieh, Mainak Bardhan, Diana Fernanda Bejarano Ramirez, Ajay Nagesh Bhat, Vijay Kumar Chattu, Daniela Contreras, Sandra Cortés, Omar B Da’ar, Bardia Danaei, Rupak Desai, M Ashworth Dirac, Haneil Larson Dsouza, Temitope Cyrus Ekundayo, Iman El Sayed, Noha Mousaad Elemam, Sayeh Ezzikouri, Amr Farwati, Farshad Farzadfar, Ginenus Fekadu, Tushar Garg, Mahaveer Golechha, Pouya Goleij, Vivek Kumar Gupta, Adel Hajj Ali, Saeed S Hamid, Harapan Harapan, Simon I Hay, Reza Homayounfar, Salman Hussain, Segun Emmanuel Ibitoye, Nahlah Elkudssiah Ismail, Linda Merin J, Shubha Jayaram, Bijay Mukesh Jeswani, Jost B Jonas, Abel Joseph, Charity Ehimwenma Joshua, Jacek Jerzy Jozwiak, Vidya Kadashetti, Tesfaye K Kanko, Rami S Kantar, Nitin Kapoor, Moien AB Khan, Sang-woong Lee, Yeong Yeh Lee, Lee-Ling Lim, Stephen S Lim, Stefan Lorkowski, Erkin M Mirrakhimov, Awoke Misganaw, Ali H Mokdad, Jibran Sualeh Muhammad, Efrén Murillo-Zamora, Christopher J L Murray, Sreenivas Narasimha Swamy, Zuhair S Natto, Robina Khan Niazi, Bogdan Oancea, In-Hwan Oh, Jagadish Rao Padubidri, Seoyeon Park, Harsh K Patel, Venkata Suresh Patthipati, Simone Perna, Vivek Podder, Sina Rashedi, Jefferson Antonio Buendia Rodriguez, Leonardo Roever, Umar Saeed, Abdallah M Samy, Danish Iltaf Satti, Allen Seylani, Pritik A Shah, Ali Shamekh, Parnian Shobeiri, Jasvinder A Singh, Anna Aleksandrovna Skryabina, Ker-Kan Tan, Nikhil Kenny Thomas, Tommi Juhani Vasankari, Song Wang, Suowen Xu, Chuanhua Yu, and Zhi-Jiang Zhang: provided data or critical feedback on data sources. Ali Ahmadi, Hubert Amu, Akshaya Srikanth Bhagavathula, Daniela Contreras, M Ashworth Dirac, Adel Hajj Ali, Simon I Hay, Bijay Mukesh Jeswani, Sang-woong Lee, Ali H Mokdad, Christopher J L Murray, Seoyeon Park, Umar Saeed, Abdallah M Samy, and Theo Vos: developed methods or computational machinery. Amirali Aali, Mohsen Abbasi-Kangevari, Eman Abu-Gharbieh, Manik Aggarwal, Bright Opoku Ahinkorah, Ali Ahmadi, Fares Alahdab, Sami Almustanyir, Hubert Amu, Amir Anoushiravani, Sina Azadnajafabad, Sara Bagherieh, Mainak Bardhan, Diana Fernanda Bejarano Ramirez, Akshaya Srikanth Bhagavathula, Ajay Nagesh Bhat, Mariah Malak Bilalaga, Antonio Biondi, Saeid Bitaraf, Srinivasa Rao Bolla, Daniela Calina, Vijay Kumar Chattu, Sandra Cortés, Omar B Da’ar, Bardia Danaei, Rupak Desai, M Ashworth Dirac, Deepa Dongarwar, Haneil Larson Dsouza, Iman El Sayed, Noha Mousaad Elemam, Mohamed A Elmonem, Aisha Elsharkawy, Sayeh Ezzikouri, Amr Farwati, Florian Fischer, Tushar Garg, Elena S George, Seyyed-Hadi Ghamari, Mohammad Ghasemi Nour, Vivek Kumar Gupta, Parham Habibzadeh, Adel Hajj Ali, Saeed S Hamid, Harapan Harapan, Sanam Hariri, Abbas M Hassan, Simon I Hay, Yuta Hiraike, Reza Homayounfar, Mohammad-Salar Hosseini, Sedighe Hosseini Shabanan, Vivian Chia-rong Hsieh, Junjie Huang, Salman Hussain, Segun Emmanuel Ibitoye, Olayinka Stephen Ilesanmi, Nahlah Elkudssiah Ismail, Chidozie C D Iwu, Linda Merin J, Shubha Jayaram, Bijay Mukesh Jeswani, Jost B Jonas, Abel Joseph, Jacek Jerzy Jozwiak, Ali Kabir, Ali Kabir, Vidya Kadashetti, Tesfaye K Kanko, Rami S Kantar, Nitin Kapoor, Joonas H Kauppila, Moien AB Khan, Min Seo Kim, Carlo La Vecchia, Bagher Larijani, Yeong Yeh Lee, Lee-Ling Lim, Chun-Han Lo, Stefan Lorkowski, Jamal Majidpoor, Mohammad-Reza Malekpour, Yasaman Mansoori, Miquel Martorell, Alexios-Fotios A Mentis, Tuomo J Meretoja, Tomislav Mestrovic, Awoke Misganaw, Abdollah Mohammadian-Hafshejani, Ali H Mokdad, Jibran Sualeh Muhammad, Efrén Murillo-Zamora, Christopher JL Murray, Mukhammad David Naimzada, Sreenivas Narasimha Swamy, Hasan Nassereldine, Zuhair S Natto, Robina Khan Niazi, Virginia Nuñez-Samudio, Bogdan Oancea, Antonio Olivas-Martinez, Jagadish Rao Padubidri, Seoyeon Park, Harsh K Patel, Venkata Suresh Patthipati, Gayatri Pemmasani, Simone Perna, Vivek Podder, Akila Prashant, Pradhum Ram, Indu Ramachandra Rao, Jefferson Antonio Buendia Rodriguez, Leonardo Roever, Gholamreza Roshandel, Umar Saeed, Amirhossein Sahebkar, Soumya Swaroop Sahoo, Abdallah M Samy, Chinmoy Sarkar, Danish Iltaf Satti, Allen Seylani, Elaheh Shaker, Parnian Shobeiri, Seyed Afshin Shorofi, Jasvinder A Singh, Paramdeep Singh, Anna Aleksandrovna Skryabina, Joan B Soriano, Majid Taheri, Ker-Kan Tan, Samar Tharwat, Bereket M Tigabu, Marco Vacante, Rohollah Valizadeh, Tommi Juhani Vasankari, Cong Wang, Song Wang, Nuwan Darshana Wickramasinghe, Mazyar Zahir, and Shira Zelber-Sagi: provided critical feedback on methods or results.
ACKNOWLEDGMENTS
Jeffrey V. Lazarus and Trenton M. White acknowledge support to ISGlobal from the grant CEX2018-000806-S funded by MCIN/AEI/10.13039/501100011033 and the “Generalitat de Catalunya” through the CERCA Program, outside of the submitted work. M. Ashworth Dirac acknowledges support from the Global Public Goods Grant from Bill & Melinda Gates Foundation, outside of the submitted work. Aqeel Ahmad thanks the Deanship of Scientific Research at Shaqra University for supporting this work. Salman Hussain acknowledges support from the Operational Programme Research, Development and Education Project, Postdoc2MUNI (No. CZ.02.2.69/0.0/0.0/18_053/0016952), outside of the submitted work. Virginia Nuñez-Samudio acknowledges support from Panamá’s La Secretaría Nacional de Ciencia, Tecnología e Innovación (Senacyt), as a member of the Sistema Nacional de Investigación (SNI), outside of the submitted work. Jagadish Rao Padubidri acknowledges support from Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal in supporting collaborative research, outside of the submitted work. Abdallah M Samy acknowledges the support from Ain Shams University and the Egyptian Fulbright Mission Program, outside of the submitted work.
The GBD Fatty Liver Disease Sustainable Development Goal Collaborators
Jeffrey V. Lazarus1,2,3,4, Hannah Han5, Henry E. Mark2, Saleh A. Alqahtani6, Jörn M. Schattenberg7, Joan B. Soriano8,9, Trenton M. White1, Shira Zelber-Sagi10,11, M. Ashworth Dirac5,12, Amirali Aali13, Mohsen Abbasi-Kangevari14, Eman Abu- Gharbieh15, Osama Abu-Shawer16, Manik Aggarwal16, Bright Opoku Ahinkorah17, Aqeel Ahmad18, Ali Ahmadi19,20, Fares Alahdab21, Motasem Alkhayyat16, Sami Almustanyir22,23, Hubert Amu24, Amir Anoushiravani25, Tahira Ashraf26, Bantalem Tilaye Tilaye Atinafu27, Sina Azadnajafabad14, Nayereh Baghcheghi28, Sara Bagherieh29, Mainak Bardhan30,31, Diana Fernanda Bejarano Ramirez32,33, Akshaya Srikanth Bhagavathula34, Neeraj Bhala35,36, Ajay Nagesh Bhat37, Mariah Malak Bilalaga37, Antonio Biondi39, Saeid Bitaraf40, Srinivasa Rao Bolla41, Antoine Boustany16, Daniela Calina42, Ismael R. Campos-Nonato43, Vijay, Kumar Chattu44,45, Sheng-Chia Chung46,47, Daniela Contreras48, Sandra Cortés49,50, Omar B. Da’ar51, Omid Dadras52,53, Xiaochen Dai5,54, Bardia Danaei55, Rupak Desai56, Shirin Djalalinia57, Deepa Dongarwar58, Haneil Larson Dsouza59,60, Temitope Cyrus Ekundayo61, Iman El Sayed62, Noha Mousaad Elemam63, Mohamed A. Elmonem64, Aisha Elsharkawy65, Sayeh Ezzikouri66, Amr Farwati67, Farshad Farzadfar14, Ginenus Fekadu68,69, Florian Fischer70, Tushar Garg71, Elena S. George72, Seyyed-Hadi Ghamari14,73, Mohammad Ghasemi Nour74, Amit Goel75, Mahaveer Golechha76, Pouya Goleij77, Vivek Kumar Gupta78, Parham Habibzadeh79, Adel Hajj Ali80, Saeed S. Hamid81, Harapan Harapan82, Sanam Hariri25,83, Maryam Hashemian25,84 Abbas M. Hassan85, Mohammed Bheser Hassen5,86, Simon I. Hay5,87, Yuta Hiraike88, Reza Homayounfar89,90, Mohammad-Salar Hosseini91, Sedighe Hosseini Shabanan92, Soodabeh Hoveidamanesh93, Vivian Chia-rong Hsieh94, Junjie Huang95, Salman Hussain96,97, Segun Emmanuel Ibitoye98, Olayinka Stephen Ilesanmi99,100, Nahlah Elkudssiah Ismail101, Chidozie CD Iwu102, Linda Merin J103, Elham Jamshidi104,105, Umesh Jayarajah106,107, Shubha Jayaram108, Bijay ghMukesh Jeswani109, Jost B. Jonas110,111, Abel Joseph16, Charity Ehimwenma Joshua112, Jacek Jerzy Jozwiak113, Ali Kabir114, Vidya Kadashetti115, Tesfaye K. Kanko116, Rami S Kantar117,118, Nitin Kapoor119,120, Ibraheem M. Karaye121, Joonas H. Kauppila122,123, Mohammad Keykhaei14,124, Moien A.B. Khan125,126, Min Seo Kim127,128, Hamid Reza Koohestani129, Ambily Kuttikkattu130, Carlo La Vecchia131, Bagher Larijani132, Sang-woong Lee133, Yeong Yeh Lee134,135, Lee-Ling Lim136,137, Stephen S. Lim5,54, Chun-Han Lo138, Stefan Lorkowski139,140, Jamal Majidpoor141, Mohammad- Reza Malekpour14, Yasaman Mansoori142, Miquel Martorell143,144, Sahar Masoudi25, Alexios-Fotios A. Mentis145, Tuomo J. Meretoja146,147, Tomislav Mestrovic148,5, Erkin M. Mirrakhimov149,150, Awoke Misganaw87,151, Abdollah Mohammadian-Hafshejani19, Ali H. Mokdad5,87, Jibran Sualeh Muhammad152, Efrén Murillo-Zamora153,154, Christopher J. L. Murray5,54, Mukhammad David Naimzada155,156, Sreenivas Narasimha Swamy157, Hasan Nassereldine5, Zuhair S. Natto158,159, Robina Khan Niazi160, Virginia Nuñez- Samudio161,162, Bogdan Oancea163, In-Hwan Oh164, Olubunmi Omotola Oladunjoye165, Antonio Olivas-Martinez166,167, Jagadish Rao Padubidri168, Seoyeon Park, Beng169, Harsh K. Patel170, Ronit Patnaik Patnaik171, Venkata Suresh Patthipati172,173, Gayatri Pemmasani174, Simone Perna175, Vivek Podder176,177, Akram Pourshams25, Akila Prashant178, Pradhum Ram179, Indu Ramachandra Rao180, Sina Rashedi181,182, Mohammad-Mahdi Rashidi14,73, Negar Rezaei14,132, Jefferson Antonio Buendia Rodriguez183, Leonardo Roever184, Gholamreza Roshandel185, Bahar Saberzadeh- Ardestani186, Umar Saeed187,188, Sher Zaman Safi189,190, Amirhossein Sahebkar191,192, Soumya Swaroop Sahoo193, Mohammad Amin Salehi194, Abdallah M. Samy195,196, Senthilkumar Sankararaman197,198, Chinmoy Sarkar199, Danish Iltaf Satti200, Allen Seylani201, Pritik A. Shah202,203, Elaheh Shaker182,204, Ali Shamekh205,206, Parnian Shobeiri207,204, Seyed Afshin Shorofi208,29, Jasvinder A. Singh210,211, Paramdeep Singh212, Md Shahjahan Siraj213, Anna Aleksandrovna Skryabina214, Amir Ali Sohrabpour25, Keita Suzuki215, Majid Taheri216,217, Ker-Kan Tan218, Samar Tharwat219, Nikhil Kenny Thomas220, Bereket M. Tigabu221, Marco Vacante39, Seyed Mohammad Vahabi194, Rohollah Valizadeh222, Tommi Juhani Vasankari223,224, Theo Vos5,54, Cong Wang225, Song Wang226, Nuwan Darshana Wickramasinghe227, Suowen Xu228,229, Chuanhua Yu230, Ismaeel Yunusa231, Mazyar Zahir232, Moein Zangiabadian233, Zhi-Jiang Zhang234
1Barcelona Institute for Global Health (ISGlobal), Hospital Clínic, University of Barcelona, Barcelona, Spain; 2EASL International Liver Foundation, Geneva, Switzerland; 3Faculty of Medicine and Health Sciences, University of Barcelona, Barcelona, Spain; 4CUNY Graduate School of Public Health and Health Policy (CUNY SPH), New York, New York, USA; 5Institute for Health Metrics and Evaluation, University of Washington, Seattle, Washington, USA; 6Organ Transplant Center, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia; 7Department of Medicine, Metabolic Liver Research Program, University Medical Center, Mainz, Germany; 8Respiratory Department, Hospital Universitario de la Princesa; School of Medicine, Universidad Autónoma de Madrid, Madrid, Spain; 9Centro de Investigación en Red de Enfermedades Respiratorias (CIBERES), Instituto de Salud Carlos III (ISCIII), Madrid, Spain; 10School of Public Health, University of Haifa, Haifa, Israel; 11Department of Gastroenterology, Tel Aviv Medical Center, Tel Aviv, Israel; 12Department of Health Metrics Sciences, Department of Family Medicine, University of Washington, Seattle, Washington, USA; 13Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran; 14Non-communicable Diseases Research Center, Tehran University of Medical Sciences, Tehran, Iran; 15Clinical Sciences Department, University of Sharjah, Sharjah, United Arab Emirates; 16Department of Internal Medicine, Cleveland Clinic, Cleveland, Ohio, USA; 17School of Public Health, University of Technology Sydney, Sydney, New South Wales, Australia; 18Department of Medical Biochemistry, Shaqra University, Shaqra, Saudi Arabia; 19Department of Epidemiology and Biostatistics, Shahrekord University of Medical Sciences, Shahrekord, Iran; 20Department of Epidemiology, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 21Mayo Evidence-based Practice Center, Mayo Clinic Foundation for Medical Education and Research, Rochester, Minnesota, USA; 22College of Medicine, Alfaisal University, Riyadh, Saudi Arabia; 23Ministry of Health, Riyadh, Saudi Arabia; 24Department of Population and Behavioral Sciences, University of Health and Allied Sciences, Ho, Ghana; 25Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran; 26University Institute of Radiological Sciences and Medical Imaging Technology, The University of Lahore, Lahore, Pakistan; 27School of Nursing and Midwifery Science, Debre Berhan University, Debre Berhan, Ethiopia; 28Nursing, Saveh University of Medical Sciences, Saveh, Iran; 29School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran; 30Department of Molecular Microbiology and Bacteriology, National Institute of Cholera and Enteric Diseases, Kolkata, West Bengal, India; 31Department of Molecular Microbiology, Indian Council of Medical Research, New Delhi, India; 32Department of Medicine, El Bosque University, Bogota, Colombia; 33Transplant Service Unit, University Hospital Foundation Santa Fe de Bogotá, Bogota, Colombia; 34Department of Health, Human Performance and Recreation, University of Arkansas, Fayetteville, Arkansas, USA; 35Institutes of Applied Health Research and Translational Medicine, Queen Elizabeth Hospital Birmingham, Birmingham, UK; 36Institute of Applied Health Research, University of Birmingham, Birmingham, UK; 37Department of General Medicine, Manipal Academy of Higher Education, Mangalore, Karnataka, India; 38Department of Clinical Sciences, University of Sharjah, Sharjah, United Arab Emirates; 39Department of General Surgery and Medical- Surgical Specialties, University of Catania, Catania, Italy; 40Department of Biostatistics and Epidemiology, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran; 41Department of Biomedical Sciences, Nazarbayev University, Nur-Sultan City, Kazakhstan; 42Department of Clinical Pharmacy, University of Medicine and Pharmacy, Craiova, Romania; 43Health and Nutrition Research Center, National Institute of Public Health, Cuernavaca, Mexico; 44Department of Community Medicine, Datta Meghe Institute of Medical Sciences, Sawangi, Maharashtra, India; 45Saveetha Medical College and Hospitals, Saveetha University, Chennai, India; 46Department of Health Informatics, University College London, London, UK; 47Health Data Research UK, London, UK; 48Clinical Epidemiology, National Autonomous University of Mexico, Mexico City, Mexico; 49Department of Public Health, Pontifical Catholic University of Chile, Santiago, Chile; 50Research Line in Environmental Exposures and Health Effects at Population Level, Centro de Desarrollo Urbano Sustentable (CEDEUS) [Advanced Center for Chronic Diseases (ACCDIS)], Santiago, Chile; 52Department of Health Systems Management, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 52Section of Global Health and Rehabilitation, Western Norway University of Applied Sciences, Bergen, Norway; 53Department of Global Public Health and Primary Care, University of Bergen, Bergen, Norway; 54Department of Health Metrics Sciences, University of Washington, Seattle, Washington, USA; 55Department of Medical Science, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 56Division of Cardiology, Atlanta Veterans Affairs Medical Center, Decatur, Georgis, USA; 57Development of Research and Technology Center, Ministry of Health and Medical Education, Tehran, Iran; 58Health Science Center, University of Texas, Houston, Texas, USA; 59Forensic Medicine and Toxicology, Kasturba Medical College Mangalore, Manipal Academy of Higher Education, Mangalore, Karnataka, India; 60Forensic Medicine and Toxicology, Kasturba Medical College Mangalore, Mangalore, Dakshina Kannada District, Karnataka, India; 61Department of Biological Sciences, University of Medical Sciences, Ondo, Ondo, Nigeria; 62Biomedical Informatics and Medical Statistics Department, Alexandria University, Alexandria, Egypt; 63Sharjah Institute for Medical Research, University of Sharjah, Sharjah, United Arab Emirates; 64Egypt Center for Research and Regenerative Medicine (ECRRM), Cairo, Egypt; 65Department of Endemic Medicine and Hepatogastroenterology, Cairo University, Cairo, Egypt; 66Department of Virology, Pasteur Institute of Morocco, Casablanca, Morocco; 67Internal Medicine Department, Hamad Medical Corporation, Doha, Qatar; 68School of Pharmacy, The Chinese University of Hong Kong, Hong Kong, China; 69Department of Pharmacy, Wollega University, Nekemte, Ethiopia; 70Institute of Public Health, Charité Medical University Berlin, Berlin, Germany; 71Department of Radiology, King Edward Memorial Hospital, Mumbai, Maharashtra, India; 72Institute for Physical Activity and Nutrition, Deakin University, Melbourne, Victoria, Australia; 73Social Determinants of Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 74E-Learning Center, Mashhad University of Medical Sciences, Mashhad, Iran; 75Department of Hepatology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India; 76Department of Health Systems and Policy Research, Indian Institute of Public Health, Gandhinagar, Gujrat, India; 77Department of Genetics, Sana Institute of Higher Education, Sari, Iran; 78Macquarie University, Sydney, Ne South Wales, Australia; 79School of Medicine, University of Maryland, Baltimore, Maryland, USA; 80Heart, Vascular, Thoracic Institute, Cleveland Clinic, Cleveland, Ohio, USA; 81Department of Medicine, Aga Khan University, Karachi, Pakistan; 82Medical Research Unit, Syiah Kuala University, Banda Aceh, Indonesia; 83Research Institute for Primordial Prevention of Non-Communicable Disease, Isfahan University of Medical Sciences, Isfahan, Iran; 84Biology Department, Utica University, Utica, New York, USA; 85Department of Plastic Surgery, University of Texas, Houston, Texas, USA; 86National Data Management Center for Health (NDMC), Ethiopian Public Health Institute, Addis Ababa, Ethiopia; 87Department of Health Metrics Sciences, School of Medicine, University of Washington, Seattle, Washington, USA; 88Division for Health Service Promotion, University of Tokyo, Tokyo, Japan; 89Non-communicable Diseases Research Center, Fasa University of Medical Sciences, Fasa, Iran; 90National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 91Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran; 92School of Medicine, Tehran University of Medical Sciences, Tehran, Iran; 93Burn Research Center, Shahid Motahari Hospital, Tehran, Iran; 94Department of Health Services Administration, China Medical University, Taichung, Taiwan; 95Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong, China; 96Czech National Centre for Evidence-Based Healthcare and Knowledge Translation, Masaryk University, Brno, Czech Republic; 97Institute of Biostatistics and Analyses, Masaryk University, Brno, Czech Republic; 98Department of Health Promotion and Education, University of Ibadan, Ibadan, Nigeria; 99Department of Community Medicine, University of Ibadan, Ibadan, Nigeria; 100Department of Community Medicine, University College Hospital, Ibadan, Ibadan, Nigeria; 101Department of Clinical Pharmacy, MAHSA University, Bandar Saujana Putra, Malaysia; 102School of Health Systems and Public Health, University of Pretoria, Pretoria, South Africa; 103Department of Orthodontics and Dentofacial Orthopedics, Dr. D. Y. Patil University, Pune, Maharashtra, India; 104Functional Neurosurgery Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 105 Division of Pulmonary Medicine, Lausanne University Hospital (CHUV), Lausanne, Switzerland; 106Postgraduate Institute of Medicine, University of Colombo, Colombo, Sri Lanka; 107Department of Surgery, National Hospital, Colombo, Sri Lanka; 108Department of Biochemistry, Government Medical College, Mysuru, Karnataka, India; 109Department of Internal Medicine, GCS Medical College, Hospital and Research Centre, Ahmedabad, Gujrat, India; 110Institute of Molecular and Clinical Ophthalmology Basel, Basel, Switzerland; 111Department of Ophthalmology, Heidelberg University, Mannheim, Germany; 112Department of Economics, National Open University, Benin City, Nigeria; 113Department of Family Medicine and Public Health, University of Opole, Opole, Poland; 114Minimally Invasive Surgery Research Center, Iran University of Medical Sciences, Tehran, Iran; 115Department of Oral and Maxillofacial Pathology, Krishna institute of Medical Sciences Deemed to be University, Karad, Maharashtra, India; 116Department of Biomedical sciences, Arba Minch University, Arba Minch, Ethiopia; 117The Hansjörg Wyss Department of Plastic and Reconstructive Surgery, Nab’a Al-Hayat Foundation for Medical Sciences and Health Care, New York, New York, USA; 118Cleft Lip and Palate Surgery Unit, Global Smile Foundation, Norwood, Massachusetts, USA; 119Department of Endocrinology, Diabetes and Metabolism, Christian Medical College and Hospital (CMC), Vellore, Tamil Nadu, India; 120Implementation Science Lab, Baker Heart and Diabetes Institute, Melbourne, Australia; 121School of Health Professions and Human Services, Hofstra University, Hempstead, New York, USA; 122Surgery Research Unit, University of Oulu, Oulu, Finland; 123Department of Molecular Medicine and Surgery, Karolinska Institute, Stockholm, Sweden; 124Students’ Scientific Research Center (SSRC), Tehran University of Medical Sciences, Tehran, Iran; 125Family Medicine Department, United Arab Emirates University, Al Ain, United Arab Emirates; 126Primary Care Department, NHS North West London, London, UK; 127Department of Genomics and Digital Health, Samsung Advanced Institute for Health Sciences and Technology (SAIHST), Seoul, South Korea; 128Public Health Center, Ministry of Health and Welfare, Wando, South Korea; 129Social Determinants of Health Research Center, Saveh University of Medical Sciences, Saveh, Iran; 130Department of Nephrology, Pushpagiri Institute of Medical Sciences and Research Centre, Thiruvalla, Kerala, India; 131Department of Clinical Sciences and Community Health, University of Milan, Milan, Italy; 132Endocrinology and Metabolism Research Institute, Tehran University of Medical Sciences, Tehran, Iran; 133Pattern Recognition and Machine Learning Lab, Gachon University, Seongnam, South Korea; 134Department of Medicine, University of Science Malaysia, Kota Bharu, Malaysia; 135School of Medical Sciences, University of Science Malaysia, Kota Bharu, Malaysia; 136Department of Medicine, University of Malaya, Kuala Lumpur, Malaysia; 137Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Shatin, New Taiwan, China; 138Department of Internal Medicine, Kirk Kerkorian School of Medicine at UNLV, Las Vegas, Nevada, USA; 139Institute of Nutritional Sciences, Friedrich Schiller University Jena, Jena, Germany; 140Competence Cluster for Nutrition and Cardiovascular Health (nutriCARD), Jena, Germany; 142Department of Anatomy, Gonabad University of Medical Sciences, gonabad, Iran; 143Shiraz University of Medical Sciences, Shiraz, Iran; 144Department of Nutrition and Dietetics, University of Concepcion, Concepción, Chile; 144Centre for Healthy Living, University of Concepción, Concepción, Chile; 145International Dx Department, BGI Genomics, Copenhagen, Denmark; 146Breast Surgery Unit, Helsinki University Hospital, Helsinki, Finland; 147University of Helsinki, Helsinki, Finland; 148University Centre Varazdin, University North, Varazdin, Croatia; 149Internal Medicine Program, Kyrgyz State Medical Academy, Bishkek, Kyrgyzstan; 150Department of Atherosclerosis and Coronary Heart Disease, National Center of Cardiology and Internal Disease, Bishkek, Kyrgyzstan; 151National Data Management Center for Health, Ethiopian Public Health Institute, Addis Ababa, Ethiopia; 152Department of Basic Medical Sciences, University of Sharjah, Sharjah, United Arab Emirates; 153Clinical Epidemiology Research Unit, Mexican Institute of Social Security, Villa de Alvarez, Mexico; 154Postgraduate in Medical Sciences, Universidad de Colima, Colima, Mexico; 155Laboratory of Public Health Indicators Analysis and Health Digitalization, Moscow Institute of Physics and Technology, Dolgoprudny, Russia; 156Experimental Surgery and Oncology Laboratory, Kursk State Medical University, Kursk, Russia; 157Mysore Medical College and Research Institute, Government Medical College, Mysore, Karnataka, India; 158Department of Dental Public Health, King Abdulaziz University, Jeddah, Saudi Arabia; 159Department of Health Policy and Oral Epidemiology, Harvard University, Boston, Massachusetts, USA; 160International Islamic University Islamabad, Islamabad, Pakistan; 161Unit of Microbiology and Public Health, Institute of Medical Sciences, Las Tablas, Panama; 162Department of Public Health, Ministry of Health, Herrera, Panama; 163Department of Applied Economics and Quantitative Analysis, University of Bucharest, Bucharest, Romania; 164Department of Preventive Medicine, Kyung Hee University, Dongdaemun- gu, South Korea; 165Department of General Internal Medicine, Baylor College of Medicine, Houston, Florida, USA; 166Department of Medicine, Salvador Zubiran National Institute of Medical Sciences and Nutrition, Tlalpan, Mexico; 167Department of Biostatistics, University of Washington, Seattle, Washington, USA; 168Department of Forensic Medicine and Toxicology, Kasturba Medical College, Mangalore, Karnataka, India; 169Yonsei University College of Medicine, Yonsei University, Seodaemun-gu, South Korea; 170Department of Internal Medicine, Ochsner Medical Center, New Orleans, Los Angeles, Califonia, USA; 171Department of General Surgery, University of Texas, Seattle, Washington, USA; 172Department of Internal Medicine, Advent Health, Palm coast, Florida, USA; 173Department of Hospital Medicine, Sound Physicians, Palm Coast, USA; 174Department of Medicine, State University of New York, Syracuse, New York, USA; 175Department of Biology, University of Bahrain, Sakir, Bahrain; 176Medical College, Tairunnessa Memorial Medical College and Hospital, Gazipur, Bangladesh; 177School of Public Health, University of Adelaide, Adelaide, South Australia, Australia; 178Department of Biochemistry, Jagadguru Sri Shivarathreeswara University, Mysuru, Karnataka, India; 179Department of Cardiology, Emory University, Atlanta, Georgia, USA; 180Department of Nephrology, Manipal Academy of Higher Education, Manipal, Karnataka, India; 181Department of Cardiology, Tehran University of Medical Sciences, Tehran, Iran; 182Department of Epidemiology, Non-Communicable Diseases Research Center (NCDRC), Tehran, Iran; 183Deparment of Pharmacology and Toxicology, University of Antioquia, Medellin, Colombia; 184Department of Clinical Research, Federal University of Uberlândia, Uberlândia, Brazil; 185Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran; 186Department of Gastroenterology, Tehran University of Medical Sciences, Terhan, Iran; 187School of Health Sciences, Foundation University, Islamabad, Pakistan; 188International Center of Medical Sciences Research (ICMSR), Islamabad, Pakistan; 189Bioscience and Nursing, MAHSA University, Selangor, Malaysia; 190Interdisciplinary Research Centre in Biomedical Materials (IRCBM), COMSATS Institute of Information Technology, Lahore, Pakistan; 191Applied Biomedical Research Center, Mashhad University of Medical Sciences, Mashhad, Iran; 192Biotechnology Research Center, Mashhad University of Medical Sciences, Mashhad, Iran; 193Department of Community and Family Medicine, All India Institute of Medical Sciences, Bathinda, Punjab, India; 194Department of Medicine, Tehran University of Medical Sciences, Tehran, Iran; 195Department of Entomology, Ain Shams University, Cairo, Egypt; 196Medical Ain Shams Research Institute, Ain Shams University, Cairo, Egypt; 197Department of Pediatrics, University Hospitals Rainbow Babies and Children’s Hospital, Cleveland, Ohio, USA; 198Department of Pediatrics, Case Western Reserve University, Cleveland, Ohio, USA; 199Department of Urban Planning and Design, University of Hong Kong, Hong Kong, China; 200Department of Medicine, Shifa College of Medicine, Shifa Tameer-e-millat University, Islamabad, Pakistan; 201National Heart, Lung, and Blood Institute, National Institute of Health, Rockville, Maryland, USA; 202Department of Infectious Diseases and Microbiology, Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka, India; 203HepatoPancreatoBiliary Surgery and Liver Transplant Unit, HealthCare Global Limited Cancer Care Hospital, Bangalore, Karnataka, India; 204Tehran University of Medical Sciences, Tehran, Iran; 205Department of Basic Sciences, Tabriz University of Medical Sciences, Tabriz, Iran; 206Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran; 207Department of International Studies, Non-Communicable Diseases Research Center (NCDRC), Tehran, Iran; 208Department of Medical-Surgical Nursing, Mazandaran University of Medical Sciences, Sari, Iran; 209Department of Nursing and Health Sciences, Flinders University, Adelaide, SA, Australia; 210School of Medicine, University of Alabama at Birmingham, Birmingham, Alabama, USA; 211Department of Medicine Service, US Department of Veterans Affairs (VA), Birmingham, Alabama, USA; 212Department of Radiodiagnosis, All India Institute of Medical Sciences, Bathinda, Punjab, India; 213Maternal and Child Health Division, International Centre for Diarrheal Disease Research, Dhaka, Bangladesh; 214Department of Infectious Diseases and Epidemiology, Pirogov Russian National Research Medical University, Moscow, Russia; 215Department of Hygiene and Public Health, Kanazawa University, Kanazawa, Japan; 216Trauma and Injury Research Center, Iran University of Medical Sciences, Tehran, Iran; 217Medical Ethics and Law Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 218Department of Surgery, National University of Singapore, Singapore, Singapore; 219Rheumatology and Immunology Unit, Mansoura University, Mansoura, Egypt; 220Department of Gastroenterology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India; 221Department of Pharmacy, Komar University of Science and Technology, Sulaymaniyah, Iraq; 222Urmia University of Medical Sciences, Urmia, Iran; 223UKK Institute, Tampere, Finland; 224Tampere University, Tampere, Finland; 2265Department of Medicine, Vanderbilt University, Nashville, Tennessee, USA; 226Department of Gastroenterology, The First Affiliated Hospital of USTC, University of Science and Technology of China, Hefei, China; 227Department of community Medicine, Rajarata University of Sri Lanka, Anuradhapura, Sri Lanka; 228Department of Endocrinology, University of Science and Technology of China, Hefei, China; 229Department of Medicine, University of Rochester, Rochester, New York, USA; 230Department of Epidemiology and Biostatistics, Wuhan University, Wuhan, China; 231Department of Clinical Pharmacy and Outcomes Sciences, University of South Carolina, Columbia, South Carolina, USA; 232Urology and Nephrology Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 233School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 234School of Medicine, Wuhan University, Wuhan, China
FUNDING INFORMATION
This work was supported by the EASL International Liver Foundation, which acknowledges funding from Intercept Pharmaceutics, as well as Bristol Myers Squibb and Merck Sharp and Dohme. The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to the data in the study and had final responsibility for the decision to submit to publication.
CONFLICTS OF INTEREST
Jeffrey V. Lazarus reports grants from Gilead Sciences and Roche and consulting fees and advisory arrangements from AbbVie, Gilead Sciences, and Roche, outside the submitted work. Jörn M. Schattenberg reports consulting fees from Apollo Endosurgery, AGED diagnostics, Bayer, Boehringer Ingelheim, Gilead Sciences, GSK, Intercept Pharmaceuticals, Ipsen, Inventiva Pharma, Madrigal, MSD, Northsea Therapeutics, Novartis, Novo Nordisk, Pfizer, Roche, Sanofi, and Siemens Healthineers, speaker fees from Boehringer Ingelheim, Echosens, MedPublico GmbH, Novo Nordisk, Madrigal Pharmaceuticals, and Histoindex, and grants from Gilead Sciences, Boehringer Ingelheim, and Siemens Healthcare GmbH, outside the submitted work. Hannah Han and M. Ashworth Dirac report support for the present manuscript from the EASL International Liver Foundation. Sandra Cortés reports support from the Fondo de Financiamiento de Centros de Investigacion en Areas Prioritarias (FONDAP) (grant number 15130011), outside the submitted work. Xiaochen Dai reports support for the present manuscript from IHME/UW as a salaried employee. Temitope Cyrus Ekundayo reports grants or contracts from The African-German Network of Excellence in Science (AGNES), the Federal Ministry of Education and Research (BMBF), and the Alexander von Humboldt Foundation (AvH) for financial support, outside the submitted work. Vivek Kumar Gupta reports grants or contracts from the National Health and Medical Research Council (NHMRC), Australia, outside the submitted work. Vivian Chia-rong Hsieh reports support from the National Science and Technology Council, Taiwan for Grant # MOST 107-2314-B-039-065-MY3 and grants or contracts from the National Science and Technology Council, Taiwan for Grant # MOST 107-2314-B-039-065-MY3, outside the submitted work. Nahlah Elkudssiah Ismail reports leadership or fiduciary roles in board, society, committee, or advocacy groups, paid or unpaid, with the Malaysian Academy of Pharmacy as council member, outside the submitted work. Abel Joseph reports support from the Bill and Melinda Gates Foundation, grants or contracts from the American College of Gastroenterology for a Clinical Research Award, and support for attending meetings and/or travel from American College of Gastroenterology Annual Meeting 2022, outside the submitted work. Jacek Jerzy Jozwiak reports payment or honoraria for lectures, presentations, speakers' bureaus, manuscript writing, or educational events from NOVART and ADAMED, outside the submitted work. Ibraheem M. Karaye reports support for attending meetings and/or travel from Hofstra University, outside the submitted work. Yeong Yeh Lee reports grants or contracts from NAFLD-related Clinical Trial Investigator for Novo Nordisk and Boehringer Ingelheim and leadership or fiduciary roles in board, society, committee, or advocacy groups, paid or unpaid, with the Malaysian Society of Gastroenterology and Hepatology as President, outside the submitted work. Lee-Ling Lim reports grants or contracts from Boehringer Ingelheim, AstraZeneca, and Abbott Nutrition, outside the submitted work. Stefan Lorkowski acknowledges funding by the German Federal Ministry of Education and Research (nutriCARD, grant agreement number 01EA1808A), grants or contracts from Akcea Therapeutics Germany, consulting fees from Danone, Novartis Pharma, and Swedish Orphan Biovitrum (SOBI), payment or honoraria for lectures, presentations, speakers' bureaus, manuscript writing, or educational events from Akcea Therapeutics Germany, AMARIN Germany, AMARIN Germany, AMGEN, Berlin-Chemie, Boehringer Ingelheim Pharma, Daiichi Sankyo Deutschland, Danone, Hubert Burda Media Holding, Janssen-Cilag, Lilly Deutschland, Novartis Pharma, Novo Nordisk Pharma, Roche Pharma, Sanofi-Aventis, and SYNLAB Holding Deutschland & SYNLAB Akademie, support for attending meetings and/or travel from AMGEN and Novo Nordisk Pharma., and participation on a Data Safety Monitoring Board or Advisory Board with Akcea Therapeutics Germany, AMGEN, Daiichi Sankyo Deutschland, Novartis Pharma, and Sanofi-Aventis, outside the submitted work. Chinmoy Sarkar reports grants or contracts from the US National Academy of Medicine – Hong Kong University International Fellowship in Global Health Leadership (2019-23), outside the submitted work. Pritik A. Shah reports support for the present manuscript from Bangalore Medical College and Research Institute, part of the Rajiv Gandhi University of Health Sciences, outside the submitted work. Jasvinder A. Singh reports consulting fees from Crealta/Horizon, Medisys, Fidia, PK Med, Two labs Inc., Adept Field Solutions, Clinical Care options, Clearview healthcare partners, Putnam associates, Focus forward, Navigant consulting, Spherix, MedIQ, Jupiter Life Science, UBM LLC, Trio Health, Medscape, WebMD, Practice Point communications, and the National Institutes of Health and the American College of Rheumatology, payment or honoraria for lectures, presentations, speakers' bureaus, manuscript writing, or educational events from Simply Speaking as a member of the speakers' bureau, support for attending meetings and/or travel from the steering committee of OMERACT, participation on a Data Safety Monitoring Board or Advisory Board with FDA Arthritis Advisory Committee, leadership or fiduciary roles in board, society, committee, or advocacy groups, paid or unpaid, with OMERACT as a steering committee member, the Veterans Affairs Rheumatology Field Advisory Committee as Chair, and UAB Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis as editor and Director, stock or stock options in TPT Global Tech, Vaxart pharmaceuticals, Atyu biopharma, Adaptimmune Therapeutics, GeoVax Labs, Pieris Pharmaceuticals, Enzolytics Inc., Seres Therapeutics, Tonix Pharmaceuticals, and Charlotte’s Web Holdings, Inc, and previously held stock options in Amarin, Viking, and Moderna pharmaceuticals, outside the submitted work. The remaining authors have no conflicts to report.
Supplementary Material
Footnotes
Abbreviations: GBD, Global Burden of Disease; HDI, Human Development Index; NCD, noncommunicable disease; SDG, Sustainable Development Goal; UGS, urban green space; UHC, universal health coverage; UI, uncertainty interval.
Jeffrey V. Lazarus is lead author; M. Ashworth Dirac is senior author.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.hepjournal.com.
Contributor Information
Jeffrey V. Lazarus, Email: jeffrey.lazarus@isglobal.org.
Hannah Han, Email: hhan5@uw.edu.
Henry E. Mark, Email: henryemark@gmail.com.
Saleh A. Alqahtani, Email: salqaht1@jhmi.edu.
Jörn M. Schattenberg, Email: schatten@uni-mainz.de.
Joan B. Soriano, Email: jbsoriano2@gmail.com.
Trenton M. White, Email: trenton.white@isglobal.org.
Shira Zelber-Sagi, Email: shira.zelber@gmail.com.
Collaborators: Amirali Aali, Mohsen Abbasi-Kangevari, Eman Abu- Gharbieh, Osama Abu-Shawer, Manik Aggarwal, Bright Opoku Ahinkorah, Aqeel Ahmad, Ali Ahmadi, Fares Alahdab, Motasem Alkhayyat, Sami Almustanyir, Hubert Amu, Amir Anoushiravani, Tahira Ashraf, Bantalem Tilaye Tilaye Atinafu, Sina Azadnajafabad, Nayereh Baghcheghi, Sara Bagherieh, Mainak Bardhan, Diana Fernanda Bejarano Ramirez, Akshaya Srikanth Bhagavathula, Neeraj Bhala, Ajay Nagesh Bhat, Mariah Malak Bilalaga, Antonio Biondi, Saeid Bitaraf, Srinivasa Rao Bolla, Antoine Boustany, Daniela Calina, Ismael R. Campos-Nonato, Kumar Chattu Vijay, Sheng-Chia Chung, Daniela Contreras, Sandra Cortés, Omar B. Da’ar, Omid Dadras, Xiaochen Dai, Bardia Danaei, Rupak Desai, Shirin Djalalinia, Deepa Dongarwar, Haneil Larson Dsouza, Temitope Cyrus Ekundayo, Iman El Sayed, Noha Mousaad Elemam, Mohamed A. Elmonem, Aisha Elsharkawy, Sayeh Ezzikouri, Amr Farwati, Farshad Farzadfar, Ginenus Fekadu, Florian Fischer, Tushar Garg, Elena S. George, Seyyed-Hadi Ghamari, Mohammad Ghasemi Nour, Amit Goel, Mahaveer Golechha, Pouya Goleij, Vivek Kumar Gupta, Parham Habibzadeh, Adel Hajj Ali, Saeed S. Hamid, Harapan Harapan, Sanam Hariri, Maryam Hashemian, Abbas M. Hassan, Mohammed Bheser Hassen, Simon I. Hay, Yuta Hiraike, Reza Homayounfar, Mohammad-Salar Hosseini, Sedighe Hosseini Shabanan, Soodabeh Hoveidamanesh, Vivian Chia-rong Hsieh, Junjie Huang, Salman Hussain, Segun Emmanuel Ibitoye, Olayinka Stephen Ilesanmi, Nahlah Elkudssiah Ismail, Chidozie CD Iwu, J Linda Merin, Elham Jamshidi, Umesh Jayarajah, Shubha Jayaram, Bijay ghMukesh Jeswani, Jost B. Jonas, Abel Joseph, Charity Ehimwenma Joshua, Jacek Jerzy Jozwiak, Ali Kabir, Vidya Kadashetti, Tesfaye K. Kanko, Rami S Kantar, Nitin Kapoor, Ibraheem M. Karaye, Joonas H. Kauppila, Mohammad Keykhaei, Moien A.B. Khan, Min Seo Kim, Hamid Reza Koohestani, Ambily Kuttikkattu, Carlo La Vecchia, Bagher Larijani, Sang-woong Lee, Yeong Yeh Lee, Lee-Ling Lim, Stephen S. Lim, Chun-Han Lo, Stefan Lorkowski, Jamal Majidpoor, Mohammad- Reza Malekpour, Yasaman Mansoori, Miquel Martorell, Sahar Masoudi, Alexios-Fotios A. Mentis, Tuomo J. Meretoja, Tomislav Mestrovic, Erkin M. Mirrakhimov, Awoke Misganaw, Abdollah Mohammadian-Hafshejani, Ali H. Mokdad, Jibran Sualeh Muhammad, Efrén Murillo-Zamora, Christopher J. L. Murray, Mukhammad David Naimzada, Sreenivas Narasimha Swamy, Hasan Nassereldine, Zuhair S. Natto, Robina Khan Niazi, Virginia Nuñez- Samudio, Bogdan Oancea, In-Hwan Oh, Olubunmi Omotola Oladunjoye, Antonio Olivas-Martinez, Jagadish Rao Padubidri, Beng Seoyeon Park, Harsh K. Patel, Ronit Patnaik Patnaik, Venkata Suresh Patthipati, Gayatri Pemmasani, Simone Perna, Vivek Podder, Akram Pourshams, Akila Prashant, Pradhum Ram, Indu Ramachandra Rao, Sina Rashedi, Mohammad-Mahdi Rashidi, Negar Rezaei, Jefferson Antonio Buendia Rodriguez, Leonardo Roever, Gholamreza Roshandel, Bahar Saberzadeh- Ardestani, Umar Saeed, Sher Zaman Safi, Amirhossein Sahebkar, Soumya Swaroop Sahoo, Mohammad Amin Salehi, Abdallah M. Samy, Senthilkumar Sankararaman, Chinmoy Sarkar, Danish Iltaf Satti, Allen Seylani, Pritik A. Shah, Elaheh Shaker, Ali Shamekh, Parnian Shobeiri, Seyed Afshin Shorofi, Jasvinder A. Singh, Paramdeep Singh, Md Shahjahan Siraj, Anna Aleksandrovna Skryabina, Amir Ali Sohrabpour, Keita Suzuki, Majid Taheri, Ker-Kan Tan, Samar Tharwat, Nikhil Kenny Thomas, Bereket M. Tigabu, Marco Vacante, Seyed Mohammad Vahabi, Rohollah Valizadeh, Tommi Juhani Vasankari, Theo Vos, Cong Wang, Song Wang, Nuwan Darshana Wickramasinghe, Suowen Xu, Chuanhua Yu, Ismaeel Yunusa, Mazyar Zahir, Moein Zangiabadian, and Zhi-Jiang Zhang
REFERENCES
- 1.Ghevariya V, Sandar N, Patel K, Ghevariya N, Shah R, Aron J, et al. Knowing what’s out there: awareness of non-alcoholic fatty liver disease. Front Med (Lausanne). 2014;1:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lazarus JV, Mark HE, Villota-Rivas M, Palayew A, Carrieri P, Colombo M, et al. The global NAFLD policy review and preparedness index: Are countries ready to address this silent public health challenge? J Hepatol. 2022;76:771–80. [DOI] [PubMed] [Google Scholar]
- 3.Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2022;7:851–61. [DOI] [PubMed] [Google Scholar]
- 4.Yüksel F, Türkkan D, Yüksel I, Kara S, Celik N, Samdanci E. Fatty liver disease in an autopsy series of children and adolescents. Hippokratia. 2012;16:61–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118:1388–93. [DOI] [PubMed] [Google Scholar]
- 6.Anderson EL, Howe LD, Jones HE, Higgins JPT, Lawlor DA, Fraser A. The prevalence of non-alcoholic fatty liver disease in children and adolescents: a systematic review and meta-analysis. PLoS One. 2015;10:e0140908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huber Y, Schulz A, Schmidtmann I, Beutel M, Pfeiffer N, Münzel T, et al. Prevalence and risk factors of advanced liver fibrosis in a population-based study in Germany. Hepatol Commun. 2022;6:1457–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nah EH, Cho S, Kim S, Chu J, Kwon E, Cho HI. Prevalence of liver fibrosis and associated risk factors in the Korean general population: a retrospective cross-sectional study. BMJ Open. 2021;11:e046529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris R, Harman DJ, Card TR, Aithal GP, Guha IN. Prevalence of clinically significant liver disease within the general population, as defined by non-invasive markers of liver fibrosis: a systematic review. Lancet Gastroenterol Hepatol. 2017;2:288–97. [DOI] [PubMed] [Google Scholar]
- 10.Huber Y, Boyle M, Hallsworth K, Tiniakos D, Straub BK, Labenz C, et al. Health-related quality of life in nonalcoholic fatty liver disease associates with hepatic inflammation. Clin Gastroenterol Hepatol. 2019;17:2085–92. [DOI] [PubMed] [Google Scholar]
- 11.Schattenberg JM, Lazarus JV, Newsome PN, Serfaty L, Aghemo A, Augustin S, et al. Disease burden and economic impact of diagnosed non-alcoholic steatohepatitis in five European countries in 2018: A cost-of-illness analysis. Liver Int. 2021;41:1227–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sepanlou SG, Safiri S, Bisignano C, Ikuta KS, Merat S, Saberifiroozi M, et al. GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories,1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:245–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Younossi Z, Stepanova M, Ong JP, Jacobson IM, Bugianesi E, Duseja A, et al. Nonalcoholic Steatohepatitis is the fastest growing cause of hepatocellular carcinoma in liver transplant candidates. Clin Gastroenterol Hepatol. 2019;17:748–55. [DOI] [PubMed] [Google Scholar]
- 14.Kanwal F, Kramer JR, Mapakshi S, Natarajan Y, Chayanupatkul M, Richardson PA, et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology. 2018;155:1828–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanna C, Rosso C, Marietti M, Bugianesi E. Non-alcoholic fatty liver disease and extra-hepatic cancers. Int J Mol Sci. 2016;17:717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li L, Liu DW, Yan HY, Wang ZY, Zhao SH, Wang B. Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes Rev. 2016;17:510–9. [DOI] [PubMed] [Google Scholar]
- 17.Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10:330–44. [DOI] [PubMed] [Google Scholar]
- 18.Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2019;69:2672–82. [DOI] [PubMed] [Google Scholar]
- 19.Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:739–52. [DOI] [PubMed] [Google Scholar]
- 20.Alexander M, Loomis AK, Fairburn-Beech J, van der Lei J, Duarte-Salles T, Prieto-Alhambra D, et al. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. 2018;16:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tomah S, Alkhouri N, Hamdy O. Nonalcoholic fatty liver disease and type 2 diabetes: where do Diabetologists stand? Clin Diabetes Endocrinol. 2020;6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood DT, et al. The need for a complex systems model of evidence for public health. Lancet. 2017;390:2602–4. [DOI] [PubMed] [Google Scholar]
- 23.Lazarus JV, Anstee QM, Hagström H, Cusi K, Cortez-Pinto H, Mark HE, et al. Defining comprehensive models of care for NAFLD. Nat Rev Gastroenterol Hepatol. 2021;18:717–29. [DOI] [PubMed] [Google Scholar]
- 24.Díaz LA, Fuentes-López E, Ayares G, Idalsoaga F, Arnold J, Márquez-Lomas A, et al. The establishment of public health policies and the burden of non-alcoholic fatty liver disease in the Americas. Lancet Gastroenterol Hepatol. 2022;7:552–9. [DOI] [PubMed] [Google Scholar]
- 25.Lazarus JV, Mark HE, Anstee QM, Arab JP, Batterham RL, Castera L, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol. 2022;19:60–78. [DOI] [PubMed] [Google Scholar]
- 26.Lazarus JV, Mark HE, Colombo M, Demaio S, Dillon JF, George J, et al. A sustainable development goal framework to guide multisectoral action on NAFLD through a societal approach. Aliment Pharmacol Ther. 2022;55:234–43. [DOI] [PubMed] [Google Scholar]
- 27.United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. 2015. Accessed August 15, 2022. https://sdgs.un.org/2030agenda
- 28.Ramirez-Rubio O, Daher C, Fanjul G, Gascon M, Mueller N, Pajín L, et al. Urban health: an example of a “health in all policies” approach in the context of SDGs implementation. Global Health. 2019;15:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ralston J, Cooper K, Powis J. Obesity, SDGs and ROOTS: a Framework for Impact. Curr Obes Rep. 2021;10:54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.United Nations Statistics Division. SDG Indicators. UNSD.2020. Accessed August 15, 2022. https://unstats.un.org/sdgs/indicators/indicators-list
- 31.Lozano R, Fullman N, Mumford JE, Knight M, Barthelemy CM, Abbafati C, et al. GBD 2019 Universal Health Coverage Collaborators. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1250–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murray C, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang H, Abbas KM, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F, et al. GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lozano R, Fullman N, Abate D, Abay SM, Abbafati C, Abbasi N, et al. GBD 2017 SDG Collaborators. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:2091–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kwon O-H, Hong I, Yang J, Wohn DY, Jung W-S, Cha M. Urban green space and happiness in developed countries. EPJ Data Sci. 2021;10:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miura T, Nagai S, Takeuchi M, Ichii K, Yoshioka H. Improved characterisation of vegetation and land surface seasonal dynamics in central Japan with Himawari-8 Hypertemporal data. Sci Rep. 2019;9:15692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Cause, REI, and Location Hierarchies.2018. Accessed August 15, 2022. https://ghdx.healthdata.org/record/ihme-data/gbd-2017-cause-rei-and-location-hierarchies
- 38.UNDP. Technical notes: calculating the human development indices. (2020). Accessed February 15, 2023. https://hdr.undp.org/sites/default/files/2021-22_HDR/hdr2021-22_technical_notes.pdf.
- 39.Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67:123–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021;18:223–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67:829–46. [DOI] [PubMed] [Google Scholar]
- 42.Kabisch N.Marselle M, Stadler J, Korn H, Irvine K, Bonn A. The Influence of Socio-economic and Socio-demographic Factors in the Association Between Urban Green Space and Health. Biodiversity and Health in the Face of Climate Change, 1st edn. Springer; 2019;5:91–119. [Google Scholar]
- 43.Jennings V, Bamkole O. The relationship between social cohesion and urban green space: an avenue for health promotion. Int J Environ Res Public Health. 2019;16:452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. GBD 2019 Diseases Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bigna JJ, Noubiap JJ. The rising burden of non-communicable diseases in sub-Saharan Africa. Lancet Glob Health. 2019;7:e1295–6. [DOI] [PubMed] [Google Scholar]
- 46.Kankeu HT, Saksena P, Xu K, Evans DB. The financial burden from non-communicable diseases in low- and middle-income countries: a literature review. Health Res Policy Syst. 2013;11:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chaker L, Falla A, van der Lee SJ, Muka T, Imo D, Jaspers L, et al. The global impact of non-communicable diseases on macro-economic productivity: a systematic review. Eur J Epidemiol. 2015;30:357–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hill PS, Buse K, Brolan CE, Ooms G. How can health remain central post-2015 in a sustainable development paradigm? Global Health. 2014;10:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bennett S, Glandon D, Rasanathan K. Governing multisectoral action for health in low-income and middle-income countries: unpacking the problem and rising to the challenge. BMJ Glob Health. 2018;3(suppl 4):e000880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shepley M, Sachs N, Sadatsafavi H, Fournier C, Peditto K. The impact of green space on violent crime in urban environments: an evidence synthesis. Int J Environ Res Public Health. 2019;16:5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ju Y, Moran M, Wang X, Avila-Palencia I, Cortinez-O’Ryan A, Moore K, et al. Latin American cities with higher socioeconomic status are greening from a lower baseline: evidence from the SALURBAL project. Environ Res Lett. 2021;16:104052. [DOI] [PMC free article] [PubMed] [Google Scholar]


