Abstract
Latino sexual minority men (LSMM) are affected by HIV and behavioral health disparities. Evidence-based HIV-prevention and behavioral health (BH) services are not sufficiently scaled up to LSMM. The current study identified multilevel barriers and facilitators to LSMM’s use of HIV-prevention and BH services. LSMM (N=290) in South Florida, a US HIV epicenter, completed a battery of measures potentially associated with pre-exposure prophylaxis (PrEP) and BH treatment use. Stochastic search variable selection (SSVS) followed by multiple linear regression analyses identified variables associated with engagement in PrEP and BH treatment. Multilevel determinants of PrEP and BH treatment engagement were identified, with most identified determinants being at the relational level (e.g., stigma, discrimination based on income and immigration status, personal recommendation for treatment). Individual (e.g., knowledge, self-efficacy) and structural (e.g., financial stress) determinants were also identified. Accordingly, modifiable leverage points to enhance the reach of PrEP and BH treatment to LSMM include educating and enhancing the perceived relevance of services, de-stigmatizing and normalizing via peer examples, bolstering self-efficacy, and building trust.
Keywords: Latino, sexual minority men, PrEP, behavioral health, health disparities, implementation
Introduction
Latina/o/xa individuals represent 18% of the population (Pew Research Center, 2020) and 23% of individuals living with HIV in the United States (Centers for Disease Control and Prevention, 2020b). Among Latina/o/x individuals, Latino sexual minority men (LSMM) account for 85% of new HIV diagnoses in the U.S. (Centers for Disease Control and Prevention, 2020a), making this population a priority for the U.S. Ending the HIV Epidemic (EHE) plan (Fauci, Redfield, Sigounas, Weahkee, & Giroir, 2019). The EHE plan is focused on regions where HIV incidence is highest, one of which is Miami-Dade County (MDC) (Office of Infectious Disease, 2020). In MDC, most new HIV cases occur among LSMM (Centers for Disease Control and Prevention, 2020a), making this area a domestic focal point for addressing LSMM HIV disparities.
In addition to HIV disparities, LSMM face mental health and substance use disparities (Rodriguez-Seijas, Eaton, & Pachankis, 2019). In a nationally representative sample of U.S. adults, Latina/o/x sexual minority individuals reported greater odds of psychiatric (e.g., depression, anxiety, trauma) and substance use disorders compared to Latina/o/x heterosexual individuals (Rodriguez-Seijas et al., 2019). Another study estimated the prevalence of clinically significant depressive symptoms at 69.2% among LSMM in the Southeast U.S. (Rhodes et al., 2013). Similar patterns are noted with LSMM’s substance use, with past six month substance use ranging from 16% to 40% depending on the geographic area (Díaz, Morales, Bein, DiláN, & RodríGuez, 1999; Ramirez-Valles, Garcia, Campbell, Diaz, & Heckathorn, 2008).
Syndemic theory articulates that co-occurring epidemics rooted in inequities worsen disease outcomes in minoritized populations (Singer & Clair, 2003). The theory posits that health outcomes (e.g., HIV, mental health, substance use) are not independent; rather, they interact synergistically to impact health (Singer & Clair, 2003). Martinez and colleagues (2016) found that among LSMM, syndemic indicators (e.g., depression, discrimination, alcohol) were associated with increased likelihood of sexual behavior that could lead to HIV acquisition or transmission. Another study examined syndemic indicators associated with Latino men who have sex with men’s (LMSM) experiences of homophobia and racism, finding that experiencing both was linked to sexual behavior that could result in HIV acquisition (Mizuno et al., 2012). As such, syndemics present unique challenges for LSMM and underscore the need to address both HIV and behavioral health (BH) disparities to optimize LSMM’s health.
Evidence-based interventions that prevent HIV acquisition (e.g., pre-exposure prophylaxis/PrEP) and treat BH concerns (i.e., mental health and substance use treatment) have been developed and implemented, to some extent, in community settings (Anderson et al., 2012; Centers for Disease Control and Prevention, 2018; Escobar & Gorey, 2018; Grant et al., 2010; Pineros-Leano, Liechty, & Piedra, 2017; Valdez et al., 2018). Despite PrEP being an evidence-based intervention for preventing acquisition of HIV and a variety of evidence-based BH treatments existing to treat BH concerns, both are insufficiently scaled up and out to LSMM (Blashill et al., 2020; Harkness et al., 2021; Parsons et al., 2017; Rhodes et al., 2013). Given the synergistic nature of HIV and BH disparities among LSMM, achieving health equity requires increasing the reach of PrEP and evidence-based BH treatments to LSMM.
Reasons for low reach and uptake of PrEP and BH treatment among LSMM have begun to be explored. LSMM report stigma-related barriers to PrEP (Lelutiu-Weinberger & Golub, 2016), psychosocial barriers (e.g., depression, substance use), and structural barriers (e.g., unstable housing, poverty) (Blashill et al., 2020). Although fewer studies have examined factors associated with LSMM’s use of BH treatments, low perceived need has been identified as a barrier among Latina/o/x individuals (Breslau et al., 2017; Cook et al., 2014; Tanner et al., 2014). Our qualitative research with LSMM, as well as individuals who deliver HIV and BH services to LSMM, in the greater Miami area identified barriers and facilitators to LSMM’s engagement in HIV-prevention and BH treatment (Harkness et al., 2021). Findings suggested a need for multilevel, culturally relevant implementation strategies to improve the reach of HIV-prevention and BH services to LSMM. Our findings suggested the need for implementation strategies that reduce complexity and cost, address LSMM’s syndemic problems and structural barriers, leverage peer networks, link LSMM to providers who fit with LSMM’s preferences, and build LSMM’s readiness for change.
Based on our qualitative findings (Harkness et al., 2021) we selected and developed a battery of quantitative measures of potential determinants of South Florida-based LSMM’s PrEP and BH treatment engagement. The current study modeled the relative importance of each factor as a predictor for two outcomes: (1) PrEP engagement and (2) BH treatment engagement. The current study builds on our prior qualitative work by quantitatively identifying multilevel leverage points to scale up PrEP and BH treatment to LSMM in the greater Miami area.
Methods
Participants and Procedures
Between February and September 2020, LSMM were recruited to participate in the current study (called DÍMELO). Inclusion criteria required that participants: (1) identified as a gay, bisexual, or man who has sex with men (i.e., transwomen were not included in the current study), (2) identified as Latino/Hispanic, (3) self-reported negative or unknown HIV status, (4) lived in the Miami area, and (5) were 18 to 60 years old. The study was available in English and Spanish. The University of Miami Institutional Review Board approved this study with a waiver of signed consent. Participants reviewed consent information within REDCap, where the study was administered, and clicked a box indicating consent to participate.
Participants were recruited through social media, listservs, community venues and events, snowball recruitment, and a “consent-to-contact” database. Study staff contacted interested individuals who completed a study screener to confirm their eligibility and enroll them via REDCap. Surveys took approximately 75 minutes and participants were compensated $40.
Measures
A prior qualitative study (Harkness et al., 2021) in conjunction with an overarching focus on syndemic (Singer & Clair, 2003), minority stress (Meyer, 2003) and intersectionality theories (Crenshaw, 1991) informed the measures, yielding a culturally tailored assessment of potential determinants of LSMM’s engagement in HIV-prevention and BH services. Measures not available in Spanish were translated via forward translation (English to Spanish), back translation (Spanish to English), and an evaluation of the original and back-translated versions to ensure meaning was retained (Kurtines & Szapocznik, 1995). Additional translated measures were available through source articles and the Center for Latino Health Research Opportunities’ Measures Library (Mitrani, O’Day, Norris, & Adebayo, 2017). Of note, this exploratory study considered 70+ variables prior for our final models; as such, Electronic Supplementary Table 1 summarizes variable names, operationalizations/definitions, rating/scoring and interpretation, and citations for each measure that was considered for our final models. In the body of the manuscript, we provide a brief overview of all measures that were considered and provide greater detail on measures selected in our final models.
Demographics
Participants completed a demographic questionnaire based on the CLaRO Measures Library and the Center for HIV and Research in Mental Health’s community survey.
Stigma, Discrimination, and Affirmation
The 5-item Everyday Discrimination Scale assessed experiences of discrimination related to various aspects of identity, including income and immigration status (Sternthal, Slopen, & Williams, 2011; Williams, Yan Yu, Jackson, & Anderson, 1997). Three subscales of the LGB Identity Scale, including concealment motivation, internalized homonegativity, and identity affirmation, each of which were 3 items (Mohr & Kendra, 2011) were included in the assessment battery. The 5-item PrEP Stigma Scale (Walsh, 2019) assessed the degree to which participants thought that taking PrEP is stigmatized. Additional measures not selected for the final models included the Climate Scale (Pachankis, Eldahan, & Golub, 2016), Anticipated HIV Stigma Scale (Golub & Gamarel, 2013), and Perceptions of Stigmatization by Others for Seeking Psychological Help Scale (Vogel, Wade, & Ascheman, 2009).
Perceived Norms and Support
The Perceived Community Norms for PrEP and Perceived Community Norms for Behavioral Health Treatment single-item measures (Andrinopoulos & Hembling, 2013) were adapted from Andrinopoulos and Hembling’s Perceived Community Norms for HIV Testing measure. Participants indicated how many people they knew who used each type of service; those reporting “all or almost all” or “half” were coded as having high perceived norms and those who did not endorse these were coded as having low perceived norms. The Psychosocial Treatment Inventory (Steketee et al., 1997) (described further below) assessed whether a doctor or personal contact (i.e., friend, family, partner) recommended they receive BH treatment. Although not in the final models, participants completed the Lubben Social Network Scale-6 (Lubben et al., 2006)
Knowledge
The PrEP Knowledge Scale, which included 13 true/false questions about PrEP (Walsh, 2019) awarded participants one point for each correct answer, resulting in sum scores from 0 (all incorrect) to 13 (all correct). Additional measures not in the final models were the HIV Knowledge Scale (Feinstein, Johnson, Parsons, & Mustanski, 2017) and Mental Health Knowledge Schedule (Evans-Lacko et al., 2010).
Self-Efficacy
The 8-item PrEP Self-Efficacy Scale (Walsh, 2019) evaluated participants’ capacity to engage in behaviors to obtain PrEP. Mean scores were computed, such that scores could range from 1 (lowest self-efficacy) to 4 (highest self-efficacy). Additional measures not included in the final models were the Attitudes Toward Seeking Professional Help Scale (Elhai, Schweinle, & Anderson, 2008) and Problem Solving Confidence Scale (Heppner, Witty, & Dixon, 2004).
Cultural Factors
The Cultural Attitudes Toward Healthcare and Mental Illness Questionnaire evaluated cultural beliefs about mental health (Jimenez, Bartels, Cardenas, Dhaliwal, & Alegría, 2012). The questionnaire asked participants to indicate what they perceived to cause mental health concerns and what they believed could help address mental health concerns. Following guidelines from Lozano and colleagues (Under Review), we computed binary composite scores (ref=no) for each of the following mental health attributions: stress/loss, problems with spirit/psyche, environment/culture, and medical causes. The scoring guidelines also yield binary scores (ref=no) for each of the following mental health supports: therapy, medical intervention, family/friend support, and alternative medicine. Additional measures not in the final models were the Health Stress subscale of the Hispanic Stress Inventory-2 (Cervantes, Fisher, Padilla, & Napper, 2015) and Vancouver Index of Acculturation (Testa et al., 2019).
Sexual Behavior, Mental Health, and Substance Use
The current study did not recruit a clinic-based sample. Therefore, we assessed sexual behavior, mental health, and substance use as clinical indicators of PrEP and BH treatment need, respectively. As an indicator of PrEP need, participants’ sexual activity level in the past six months was coded as: (1) not sexually active, (2) sexually active but not meeting CDC HIV PrEP guidelines or (3) sexually active and meeting CDC HIV PrEP guidelines (Centers for Disease Control and Prevention, 2018). Participants also reported their likelihood of acquiring HIV in the next year (Golub & Gamarel, 2013) as an indicator of perceived need for PrEP, although this was not included in the final model.
Although participants completed measures related to BH treatment need, none were selected for the final models. Measures included the Center for Epidemiological Studies Depression Scale (Andresen, Malmgren, Carter, & Patrick, 1994), Generalized Anxiety Disorder Scale (Spitzer, Kroenke, Williams, & Löwe, 2006). Primary Care PTSD Screen (Prins et al., 2016), Somatic Symptom Scale-8 (Gierk et al., 2014), Perceived Stress Scale-4 (Warttig, Forshaw, South, & White, 2013), Adverse Childhood Experiences Scale (Felitti et al., 1998), Alcohol Use Disorders Identification Test-C (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998), and the substance use questionnaire from HPTN083 (HPTN 083 study team, 2017). In the Psychosocial Treatment Inventory, participants indicated if they perceived themselves to need BH treatment, which was selected for inclusion in the final BH model (Steketee et al., 1997).
Barriers and Facilitators to Using Services
From our qualitative findings (Harkness et al., 2021), we developed two new measures: (1) the PrEP Barriers and Facilitators Measure and (2) the Behavioral Health Treatment Barriers and Facilitators Measure. The Barriers to Treatment Participation Scale (Kazdin, Holland, Crowley, & Breton, 1997) was used as a point of departure to develop these new measures. To score these, we conducted a theoretically derived series of exploratory factor analyses (EFA). Items within each scale were theoretically grouped. We ran an EFA for all items in the theoretical groups to determine the number of subscales within each theoretical grouping. Unidimensional groups became one subscale and multidimensional groups (i.e., eigenvalues >1) became multiple subscales. Additionally, our team is in the process of conducting a validation study of this measure to guide scoring further. Subscales selected for the final PrEP model were: negative past experience with PrEP (barrier), PrEP mistrust (barrier), PrEP navigation support (facilitator), and PrEP as altruism (facilitator). Subscales selected for the final BH model were: BH knowledge (facilitator) and BH being normalized (facilitator).
PrEP and Behavioral Health Treatment Cascades
The outcome variables were PrEP and BH treatment engagement, measured by stages of change cascades (Prochaska & Velicer, 1997). The PrEP cascade was based on Parsons and colleagues (2017) with survey questions from prior studies informing participants’ position on the PrEP cascade (Grov, Rendina, Whitfield, Ventuneac, & Parsons, 2016; Grov, Whitfield, Rendina, Ventuneac, & Parsons, 2015; Parsons et al., 2017; Rendina, Whitfield, Grov, Starks, & Parsons, 2017). A BH treatment cascade was constructed based on participants’ responses to the Psychosocial Treatment Inventory (Steketee et al., 1997). For both cascades, there were five “levels” consistent with stages of change theory (Prochaska & Velicer, 1997): pre-contemplation, contemplation, preparation, initiation, and maintenance.
Data Analyses
The final analytic sample was 290 after surveys that were invalid (i.e., failing the attention check) or duplicates (N=12) were excluded. Descriptive statistics explored demographics and variable distributions. Stochastic search variable selection (SSVS; described below) requires complete data on all variables. Independent variables with sparse missing data and at least 80% completed items were scored (Graham, 2009) such that sum and mean scores were computed based on completed items.
Given the substantial number of theoretically identified predictors, we used SSVS to select the most important predictors for each outcome in our final models while minimizing Type I and Type II errors. SSVS is a Bayesian variable selection method that estimates the probability that each predictor is related to the outcome (i.e., has a non-zero regression coefficient) while accounting for uncertainty in which other predictors are included in the model (Bainter, McCauley, Wager, & Losin, 2020; George & McCulloch, 1993). SSVS samples thousands of predictor combinations to identify the best fitting models. After sampling, the marginal inclusion probability for each predictor (i.e., the proportion of times each predictor was included in the sampled models) identifies which predictors are more stably associated with the outcome.
We performed SSVS using the SSVSforPsych shiny app (Bainter et al., 2020), specifying the following: 0.5 prior inclusion probability, 1000 burn-in iterations, 10000 total iterations. Categorical variables were dummy coded. Independent variables with markedly higher marginal inclusion probabilities were included in final multiple linear regression models.
Results
Demographics and Descriptive
Most participants identified as White Latino (79.3%), gay (83.8%), and US citizens (75.2%). Of those born outside the continental US (51.4%), Cuba, Colombia, and Venezuela were the most common countries of origin. Most participants were sexually active and 53.8% met CDC HIV PrEP guidelines. Participants had high behavioral health burden (e.g., 52.8% clinically significant depressive symptoms). Most participants were in the “pre-contemplation” stage regarding both PrEP and BH treatment. See Table 1 for complete descriptives.
Table 1.
Descriptive Statistics: Demographics and Key Variables
| Variable | Frequency (%) / Mean (SD) |
|---|---|
| Age | 31.9 (8.32) |
| Sexual orientation | |
| Gay | 243 (83.8%) |
| Bisexual | 26 (9.0%) |
| Another sexual minority identity | 21 (7.2%) |
| Nativity | |
| Continental United States | 140 (48.3%) |
| Caribbean (e.g., Cuba, Dominican Republic, Jamaica, Puerto Rico) |
35 (12.1%) |
| Central America (e.g., Guatemala) | 19 (6.6%) |
| North America (Mexico) | 2 (0.7%) |
| South America (e.g., Argentina, Chile, Colombia, Ecuador, Peru, Venezuela) |
92 (31.7%) |
| Other | 1 (0.3%) |
| Decline to answer | 1 (0.3%) |
| Citizenship | |
| United States citizen | 218 (75.2%) |
| Permanent resident | 25 (8.6%) |
| Undocumented | 4 (1.4%) |
| Student Visa | 7 (2.4%) |
| Dependent on someone else’s visa | 1 (0.3%) |
| Asylum | 11 (3.7%) |
| Temporary resident | 6 (2.1%) |
| Temporary work visa | 2 (0.7%) |
| Tourist visa | 4 (1.4%) |
| Expired visa | 2 (0.7%) |
| Temporary protected immigrant | 3 (1.0%) |
| Other | 4 (1.4%) |
| Missing (Decline to answer) | 3 (1.0%) |
| Race & Ethnicity | |
| White Latino | 230 (79.3%) |
| Black Latino | 14 (4.8%) |
| Asian Latino | 2 (0.7%) |
| Indigenous Latino | 11 (3.8%) |
| Other Race and Latino | 4 (1.4%) |
| Multiracial Latino | 26 (9.0%) |
| Missing Race (Decline) & Latino | 3 (1.0%) |
| Street Race* | |
| White | 79 (27.2%) |
| Black | 8 (2.8%) |
| Asian | 2 (0.7%) |
| American Indian/Indigenous | 1 (0.3%) |
| Hispanic/Latino | 166 (57.2%) |
| Middle Eastern/Arab | 22 (7.6%) |
| Another Race | 5 (1.7%) |
| Don’t Know | 6 (2.1%) |
| Missing (Decline to Answer) | 1 (0.3%) |
| Preferred language | |
| English only | 167 (57.6%) |
| Spanish only | 50 (17.2%) |
| Both Spanish and English | 72 (24.8%) |
| Missing | 1 (0.3%) |
| Education level | |
| 9th to 11th grade | 4 (1.4%) |
| GED (High school equivalent) | 3 (1.0%) |
| High School Diploma | 22 (7.6%) |
| Some college/university | 69 (23.8%) |
| College/University degree | 192 (66.2%) |
| Financial stress | |
| Always or Usually | 77 (26.6%) |
| Sometimes | 108 (37.2%) |
| Rarely or Never | 102 (35.2%) |
| Missing (Decline to answer) | 3 (1.0%) |
| Relationship status | |
| Married/Formal Commitment | 33 (11.4%) |
| Partner/Lover | 46 (15.9%) |
| Boyfriend/Girlfriend | 52 (17.9%) |
| Casually dating | 31 (10.7%) |
| Single | 128 (44.1%) |
| Have health insurance | 219 (75.5%) |
| Clinically significant depression | 153 (52.8%) |
| Anxiety (moderate or higher) | 113 (39.0%) |
| PTSD: positive screen | 57 (19.7%) |
| Substance use treatment indication | 74 (25.5%) |
| Behavioral health cascade | |
| Precontemplation | 163 (56.2%) |
| Contemplation | 54 (18.6%) |
| Preparation | 12 (4.1%) |
| Action and Initiation | 19 (6.6%) |
| Maintenance | 40 (13.8%) |
| Missing (Unknown) | 2 (0.7%) |
| PrEP cascade | |
| Precontemplation | 118 (40.7%) |
| Contemplation | 62 (21.4%) |
| Preparation | 34 (11.7%) |
| Action and Initiation | 1 (0.3%) |
| Maintenance | 74 (25.5%) |
| Missing (Unknown) | 3 (1.0%) |
”If you were walking down the street, what race do you think other people who do not know you personally would assume you were based on what you look like?”
PrEP Cascade
SSVS identified 11 variables with higher inclusion probabilities (Supplementary Electronic Materials shows all variables that were considered), which were entered into a multiple linear regression model (see Table 2). Collectively, the variables in the regression model were significantly associated with PrEP engagement, F(12,268) = 19.08, p < 0.001, adj. R2 = 0.437. Participants who were less engaged in PrEP reported greater PrEP stigma (p = 0.03), discrimination based on income (p = 0.015), financial stress (p = 0.026), negative past experiences with PrEP (p = 0.043), and PrEP mistrust (p = 0.037). Those more engaged in PrEP showed greater PrEP knowledge (p < 0.001), self-reported sexual behavior that met CDC HIV PrEP guidelines (p = 0.029; relative to those not sexually active), had higher PrEP self-efficacy (p = 0.031), and viewed PrEP navigation support as a facilitator to PrEP use (p = 0.024). Unexpectedly, greater sexual orientation concealment motivation was associated with greater PrEP engagement (p < 0.001). Although altruism as a PrEP facilitator was selected based on SSVS, it did not reach statistical significance in the regression model (p = 0.082).
Table 2.
Stochastic Search Variable Selection and Multiple Linear Regression Models
| Model 1: PrEP Cascade | ||||
|---|---|---|---|---|
|
| ||||
| Predictors | Descriptive Statistics of Predictor Variable (Mean/SD + Range or Frequency/%) | SSVS Marginal Inclusion Probability (N=252)♦ | Multiple Linear Regression Model (N=281)♦ | |
|
| ||||
| B (SE) | Effect Size (semi-partial correlation, sr) | |||
| PrEP knowledge (objective) | 7.95 (3.43); Range: 0–13 | 1.00 | 0.21 (0.03)** | 0.38 |
|
| ||||
| Discrimination: income | 6.16 (2.09); Range: 5–18 | 0.84 | −0.09 (0.04)* | −0.11 |
|
| ||||
| Sexual behavior (ref: not sexually active): | 31 (10.7%) | |||
| Sexually active meeting CDC PrEP guidelines | 156 (53.8%) | 0.82 | 0.58 (0.26)* | 0.10 |
| Sexually active | 100 (34.5%) | 0.20 | −0.09 (0.27) | −0.01 |
|
| ||||
| PrEP facilitators: altruism | 3.77 (1.50); Range: 1–5 | 0.68 | 0.11 (0.06)+ | 0.08 |
|
| ||||
| PrEP self-efficacy | 3.19 (0.60); Range: 1–4 | 0.55 | 0.33 (0.15)* | 0.10 |
|
| ||||
| PrEP barriers: mistrust | 2.35 (0.96); Range: 1–5 | 0.54 | −0.18 (0.09)* | −0.09 |
|
| ||||
| Concealment motivation | 3.38 (1.57); Range: 1–6 | 0.53 | 0.17 (0.05)** | 0.15 |
|
| ||||
| PrEP facilitators: navigation support | 3.84 (1.25); Range: 1–5 | 0.40 | 0.17 (0.08)* | 0.10 |
|
| ||||
| PrEP barriers: negative experience | 1.50 (1.16); Range: 1–5 | 0.39 | −0.14 (0.07)* | −0.09 |
|
| ||||
| Financial stress | 3.15 (1.22); Range: 1–5 | 0.29 | −0.14 (0.06)* | −0.10 |
|
| ||||
| PrEP stigma | 1.99 (0.84); Range: 1–4.60 | 0.26 | −0.22 (0.10)* | −0.10 |
|
| ||||
| Model 2: Behavioral Health Treatment Cascade | ||||
|
| ||||
| Predictors | Descriptive Statistics of Predictor Variable (Mean/SD + Range or Frequency/%) | SSVS Marginal Inclusion Probability (N=253)♦ | Multiple Linear Regression Model (N=284)♦ | |
|
| ||||
| B (SE) | Effect Size (semi-partial correlation, sr) | |||
|
| ||||
| A doctor or provider suggested treatment | 28 (9.7%) | 1.00 | 1.18 (0.22)** | 0.35 |
|
| ||||
| Perceived self to need treatment | 168 (57.9%) | 1.00 | 0.92 (0.14)** | 0.27 |
|
| ||||
| Would seek family/friend support for BH | 252 (86.9%) | 0.96 | −0.69 (0.19)** | −0.15 |
|
| ||||
| High perceived community norms for BH treatment | 33 (11.4%) | 0.96 | 0.87 (0.19)** | 0.19 |
|
| ||||
| Friend/partner/family suggested treatment | 99 (34.1%) | 0.93 | 0.54 (0.15)** | 0.15 |
|
| ||||
| BH facilitators: BH being normalized | 3.34 (1.25); Range: 1–5 | 0.59 | −0.22 (0.06)** | −0.14 |
|
| ||||
| BH facilitators: knowledge | 3.84 (1.33); Range: 1–5 | 0.47 | 0.21 (0.06)** | 0.15 |
|
| ||||
| Attribute MH concerns to environment/culture | 203 (70.0%) | 0.45 | 0.30 (0.14)* | 0.09 |
|
| ||||
| Discrimination: immigration status | 5.34 (1.36); Range: 5–18 | 0.21 | −0.10 (0.05)* | −0.09 |
Note. The full list of marginal inclusion probabilities for each model is included in Electronic Supplementary Tables 1 and 2.
p < .01
p < .05
p < .10
Behavioral Health Cascade
SSVS identified nine variables with higher inclusion probabilities (see electronic supplementary materials for all variables considered by SSVS), which were included in a multiple linear regression model (see Table 2). All variables were individually and collectively associated with BH treatment engagement, F(9,274) = 32.67, p < 0.001, adj. R2 = 0.502. LSMM were further along the BH treatment cascade if a medical provider recommended treatment (p < 0.001), they perceived themselves to need treatment (p < 0.001), they perceived there to be high community norms for BH treatment (p < 0.001), a friend, romantic partner, or family member suggested treatment (p < 0.001), they reported that knowledge of BH services did or would facilitate their use of services (p < 0.001), and they attributed mental health concerns to environmental/cultural causes (p = 0.034). LSMM who were less engaged in BH treatment preferred family/friend support for mental health concerns (p < 0.001), reported that BH treatment being normalized did or would facilitate their use of BH treatment (p < 0.001), and reported more immigration-based discrimination (p = 0.042).
Discussion
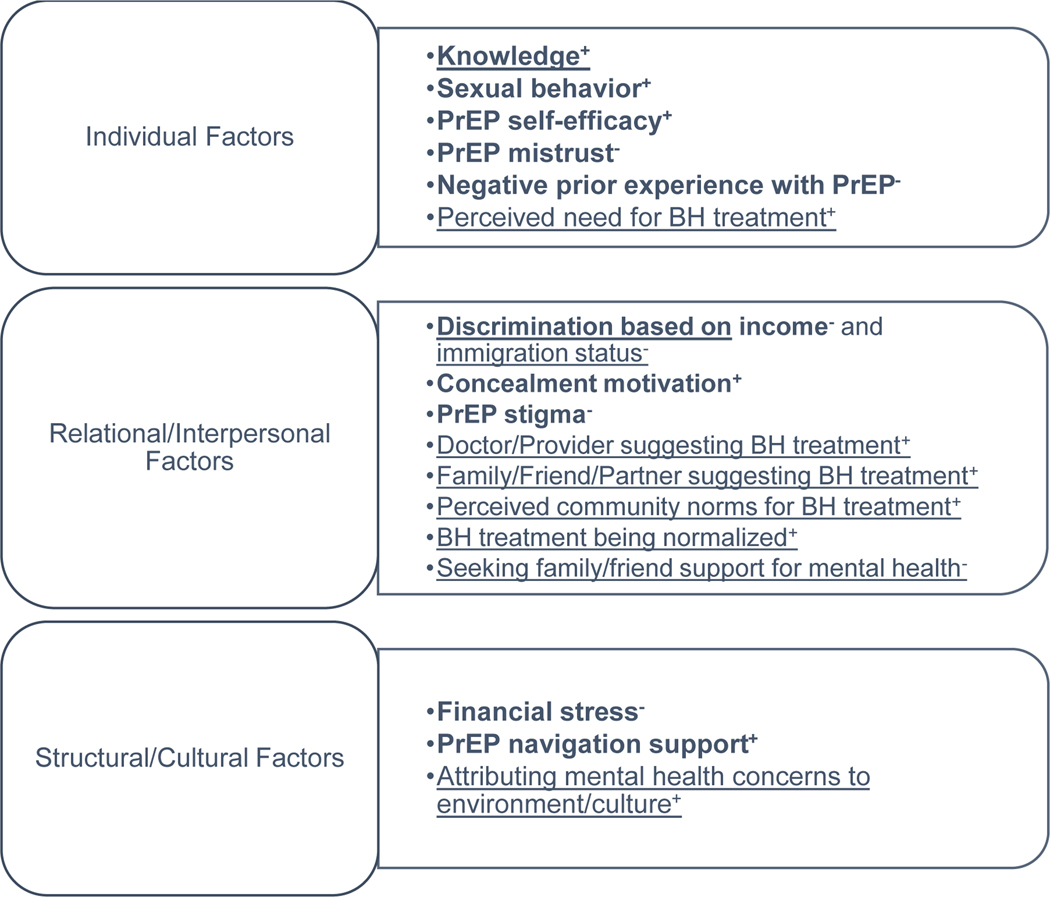
The purpose of this exploratory study was to identify multilevel factors that are quantitatively associated with engagement in PrEP and BH treatment among LSMM in South Florida. Figure 1 distills our key findings into individual, interpersonal/relational, and structural/cultural level determinants and suggests that most determinants were at the interpersonal/relational level. Identifying these factors is important given the HIV disparities that LSMM face in South Florida and across the US, as well as BH disparities which also fuel the HIV epidemic. Furthermore, we utilized modern statistical modeling (Bainter et al., 2020) to increase replicability and inform implementation planning to address disparities.
Figure 1.
Multilevel Model of LSMM’s PrEP and Behavioral Health Treatment Engagement
Note. Constructs associated with only PrEP engagement are in bold. Constructs associated with only BH treatment engagement are underlined. Constructs associated with both PrEP and BH treatment engagement are bolded and underlined. Facilitators+ and barriers− are noted.
Key relational and interpersonal factors associated with both PrEP and BH treatment engagement were discrimination (based on income and immigration status). Consistent with prior literature, PrEP stigma was a relational determinant impeding PrEP engagement (Lelutiu-Weinberger & Golub, 2016). BH treatment engagement was positively associated with several relational factors, such as LSMM’s medical providers recommending treatment, people in their social network suggesting treatment, and knowing more people who had engaged in BH treatment. LSMM who preferred to talk to a friend or family member about their mental health concerns, however, were less engaged in professional BH treatment. Similar findings have been shown among Latina/o/x adults in the U.S. (Villatoro, Morales, & Mays, 2014). The fact that LSMM who preferred friend or family support for mental health has implications for developing culturally congruent peer-led outreach and BH interventions (Jacquez, Vaughn, & Suarez-Cano, 2019; Rhodes, Foley, Zometa, & Bloom, 2007; Sun et al., 2015)
Individual factors were also associated with PrEP and BH treatment engagement. Knowledge about PrEP and BH treatment was associated positively with engagement in these services. As documented in prior literature, knowledge and stigma are linked and peers can be a source of either stigmatizing or normalizing information (Harkness et al., 2021; Hernandez Altamirano, Mayo, Chan, Safren, & Harkness, 2020). Although knowledge is an individual-level factor, it could be modified through LSMM’s relational networks. LSMM’s perception that they needed BH treatment was also associated with more engagement. Perceived need is also an individual-level determinant of engagement, suggesting the utility of implementation strategies enhancing the perceived relevance of PrEP and BH treatment to LSMM. This may be particularly important for PrEP, as LSMM who were sexually active, but not meeting guidelines for “higher risk” of acquiring HIV based on CDC criteria, were not more engaged than those who were not sexually active. CDC recently released new guidelines for providers to inform all sexually active adults about PrEP (Centers for Disease Control and Prevention, 2021), suggesting the potential need for providers to align with these new PrEP practice guidelines to achieve EHE goals.
Finally, structural and cultural factors were associated with engagement in services. Financial stress was associated with less engagement in PrEP services, which suggests the need for structural-level implementation strategies (e.g., reducing cost of PrEP services – including follow up care) to address this determinant. LSMM who viewed PrEP navigation support as a facilitator to PrEP use were more engaged in PrEP, suggesting the utility of building in this type of strategy to clinics and community health centers to enhance engagement (Blashill et al., 2021; Doblecki-Lewis et al., 2019). For BH treatment, those who attributed mental health concerns to environment/culture were more engaged in treatment, suggesting that outreach strategies might underscore the relevance of treatment for addressing environmental/cultural stressors that may be important to LSMM.
We also identified a counterintuitive finding that warrants further exploration. LSMM with higher concealment motivation were more engaged in PrEP. Our finding that concealment motivation (i.e., viewing one’s sexual orientation as personal/private, being careful about who knows about one’s sexual and romantic relationships, keeping same sex romantic relationships private) was associated with more PrEP engagement was unexpected given our prior qualitative findings suggesting LSMM with higher stigma or who are not “out” might be less engaged in PrEP (Harkness et al., 2021). Concealment motivation is a unique construct, though, compared to stigma and outness, as shown by the operationalization of the construct by this measure. Further, concealment motivation may have been associated with more PrEP engagement when contextualized by the other factors in the regression model; for example, LSMM who were more motivated to conceal their sexual orientation but also had high PrEP knowledge, self-efficacy for obtaining PrEP, and navigation support may have been particularly prepared to obtain PrEP.
A secondary finding is the extent to which LSMM’s PrEP and BH treatment needs are unmet. Although LSMM whose sexual behavior was consistent with CDC HIV PrEP guidelines were more engaged in PrEP services, research and the new CDC guidelines suggest the need to discuss PrEP with all sexually active adults (Beymer et al., 2017; Centers for Disease Control and Prevention, 2021; Freeborn, Portillo, Boyer, & Santos, 2020). BH treatment appeared to be even more insufficiently reaching LSMM in this study, as illustrated by the overall level of BH concerns compared to the overall engagement in BH treatment.
Despite the strengths of this study, it has limitations. It is unknown the extent to which the BH treatments LSMM received were evidence-based. Although the predictors for each model largely overlapped, there were some differences, which affects the comparability of the PrEP and BH models. Our prior qualitative work and relevant theories identified potentially important and likely correlated predictors. Because we did not have a sufficient theoretical basis to predict a priori which factors would be most important in a multiple regression analysis, we utilized SSVS to identify predictors that were most reliably associated with the outcome accounting for uncertainty in which other variables were included (Bainter et al., 2020). Additionally, we took this approach given the overarching purpose of the study, which was to identify the most relevant predictors from our qualitative work and from prior research, versus testing a specific set of pathways of associations. Accordingly, the current study also did not examine moderators and mechanisms of action, which can be tested in longitudinal designs. Finally, this study did not examine PrEP and BH treatment determinants among other key populations affected by HIV disparities. For example, Latina transwomen were not included in the current study because of the need to not conflate the needs of transwomen and MSM (Bass et al., 2022; T. C. Poteat, van der Merwe, Sevelius, & Keatley, 2021; Sevelius, Keatley, Calma, & Arnold, 2016) and research showing that transwomen have unique HIV prevention needs (Chyten-Brennan, Patel, Anastos, & Hanna, 2022; Dang et al., 2022; T. Poteat, German, & Flynn, 2016). Research specifically examining the needs of other key populations affected by HIV (without conflating these communities), including Latina transwomen, is needed.
Conclusion
In summary, the current study identified multilevel, modifiable factors associated with LSMM’s engagement in PrEP and BH treatment. Addressing relational (e.g., stigma, perceived norms), individual (e.g., knowledge, self-efficacy), and structural/cultural (e.g., financial stress) determinants identified in our study through a multilevel implementation strategy could facilitate LSMM’s engagement in both PrEP and BH treatment. Implementation strategies that seek to scale up PrEP and BH treatment to LSMM are key to Ending the HIV Epidemic.
Supplementary Material
Acknowledgements:
We would like to thank Pranusha Atuluru, Bill Chan, Tiffany Glynn, Michaela Larson, Cassandra Michel, Vanessa Morales, Rosana Smith-Alvarez, Jaislene Viñas, Joey Waknin, Elliott Weinstein, and Annette Yates for their assistance with this project. We also thank every participant in the study and the many community members and partners who shared information about the study to prospective participants.
Funding:
Data collection for this study was supported by P30AI073961 (Pahwa) and U54MD002266 (Behar-Zusman). Additional research support was provided by P30MH116867 (Safren). Some of the author time was supported by K24DA040489 (Safren), K23MD015690 (Harkness), and the Providence/Boston Center for AIDS Research P30AI042853 (Rogers). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest: Dr. Safren receives royalties from Oxford University Press, Gilford Publications, and Springer/Humana Press for books on cognitive behavioral therapy. The authors have no other conflicts of interest to disclose.
Declarations
Ethics Approval: All study procedures were reviewed by the University of Miami Institutional Review Board and were performed in line with the principles of the Declaration of Helsinki.
Consent to Participate: Informed consent was obtained from all individual participants included in the study.
Consent for Publication: Not applicable
As recommended by del Río-González (2021), we use “Latina/x/o” when referring to the community at large and “Latino” when referring to men.
Availability of Data and Material:
The data that support the findings of this study are available upon reasonable request (e.g., methodologically sound proposal and signed data use agreement) from the corresponding author [AH], following publication.
References
- Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, … Team, F. the iPrEx S. (2012). Emtricitabine-Tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Science Translational Medicine, 4(151), 151ra125–151ra125. 10.1126/scitranslmed.3004006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, & Patrick DL (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine, 10(2), 77–84. [PubMed] [Google Scholar]
- Andrinopoulos K, & Hembling J. (2013). Health service utilization among men who have sex with men and transgender women, San Salvador, El Salvador 2011–2012. MEASURE Evaluation. Retrieved from MEASURE Evaluation website: https://www.measureevaluation.org/resources/publications/tr-13-92 [Google Scholar]
- Bainter SA, McCauley TG, Wager T, & Losin EAR (2020). Improving practices for selecting a subset of important predictors in psychology: An application to predicting pain. Advances in Methods and Practices in Psychological Science. (Sage CA: Los Angeles, CA: ). 10.1177/2515245919885617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass SB, Kelly PJ, Brajuha J, Gutierrez-Mock L, Koester K, D’Avanzo P, & Sevelius J. (2022). Exploring barriers and facilitators to PrEP use among transgender women in two urban areas: Implications for messaging and communication. BMC Public Health, 22(1), 17. 10.1186/s12889-021-12425-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beymer MR, Weiss RE, Sugar CA, Bourque LB, Gee GC, Morisky DE, … Bolan RK (2017). Are Centers for Disease Control and Prevention Guidelines for Preexposure Prophylaxis Specific Enough? Formulation of a Personalized HIV Risk Score for Pre-Exposure Prophylaxis Initiation. Sexually Transmitted Diseases, 44(1), 49–57. 10.1097/OLQ.0000000000000535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blashill AJ, Brady JP, Rooney BM, Rodriguez-Diaz CE, Horvath KJ, Blumenthal J, … Safren SA (2020). Syndemics and the PrEP cascade: Results from a sample of young Latino men who have sex with men. Archives of Sexual Behavior, 49(1), 125–135. 10.1007/s10508-019-01470-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blashill AJ, Gordon JR, Rojas SA, Ramers CB, Lin C-D, Carrizosa CM, … Wells KJ (2021). Pilot randomised controlled trial of a patient navigation intervention to enhance engagement in the PrEP continuum among young Latino MSM: A protocol paper. BMJ Open, 11(5), e040955. 10.1136/bmjopen-2020-040955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Cefalu M, Wong EC, Burnam MA, Hunter GP, Florez KR, & Collins RL (2017). Racial/ethnic differences in perception of need for mental health treatment in a US national sample. Social Psychiatry and Psychiatric Epidemiology, 52(8), 929–937. 10.1007/s00127-017-1400-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT Alcohol Consumption Questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine, 158(16), 1789–1795. 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: A clinical practice guideline. Retrieved from https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2020a). Diagnoses of HIV infection in the United States and dependent areas, 2018 (No. 31). Centers for Disease Control and Prevention. Retrieved from Centers for Disease Control and Prevention website: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-updated-vol-31.pdf
- Centers for Disease Control and Prevention. (2020b). Estimated HIV incidence and prevalence in the United States, 2014–2018 (No. 25). Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-25-1.pdf?deliveryName=FCP_2_USCDCNPIN_162-DM27706&deliveryName=USCDC_1046-DM27774 [Google Scholar]
- Centers for Disease Control and Prevention. (2021). US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 update: A clinical practice guideline. Retrieved from https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
- Cervantes RC, Fisher DG, Padilla AM, & Napper LE (2015). The Hispanic Stress Inventory Version 2: Improving the assessment of acculturation stress. Psychological Assessment, 28(5), 509–522. 10.1037/pas0000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chyten-Brennan J, Patel VV, Anastos K, & Hanna DB (2022). The role of gender-affirming hormonal care in HIV care continuum outcomes when comparing transgender women with cisgender sexual minority men. JAIDS Journal of Acquired Immune Deficiency Syndromes, 10.1097/QAI.0000000000003056. 10.1097/QAI.0000000000003056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, Zuvekas SH, Carson N, Wayne GF, Vesper A, & McGuire TG (2014). Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Services Research, 49(1), 206–229. 10.1111/1475-6773.12095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K. (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review, 43(6), 1241–1299. [Google Scholar]
- Dang M, Scheim AI, Teti M, Quinn KG, Zarwell M, Petroll AE, … John SA (2022). Barriers and Facilitators to HIV Pre-Exposure Prophylaxis Uptake, Adherence, and Persistence Among Transgender Populations in the United States: A Systematic Review. AIDS Patient Care and STDs, 36(6), 236–248. 10.1089/apc.2021.0236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Río-González AM (2021). To Latinx or not to Latinx: A question of gender inclusivity versus gender neutrality. American Journal of Public Health, 111(6), 1018–1021. 10.2105/AJPH.2021.306238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz RM, Morales ES, Bein E, DiláN E, & RodríGuez RA (1999). Predictors of sexual risk in Latino gay/bisexual men: The role of demographic, developmental, social cognitive, and behavioral variables. Hispanic Journal of Behavioral Sciences, 21(4), 480–501. 10.1177/0739986399214007 [DOI] [Google Scholar]
- Doblecki-Lewis S, Butts S, Botero V, Klose K, Cardenas G, & Feaster D. (2019). A randomized study of passive versus active PrEP patient navigation for a heterogeneous population at risk for HIV in South Florida. Journal of the International Association of Providers of AIDS Care, 18. 10.1177/2325958219848848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Schweinle W, & Anderson SM (2008). Reliability and validity of the attitudes toward Seeking Professional Psychological Help Scale-Short Form. Psychiatry Research, 159(3), 320–329. 10.1016/j.psychres.2007.04.020 [DOI] [PubMed] [Google Scholar]
- Escobar KM, & Gorey KM (2018). Cognitive behavioral interventions for depression among Hispanic people: Promising meta-analytic evidence for deep cultural adaptations. Social Work in Mental Health, 16(6), 746–758. 10.1080/15332985.2018.1476284 [DOI] [Google Scholar]
- Evans-Lacko S, Little K, Meltzer H, Rose D, Rhydderch D, Henderson C, & Thornicroft G. (2010). Development and psychometric properties of the Mental Health Knowledge Schedule. Canadian Journal of Psychiatry. Revue Canadienne De Psychiatrie, 55(7), 440–448. 10.1177/070674371005500707 [DOI] [PubMed] [Google Scholar]
- Fauci AS, Redfield RR, Sigounas G, Weahkee MD, & Giroir BP (2019). Ending the HIV epidemic: A plan for the United States. JAMA, 321(9), 844–845. 10.1001/jama.2019.1343 [DOI] [PubMed] [Google Scholar]
- Feinstein BA, Johnson BA, Parsons JT, & Mustanski B. (2017). Reactions to testing HIV negative: Measurement and associations with sexual risk behaviour among young MSM who recently tested HIV negative. AIDS and Behavior, 21(5), 1467–1477. 10.1007/s10461-016-1525-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Freeborn K, Portillo C, Boyer CB, & Santos GM (2020). Misclassification of sexual health risks in a self-identified low risk cohort of men who have sex with men (MSM) enrolled in a community based PrEP program. AIDS Care, 32(2), 230–237. 10.1080/09540121.2019.1620167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George E,I, & McCulloch RE (1993). Variable selection via Gibbs sampling. Journal of the American Statistical Association, 88(423), 881–889. [Google Scholar]
- Gierk B, Kohlmann S, Kroenke K, Spangenberg L, Zenger M, Brähler E, & Löwe B. (2014). The Somatic Symptom Scale-8 (SSS-8): A brief measure of somatic symptom burden. JAMA Internal Medicine, 174(3), 399–407. 10.1001/jamainternmed.2013.12179 [DOI] [PubMed] [Google Scholar]
- Golub SA, & Gamarel KE (2013). The impact of anticipated HIV stigma on delays in HIV testing behaviors: Findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care and STDs, 27(11), 621–627. 10.1089/apc.2013.0245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JW (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, … Glidden DV (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine, 363(27), 2587–2599. 10.1056/NEJMoa1011205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Rendina HJ, Whitfield THF, Ventuneac A, & Parsons JT (2016). Changes in Familiarity with and Willingness to Take Preexposure Prophylaxis in a Longitudinal Study of Highly Sexually Active Gay and Bisexual Men. LGBT Health, 3(4), 252–257. 10.1089/lgbt.2015.0123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Whitfield THF, Rendina HJ, Ventuneac A, & Parsons JT (2015). Willingness to take PrEP and potential for risk compensation among highly sexually active gay and bisexual men. AIDS and Behavior, 19(12), 2234–2244. 10.1007/s10461-015-1030-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness A, Satyanarayana S, Mayo D, Smith-Alvarez R, Rogers BG, Prado G, & Safren SA (2021). Scaling up and out HIV-prevention and behavioral health services to Latino sexual minority men in South Florida: Multilevel implementation barriers, facilitators, and strategies. AIDS Patient Care & STDs, 35(5), 167–179. 10.1089/apc.2021.0018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heppner PP, Witty TE, & Dixon WA (2004). Problem-solving appraisal and human adjustment: A review of 20 years of research using the Problem Solving Inventory. The Counseling Psychologist, 32(3), 344–428. 10.1177/0011000003262793 [DOI] [Google Scholar]
- Hernandez Altamirano D, Mayo D, Chan B, Safren SA, & Harkness A. (2020, November). PrEP knowledge as a protective factor for intent to use PrEP among Latinx Sexual Minority Men in Miami. Poster presentation presented at the Association for Behavioral and Cognitive Therapies 54th Annual Convention (Held Virtually due to COVID-19), Philadelphia, PA, United States. Philadelphia, PA, United States. [Google Scholar]
- HPTN 083 study team. (2017). HPTN 083 Enrollment Behavioral CASI - English Version 2.0. [Google Scholar]
- Jacquez F, Vaughn LM, & Suarez-Cano G. (2019). Implementation of a stress intervention with Latino immigrants in a non-traditional migration city. Journal of Immigrant and Minority Health, 21(2), 372–382. 10.1007/s10903-018-0732-7 [DOI] [PubMed] [Google Scholar]
- Jimenez DE, Bartels SJ, Cardenas V, Dhaliwal SS, & Alegría M. (2012). Cultural beliefs and mental health treatment preferences of ethnically diverse older adult consumers in primary care. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 20(6), 533–542. 10.1097/JGP.0b013e318227f876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M, & Breton S. (1997). Barriers to Treatment Participation Scale: Evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 38(8), 1051–1062. 10.1111/j.1469-7610.1997.tb01621.x [DOI] [PubMed] [Google Scholar]
- Kurtines WM, & Szapocznik J. (1995). Cultural competence in assessing Hispanic youths and families: Challenges in the assessment of treatment needs and treatment evaluation for Hispanic drug-abusing adolescents. NIDA Research Monograph, 156, 172–189. [PubMed] [Google Scholar]
- Lelutiu-Weinberger C, & Golub SA (2016). Enhancing PrEP access for Black and Latino men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 73(5), 547–555. 10.1097/QAI.0000000000001140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano A, Lee T, Fernandez A, Prado G, Safren S, Jimenez D, & Harkness A. (Under Review). Factor structure and measurement invariance of the Cultural Attitudes Toward Healthcare and Mental Illness Questionnaire among Latino sexual minority men. [Google Scholar]
- Lubben J, Blozik E, Gillmann G, Iliffe S, von Renteln Kruse W, Beck JC, & Stuck AE (2006). Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. The Gerontologist, 46(4), 503–513. 10.1093/geront/46.4.503 [DOI] [PubMed] [Google Scholar]
- Martinez O, Arreola SG, Wu E, Muñoz-Laboy M, Levine E, Rutledge SE, … Sandfort T. (2016). Syndemic factors associated with adult sexual HIV risk behaviors in a sample of Latino men who have sex with men in New York City. Drug and Alcohol Dependence, 166(1), 258–262. 10.1016/j.drugalcdep.2016.06.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrani VB, O’Day JE, Norris TB, & Adebayo OW (2017). Development and dissemination of the El Centro Health Disparities Measures Library. Journal of Nursing Scholarship, 49(5), 564–571. 10.1111/jnu.12321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno Y, Borkowf C, Millett GA, Bingham T, Ayala G, & Stueve A. (2012). Homophobia and racism experienced by Latino men who have sex with men in the United States: Correlates of exposure and associations with HIV risk behaviors. AIDS and Behavior, 16(3), 724–735. 10.1007/s10461-011-9967-1 [DOI] [PubMed] [Google Scholar]
- Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The Lesbian, Gay, and Bisexual Identity Scale. Journal of Counseling Psychology, 58(2), 234–245. 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Office of Infectious Disease. (2020, November 3). Priority jurisdictions: Phase I. Retrieved June 7, 2021, from HIV.gov website: https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/jurisdictions/phase-one
- Pachankis JE, Eldahan AI, & Golub SA (2016). New to New York: Ecological and psychological predictors of health among recently arrived young adult gay and bisexual urban migrants. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 50(5), 692–703. 10.1007/s12160-016-9794-8 [DOI] [PubMed] [Google Scholar]
- Parsons JT, Rendina HJ, Lassiter JM, Whitfield THF, Starks TJ, & Grov C. (2017). Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States: The motivational PrEP cascade. Journal of Acquired Immune Deficiency Syndromes (1999), 74(3), 285–292. 10.1097/QAI.0000000000001251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. (2020). U.S. Hispanic population surpassed 60 million in 2019, but growth has slowed. Retrieved June 24, 2021, from Pew Research Center website: https://www.pewresearch.org/fact-tank/2020/07/07/u-s-hispanic-population-surpassed-60-million-in-2019-but-growth-has-slowed/
- Pineros-Leano M, Liechty JM, & Piedra LM (2017). Latino immigrants, depressive symptoms, and cognitive behavioral therapy: A systematic review. Journal of Affective Disorders, 208, 567–576. 10.1016/j.jad.2016.10.025 [DOI] [PubMed] [Google Scholar]
- Poteat TC, van der Merwe LLA, Sevelius J, & Keatley J. (2021). Inclusion as illusion: Erasing transgender women in research with MSM. Journal of the International AIDS Society, 24(1), e25661. 10.1002/jia2.25661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat T, German D, & Flynn C. (2016). The conflation of gender and sex: Gaps and opportunities in HIV data among transgender women and MSM. Global Public Health, 11(7–8), 835–848. 10.1080/17441692.2015.1134615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, … Tiet QQ (2016). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and evaluation within a Veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211. 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, & Velicer WF (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion: AJHP, 12(1), 38–48. 10.4278/0890-1171-12.1.38 [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J, Garcia D, Campbell RT, Diaz RM, & Heckathorn DD (2008). HIV infection, sexual risk behavior, and substance use among Latino gay and bisexual men and transgender persons. American Journal of Public Health, 98(6), 1036–1042. 10.2105/AJPH.2006.102624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina HJ, Whitfield THF, Grov C, Starks TJ, & Parsons JT (2017). Distinguishing hypothetical willingness from behavioral intentions to initiate HIV pre-exposure prophylaxis (PrEP): Findings from a large cohort of gay and bisexual men in the U.S. Social Science & Medicine (1982), 172, 115–123. 10.1016/j.socscimed.2016.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Foley KL, Zometa CS, & Bloom FR (2007). Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. American Journal of Preventive Medicine, 33(5), 418–427. 10.1016/j.amepre.2007.07.023 [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Martinez O, Song E-Y, Daniel J, Alonzo J, Eng E, … Reboussin B. (2013). Depressive symptoms among immigrant Latino sexual minorities. American Journal of Health Behavior, 37(3), 404–413. 10.5993/AJHB.37.3.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, & Pachankis JE (2019). Prevalence of psychiatric disorders at the intersection of race and sexual orientation: Results from the National Epidemiologic Survey of Alcohol and Related Conditions-III. Journal of Consulting and Clinical Psychology, 87(4), 321–331. 10.1037/ccp0000377 [DOI] [PubMed] [Google Scholar]
- Sevelius JM, Keatley J, Calma N, & Arnold E. (2016). ‘I am not a man’: Trans-specific barriers and facilitators to PrEP acceptability among transgender women. Global Public Health, 11(7–8), 1060–1075. 10.1080/17441692.2016.1154085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M, & Clair S. (2003). Syndemics and public health: Reconceptualizing disease in bio-social context. Medical Anthropology Quarterly, 17(4), 423–441. 10.1525/maq.2003.17.4.423 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Steketee G, Perry J, Goisman R, Warshaw M, Massion A, Peterson L, … Keller M. (1997). The psychosocial treatments interview for anxiety disorders. A method for assessing psychotherapeutic procedures in anxiety disorders. The Journal of Psychotherapy Practice and Research, 6(3), 194–210. [PMC free article] [PubMed] [Google Scholar]
- Sternthal MJ, Slopen N, & Williams DR (2011). Racial disparities in health: How much does stress really matter? Du Bois Review: Social Science Research on Race, 8(1), 95–113. 10.1017/S1742058X11000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun CJ, García M, Mann L, Alonzo J, Eng E, & Rhodes SD (2015). Latino sexual and gender identity minorities promoting sexual health within their social networks: Process evaluation findings from a lay health advisor intervention. Health Promotion Practice, 16(3), 329–337. 10.1177/1524839914559777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner A, Reboussin B, Mann L, Ma A, Song E, Alonzo J, & Rhodes S. (2014). Factors influencing health care access perceptions and care-seeking behaviors of immigrant Latino sexual minority men and transgender individuals: Baseline findings from the HOLA intervention study. Journal of Health Care for the Poor and Underserved, 25(4), 1679–1697. 10.1353/hpu.2014.0156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa S, Doucerain MM, Miglietta A, Jurcik T, Ryder AG, & Gattino S. (2019). The Vancouver Index of Acculturation (VIA): New evidence on dimensionality and measurement invariance across two cultural settings. International Journal of Intercultural Relations, 71, 60–71. 10.1016/j.ijintrel.2019.04.001 [DOI] [Google Scholar]
- Valdez LA, Flores M, Ruiz J, Oren E, Carvajal S, & Garcia DO (2018). Gender and cultural adaptations for diversity: A systematic review of alcohol and substance abuse interventions for Latino males. Substance Use & Misuse, 53(10), 1608–1623. 10.1080/10826084.2017.1417999 [DOI] [PubMed] [Google Scholar]
- Villatoro AP, Morales ES, & Mays VM (2014). Family culture in mental health help-seeking and utilization in a nationally representative sample of Latinos in the United States: The NLAAS. American Journal of Orthopsychiatry, 84(4), 353–363. 10.1037/h0099844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, & Ascheman PL (2009). Measuring perceptions of stigmatization by others for seeking psychological help: Reliability and validity of a new stigma scale with college students. Journal of Counseling Psychology, 56(2), 301–308. 10.1037/a0014903 [DOI] [Google Scholar]
- Walsh JL (2019). Applying the information–motivation–behavioral skills model to understand PrEP intentions and use among men who have sex with men. AIDS and Behavior, 23(7), 1904–1916. 10.1007/s10461-018-2371-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warttig SL, Forshaw MJ, South J, & White AK (2013). New, normative, English-sample data for the Short Form Perceived Stress Scale (PSS-4). Journal of Health Psychology, 18(12), 1617–1628. 10.1177/1359105313508346 [DOI] [PubMed] [Google Scholar]
- Williams DR, Yan Yu, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available upon reasonable request (e.g., methodologically sound proposal and signed data use agreement) from the corresponding author [AH], following publication.