Abstract
Introduction
The aneurysms of the anterior inferior cerebellar artery (AICA) are rare lesions of the posterior circulation and to treat them is challenging. We aim to present anatomical and morphological characteristics of AICA aneurysms in a series of 15 patients.
Method
The DSA and CT angiography images of AICA aneurysms in 15 consecutive patients were analyzed retrospectively. Different anatomical characteristics were quantified, including morphology, location, width, neck width, length, bottleneck factor, and aspect ratio.
Results
Eighty percent of the patients were females. The age was 52.4 ± 9.6 (mean ± SD) years. 11 patients were smokers. Ten patients had a saccular aneurysm and five patients had a fusiform aneurysm. Aneurysm in 10 patients were located in the proximal segment, in three patients in the meatal segment, and in two patients in the distal segment. Ten out of 15 patients presented with a ruptured aneurysm. The size of AICA aneurysms was 14.8 ± 18.9 mm (mean ± SD). The aspect ratio was 0.92 ± 0.47 (mean ± SD) and bottleneck factor was 1.66 ± 1.65 (mean ± SD).
Conclusion
AICA aneurysms are rare lesions of posterior circulation predominantly found in females, present predominantly with subarachnoid hemorrhage, and are mostly large in size.
Keywords: AICA aneurysms, characteristics of AICA aneurysms, CT angiography, radiological features, clinical outcome
1. Introduction
The aneurysm of the anterior inferior cerebellar artery (AICA) are very rare and they account for <1% of all intracranial aneurysms (1, 2). The reported case reports of AICA aneurysms have a single or a few patients (1, 3–62), except for a few larger case series (63), including a large series of AICA aneurysms reported by Drake and colleagues (64). However, in this series, the aneurysms originating from the basilar trunk that is near the origin of AICA were included. AICA aneurysms are more often large in size, which makes their surgical and endovascular treatments challenging. Coiling is the favored treatment of posterior circulation aneurysms (65). However, in selected cases surgery might be a better choice, particularly in larger sized AICA aneurysms (26, 57). The surgical approach depends on location of aneurysm in relation to clivus. Aneurysms laying high can be approached through sub-temporal approach and low laying aneurysms are approached through retro-sigmoidal corridor. The morphological features may be helpful in deciding upon a treatment strategy. Due to the rarity of these lesions, the anatomical and radiological characteristics in unselected patient cohorts with AICA aneurysms have seldom been reported. In this series, we report the radiological features including shape, size, aspect ratio (maximum perpendicular height divided by neck diameter), bottleneck factor (maximum height to width ratio), and frequencies of aneurysm location in different segments of AICA aneurysms in a medium-size series. We report 15 consecutive patients harboring AICA aneurysms admitted from 1968 to 2017 in Helsinki University Hospital, department of Neurosurgery.
2. Methods
2.1. Patients and radiological data
Through retrospective analysis of our aneurysm data base, a total of 21 patients harbouring AICA aneurysms were identified. Six patients were excluded because of missing CT angiography scans or DSA. The remaining 15 patients harboring AICA aneurysms were included in the study. A 4-slice scanner (GE Lightspeed QX/I; GE Medical Systems, Milwaukee, Wisconsin, USA) was used for analyzing CT angiography images until 2007. Since then, a 32-slice scanner (GE LightSpeed Pro 32) or a 64-row scanner (GE lightSpeed VCT Advantage) was used to analyze CT angiography images. The digital archiving system of the hospital (IMPAX, version 5.3, Agfa, Mortsel, Belgium) was used to store the images. Two board-certified neurosurgeons analyzed the CTA scans.
The study was approved by the local ethical committee. The ethical number for the aneurysm database is HUS/197/2016. For retrospective data collection, an additional approval/consent was not required.
2.2. Radiological measurements
For each aneurysm, the maximal length, width, neck diameter, shape (saccular/fusiform), and the location at different segments of AICA were quantified. The above measurements were used to calculate aspect ratio and bottleneck factor.
2.3. Statistical analysis
The commercial statistical software IBM SPSS (version 20.0.0.) was used to analyze the data. The data is presented as mean ± SD or in frequencies (percentage).
3. Results
3.1. Patients and aneurysms
In our series (from 1968 to 2017), a total of 9,832 patients harboring intracranial aneurysms were studied. 21 patients out of 9,832 had AICA aneurysms showing an incidence of AICA aneurysms occurrence in about 0.22% of all intracranial aneurysms. Due to missing proper scans, we could analyze AICA aneurysms in 15 patients. Out of the 15 patients with AICA aneurysms, 12 (80%) were female and 3 (20%) were males. The mean age of the patients was 52.4 ± 9.6 years. In this case series, 11 (73%) of the patients were smokers. Also, 11 (73%) of the patients had a ruptured aneurysm (Table 1).
Table 1.
Radiological characteristics of anterior inferior cerebellar artery aneurysms.
| Total number | Percentage | |
|---|---|---|
| Number of patients | 15 | |
| Age, years (mean ± SD) | 52.4 ± 9.6 | |
| Males | 3 | 20 |
| Females | 12 | 80 |
| Current smoker | 11 | 73.3 |
| Non-smoker | 4 | 26.7 |
| Presentation with SAH | 11 | 73.3 |
| Non-SAH | 4 | 26.7 |
| Cranial nerve deficits | ||
| Yes | 5 | 33.3 |
| No | 10 | 66.7 |
| Shape | ||
| Saccular | 10 | 66.7 |
| Fusiform | 5 | 33.3 |
| Side | ||
| Left | 7 | 46.7 |
| Right | 8 | 53.3 |
| Location | ||
| Proximal | 10 | 66.6 |
| Meatal | 3 | 20 |
| Distal | 2 | 13.3 |
3.2. Radiological characters of AICA aneurysms
Ten (67%) patients had a saccular aneurysm and five (33%) patients had a fusiform aneurysm. Ten (67%) aneurysms were located in the pre-meatal segment, three (20%) aneurysms were located in the meatal segment, and the two (13%) aneurysms were located in the post-meatal segment. The AICA aneurysms had a mean size of 14.8 ± 18.9 mm. The ACIA aneurysm had a mean aspect ratio of 0.92 ± 0.47 and they had a mean bottleneck factor of 1.66 ± 1.65 (Table 2). Interestingly, in the proximal segment 30% and in the distal segments 40% of the aneurysms were fusiform (Tables 1, 2).
Table 2.
Radiological characteristics of anterior inferior cerebellar artery aneurysms (n = 15).
| Radiological characteristics | Mean ± SD |
|---|---|
| Aneurysm size (mm), (n = 15) | 14.8 ± 18.9 |
| Width (mm) | 14.8 ± 18.9 |
| Length (mm) | 16.9 ± 20.3 |
| Neck (mm) | 12.6 ± 13.1 |
| Aspect ratio of saccular aneurysms (n = 10) | 0.92 ± 0.47 |
| Bottleneck factor of saccular aneurysms (n = 10) | 1.66 ± 1.65 |
3.3. Clinical presentation and outcomes
Out of 15 patients, 11 (63.3%) presented with subarachnoid hemorrhage, and 4 (26.7%) patients with incidental findings. Among the ruptured cases 9 out of 11 (81.8%) presented with a good grade SAH (Hunt and Hess grade 1–3) and the remaining 2 out of 11 patients presented with a poor grade SAH (Hunt and Hess 4–5). In radiological analysis 3 out of 15 patients presented with intracerebral hematoma and 6 out of 15 patients presented with intraventricular hemorrhage as reported by Muhammad et al. in 2023. 11 out of 15 patients were treated surgically, only one patient was treated with endovascular coiling and 3 patients remain conservative. One of the conservatively treated patient lived more than 40 years and finally died in 2012 due to other systemic diseases and not due to SAH. In other two cases, patients were admitted with poor grade SAH and did not survive from severe SAH. All the unruptured aneurysms had good clinical outcomes (mRS 1–2) on discharge. In patients with ruptured AICA aneurysms, 9 out of 11 patients (81.8%) had good clinical outcomes (mRS 1–2) and 2 out of 11 patients (18.2%) had poor clinical (mRS 3–6) outcomes (66).
4. Discussion
AICA aneurysms are rare and have been reported in <1% of all intracranial aneurysms (1, 2). Our data show that the incidence of AICA aneurysms in an unselected cohort was 0.22%. The most common presentation of an AICA aneurysm is subarachnoid hemorrhage (SAH). Seventy three percent of patients in our series presented with SAH, which is similar to previously published data (63). A review of data from already published case reports of 56 patients revealed that 81% of patients presented with SAH, which is slightly greater than our series and the series presented previously. Patients with more insidious onset present with cranial nerve deficits very similar to cerebellopontine angle space occupying lesions. However, patients with SAH may also have cranial nerve deficits often in the seventh and eighth cranial nerves. In our series, 33% (N = 5) of the patients had cranial nerve (VI, VII, VIII, or IX) deficits (Table 1). Rarely, patients with an AICA aneurysm present with convulsive seizure (36). In our series, none of the patients presented with epilepsy. AICA can be anatomically divided into four segments including (67) anterior pontine (a1), lateral pontine (a2), flocculopeduncular (a3), and cortical (a4). The lateral pontine segment has a close relationship with the porus of the internal acoustic meatus and with the facial and cochleovestibular nerves. AICA aneurysms can be categorized into proximal, meatal, and distal (58). Our data shows that 67% (n = 10) of the aneurysms were located proximally, 20% (n = 3) were in the meatal region, and only 13% (n = 2) were located distally. Our data are consistent with a previously published short case series where five out of six aneurysms were located proximally (1). Meatal aneurysms can be further classified into three subtypes (58). Type I (also called remote) are localized in the vascular loop outside the meatus. Type II (plugged) aneurysms are partially buried in the internal-acoustic meatus, and type III (buried) are entirely contained by the internal auditory canal). In our series, we found three aneurysms that were located in the meatal segment. Two of these were type I and one was type II (not shown in the table). The location of the aneurysm facilitates the planning of a suitable surgical approach if surgery is indicated (Figures 1–3). Most of the AICA aneurysms are reached through retrosigmoid approach (Figures 1–3). The mean ± SD size of the AICA aneurysms was 14.8 ± 18.9. The mean ± SD width was 16.9 ± 20.3 mm and the mean ± SD length was 16.9 ± 20.3 (Table 2). It is noteworthy that 73% of the patients were smokers and smoking is a potential risk factor for aneurysm formation and rupture. Further analysis of saccular aneurysms (n = 10) revealed a mean ± SD aspect ratio of 0.92 ± 0.47 and a mean ± SD bottleneck factor of 1.66 ± 1.65 (Table 2). Our data demonstrate that most AICA aneurysms are larger in size, which is consistent with a previous report that analyzed 10 thrombosed AICA aneurysms (20). In most cases in this series, the aneurysm size was >10 mm; two of these aneurysms were giant.
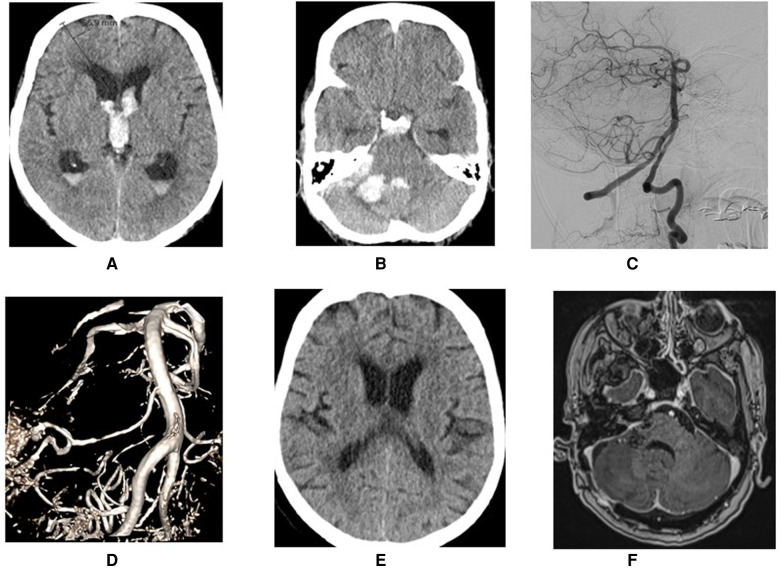
Figure 1.
Demonstration of a ruptured AICA aneurysms at proximal location (A,B) that was treated surgically through retrosigmoid approach (C). Another patients with ruptured high laying AICA aneurysm (D,E) that was treated through sub-temporal approach (F).
Figure 3.
Demonstration of a ruptured AICA aneurysms at meatal loop with intra cerebral hemorrhage (A–C) that was treated through retrosigmoid approach (D–F).
Figure 2.
Demonstration of a ruptured AICA aneurysms with intra cerebral hemorrhage (A–C) that was treated through retrosigmoid approach (D–F).
5. Conclusion
AICA aneurysms are rare posterior circulation lesions predominantly found in females, present predominantly with subarachnoid hemorrhage, are mostly large in size.
6. Limitations
Our analysis was retrospective and may not completely reflect the natural history of anatomical and radiological parameters. The aspect ratio was quantified in a few cases after rupture and hence the possibility remains that the aspect ratio might have changed due to morphological changes after rupture and to a compression effect due to subarachnoid blood. Due to the small number of patients, we could not analyze the influence of aspect ratio, bottleneck factor, and segmental location of the aneurysm on aneurysm rupture.
Funding Statement
SM was supported by Ehrnrooth foundation for clinical vascular and skull base fellowship.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the local ethical committee that approved the study of intracranial aneurysms. The ethical number for the aneurysm database is HUS/197/2016. An additional approval/consent for retrospective data collection was not required. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
SM and MN contributed to the conception and design of the study. SM performed the statistical analysis. SM wrote the first draft of the manuscript. AH, HK, BJ, and RK, DH, MN wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) SM and BJ declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Li X, Zhang D, Zhao J. Anterior inferior cerebellar artery aneurysms: six cases and a review of the literature. Neurosurg Rev. (2012) 35(1):111–9; discussion 9. 10.1007/s10143-011-0338-1 [DOI] [PubMed] [Google Scholar]
- 2.Sanai N, Tarapore P, Lee AC, Lawton MT. The current role of microsurgery for posterior circulation aneurysms: a selective approach in the endovascular era. Neurosurgery. (2008) 62(6):1236–49. ; discussion 49–53. [DOI] [PubMed] [Google Scholar]
- 3.Adorno JO, de Andrade GC. Aneurysm of the anterior inferior cerebellar artery: case report. Arq Neuropsiquiatr. (2002) 60(4):1019–24. 10.1590/S0004-282X2002000600026 [DOI] [PubMed] [Google Scholar]
- 4.Aguiar GB, Veiga JC, Jory M, Souza RB, Mattar Neto B, Conti ML. Fusiforme aneurysm of the anterior inferior cerebellar artery and arteriovenous malformation fed by the same vessel. Medicina (B Aires). (2012) 72(3):245. [PubMed] [Google Scholar]
- 5.Akyuz M, Tuncer R. Multiple anterior inferior cerebellar artery aneurysms associated with an arteriovenous malformation: case report. Surg Neurol. (2005) 64(Suppl 2):S106–8. 10.1016/j.surneu.2005.07.037 [DOI] [PubMed] [Google Scholar]
- 6.Andrade G, Faquini I, Azevedo-Filho H, Laercio J, Camara D, Mendes JC, et al. Dissecting anterior inferior cerebellar artery aneurysm treated by endovascular route: report of three cases and review. Arq Neuropsiquiatr. (2010) 68(4):645–7. 10.1590/S0004-282X2010000400031 [DOI] [PubMed] [Google Scholar]
- 7.Baskaya MK, Coscarella E, Jea A, Morcos JJ. Aneurysm of the anterior inferior cerebellar artery-posterior inferior cerebellar artery variant: case report with anatomical description in the cadaver. Neurosurgery. (2006) 58(2):E388.; discussion E. 10.1227/01.NEU.0000199344.63306.DD [DOI] [PubMed] [Google Scholar]
- 8.Cantore GP, Ciappetta P, Vagnozzi R, Bozzao L. Giant aneurysm of the anterior inferior cerebellar artery simulating a cerebellopontine angle tumor. Surg Neurol. (1982) 18(1):76–8. 10.1016/0090-3019(82)90025-8 [DOI] [PubMed] [Google Scholar]
- 9.DiMaio S, Mohr G, Dufour JJ, Albrecht S. Distal mycotic aneurysm of the AICA mimicking intracanalicular acoustic neuroma. Can J Neurol Sci. (2003) 30(4):388–92. 10.1017/S0317167100003139 [DOI] [PubMed] [Google Scholar]
- 10.Ebara M, Tanaka T, Sawauchi S, Morooka S, Yuhki K, Abe T. A ruptured aneurysm of the anterior and posterior inferior cerebellar artery: a case report. No Shinkei Geka. (1999) 27(11):1013–7. [PubMed] [Google Scholar]
- 11.Fukuya T, Kishikawa T, Ikeda J, Kudo S, Kuwano H, Matsumoto S, et al. Aneurysms of the peripheral portion of the anterior inferior cerebellar artery; report of two cases. Neuroradiology. (1987) 29(5):493–6. 10.1007/BF00341751 [DOI] [PubMed] [Google Scholar]
- 12.Gleeson MJ, Cox TC, Strong AJ. Aneurysm of the anterior inferior cerebellar artery mimicking an intracanalicular acoustic neuroma. J Laryngol Otol. (1989) 103(1):107–10. 10.1017/S0022215100108163 [DOI] [PubMed] [Google Scholar]
- 13.Gopalakrishnan CV, Menon G, Nair S. Aneurysm of the anterior inferior cerebellar artery-posterior inferior cerebellar artery variant: two case reports and review of literature. Br J Neurosurg. (2009) 23(5):554–6. 10.1080/02688690902987778 [DOI] [PubMed] [Google Scholar]
- 14.Goto S, Ohshima T, Yamamoto T, Nishihori M, Nishizawa T, Shimato S, et al. A case of ruptured intrameatal aneurysm successfully treated with coil embolization. Nagoya J Med Sci. (2015) 77(1–2):307–13. [PMC free article] [PubMed] [Google Scholar]
- 15.Honda Y, Tanaka R, Kameyama S. Ruptured distal anterior inferior cerebellar artery aneurysm–case report. Neurol Med Chir (Tokyo). (1994) 34(11):763–7. 10.2176/nmc.34.763 [DOI] [PubMed] [Google Scholar]
- 16.Ishii D, Takechi A, Shinagawa K, Sogabe T. Endovascular treatment for ruptured distal anterior inferior cerebellar artery aneurysm -case report. Neurol Med Chir (Tokyo). (2010) 50(5):396–9. 10.2176/nmc.50.396 [DOI] [PubMed] [Google Scholar]
- 17.Ito J, Takeda N, Suzuki Y, Takeuchi S, Osugi S, Yoshida Y. The anterior inferior cerebellar arteries originating from the internal carotid artery (author’s transl). No to Shinkei. (1979) 31(10):999–104. [PubMed] [Google Scholar]
- 18.Jinbo Y, Zheng Z, Jiaquan H, Hui Y, Jun L. Embolization of a ruptured aneurysm of the distal anterior inferior cerebellar artery with parent artery preservation. Neurol India. (2010) 58(5):786–8. 10.4103/0028-3886.72170 [DOI] [PubMed] [Google Scholar]
- 19.Johnson JH, Jr, Kline DG. Anterior inferior cerebellar artery aneurysms. Case report. J Neurosurg. (1978) 48(3):455–60. 10.3171/jns.1978.48.3.0455 [DOI] [PubMed] [Google Scholar]
- 20.Kanamori F, Kawabata T, Muraoka S, Kojima T, Watanabe T, Hatano N, et al. Ruptured partially thrombosed anterior inferior cerebellar artery aneurysms: two case reports and review of literature. Nagoya J Med Sci. (2016) 78(4):517–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang HS, Roh HG, Han MH, Koh YC. Successful endovascular occlusion of a ruptured distal anterior inferior cerebellar artery aneurysm of the caudal trunk: case report. Interv Neuroradiol. (2007) 13(3):271–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kiya K, Uozumi T, Emoto K, Matsuoka T. Anterior inferior cerebellar artery aneurysm at the internal auditory meatus—case report. Neurol Med Chir (Tokyo). (1989) 29(7):592–5. 10.2176/nmc.29.592 [DOI] [PubMed] [Google Scholar]
- 23.Kiya K, Uozumi T, Emoto K, Matsuoka T. Aneurysm of the anterior inferior cerebellar artery at the internal auditory meatus: case report and review of the literature. Hiroshima J Med Sci. (1989) 38(1):39–44. [PubMed] [Google Scholar]
- 24.Koizumi H, Kurata A, Suzuki S, Miyasaka Y, Tanaka C, Fujii K. Endosaccular embolization for a ruptured distal anterior inferior cerebellar artery aneurysm. Radiol Case Rep. (2012) 7(2):651. 10.2484/rcr.v7i2.651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kyoshima K, Matsuda M, Handa J. Cerebral aneurysm of the distal anterior inferior cerebellar artery: case report. Nihon Geka Hokan. (1995) 64(6):139–45. [PubMed] [Google Scholar]
- 26.Lee BS, Witek AM, Moore NZ, Bain MD. Treatment of an anterior inferior cerebellar artery aneurysm with microsurgical trapping and in situ posterior inferior cerebellar artery to anterior inferior cerebellar artery bypass: case report. Oper Neurosurg (Hagerstown). (2018) 15(4):418–24. 10.1093/ons/opx275 [DOI] [PubMed] [Google Scholar]
- 27.Lee SJ, Koh JS, Ryu CW, Lee SH. Ruptured intrameatal aneurysm of the anterior inferior cerebellar artery accompanying an arteriovenous malformation: a case report. Cerebellum. (2012) 11(3):808–12. 10.1007/s12311-011-0349-z [DOI] [PubMed] [Google Scholar]
- 28.Lv X, Li Y, Liu A, Zhang J, Wu Z. Parent artery occlusion for peripheral anterior inferior cerebellar artery aneurysm. A case report and review of the literature. Neuroradiol J. (2008) 21(2):261–5. 10.1177/197140090802100219 [DOI] [PubMed] [Google Scholar]
- 29.Mahmoud M, El Serwi A, Alaa Habib M, Abou Gamrah S. Endovascular treatment of AICA flow dependent aneurysms. A report of three cases and review of the literature. Interv Neuroradiol. (2012) 18(4):449–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marchini AK, Mosimann PJ, Guichard JP, Boukobza M, Houdart E. Anterior inferior cerebellar artery aneurysms mimicking vestibular schwannomas. J Neuroimaging. (2014) 24(4):404–6. 10.1111/j.1552-6569.2012.00752.x [DOI] [PubMed] [Google Scholar]
- 31.Martin RG, Grant JL, Peace D, Theiss C, Rhoton AL, Jr. Microsurgical relationships of the anterior inferior cerebellar artery and the facial-vestibulocochlear nerve complex. Neurosurgery. (1980) 6(5):483–507. 10.1227/00006123-198005000-00001 [DOI] [PubMed] [Google Scholar]
- 32.Mascitelli JR, McNeill IT, Mocco J, Berenstein A, DeMattia J, Fifi JT. Ruptured distal AICA pseudoaneurysm presenting years after vestibular schwannoma resection and radiation. J Neurointerv Surg. (2016) 8(5):e19. 10.1136/neurintsurg-2015-011736.rep [DOI] [PubMed] [Google Scholar]
- 33.Matsushige T, Ikawa F, Ohbyashi N, Imada Y, Kajiwara Y, Inagawa T. Ruptured aneurysm arising from the anterior medullary segment of the posterior inferior cerebellar artery: report of two cases. No Shinkei Geka. (2004) 32(8):867–74. [PubMed] [Google Scholar]
- 34.Matsuyama T, Okuchi K, Norimoto K, Ueyama T. Ruptured dissecting anterior inferior cerebellar artery aneurysm–case report. Neurol Med Chir (Tokyo). (2002) 42(5):214–6. 10.2176/nmc.42.214 [DOI] [PubMed] [Google Scholar]
- 35.Menovsky T, Andre Grotenhuis J, Bartels RH. Aneurysm of the anterior inferior cerebellar artery (AICA) associated with high-flow lesion: report of two cases and review of literature. J Clin Neurosci. (2002) 9(2):207–11. [DOI] [PubMed] [Google Scholar]
- 36.Mizushima H, Kobayashi N, Yoshiharu S, Kazuo H, Dohi K, Sasaki K, et al. Aneurysm of the distal anterior inferior cerebellar artery at the medial branch: a case report and review of the literature. Surg Neurol. (1999) 52(2):137–42. 10.1016/S0090-3019(99)00042-7 [DOI] [PubMed] [Google Scholar]
- 37.Mori K, Miyazaki H, Ono H. Aneurysm of the anterior inferior cerebellar artery at the internal auditory meatus. Surg Neurol. (1978) 10(5):297–300. [PubMed] [Google Scholar]
- 38.Nakagawa K, Sakaki S, Kimura H, Matsuoka K. Aneurysm of the anterior inferior cerebellar artery at the internal auditory meatus. Surg Neurol. (1984) 21(3):231–5. 10.1016/0090-3019(84)90192-7 [DOI] [PubMed] [Google Scholar]
- 39.Nishimoto A, Fujimoto S, Tsuchimoto S, Matsumoto Y, Tabuchi K, Higashi T. Anterior inferior cerebellar artery aneurysm. Report of three cases. J Neurosurg. (1983) 59(4):697–702. 10.3171/jns.1983.59.4.0697 [DOI] [PubMed] [Google Scholar]
- 40.Oh JS, Yoon SM. Endovascular treatment for ruptured distal anterior inferior cerebellar artery aneurysm. (2014) 16(1):20–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okumura Y, Sakaki T, Hirabayashi H, Shimomura T. Intrameatal aneurysm successfully treated by meatal loop trapping–case report. Neurol Med Chir (Tokyo). (1999) 39(2):161–4. 10.2176/nmc.39.161 [DOI] [PubMed] [Google Scholar]
- 42.Pasler D, Baldauf J, Runge U, Schroeder HW. Intrameatal thrombosed anterior inferior cerebellar artery aneurysm mimicking a vestibular schwannoma. J Neurosurg. (2011) 114(4):1057–60. 10.3171/2010.9.JNS10491 [DOI] [PubMed] [Google Scholar]
- 43.Pritz MB. Aneurysms of the anterior inferior cerebellar artery. Acta Neurochir. (1993) 120(1–2):12–9. 10.1007/BF02001463 [DOI] [PubMed] [Google Scholar]
- 44.Russegger L, Furtschegger A. Aneurysms of the anterior inferior cerebellar artery. A case report and review of the literature. Nervenarzt. (1990) 61(8):499–503. [PubMed] [Google Scholar]
- 45.Saito R, Tominaga T, Ezura M, Shimizu H, Yoshimoto T. Distal anterior inferior cerebellar artery aneurysms: report of three cases and literature review. No Shinkei Geka. (2001) 29(8):709–14. [PubMed] [Google Scholar]
- 46.Santillan A, Gobin YP, Patsalides A, Riina HA, Rosengart A, Stieg PE. Endovascular management of distal anterior inferior cerebellar artery aneurysms: report of two cases and review of the literature. Surg Neurol Int. (2011) 2:95. 10.4103/2152-7806.82577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Santucci N, Gazzeri G, Magliocco C. Aneurysm of the anterior inferior cerebellar artery (AICA). 18th case in the literature. Riv Neurol. (1985) 55(1):30–7. [PubMed] [Google Scholar]
- 48.Sarkar A, Link MJ. Distal anterior inferior cerebellar artery aneurysm masquerading as a cerebellopontine angle tumor: case report and review of literature. Skull Base. (2004) 14(2):101–6. ; discussion 6–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sasame J, Nomura M. Dissecting aneurysm of anterior inferior cerebellar artery initially presenting with nonhemorrhagic symptom. J Stroke Cerebrovasc Dis. (2015) 24(8):e197–9. 10.1016/j.jstrokecerebrovasdis.2015.03.055 [DOI] [PubMed] [Google Scholar]
- 50.Singh S, Mittal RS, Purohit D, Shekhawat J. Spontaneous resolution of ruptured dissecting anterior inferior cerebellar artery aneurysm: a rare case report. Asian J Neurosurg. (2017) 12(3):570–2. 10.4103/1793-5482.145561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Spallone A, De Santis S, Giuffre R. Peripheral aneurysms of the anterior inferior cerebellar artery. Case report and review of literature. Br J Neurosurg. (1995) 9(4):537–41. 10.1080/02688699550041197 [DOI] [PubMed] [Google Scholar]
- 52.Suh SH, Kim DJ, Kim DI, Kim BM, Chung TS, Hong CK, et al. Management of anterior inferior cerebellar artery aneurysms: endovascular treatment and clinical outcome. AJNR Am J Neuroradiol. (2011) 32(1):159–64. 10.3174/ajnr.A2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sun Y, Wrede KH, Chen Z, Bao Y, Ling F. Ruptured intrameatal AICA aneurysms—a report of two cases and review of the literature. Acta Neurochir. (2009) 151(11):1525–30. 10.1007/s00701-009-0269-6 [DOI] [PubMed] [Google Scholar]
- 54.Suzuki K, Meguro K, Wada M, Fujita K, Nose T. Embolization of a ruptured aneurysm of the distal anterior inferior cerebellar artery: case report and review of the literature. Surg Neurol. (1999) 51(5):509–12. 10.1016/S0090-3019(97)00462-X [DOI] [PubMed] [Google Scholar]
- 55.Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y, et al. Trapping of ruptured dissecting aneurysm of distal anterior inferior cerebellar artery—case report. Brain Nerve. (2009) 61(2):203–7. [PubMed] [Google Scholar]
- 56.Tamura Y, Shirai W, Tokumitsu N. Intrameatal aneurysm of distal anterior inferior cerebellar artery manifesting a subarachnoid hemorrhage: a report of 2 cases. No Shinkei Geka. (2018) 46(8):673–81. [DOI] [PubMed] [Google Scholar]
- 57.Taussky P, Garber S, Schmidt RH. Surgical management of a ruptured and unruptured distal anterior inferior cerebellar artery aneurysm. Report of 2 cases and review of the literature. Cent Eur Neurosurg. (2011) 72(2):108–11. 10.1055/s-0030-1268498 [DOI] [PubMed] [Google Scholar]
- 58.Yamakawa H, Hattori T, Tanigawara T, Sahashi Y, Ohkuma A. Intracanalicular aneurysm at the meatal loop of the distal anterior inferior cerebellar artery: a case report and review of the literature. Surg Neurol. (2004) 61(1):82–8; discussion 8. 10.1016/S0090-3019(03)00270-2 [DOI] [PubMed] [Google Scholar]
- 59.Yokoyama S, Kadota K, Asakura T, Kawazoe K. Aneurysm of the distal anterior inferior cerebellar artery—case report. Neurol Med Chir (Tokyo). (1995) 35(8):587–90. 10.2176/nmc.35.587 [DOI] [PubMed] [Google Scholar]
- 60.Zager EL. Isolated trigeminal sensory loss secondary to a distal anterior inferior cerebellar artery aneurysm: case report. Neurosurgery. (1991) 28(2):288–91. 10.1227/00006123-199102000-00018 [DOI] [PubMed] [Google Scholar]
- 61.Zlotnik EI, Sklyut JA, Smejanovich AF, Stasenko EN. Saccular aneurysm of the anterior inferior cerebellar-internal auditory artery. Case report. J Neurosurg. (1982) 57(6):829–32. 10.3171/jns.1982.57.6.0829 [DOI] [PubMed] [Google Scholar]
- 62.Zotta DC, Stati G, De Paulis D, Galzio RJ. Intrameatal aneurysm of the anterior inferior cerebellar artery. J Clin Neurosci. (2011) 18(4):561–3. [DOI] [PubMed] [Google Scholar]
- 63.Gonzalez LF, Alexander MJ, McDougall CG, Spetzler RF. Anteroinferior cerebellar artery aneurysms: surgical approaches and outcomes—a review of 34 cases. Neurosurgery. (2004) 55(5):1025–35. 10.1227/01.NEU.0000141083.00866.82 [DOI] [PubMed] [Google Scholar]
- 64.Bojanowski MW BI, Robert T. Anterior inferior cerebellar artery aneurysms. In: Rangel-Castilla LNP, Siddiqui AH, Spetzler RF, Levy EI, editors. Decision making in neurovascular disease. Thieme; (2018). [Google Scholar]
- 65.Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Russin JJ, et al. The barrow ruptured aneurysm trial: 6-year results. J Neurosurg. (2015) 123(3):609–17. 10.3171/2014.9.JNS141749 [DOI] [PubMed] [Google Scholar]
- 66.Muhammad S, Hafez A, Kaukovalta H, Jahromi BR, Kivisaari R, Hanggi D, et al. Treatment and outcome of anterior inferior cerebellar artery (AICA) aneurysms: helsinki series of 15 consecutive patients. Asian J Neurosurg. (2023) 18(1):30–5. 10.1055/s-0042-1758844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rodriguez-Hernandez A, Rhoton AL, Jr, Lawton MT. Segmental anatomy of cerebellar arteries: a proposed nomenclature. Laboratory investigation. J Neurosurg. (2011) 115(2):387–97. 10.3171/2011.3.JNS101413 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.