Abstract
Simian-human immunodeficiency virus (SHIV) infection in macaques provides a convenient model for testing vaccine efficacy and for understanding viral pathogenesis in AIDS. We immunized macaques with recombinant, Salmonella typhimurium (expressing Gag) or soluble Gag in adjuvant to generate T-cell-dependent lymphoproliferative or serum antibody responses. Immunized animals were challenged by intrarectal inoculation with SHIV89.6PD. Virus infection was accompanied by rapid losses of lymphoproliferative responses to Gag or phytohemagglutinin. By 8 weeks, mitogen responses recovered to near normal levels but antigen-specific immunity remained at low or undetectable levels. Serum antibody levels were elevated initially by virus exposure but soon dropped well below levels achieved by immunization. Our studies show a rapid depletion of preexisting Gag-specific CD4+ T cells that prevent or limit subsequent antiviral cellular and humoral immune responses during acute SHIV infection.
The unique challenge for AIDS vaccine development is to elicit strong immunity against a virus that infects and destroys CD4+ T cells. Vaccination strategies must provide sufficient protection against infection or disease while avoiding the possibility of activating these helper T cells and targeting them for elimination. Our studies examine the effects of acute virus infection on immune responses to Gag protein in vaccinated animals. In particular, we use vaccination as a tool to elicit specific immunity and then assess the effects of simian-human immunodeficiency virus (SHIV) infection in terms of changes in these immune responses. Our goals are to understand further the host-pathogen interaction, to examine the effects of acute infection on the CD4+ T-cell repertoire, and to evaluate the consequences of eliciting only limited types of immune responses.
We selected two distinct approaches for generating Gag-specific immunity in macaques. In an effort to promote cellular immune responses, we developed recombinant Salmonella typhimurium strains expressing the simian immunodeficiency virus (SIV) p27Gag protein. Intragastric (i.g.) immunization of mice with recombinant Salmonella elicited strong cytotoxic-T-cell (CTL) responses and secretory immunoglobulin A (secretory IgA) (17). The same recombinant bacterial strain elicited antigen-specific lymphoproliferative responses in macaques, though we did not observe cytotoxic-T-cell or secretory IgA responses (15). Alternatively, we employed a conventional intramuscular (i.m.) immunization with purified recombinant p27 (14) to elicit serum IgG responses. Based on a previous study of Gag-specific antibody responses in human-immunodeficiency virus (HIV)-positive people (1), we assumed that serum antibodies to Gag in macaques would also be a T-cell-dependent response. These immunization methods provided two independent approaches to assessing CD4+ T-cell function during acute infection of macaques. The pathogenic SHIV89.6PD was selected as a challenge stock for these immunization studies. SHIV89.6PD caused virulent infections in rhesus macaques after intrarectal virus inoculation (4). Infection was apparent within weeks after inoculation, as judged by high levels of antigenemia in plasma, efficient virus isolation from peripheral blood mononuclear cells (PBMC), and substantial losses of CD4+ T cells and CD20+ B cells (13).
Efforts to understand HIV, SIV, or SHIV infection are confounded by the paradox that activated CD4+ T cells are required for effective antiviral immune responses and also constitute the fertile ground for virus replication. High-level lymphoproliferative responses to HIV-1 p24 protein have been correlated with slower disease progression or a positive treatment outcome (8), while others have reported that broad proliferative responses to HIV-1 epitopes place the individual at greater risk for disease progression, presumably by increasing the numbers of activated CD4+ T cells available for virus replication (11). These results emphasize that CD4+ T cells have many roles during lentivirus infection and it is not possible to predict the consequences of eliciting strong helper responses through vaccination.
Our studies of immunization and SHIV challenge examine one specific aspect of immunity that may be important for a vaccine against HIV in humans. Changes in immunity during the initial few weeks after virus challenge in macaques provide an explanation for the generally poor humoral immune responses during natural infection and may show how a virulent virus can eliminate vaccine-induced immunity when insufficient or incorrect effector mechanisms are in place prior to virus exposure.
MATERIALS AND METHODS
p27 vaccination.
Twelve captivity-bred, SIV-seronegative rhesus macaques (Macaca mulatta) were divided randomly into four groups and immunized by two routes with the SIV capsid antigen. The routes for p27 immunization were i.m. injection with 100 μg of purified SIV p27 in a solution containing 1 mg/ml of polyphosphazene (Adjumer; Avant Immunotherapeutics, Cambridge, Mass.) or i.g. intubation with approximately 1011 recombinant, attenuated Salmonella typhimurium PV4570 cells expressing SIV p27 (14, 15, 17). Animals were immunized three times (weeks −43, −35, and −2 relative to virus challenge). We determined previously the amount of p27 protein produced by recombinant strain PV4570 (14). Using these values, we calculated that animals, including those assigned to i.m., i.g., and mixed regimens, received between 205 and 300 μg of p27 over the course of three immunizations. Macaques were monitored for p27-specific cellular and humoral immune responses after each immunization, and a detailed account of p27-specific immune responses was reported previously (15). Table 1 summarizes immunizations and p27-specific immune responses that were detected 1 week prior to virus challenge.
TABLE 1.
p27 immunization summary
| Groupa | Animal no. | Immune responseb
|
|
|---|---|---|---|
| Proliferationc (SI) | Antibody titerd | ||
| MMM | r94052 | 7.8 | 300,000 |
| r94061 | 8.6 | 300,000 | |
| r94071 | 1.1 | 150,000 | |
| MGG | r94057 | 4.9 | 1,600 |
| r94066 | 95.2 | 1,600 | |
| r94076 | 34.9 | 1,600 | |
| GMM | r94045 | 18.3 | 150,000 |
| r94063 | 4.3 | 150,000 | |
| r94072 | 4.1 | 100,000 | |
| GGG | r94058 | 21.2 | <400 |
| r94068 | 15.2 | <400 | |
| r94082 | 0.6 | <400 | |
Animals are grouped according to immunization regimen, each of which included three separate antigen exposures. M represents i.m. immunization with soluble p27 in adjuvant. G represents i.g. immunization with recombinant S. typhimurium. Immunization occurred at 43, 35, and 2 weeks prior to intrarectal virus challenge with SHIV89.6PD.
p27-specific responses 1 week before SHIV challenge.
Lymphoproliferation was elicited by in vitro exposure to purified recombinant p27 antigen. SI values were calculated as described in the text. SI values of ≥5.0 were considered positive.
Antibody titer is the maximum dilution of serum or plasma that was positive for virus-binding antibodies. The minimum dilution used in these assays was 1:400.
Virus challenge.
Ketamine hydrochloride (10 mg/kg of body weight) was used to restrain macaques before virus inoculation and blood collections. Macaques were inoculated intrarectally with 2,500 tissue culture infectious doses of a cell-free SHIV89.6PD virus stock following published protocols (5, 16). This dose (2,500) tissue culture infectious dose was shown previously to be the minimum dose required to establish infection after intrarectal virus inoculation (13). Derivation of the pathogenic SHIV89.6PD stock (6, 7) and the disease course in naive rhesus macaques after intrarectal inoculation (13) have been reported elsewhere.
Blood collection.
Whole venous blood was collected in heparinized tubes at 1, 2, 4, 8, 11, 15, and 19 weeks after virus challenge. General Medical Laboratories (Madison, Wis.) performed automated, complete blood counts on all samples. Cells for lymphocyte phenotyping were prepared by osmotic lysis of whole blood to remove erythrocytes. PBMC were isolated from whole blood after density gradient centrifugation with Ficoll-Hypaque (Pharmacia, Uppsala, Sweden). Plasma was decanted from the lowest-density fraction and was stored at −70°C.
Detecting serum antibody responses.
We used microtiter plates coated with HIV-2 antigens (Sanofi/Pasteur, Chaska, Minn.) to screen macaque sera for virus-binding antibodies before and after SHIV infection. Enzyme-linked immunoabsorbent assays were done according to manufacturers’ instructions, with plasma samples diluted 1:400 in phosphate-buffered saline (PBS). Results are reported as absorbance values at 450 nm.
Assay for lymphoproliferation.
Fresh PBMC (2 × 105) were cultured in flat-bottomed, 96-well plates with 200 μl of medium, phytohemagglutinin PHA (5 μl/ml), myoglobin (5 μg/ml), or recombinant p27 (5 μg/ml). [3H]thymidine (1 μCi; Dupont NEN, Boston, Mass.) was added to each well at 16 h before harvesting. Cells were collected onto glass fiber filters, and thymidine incorporation was measured by scintillation counting. All conditions were done in triplicate and counts per minute were averaged. Results are reported as stimulation indices (SI) (calculated as counts per minute for specific antigen/counts per minute for medium) for cultures harvested on day 4 of PHA stimulation or day 7 of p27 stimulation. PBMC cultured with myoglobin for 7 days had SI values of ≤1.5 (data not shown). We used the convention that positive SI values should be greater than three times that of the negative (myoglobin) control after background correction of data. For these studies, SI values of ≥5 were considered positive.
Lymphocyte phenotyping.
Cells were fixed in 1% paraformaldehyde and stained for lymphocyte surface markers as reported previously (13). Briefly, 5 × 105 cells were stained for 60 min at 4°C in phosphate-buffered saline containing 5% fetal bovine serum and an antibody against CD2, CD4, or CD20 conjugated directly to fluorescein-5-isothiocyanate. A total of 10,000 events were collected on a FACScan flow cytometer (Becton Dickinson, Indianapolis, Ind.). The absolute number of CD4+ and CD20+ cells per microliter of blood was calculated by multiplying the percentage of each lymphocyte subset times the absolute number of lymphocytes per microliter of blood from complete blood counts. The percentage of CD4+ or CD20+ cells remaining in circulation over the course of infection was calculated for each animal by using the following formulas: % remaining (at week x) = 100 + % change; % change = 100 × [(no. of cells at week x − no. of cells prior to infection)/no. of cells prior to infection].
RESULTS
p27-specific immunity prior to SHIV challenge.
Four groups of rhesus macaques were immunized three times each against the SIV capsid antigen prior to SHIV challenge (Table 1). p27 was administered at weeks −43, −35, and −2 relative to virus challenge by i.m. injection of purified p27, by i.g. intubation with recombinant attenuated S. typhimurium expressing SIV p27 (PV4570), or by a combination of these routes. Group MMM received three i.m. injections of purified p27, and the average end point antibody titer at 1 week before virus challenge was 1:250,000. Group GMM was given initially a single i.g. dose of recombinant S. typhimurium and then two i.m. booster injections of p27. The average end point titer of virus-specific antibodies in this group was 1:130,000 by 1 week prior to virus challenge. Previous studies with PV4570 indicated that a single immunization could prime capsid-specific lymphoproliferative responses, and the effect lasted at least 30 weeks (15). Although group GMM macaques did not have substantial lymphoproliferation at 1 week prior to SHIV inoculation, they were primed to p27 by the single PV4570 immunization at week −43 relative to infection.
Group GGG macaques received three PV4570 immunizations by the i.g. route. These animals developed lymphoproliferative responses to p27 but did not develop substantial serum antibody responses specific for p27. Group MGG macaques were immunized i.m. with p27 at week −43 and then received two booster immunizations with PV4570. The second PV4570 immunization at two weeks prior to challenge induced proliferation to p27 with an average SI of 45. These macaques had low-level serum antibody responses stimulated by the initial i.m. injection; however, the average antibody titer was only 1:1,600 by 1 week before virus inoculation (Table 1). These data on immune responses to p27 immunization summarize results that were reported previously (15) and are included here to document the baseline conditions for animals in the virus challenge study.
i.g., i.m., or combined immunizations did not protect against intrarectal SHIV89.6PD infection or subsequent disease.
PBMC from all 12 macaques were positive for virus isolation by 2 weeks after intrarectal SHIV inoculation. The number of PBMC required to detect infectious virus ranged from 102 to 106 (data not shown) and did not correlate with immunization schedules, preinfection proliferative responses, or antibody titers. All macaques remained virus isolation positive for at least 26 weeks after inoculation, except for rapidly progressing animals that were euthanatized prior to this time.
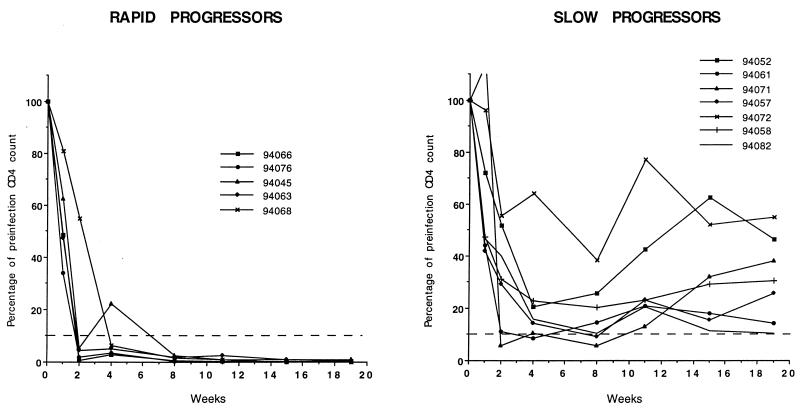
We examined CD4+ T-cell and CD20+ B-cell populations as a measure of disease course after virus challenge. Figure 1 depicts the percentages of circulating CD4+ T cells remaining after intrarectal SHIV challenge. Animals were classified as rapid or slow progressors on the basis of multiple markers, including CD4+ T-cell count and CD20+ B-cell count; these markers were correlated with duration of survival after infection (13). Four of the six macaques in groups MMM and GMM had positive anti-Gag serum antibody responses at the time of infection yet had ≤10% of starting CD4+ T-cell levels remaining by 2 weeks after virus challenge. One macaque from group MMM and one from group GMM had ∼50% of their circulating CD4+ T cells remaining throughout the 19 weeks of observation. Two macaques in group MMM that experienced large initial CD4+ T-cell losses subsequently showed increasing CD4+ T-cell levels that reached an average of 490 cells/μl of blood. This value is at the low end of the normal range for age-matched animals (10). Two macaques in group GMM experienced large, initial CD4+ T-cell losses and remained at low levels, with CD4+ T-cell numbers below 50 cells/μl of blood by 8 weeks after challenge.
FIG. 1.
CD4+ T-cell depletion in rapid- or slow-progressor macaques after intrarectal SHIV89.6PD inoculation. The pattern of CD4+ T-cell loss is shown for each animal in this challenge study over the interval from infection (week 0) to 19 weeks. Individual animals are identified by their unique five-digit codes. Data are expressed as the percentage of preinfection values based on the absolute CD4+ T cell count in blood. Animals were classified as rapid or slow progressors according to criteria published previously (13).
Macaques in groups MGG and GGG had mainly lymphoproliferative responses to Gag before virus challenge. Three of these six macaques had <10% of starting CD4+ T-cell levels remaining by 4 weeks after virus challenge. Only a single macaque (r94057) from group MGG had >10% of starting CD4+ T-cell levels at 19 weeks after challenge. Two macaques from group GGG had ≤10% CD4+ T cells remaining at 19 weeks after challenge.
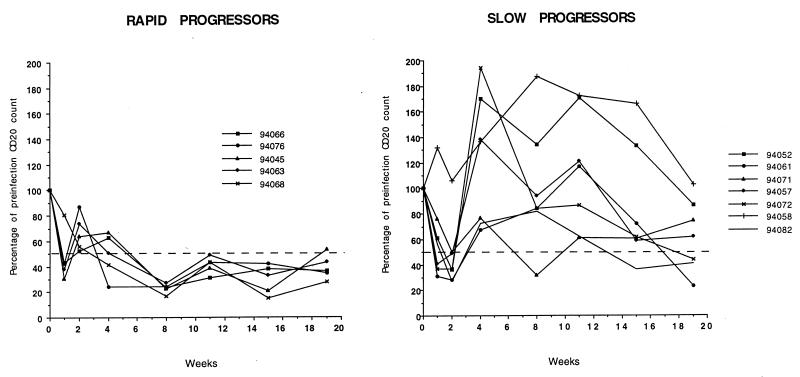
Macaques that maintained >10% of the original circulating CD4+ T-cell levels and were classified as slow progressors also had <50% loss of their circulating B cells (Fig. 2). Macaques that did not maintain at least 10% of their CD4+ cells had more dramatic B-cell losses, sometimes reaching 80% decline compared with preinfection values. A single macaque from each group (r94052, r94072, r94057, and r94058) maintained ∼40% of their starting circulating CD4+ T-cell levels and had increased B-cell numbers early in infection. In contrast, macaques that lost >90% of starting circulating CD4+ T cell levels (r94068, r94063, r94045, r94066, and r94076) also lost >50% of circulating B cells within 4 weeks of virus inoculation. Overall, the consequences of virus infection in immunized animals were similar to those in a previous study of intrarectal SHIV89.6PD challenge in unimmunized macaques (13). All three of the MMM group animals were classified as slow progressors (Fig. 1 and 2). These data suggest a slight positive benefit for i.m. p27 immunization but are not statistically significant with these small groups.
FIG. 2.
CD20+ B-cell depletion in rapid- or slow-progressor macaques after intrarectal SHIV89.6PD inoculation. The pattern of CD20+ B-cell loss is shown for each animal in this challenge study over the interval from infection (week 0) to 19 weeks. Data are expressed as the percentage of preinfection values based on the absolute CD20+ B-cell count in blood. Animals were classified as rapid or slow progressors according to criteria published previously (13).
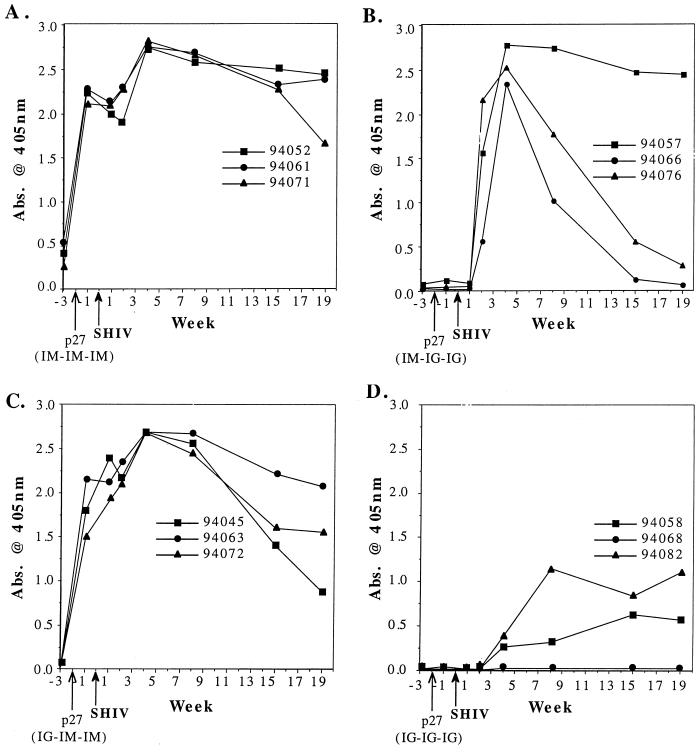
SHIV challenge provided a transient boost for Gag-specific antibody responses in immunized macaques.
Macaques in groups MMM and GMM were immunized i.m. with p27 at 2 weeks prior to SHIV challenge and had high Gag-specific serum antibody responses, with average end point titers of 1:250,000 and 1:130,000 respectively (Table 1). Anamnestic antibody responses were first evident by four weeks after intrarectal SHIV inoculation (Fig. 3). p27-specific end point titers at 4 weeks were approximately 1:650,000 in group MMM and 1:400,000 in group GMM, indicating a substantial boosting of antibody responses after virus infection.
FIG. 3.
Serum antibody responses to virus protein among immunized and virus-challenged macaques. Virus-binding serum antibodies were detected in commercial enzyme-linked immunosorbent assay HIV-2 detection kits as described in the text. Data are represented as the average optical density (Abs. 405 nm) for triplicate replications of each sample. The pattern of serum antibody responses is shown for the period from 3 weeks before (−3 weeks) to 19 weeks after SHIV89.6PD challenge. Values for individual animals are identified by their respective five-digit codes. (A) data for the MMM group of macaques (three i.m. p27 immunizations); (B) results for the MGG group (one i.m. followed by two i.g. immunizations); (C) pattern of responses for group GMM animals (one i.g. followed by two i.m. immunizations); (D) profile of serum antibody responses in group GGG animals (three i.g. immunizations).
Group MGG macaques received a single i.m. p27 injection at 43 weeks before SHIV infection. Antibody responses elicited by the p27 immunization were not boosted by two subsequent doses with i.g. administration of PV4570 (15). Animals in this MGG group had p27-specific serum antibody titers of 1:1,600 before SHIV inoculation (Table 1). Two weeks after virus challenge, three of three macaques in the group MGG had large increases in virus-specific serum antibodies. Group GGG macaques were never immunized i.m. with p27 and had low or undetectable antibody responses until 4 weeks after virus challenge. Antibody levels in these animals were only moderate, with p27-specific end point titers of 1:400 to 1:25,000 by 15 weeks after challenge. In contrast, the Gag-specific antibody recall response of group MGG peaked by 4 weeks after challenge, with an average end point titer of 1:350,000. A single group MGG macaque, r94057, had an end point titer of greater than 1:1,000,000 for the recall antibody response.
The large recall antibody responses stimulated by SHIV challenge (groups MMM, MGG, and GMM) declined over the subsequent 19 weeks of observation. The first sign of declining antibody responses was seen by 8 weeks after challenge in two of three group MGG macaques and by 11 weeks in three of three group GMM macaques. Serum antibody responses to virus remained only in the lower range after virus challenge of group GGG animals (Fig. 3). Recall antibody responses declined most rapidly in MGG animals, and this decline was more pronounced than that observed for GMM animals (Fig. 3). There was no substantial decline in serum antibody levels for MMM animals (Fig. 3). These data argue that the fall in antibody levels for MGG and GMM animal groups was due to virus depletion of Gag-specific helper responses and was not due to lower levels of virus antigen.
Effects of SHIV89.6PD on cellular immune responses.
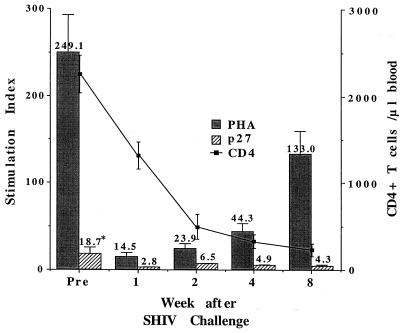
The average SI in response to p27 was 18.0 ± 7.6 for all 12 macaques prior to SHIV challenge (Fig. 4). The average SI was higher for groups MGG and GGG (SI = 28.7), which were immunized with PV4570 at 2 weeks before virus challenge. One week after SHIV inoculation the average SI for all 12 animals had decreased to 2.8 ± 0.7, and these antigen-specific responses remained low. The average p27 SI was only 4.3 ± 2.0 by 8 weeks after challenge. These values are below the cutoff value of 5.0 and are negative for proliferative responses to p27 antigen.
FIG. 4.
Lymphoproliferative responses to SIV p27 and PHA before and after SHIV89.6PD challenge. Data are presented as the average SI (defined in the text) for all animals in this study before (Pre) and after virus challenge until 8 weeks after inoculation. Solid bars denote results for mitogen-induced (PHA) proliferation, and hatched bars show the results for antigen-specific (p27) proliferation. The standard error of the mean for each data set is indicated by appropriate error bars. Average CD4+ T-cell counts (squares) are overlaid on the proliferation data to represent the overall pattern of T-cell loss during the 8 weeks after SHIV89.6PD inoculation. Absolute CD4+ T-cell counts are presented as number of cells per microliter of venous blood.
PBMC from all 12 macaques also showed marked reductions in mitogen-induced proliferation by 1 week after SHIV inoculation. The average SI in response to PHA was 249.1 ± 44.0 before SHIV infection; 1 week after challenge the average SI was down to 14.5 ± 5.4. However, mitogen-induced proliferation increased gradually from weeks 2 to 8 after challenge, despite the continual decrease in absolute numbers of circulating CD4+ T cells. By 8 weeks after challenge the average SI in response to PHA was 133 ± 27.1, while the absolute number of CD4+ T cells per microliter of blood had dropped from 2,245 ± 218.0 (prior to infection) to 229.4 ± 74.9.
DISCUSSION
Macaques were immunized with SIV p27 antigen by i.m. or i.g. routes. The i.m. immunization used a conventional approach with soluble antigen in adjuvant. The i.g. immunization delivered p27 as an intracellular protein produced by recombinant, attenuated S. typhimurium. Previous studies compared these routes and showed that distinct immune responses were elicited by each type of immunization, with i.m. delivery favoring a serum IgG response and i.g. delivery promoting a lymphoproliferative response (15). We did not detect significant cytotoxic lymphocyte responses to Gag antigen in any of the immunized animals (not shown). Animals exhibiting mainly serum IgG or mainly lymphoproliferative responses were exposed to the virulent strain SHIV89.6PD. We observed rapid loss of CD4+ T-cell responses to Gag that occurred within a week after virus challenge and in parallel with loss of mitogen responses. However, mitogen responses recovered to near normal levels while virus-specific immunity remained very low or undetectable.
Pathogenic effects of virus challenge were evaluated by measuring changes in CD4+ and CD20+ blood lymphocyte levels; these markers provided useful prognoses in a previous study of SHIV89.6PD infection (13). Additional measures of immune responses to virus included serum antibody levels along with lymphoproliferative responses to p27 antigen and PHA. Outcomes of virus challenge were similar to what had been observed previously in naive animals inoculated intrarectally with an identical SHIV89.6PD dose (13). Strong serum antibody responses to Gag or strong lymphoproliferative responses to Gag were insufficient to protect against virulent virus challenge by the intrarectal route. Because of the small groups used in this study, we cannot draw conclusions about the effects of immunization on disease progression rates.
A rapid and dramatic effect of virus infection was to reduce proliferative responses to both PHA and viral antigen. Proliferation in response to PHA declined substantially within 1 week and then increased during the interval of 2 to 8 weeks after SHIV inoculation. Eight weeks after virus inoculation, SI values for PHA were 50% of preinfection values and remained above 100 in 60% of the slow-progressor animals (data not shown) when tested at various times during infection (36 to 68 weeks). Changes in the response of human PBMC to mitogen occur during later stages of HIV infection, where declining proliferative responses to recall antigens and alloantigens precede the loss of response to polyclonal mitogenic stimulation (2, 12). Studies examining individuals early after seroconversion noted a transient decrease in proliferation to PHA; responses to mitogen increased during the subsequent asymptomatic period (9). This pattern of acute loss and then regain of mitogen responsiveness is similar to our findings in macaques that were infected acutely with SHIV89.6PD and suggests the transient effect of a viral or host factor that nonspecifically suppresses the proliferative response.
Virus inoculation also affected antigen-specific lymphoproliferative responses. In animals immunized i.g. with recombinant Salmonella and then challenged with SHIV89.6PD, we observed a sharp drop in the lymphoproliferative response to p27 antigen in vitro. In contrast to the mitogen responses, this antigen-specific response did not return over the course of 8 weeks after infection. Longer-term studies showed low, but significant levels of lymphoproliferative responses to p27 antigen by around 35 weeks after virus exposure, but these responses were observed only in animals with very slowly progressing disease (not shown). High-level proliferative responses elicited by i.g. immunization were reduced substantially and rapidly by acute virus infection. These data suggest that antigen-specific helper T cells were destroyed to such an extent that recovery was not possible during the same time interval (8 weeks) that allowed return of mitogen responses. Overall, these data show a transient effect on polyclonal responses and a durable effect on antigen-specific responses. Inappropriate polyclonal activation followed by antigen stimulation might be sufficient for activation-induced cell death mechanisms that would delete clones specific for an abundant viral antigen. In addition, polyclonal or clonal activation may cause these cells to be preferred targets for productive virus infection.
It was interesting also to evaluate the effects of virus infection on p27 serum antibody responses elicited by conventional, i.m. immunization. After primary plus two or three booster immunizations, we observed routinely that p27-binding, serum antibody titers reached or exceeded 300,000. This is a curious situation, because titers of serum antibody to Gag antigen rarely exceed 50,000 in SHIV- or SIV-infected animals, and in rapidly progressing macaques we were unable to measure any serum antibody to virus protein (3, 13). In the case of HIV infection, serum antibody levels reach much higher titers (1, 18), possibly reflecting the relatively slow disease progression in man. Animals with serum antibody responses after immunization showed a boost of these responses following virus infection. Indeed, the boost occurred ∼4 weeks after infection, and this was similar to the earliest appearance of serum antibody responses after infection of unimmunized animals (13). The elevated antibody responses were not maintained after infection, and the rate of decline was inversely related to the number of i.m. immunizations. Despite extensive immunization, antibody levels declined after infection until serum titers of <50,000 were reached. These low levels are consistent with the titers observed after infection in unimmunized macaques.
Acute viral pathogenesis affected both B-cell and helper T-cell responses in immunized macaques. These data are consistent with our previous characterization of SHIV89.6PD infection that documented extensive depletion in both of these cellular compartments, especially among the most rapidly progressing animals (13). The simplest explanation of these data might be that infection deletes preferentially the virus-specific CD4+ T cells. Loss of this crucial population is most extensive in rapidly progressing animals and is a prerequisite for loss of T-cell-dependent B-cell responses. In this way, acute infection reduces the helper T-cell repertoire by decreasing the frequency of clones that react specifically with viral antigen and are needed to support CD8+ T-cell and B-cell effector responses.
A recent publication noted that serum antibody responses to HIV Gag antigens in humans appeared to be T-cell dependent compared to antibody responses to Env antigens, which appeared T-cell independent. These authors concluded that loss of T-cell help during disease progression was responsible for declining serum antibody titers to Gag, and this in turn explained the well-known phenomenon that declining antibodies to Gag often predict AIDS onset (1). Our data show that depletion of helper responses to Gag occurs within a few weeks after SHIV89.6PD inoculation. Loss of specific helper functions are observed directly in the lymphoproliferation assay and may be observed indirectly in the rapid loss of Gag-specific serum immunoglobulin after virus infection.
It is important to note that all three group MMM animals maintained high serum antibody responses after virus infection. These animals also grouped into the slow-progressor classification based on modest loss of CD4+ and CD20+ lymphocytes after virus challenge. It is reasonable to conclude that high levels of T-cell help achieved through multiple immunizations coupled with only a modest delince in CD4+ T-cell count, maintained sufficient immunity to support high levels of virus-binding antibodies in serum. This pattern of antibody recall responses with little or no subsequent decline in these levels is a simple and convenient diagnostic that might help to evaluate other vaccines and their ability to prevent acute destruction of antiviral immunity.
Events during the first weeks after SHIV89.6PD infection alter the host immune response and dictate the eventual rate of disease progression. Loss of antigen-specific helper responses are the earliest and probably most important event in the mechanism for viral pathogenesis.
ACKNOWLEDGMENTS
We acknowledge Yichen Lu and Sharon Jenkins at Avant Immunotherapeutics, Inc., for kindly providing the adjuvant Adjumer used for i.m. p27 injections and the SHIV89.6PD viral stock. We thank Marta Dykhuizen, Paul Hinds, and Jacque Mitchen for technical support with animal evaluations and Kristen Elmer and Kathy Schell for assistance with flow cytometry.
This research was supported by grant RR00167 (Primate Research Center) and PHS grants AI36643 and AI41977 (C.D.P.).
Footnotes
Manuscript 38-023 from the Wisconsin Regional Primate Research Center.
REFERENCES
- 1.Binley J M, Klasse P J, Cao Y, Jones I, Markowitz M, Ho D D, Moore J P. Differential regulation of the antibody responses to Gag and Env proteins of human immunodeficiency virus type 1. J Virol. 1997;71:2799–2809. doi: 10.1128/jvi.71.4.2799-2809.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clerici M, Stocks N I, Zajac R A, Boswell R N, Lucey D R, Via C S, Shearer G M. Detection of three distinct patterns of T helper cell dysfunction in asymptomatic, human immunodeficiency virus-seropositive patients. Independence of CD4+ cell numbers and clinical staging. J Clin Investig. 1989;84:1892–1899. doi: 10.1172/JCI114376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dykhuizen M, Mitchen J, Montefiori D C, Thomsen J, Acker L, Lardy H, Pauza C D. Determinants of disease in the SIV-infected rhesus macaque: characterizing animals with low antibody responses and rapid progression. J Gen Virol. 1998;79:2461–2467. doi: 10.1099/0022-1317-79-10-2461. [DOI] [PubMed] [Google Scholar]
- 4.Lu Y C, Pauza C D, Lu X S, Montefiori D C, Miller C J. Rhesus macaques that become systemically infected with pathogenic SHIV89.6-PD after intravenous, rectal, or vaginal inoculation and fail to make an antiviral antibody response rapidly develop AIDS. J Acquired Immune Defic Syndr Hum Retrovirol. 1998;19:6–18. doi: 10.1097/00042560-199809010-00002. [DOI] [PubMed] [Google Scholar]
- 5.Pauza C D, Emau P, Salvato M S, Trivedi P, MacKenzie D, Malkovsky M, Uno H, Schultz K T. Pathogenesis of SIVmac251 after atraumatic inoculation of the rectal mucosa in rhesus monkeys. J Med Primatol. 1993;22:154–161. [PubMed] [Google Scholar]
- 6.Reimann K A, Li J T, Veazy R, Halloran M, Park I-W, Karlsson G B, Sodroski J, Letvin N L. A chimeric simian/human immunodeficiency virus expressing a primary patient human immunodeficiency virus type 1 isolate env causes an AIDS-like disease after in vivo passage in rhesus monkeys. J Virol. 1996;70:6922–6928. doi: 10.1128/jvi.70.10.6922-6928.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reimann K A, Li J T, Voss G, Lekutis C, Tenner-Racz K, Racz P, Lin W, Montefiori D C, Lee-Parritz D E, Lu Y, Collman R G, Sodroski J, Letvin N L. An env gene derived from a primary human immunodeficiency virus type 1 isolate confers high in vivo replicative capacity to a chimeric simian/human immunodeficiency virus in rhesus monkeys. J Virol. 1996;70:3198–3206. doi: 10.1128/jvi.70.5.3198-3206.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenberg E S, Billingsley J M, Caliendo A M, Boswell S L, Sax P E, Kalams S A, Walker B D. Vigorous HIV-1-specific CD4+ T cell responses associated with control of viremia. Science. 1997;278:1447–1450. doi: 10.1126/science.278.5342.1447. [DOI] [PubMed] [Google Scholar]
- 9.Schellekens P, Roos M, de Wolf F, Lange J, Miedema F. Low T-cell responsiveness to activation via CD3/TCR is a prognostic marker for acquired immunodeficiency syndrome (AIDS) in human immunodeficiency virus-1 (HIV-1)-infected men. J Clin Immunol. 1990;10:121–127. doi: 10.1007/BF00918194. [DOI] [PubMed] [Google Scholar]
- 10.Schenkel A, Uno H, Pauza C D. Asymptomatic simian immunodeficiency virus infection decreases blood CD4+ T cells by accumulating recirculating lymphocytes in the lymphoid tissues. J Virol. 1998;73:601–607. doi: 10.1128/jvi.73.1.601-607.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schrier R D, Wiley C A, Spina C, McCutchan J A, Grant I. Pathogenic and protective correlates of T cell proliferation in AIDS. J Clin Investig. 1996;98:731–740. doi: 10.1172/JCI118845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schulick R D, Clerici M, Dolan M J, Shearer G M. Limiting dilution analysis of interleukin-2-producing T cells responsive to recall and alloantigens in human immunodeficiency virus-infected and uninfected individuals. Eur J Immunol. 1993;23:412–417. doi: 10.1002/eji.1830230217. [DOI] [PubMed] [Google Scholar]
- 13.Steger K K, Dykhuizen M, Mitchen J L, Hinds P W, Preuninger B L, Wallace M, Thomson J, Montefiori D C, Lu Y, Pauza C D. CD4+-T-cell and CD20+-B-cell changes that predict rapid disease progression after simian-human immunodeficiency virus infection in macaques. J Virol. 1998;72:1600–1605. doi: 10.1128/jvi.72.2.1600-1605.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steger K K, Pauza C D. Immunization of Macaca mulatta with aroA-attenuated Salmonella typhimurium expressing SIV p27 antigen. J Med Primatol. 1997;26:44–50. doi: 10.1111/j.1600-0684.1997.tb00318.x. [DOI] [PubMed] [Google Scholar]
- 15.Steger K K, Valentine P, Heffron F, So M, Pauza C D. Recombinant, attenuated Salmonella typhimurium stimulate cell-mediated immune responses to SIV capsid antigen in rhesus macaques. 1998. Vaccine, in press. [DOI] [PubMed] [Google Scholar]
- 16.Trivedi P, Meyer K K, Streblow D N, Preuninger B L, Schultz K T, Pauza C D. Selective amplification of simian immunodeficiency virus genotypes after intrarectal inoculation of rhesus monkeys. J Virol. 1994;62:7649–7653. doi: 10.1128/jvi.68.11.7649-7653.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valentine P J, Meyer K, Rivera M M, Lipps C, Pauza C D, Maziarz R T, So M, Heffron F. Induction of SIV capsid-specific CTL and mucosal slgA in mice immunized with a recombinant S. typhimurium AroA mutant. Vaccine. 1996;14:138–146. doi: 10.1016/0264-410x(95)00130-s. [DOI] [PubMed] [Google Scholar]
- 18.Zwart G, van der Hoek L, Valk M, Cornelissen M T E, Baan E, Dekker J, Koot M, Kuiken C L, Goudsmit J. Antibody responses to HIV-1 envelope and gag epitopes in HIV-1 seroconverters with rapid versus slow disease progression. Virology. 1994;201:285–293. doi: 10.1006/viro.1994.1293. [DOI] [PubMed] [Google Scholar]