Summary
Background
Lack of timely care is a predictor of poor outcomes in acute cardiovascular emergencies including stroke. We assessed the presence of delay in seeking appropriate care among those who died due to cardiac/stroke emergencies in a community in northern India and identified the reasons and determinants of this delay.
Methods
We conducted a social audit among all civil-registered premature (30–69 years) deaths due to acute cardiac event or stroke in the district. The three-delays model was used to qualitatively classify the delays in care-seeking—deciding to seek care, reaching the appropriate health facility (AHF) and initiating definitive treatment. Based on the estimated time from symptom onset to reaching AHF, we classified patients as early (reached within one hour) or delayed arrivers. We used mixed-effect logistic regression with postal code as a random effect to identify determinants of delayed arrival.
Findings
Only 10.8% of the deceased reached an AHF within one hour. We noted level-1 delay in 38.4% (60% due to non-recognition of seriousness); level-2 delay in 20% (40% due to going to an inappropriate facility) and level-3 delay in 10.8% (57% due to lack of affordability). Patients with a monthly family income of >270US$ (aOR 0.44; 95% CI 0.21–0.93) were less and those staying farther from AHF (aOR 1.12; 95% CI 1.01–1.25 for each Km) were more likely to have delayed arrival in AHF.
Interpretation
A small proportion of patients with cardiac and stroke emergencies reach health facility early with delays at multiple levels. Addressing the reasons for delay could prevent these deaths.
Funding
: Indian Council of Medical Research, New Delhi, India.
Keywords: CVDs, Delay, Health services, Mortality, Stroke
Research in context.
Evidence before this study
Hospital-based studies in India have reported prehospital delay of more than 6 h among 36%–42% of admitted acute myocardial infarction due to misdiagnosis of symptoms, inadequate prehospital healthcare infrastructure, high cost of care, lack of health insurance coverage, and making multiple stops to the facility.
Added value of this study
This first community-based study from India provides insights on delays in access to acute cardiac and stroke care at various levels and their determinants and reasons among those who died of an acute cardiac condition or stroke, the two most important killers of adults in India. The study enhances the understanding on complex web of health seeking behavior and the mobility of patients between local practitioner, transfers and referrals to reaching an appropriate healthcare facility.
Implications of all the available evidence
The study clearly identified affordability and accessibility as important factors for delays resulting in mortality and identified better insurance coverage and appropriate equipped ambulance linkages along with programs to improve recognition of a heart or brain attack among the populace.
Introduction
Globally 17.9 million people are estimated to die due to cardiovascular diseases (CVD) each year1 with two-fifths of them being premature deaths in the age group of 30–69 years.2 Ischemic heart diseases (IHD) and stroke constituted 85% of all CVD deaths in 2019.3 In India, CVD accounts for 36% of all deaths occurring in the age group of 30–69 years.4 Preventing these deaths should be a public health priority globally as well as in India.
Lack of timely care is one of the important predictors of poorer outcomes in cardiovascular emergencies. Delayed presentation leads to delay or failure to provide the most beneficial therapies like thrombolysis for myocardial infarction/ischemic stroke leading to poorer disease outcomes. It is estimated that interventions that reduce delays in care in patients with myocardial infarction (MI) could decrease risk of mortality by 30%.5 A study reported that every 30 min delay in MI patients increased 1-year mortality by 7.5%.6 It is well established that the sooner a thrombolytic therapy is given to stroke patients, the greater the benefit, especially if started within 90 min.7 A reduction in delay in receiving appropriate acute care should be the cornerstone of planning acute cardiac and stroke services in all countries.
Hospital-based studies from India have shown that between 36% and 42% of admitted acute myocardial infarction (MI) patients have a prehospital delay of more than 6 h.8, 9, 10 Only one-third of ST-segment elevation myocardial infarction (STEMI) patients had a door-to-needle time of less than 30 min within the hospital.11 Service providers have reported that delays in receiving appropriate cardiac care were due to misperception of symptoms, insufficient prehospital healthcare, high cost of treatment and lack of coverage with health insurance and making multiple visits before coming to the facility.12 In a tertiary hospital-based study, the mean prehospital time for clinically suspected stroke was 716 min and the mean total in-hospital delay was 94 min. Lack of awareness of stroke symptoms led to the delayed seeking of treatment and in-hospital delays were due to patient admission procedures, lack of staff to transport the patient, and the distance between the stroke unit and radiodiagnosis facility.13
These hospital-based studies, reflect the situation of only the patients who reach the hospital. There is a lack of community-based studies from India to provide information on the amount and nature of delays in CVD/stroke patients who do not reach the hospital. This study was done to estimate the delays among persons aged 30–69 years who died prematurely due to acute CVD events including stroke in district Faridabad and identify the reasons and determinants of this delay. The study received ethical clearance from the Institutional Ethics Committee of the All India Institute of Medical Sciences (AIIMS), New Delhi.
Study framework
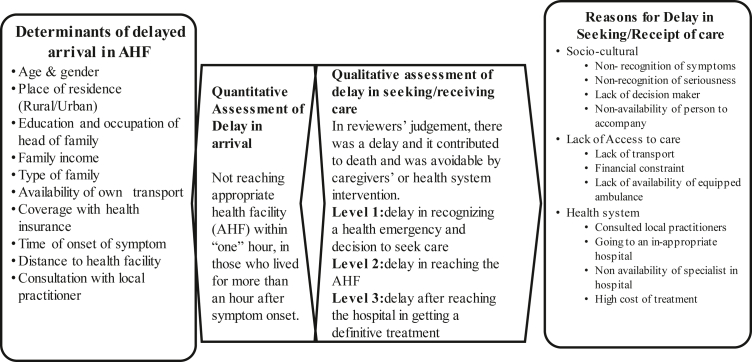
The study adapts the ‘three delay’ model (3DM) used in addressing maternal mortality.14,15 The model proposes three critical points (or levels) of delay in seeking/receiving care - i) in recognizing a health emergency and deciding to seek care, ii) in reaching the right facility for care and iii) in getting a definitive treatment after reaching the hospital. The understanding gained by this model has been used for implementing public health interventions like centralized ambulance services, providing free obstetric care, and setting up first referral units to provide essential obstetric care. However, the delays are systemic and not specific to obstetric emergencies.16 The same model has been applied for neonatal care as well as to essential surgical care and may apply to cardiac and stroke care as well.17,18 (Fig. 1).
Fig 1.
Conceptual framework of the study.
While there does exist complex interplay between the three phases, one type of delay is not linked inextricably with another. Also, in this model, the first level delay is related to socio-economic and cultural factors, the second level is affected by access to health services and the third level delay is indicative of the quality of care issues (Fig. 1). Reasons or causes in our framework were related to the circumstances of the terminal event and are based on the description of the actions from the onset of symptoms to the time of death. The reasons for the delay were reported by the caregivers and could be related to family-related factors or health-system related factors. These have been identified as recognition, physical and financial access and quality of care.19 Determinants or risk factors are more distal factors, not directly related to the terminal event but contribute indirectly to the delay. The determinants of reaching a health facility late were related to household-related factors including socio-economic status, distance from the facility, availability of transport etc. as derived from a literature review including maternal death audit instruments.8, 9, 10, 11, 12, 13,20
Methods
This descriptive study was conducted in two out of three tehsils (Badkhal and Ballabgarh) of the Faridabad district of Haryana, India with an estimated population of 21 lakhs in 2020.21 We acquired a list of deaths registered between 1st July 2019 and 30th June 2020 from the Birth and Death Registrar's office of both tehsils after getting written permission from the Municipal Commissioner, Faridabad. While the initial list was retrospective, bi-monthly visits were made to update the list prospectively from September 2019. All premature (30–69 years of age) deaths that occurred during this period among the residents were arranged by geographical area (sector/village). The list included lay reports of the cause of death and all non-injury deaths were included for verbal autopsy (VA).
The family members of the deceased were approached by trained field workers and explained about the study followed by a request for their consent. The preferred family member was one who was involved in care at the time of the terminal event. We used a validated VA tool that had 5 sections - identification details, a narrative of the terminal event, past history, 42 item symptom checklist, and treatment history.22 The filled verbal autopsy forms were reviewed by three physicians and the cause of death was assigned as per the International Classification of Disease-10 (ICD-10). All the physicians involved were certified coders of the MINErVA Network.23 If the physician found difficulty in coding a particular form, this was reviewed by a second physician in the team and the consensus code was considered final. The deaths due to an acute cardiovascular condition and stroke (ICD Codes – I10-11, I13, I20-26, I42, I44-51, I60, I64) were taken up for social audit. The patients who died in sleep or suddenly and did not have a chance to seek care were excluded from social audit.
Assessment of the presence of delay in seeking/receiving care
The family members of the deceased were approached by the trained medical social worker and consent was taken for social audit. A Social audit tool was developed based on a literature review of Maternal Death Audit tool20 and variables listed in the study framework. We measured delays in seeking care in qualitative terms based on the subjective assessment of the description of the terminal event by the authors. A delay was judged to have happened if, in the reviewers' opinion, it contributed to the death and could have been "avoided" with caregiver or health system intervention.24 Three of us (MA, RK, KA) jointly reviewed first 10 forms to develop a common understanding of the three delays classification and its reasons. Subsequently, each form was read by one of the authors (MA) to perform a subjective assessment of the reported delay and reasons given for any such delay reported. There could be multiple delays in a single patient, and these were included at all those levels.
Estimation of the delay in arrival to the appropriate health facility (AHF)
Each of the respondents was asked to provide a detailed timeline of the terminal event, especially of the key endpoints like recognition of symptoms, the decision to seek care, reaching the first health facility and all subsequent ones till reaching the final facility. Based on the timelines provided, we estimated the time intervals between the critical points identified in the above definitions.
Estimation of distance to the nearest AHF
We simultaneously carried out mapping of cardiac and stroke services in the district through a health facility survey which included the availability of human resources, equipment and service provision and plotted the geospatial coordinates of all the health facilities. Based on the reported service availability, we identified hospitals that provided definitive treatment for acute cardiac events/stroke and labeled these as appropriate health facilities (AHF). Definitive treatment was defined as the availability of drug therapy to dissolve the clot or restore flow - fibrinolytic agents (streptokinase, tissue plasminogen activator), or primary coronary angioplasty facility and antithrombins (heparin) therapy.25 We plotted the geospatial coordinates of the deceased residences and measured the distance between them and the nearest AHF using their GPS coordinates. We also identified the postal code of the residence and treated it as a variable.
The data were analyzed using Stata statistical software version 15.0. After cleaning the dataset, it was noted that details on income were not available for 26 participants. These were imputed based on the median value of the households with the same occupation group as the head of the household. The pathway of care till death was traced for each patient to document their health care seeking. A cumulative frequency curve was drawn to plot time to reaching the facility and death.
Based on the estimated time from onset of symptom to reaching AHF, we classified arrival to a health facility as early (reaching within the first hour) or late. We used mixed-effect logistic regression using age, sex, place of residence, education and occupation of the head of the family, family income, distance to the nearest AHF (as a continuous variable), type of family, health insurance coverage, ownership of transport, time of event and consultation with a local practitioner as fixed effects and postal code as a random effect to identify determinants of delayed arrival. All analyses were done separately for stroke and cardiac events except for the logistic regression due to small numbers. The differences in delays in seeking/receiving care between stroke and cardiac emergencies were tested for significance using Chi-square test. A similar analysis was also done to look at differences between the pandemic period (after March 25, 2020) and the pre-pandemic period.
In addition, we conducted in-depth interviews (IDI) with 6 cardiologists and 2 neurologists/neurosurgeons of the hospitals with definitive treatment in the district to understand their perspective on delays and barriers to care for data triangulation. We undertook a thematic content analysis of these interviews using a deductive approach based on the three-delay model framework.
Role of funding source
Indian Council of Medical Research (funding agency) had no role in study design, data collection, data analysis, interpretation and writing of the paper.
Results
From a total of 7164 deaths registered during the study period in the selected tehsils of Faridabad, 4089 (57%) deaths between 30 and 69 years were identified. Among the 3415 deaths of residents of the selected tehsils, 519 had incorrect addresses and 382 interviews could not be done due to COVID-19 related movement restrictions. Of the 2466 deaths with verbal autopsies, 761 (30.8%) were classified as due to CVDs. Of these, 517 deaths were classified as due to the pre-decided ICD codes and were eligible for assessment of delays in acute cardiac/stroke care. Social audits were done for 435 deaths and the remaining 82 could not be contacted or refused (Supplementary Fig. S1).
The profile of the deceased is shown in Supplementary Table. S1. There was a male preponderance (67.4%), 74.2% resided in urban areas and 81.6% were married. About half of the families had income below USD 270 per month, 21% of families did not own a vehicle and 53% were not covered by any health insurance scheme.
The characteristics of the terminal event are shown in Table 1. An ambulance was used in only 4.1% of the cases (8.1% in stroke cases) and in 32% of cases a vehicle was borrowed or hired to transfer the patient to hospital. Sixty-seven percent of the deaths occurred outside hospitals with about 21% occurring in transit. Only in 19.5% of the cases, the first health facility visit was to an AHF, 81% of which were from urban areas. Among those who sought care, the mean number of facilities visited was 1.7(SD: 1.03).
Table 1.
Description of the terminal acute cardiac or stroke event and related care seeking.
| Parameter | Cardiac event n = 323 | Stroke n = 112 | Total n = 435 |
|---|---|---|---|
| Time of onset of first symptom, n (%) | |||
| 6:00 am–1:59 pm | 129 (39.9) | 58 (51.8) | 187 (43.0) |
| 2:00 pm–9:59 pm | 100 (31.0) | 40 (35.7) | 140 (32.2) |
| 10:00 pm–5:59 am | 94 (29.1) | 14 (12.5) | 108 (24.8) |
| Transport used while taking to the hospital, n (%) | |||
| Did not use transport | 127 (39.3) | 38 (33.9) | 165 (37.9) |
| Ambulance | 9 (2.8) | 9 (8.1) | 18 (4.1) |
| Own vehicle | 85 (26.3) | 28 (25.0) | 113 (26.0) |
| Borrowed or hired vehicle | 102 (31.6) | 37 (33.0) | 139 (32.0) |
| No. of hospital visited, n (%) | |||
| 0 | 186 (57.6) | 49 (43.8) | 235 (54.0) |
| 1 | 80 (24.8) | 27 (24.1) | 107 (24.6) |
| 2 | 34 (10.5) | 23 (20.5) | 57 (13.1) |
| 3 | 16 (4.9) | 7 (6.2) | 23 (5.3) |
| 4 or more | 7 (2.2) | 6 (5.4) | 13 (3.0) |
| Place of death, n (%) | |||
| Home | 147 (45.5) | 52 (46.4) | 199 (45.8) |
| Transit | 75 (23.2) | 17 (15.2) | 92 (21.2) |
| Hospital | 101 (31.3) | 43 (38.4) | 144 (33.0) |
| % Where first hospital visit was to an Appropriate Health Facility | 62 (19.2) | 23 (20.5) | 85 (19.5) |
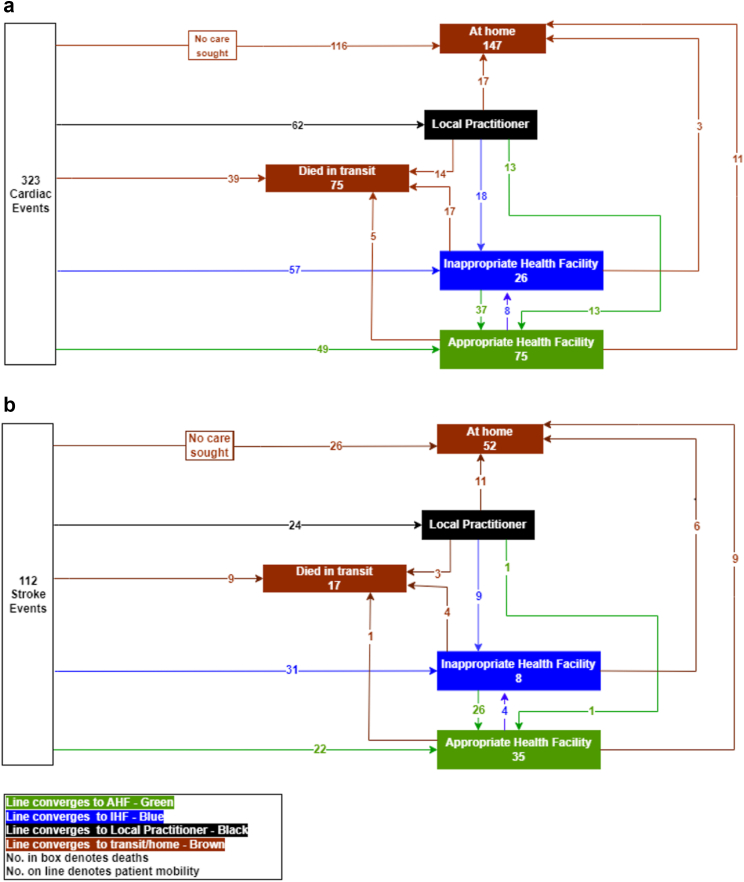
The care-seeking pathways of the terminal event for stroke and cardiac event are shown in Fig. 2. During the cardiac event, 36% (116/323) did not seek care, 15% (49/323) went directly to an AHF and 13 (4.2%) reached after being referred by the local practitioner. For stroke, these proportions were 23%, 19.6% and 1% respectively. One-fifth (62/323) of those with a cardiac emergency and 21% (24/112) with stroke sought treatment from a local practitioner who were more likely to refer to a non-AHF than AHF. About 4.3% of cardiac and 13.4% of stroke patients who reached a hospital went back and died at home.
Fig. 2.
Care seeking pathways of the terminal event of acute cardiac condition (Panel a.) and stroke (Panel b.).
The social audit showed that no delay was noted in 48% of cardiac cases and 33.9% of stroke cases (p value < 0.005). One-third of the deaths (38.4%; same in stroke and cardiac cases) reported level-1 delay which was due to non-recognition of symptoms as myocardial infarction or stroke (59.9%) and underestimating the seriousness of the situation (17.3%). In 16.2% of cases consulting a local practitioner was also adjudged to have led to a delay, more for stroke. Twenty percent of the cases (25.9% for stroke; p < 0.0001) reported level-2 delays which were attributed to lack of affordability (29.9%), going to an inappropriate hospital (40.2%) and delay in arranging transport (12.6%). Level-3 delay was present in 10.8% of cases (16.1% in stroke; p < 0.0001) with lack of affordability (57.4%) being reported as the prime reason. More than one level of delay was seen in 13.1% (57/435) of cases (Table 2). Eighty seven (20.5%) of these 425 cases died during the period of COVID-19 lockdown. Our analysis did not show any significant differences in the occurrence of the three levels of delay during this period.
Table 2.
Level of delays in seeking/receiving care and their reasons among those who died due to acute cardiac and stroke event in district Faridabad.
| Levels of delay & reasonsa | Overall |
||
|---|---|---|---|
| Cardiac event N = 323 |
Stroke N = 112 |
Total N = 435 |
|
| No delay | 155 (48.0) | 38 (33.9) | 193 (44.4) |
| Level-1 delay | 124 (38.4) | 43 (38.4) | 167 (38.4) |
| Reasons for Level 1 delay | n = 124 | n = 43 | n = 167 |
| Non- recognition of symptoms to be related to heart or brain attack | 79 (63.7) | 21 (48.8) | 100 (59.9) |
| Did not appreciate seriousness of problem | 22 (17.8) | 7 (16.3) | 29 (17.3) |
| Consulted neighbourhood practitioner | 14 (11.3) | 13 (30.2) | 27 (16.2) |
| Lack of decision maker | 3 (2.4) | 2 (4.7) | 5 (3.0) |
| Financial constraint | 6 (4.8) | 0 (0.0) | 6 (3.6) |
| Level-2 delay | 58 (18.0) | 29 (25.9) | 87 (20) |
| Reasons for Level-2 delay | n = 58 | n = 29 | n = 87 |
| Lack of affordability | 16 (27.6) | 10 (34.5) | 26 (29.9) |
| Going to a hospital where appropriate care was not available. | 18 (31.0) | 17 (58.6) | 35 (40.2) |
| Delay in arranging transport | 10 (17.3) | 1 (3.5) | 11 (12.6) |
| Non-availability of a person to accompany the patient | 9 (15.5) | 1 (3.5) | 10 (11.5) |
| Hesitancy to visit a facility during COVID-19 | 5 (8.6) | 0 (0.0) | 5 (5.7) |
| Level-3 delay | 29 (9.0) | 18 (16.1) | 47 (10.8) |
| Reasons for Level 3 delay | n = 29 | n = 18 | n = 47 |
| Lack of money | 14 (48.3) | 13 (72.2) | 27 (57.4) |
| Non-availability of specialist or ICU bed in the facility | 15 (51.7) | 5 (27.8) | 20 (42.6) |
Multiple levels of delays possible in a case.
The median (IQR) time interval between the onset of symptoms and death was 2.0 (0.76, 12.0) hours in a cardiac event and 22.4 (1.8, 75.9) hours in a stroke (Supplementary Fig. S2). Among those who reached an AHF, the median (IQR) time interval between the onset of symptoms and reaching it was 1.5 (1.0, 56.0) hours in a cardiac event and 2.2 (1.1, 9.0) hours in a stroke. Only 10.8% of the subjects reached an appropriate health facility early i.e., within the first “golden” hour of the onset of the symptoms. This was similar in cardiac and stroke cases.
Using mixed-effect logistic regression, we identified that for a given postal code, after adjusting for other variables patients with a monthly family income of >270US$ (aOR 0.44; 95%CI 0.21–0.93) were less and those staying farther from AHF (aOR 1.12; 95%CI 1.01–1.25 for each kilometer distance) were more likely to have a delay (Table 3). We further probed the rural-urban differential. While in bivariate analysis, urban residents had an odds ratio of 0.76 (95% CI; 0.36–1.58), once adjusted for other variables especially distance to AHF, the odds ratio changed to 2.7 (95%CI 0.91–7.97). The mean distance to AHF was 4.1 km (SD 2.2) and 12.2 km (SD 5.3) for urban and rural residents respectively and it was the main contributor to the change in OR after adjustment.
Table 3.
Determinants of delay in reaching an appropriate health facility from onset of symptoms among acute cardiac and stroke deaths in District Faridabad.
| Parameter | Within 1 h N = 47, n (%) | After 1 h N = 388, n (%) | Crude OR (95%CI) | Adjusted OR (95%CI) |
|---|---|---|---|---|
| Age in years | ||||
| ≤60 | 28 (12.1) | 204 (87.9) | 0.75 (0.41–1.39) | 0.80 (0.41–1.57) |
| >60 | 19 (9.4) | 184 (90.6) | Reference | Reference |
| Gender | ||||
| Male | 34 (11.6) | 259 (88.4) | 0.77 (0.39–1.50) | 1.10 (0.51–2.36) |
| Female | 13 (9.2) | 129 (90.9) | Reference | Reference |
| Place of residence | ||||
| Rural | 10 (8.9) | 102 (91.1) | Reference | Reference |
| Urban | 37 (11.5) | 286 (88.5) | 0.76 (0.36–1.58) | 2.70 (0.91–7.97) |
| Education of head of the family | ||||
| Primary & illiterate | 13 (6.2) | 196 (93.8) | Reference | Reference |
| Above primary | 34 (15.0) | 192 (85.0) | 0.37 (0.19–0.73) | 0.52 (0.24–1.11) |
| Occupation of head of family | ||||
| Professional/semi-professional/clerical | 21 (14.5) | 124 (85.5) | 0.58 (0.31–1.07) | 0.60 (0.31–1.16) |
| Skilled/semi-skilled/unskilled worker | 26 (9.0) | 264 (91.0) | Reference | Reference |
| Monthly family income (INR) | ||||
| ≤270 US$ | 14 (6.2) | 213 (93.8) | Reference | Reference |
| >270 US$ | 33 (15.9) | 175 (84.1) | 0.35 (0.18–0.67) | 0.44 (0.21–0.93) |
| Type of Family | ||||
| Nuclear | 16 (11.4) | 125 (88.7) | Reference | Reference |
| Joint | 31 (10.5) | 263 (89.5) | 1.09 (0.57–2.06) | 1.56 (0.75–3.23) |
| Own a transport vehicle | ||||
| Four-wheeler/Two-wheeler | 42 (12.2) | 302 (87.8) | 0.42 (0.16–1.09) | 0.63 (0.22–1.81) |
| None | 5 (5.5) | 86 (94.5) | Reference | Reference |
| Health insurance status | ||||
| Private/Govt. insurance | 27 (13.2) | 177 (86.8) | 0.62 (0.34–1.15) | 0.87 (0.44–1.69) |
| None | 20 (8.7) | 211 (91.3) | Reference | Reference |
| Time of onset of symptom | ||||
| 6:00 am–9:59 pm | 31 (9.5) | 296 (90.5) | 1.66 (0.87–3.17) | 1.42 (0.71–2.85) |
| 10:00 pm–5:59 am | 16 (14.8) | 92 (85.2) | Reference | Reference |
| Distance to Appropriate Health Facility (in km), median (IQR) | 4.1 (2.2, 6.8) | 5.2 (3.1, 7.8) | 1.10(1.01–1.20) | 1.12 (1.01–1.25) |
| Consulted a local practitioner | ||||
| Yes | 4 (4.7) | 82 (95.4) | 2.88 (1.01–8.26) | 2.39 (0.79–7.21) |
| No | 43 (12.3) | 306 (87.7) | Reference | Reference |
In their interviews, specialists identified poor risk perception and non-recognition or late recognition of symptoms as major reasons for level-1 delay. Additional factors identified were a lack of awareness of the availability of cardiac/stroke services in public facilities, fear of the high cost of treatment combined with poor paying capacity of the people. Lack of adequate ambulance services, awareness and recognition of these conditions by primary care providers and triage capacity of the first responders in the ambulance were identified as additional barriers to reaching the appropriate place of care. The high cost of treatment and fear of over-use of interventions at private facilities were also listed as key reasons for level-3 delay.
Discussion
This is, to our best knowledge, the first community-based study to identify delays in acute cardiac and stroke care among the deceased using social audit methodology. About 55% of the deaths reported a delay and most of it occurred at home due to delay in seeking care and the least occurred at the facility level. The inability to recognize the severity of illness and financial constraints were identified as major reasons for the delays in seeking care. About half of the deceased did not visit any health facility during their terminal illness and only one in ten subjects reached an appropriate health facility within the first hour after onset of the symptoms. Those staying closer to a facility or families with higher income were more likely to reach within the first hour. In general, stroke reported greater delays especially at level 2 and 3.
Previous hospital-based studies from the Indian subcontinent have also reported delays at the level of deciding to seek care. In patients of myocardial infarction and stroke presenting to tertiary hospitals, the mean interval between onset of symptom and arrival at the hospital was reported to be between 6 and 13 h in various studies.10,13,26, 27, 28 This was much lower (around 2 h) in our study as ours was a community-based study and only one-third of the deaths occurred in a hospital. Tertiary hospitals receive referred patients including many from distant places and thus time to arrival could be high.
While we did not find age to be an important determinant of delay, previous studies have reported older age to be associated with higher delay.8, 9, 10,27, 28, 29 Few studies have reported a higher delay among women,14,28 but many studies including ours did not find so.27,28,30,31 The primary reason for delay identified in all studies has been the lack of awareness of the symptoms to be related to MI or stroke resulting in non-recognition of the severity of their illness. Our study confirms these findings.
The evidence on the influence of socio-economic factors like education or income on delay are mixed. In general, income has been found to be more important than education in explaining the delay. We found family income to be an important determinant of delay as reported in other studies.28,29 In our study as well as in the study by Mohan et al.,9 lack of insurance coverage was not associated with delay. However, unlike 8% coverage with insurance reported in Mohan et al.,9 our study had a much higher 47% coverage.
Most previous studies have reported that rural residents take longer to reach hospital.32 Main reasons cited for delay in the rural areas are distance, availability of transport and poorer socio-economic conditions. Our study shows that it is the distance and not socio-economic status that primarily explains this rural-urban difference. Also, Faridabad is largely an urban (65%) district and even rural areas have good road connectivity. Most of the AHF mapped by us were at the centre of the district making them accessible. The classification of rural/urban areas was based on 2011 census. There is rapid urbanization occurring in the district and this could have resulted in misclassification of rural/urban areas.
A low use of ambulance (varying from 3.9% to 37%) and higher use of private vehicle has been almost universally reported among studies from the subcontinent.9,28,29,31 This is in contrast to developed countries like Hongkong and USA where its use is much higher.33,34 While we did not find a higher delay if family members consulted a local practitioner or a primary care provider, others have reported so.27,28 This delay occurs due to the time taken for the consultation as well as due to these care-providers failing to recognize the severity of the condition, not providing immediate care and, referring to an inappropriate hospital.
This study enabled us to compare the delays between stroke and cardiac emergencies. It showed that there was higher likelihood of delay occurring in stroke cases, especially at level 2 and level 3. These may be attributed to poorer availability of stroke services than cardiac services in the district and also elsewhere in India. This was confirmed by service mapping done by us in the district (not published). Due to small number of cases, we could not compare the determinants of delayed arrival between stroke and cardiac deaths.
The strengths of this study are that this is population-based and covers both acute cardiac and stroke care by audit of large number of deaths in a geographically circumscribed area with defined population and universal registration of deaths, using the established three-delay model which are clearly linked to public health interventions. Data triangulation with the qualitative component further validates our finding. The weaknesses were inability to do verbal autopsy in 11% deaths due to COVID-19 restrictions, since only deaths were covered this does not reflect the delays in all acute cardiac or stroke cases. Hospital based studies have shown that during lockdown due to pandemic restrictions, there was an increase in delays in stroke and cardiac patients reaching the hospitals.35,36 Our sub-analysis, though small in numbers, did not reveal higher health system access delay in deaths that occurred during the period when lockdown was imposed. The delays assessed qualitatively and quantitatively did not always arrive at same conclusion, for example, there might be no delays reported qualitatively yet they may reach AHF after 1 h. Though a formal sample size estimation was not done as a geographical defined area was saturated, the sample size appears to be sufficient to estimate proportion of delays, though not separately for stroke. Due to smaller numbers, estimates for some of the covariates had wide confidence intervals.
The delays identified in the study point out to the need for interventions at population and health system levels. There have been many health system initiatives in India to reduce delays in cardiac and stroke care. These include a hub-and-spoke model for myocardial infarction management, where primary angioplasty is offered to patients presenting to hub hospitals with catheterization capacities or those close to it (within 30 min) and thrombolysis to those presenting to spoke hospitals, who are then shifted within 2–24 h to the hub hospital for catheterization and angioplasty.37 Mobile units as specialized ambulances equipped with the personnel, equipment, and imaging capability to diagnose and treat acute stroke in the prehospital setting have been shown to be effective.38 Mission DELHI (Delhi Emergency Life Heart-Attack Initiative) initiative employs a pair of motorcycle-borne trained paramedic nurses as the first responders to a call, who do clinical assessment, take an ECG, and establish a virtual connect with the cardiologists to deliver specific treatment. By this time, an equipped ambulance arrives and transports the patient for further treatment.39 Linking primary care physician by telemedicine facilities with cardiologists has also been successfully attempted. A similar tele-stroke model appropriate for poor resources countries and development of uniform stroke care pathways are also steps in similar direction.40,41
While many of these have been implemented in an ad-hoc mode, a fully integrated district level scalable model needs to be developed in an implementation research paradigm. Establishment of cardiac care units at district hospitals under National Programme for Cancer, Diabetes and Cardiovascular Diseases and Stroke is also aimed at improving access to cardiac care in public facilities.42 These can be strengthened to provide integrated care for stroke and acute cardiac event.
These health system interventions should be supplemented by efforts to create public awareness in recognizing symptoms of heart attack and stroke and by improving insurance coverage for these life threatening conditions. Community educational campaigns to improve symptom awareness to promote early recognition and care-seeking and use of ambulance have been shown to be effective.43, 44, 45 Training of formal and informal primary care providers to recognize these conditions and refer them to an appropriate hospital has also proved useful.46
This study confirms the urgency of the need to strengthen cardiac and stroke acute care responses to improve outcomes due to the burgeoning cardiovascular burden in India. We have the necessary evidence to reduce the delays in cardiac and stroke care and the benefits of this must reach people at the earliest.
Contributors
Conceptualizaiton -AK, AR and RK; funding acquisition- AK; study planning-AK, AR, RA and RB; methodology-AK, AR, RB and RK; Supervision-AK, MA and RK; Writing – original draft & Finalization-AK; Data curation & Data analysis-MA; Project administration-MA, RA and RK; Validation-AK and AR; Writing – review & editing-MA, RK, RA, RB and AR.
Data sharing statement
The data used for current study is available with the corresponding author. It can be shared with the researcher upon getting approval from Institutional Ethics Committee.
Declaration of interests
We declare no financial or any other competing interests among authors.
Acknowledgments
We are thankful to the Indian Council of Medical Research (ICMR), India for granting fund with grant number 5/4/8-2/2019-NCD-1 for this study. We acknowledge the study team members including field worker, medical social worker for data collection. We are thankful to the caregivers of deceased for their active participation in the study, heath facility in-charges for their support in mapping of services; and the specialists who have given their valuable time for sharing their views on delays and barriers in acute cardiac and stroke care in the district.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100222.
Appendix A. Supplementary data
References
- 1.Cardiovascular diseases (CVDs) [Internet] https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds [cited 2022 Mar 12]. Available from:
- 2.Global health estimates: leading causes of death [Internet] https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death [cited 2022 Dec 5]. Available from:
- 3.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.India - sample registration system (srs)-cause of death in India 2016-2018 [Internet] https://censusindia.gov.in/nada/index.php/catalog/44232 [cited 2022 Dec 26]. Available from:
- 5.Peacock W.F., Hollander J.E., Smalling R.W., Bresler M.J. Reperfusion strategies in the emergency treatment of ST-segment elevation myocardial infarction. Am J Emerg Med. 2007;25(3):353–366. doi: 10.1016/j.ajem.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 6.De Luca G., Suryapranata H., Ottervanger J.P., Antman E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;09(10):1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 7.Hacke W., Donnan G., Fieschi C., et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363(9411):768–774. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- 8.Rajagopalan R.E., Chandrasekaran S., Pai M., Rajaram R., Mahendran S. Pre-hospital delay in acute myocardial infarction in an urban Indian hospital: a prospective study. Natl Med J India. 2001;14(1):8–12. [PubMed] [Google Scholar]
- 9.Mohan B., Bansal R., Dogra N., et al. Factors influencing prehospital delay in patients presenting with ST-elevation myocardial infarction and the impact of prehospital electrocardiogram. Indian Heart J. 2018;70(Suppl 3):S194–S198. doi: 10.1016/j.ihj.2018.10.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choudhary An Observational study of prehospital and hospital delay in reperfusion for acute myocardial infarction at a University Hospital in India [Internet] https://www.j-pcs.org/article.asp?issn=2395-5414;year=2016;volume=2;issue=3;spage=163;epage=168;aulast=Choudhary [cited 2022 Mar 14]. Available from:
- 11.Mohanan P.P., Mathew R., Harikrishnan S., et al. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34(2):121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel A., Mohanan P.P., Prabhakaran D., Huffman M.D. Pre-hospital acute coronary syndrome care in Kerala, India: a qualitative analysis. Indian Heart J. 2017;69(1):93–100. doi: 10.1016/j.ihj.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abraham S.V., Krishnan S.V., Thaha F., Balakrishnan J.M., Thomas T., Palatty B.U. Factors delaying management of acute stroke: an Indian scenario. Int J Crit Illn Inj Sci. 2017;7(4):224–230. doi: 10.4103/IJCIIS.IJCIIS_20_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thaddeus S., Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091–1110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 15.Mukuru M., Gorry J., Kiwanuka S.N., Gibson L., Musoke D., Ssengooba F. Designed to fail? Revisiting Uganda's maternal health policies to understand policy design issues underpinning missed targets for reduction of maternal mortality ratio (MMR): 2000-2015. Int J Health Policy Manag. 2021;11(10):2124–2134. doi: 10.34172/ijhpm.2021.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calvello E.J., Skog A.P., Tenner A.G., Wallis L.A. Applying the lessons of maternal mortality reduction to global emergency health. Bull World Health Organ. 2015;93(6):417–423. doi: 10.2471/BLT.14.146571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Upadhyay R.P., Krishnan A., Rai S.K., Chinnakali P., Odukoya O. Need to focus beyond the medical causes: a systematic review of the social factors affecting neonatal deaths. Paediatr Perinat Epidemiol. 2014;28(2):127–137. doi: 10.1111/ppe.12098. [DOI] [PubMed] [Google Scholar]
- 18.Bagguley D., Fordyce A., Guterres J., et al. Access delays to essential surgical care using the Three Delays Framework and Bellwether procedures at Timor Leste's national referral hospital. BMJ Open. 2019;9(8) doi: 10.1136/bmjopen-2019-029812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D'Ambruoso L., Kahn K., Wagner R.G., et al. Moving from medical to health systems classifications of deaths: extending verbal autopsy to collect information on the circumstances of mortality. Glob Health Res Policy. 2016;1:2–12. doi: 10.1186/s41256-016-0002-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cahyanti R.D., Widyawati W., Hakimi M. The reliability of maternal audit instruments to assign cause of death in maternal deaths review process: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2021;21(1):380. doi: 10.1186/s12884-021-03840-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faridabad population 2022 [Internet] https://www.indiacensus.net/district/faridabad [cited 2022 Jul 27]. Available from:
- 22.Krishnan A., Kumar R., Nongkynrih B., Misra P., Srivastava R., Kapoor S.K. Adult mortality surveillance by routine health workers using a short verbal autopsy tool in rural north India. J Epidemiol Community Health. 2012;66(6):501–506. doi: 10.1136/jech.2010.127480. [DOI] [PubMed] [Google Scholar]
- 23.Krishnan A., Gupta V., Nongkynrih B., et al. Mortality in India established through verbal autopsies (MINErVA): strengthening national mortality surveillance system in India. J Glob Health. 2020;10(2) doi: 10.7189/jogh.10.020431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Upadhyay R.P., Rai S.K., Krishnan A. Using three delays model to understand the social factors responsible for neonatal deaths in rural Haryana, India. J Trop Pediatr. 2013;59(2):100–105. doi: 10.1093/tropej/fms060. [DOI] [PubMed] [Google Scholar]
- 25.Aylward P. Acute myocardial infarction: early treatment. https://www.nps.org.au/australian-prescriber/articles/acute-myocardial-infarction-early-treatment [cited 2022 Jul 27]. Available from:
- 26.Arulprakash N., Umaiorubahan M. Causes of delayed arrival with acute ischemic stroke beyond the window period of thrombolysis. J Fam Med Prim Care. 2018;7(6):1248–1252. doi: 10.4103/jfmpc.jfmpc_122_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Srivastava A.K., Prasad K. A study of factors delaying hospital arrival of patients with acute stroke. Neurol India. 2001;49(3):272–276. [PubMed] [Google Scholar]
- 28.Panda P., Singh N.V., Kaur N., et al. Delay in seeking medical treatment among patients with acute coronary syndrome. Cureus. 2021;13(8) doi: 10.7759/cureus.17369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rafi A., Sayeed Z., Sultana P., Aik S., Hossain G. Pre-hospital delay in patients with myocardial infarction: an observational study in a tertiary care hospital of northern Bangladesh. BMC Health Serv Res. 2020;20(1):633. doi: 10.1186/s12913-020-05505-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kafle R.C., Paudel N., Jha G.S., Sharma D., Alurkar V.M. Factors associated with pre-hospital delay before reperfusion therapy in patients with ST-segment elevation myocardial infarction. J Lumbini Med Coll. 2018;6(2):68–72. [Google Scholar]
- 31.George L., Ramamoorthy L., Satheesh S., Saya R.P., Subrahmanyam D.K.S. Prehospital delay and time to reperfusion therapy in ST elevation myocardial infarction. J Emerg Trauma Shock. 2017;10(2):64–69. doi: 10.4103/0974-2700.201580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varjoranta T., Raatiniemi L., Majamaa K., Martikainen M., Liisanantti J.H. Prehospital and hospital delays for stroke patients treated with thrombolysis: a retrospective study from mixed rural-urban area in Northern Finland. Australas Emerg Care. 2019;22(2):76–80. doi: 10.1016/j.auec.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 33.Lau K.K., Yu E.L., Lee M.F., Ho S.H., Ng P.M., Leung C.S. Ambulance use affects timely emergency treatment of acute ischaemic stroke. Hong Kong Med J Xianggang Yi Xue Za Zhi. 2018;24(4):335–339. doi: 10.12809/hkmj177025. [DOI] [PubMed] [Google Scholar]
- 34.Jauch E.C., Saver J.L., Adams H.P., et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 35.Ramachandran D., George G.B., Panicker P., Aravind R., Suresh M.K., Iype T. COVID-19 and stroke trends in A tertiary care center from south India -our monsoon experience. Neurol India. 2022;70(5):1942–1946. doi: 10.4103/0028-3886.359188. [DOI] [PubMed] [Google Scholar]
- 36.Choudhary R., Gautam D., Mathur R., Choudhary D. Management of cardiovascular emergencies during the COVID-19 pandemic. Emerg Med J. 2020;37(12):778–780. doi: 10.1136/emermed-2020-210231. [DOI] [PubMed] [Google Scholar]
- 37.Alexander T., Mullasari A., Nallamothu B. Management strategies for acute STEMI in low- and middle-income countries: experience of the Tamil Nadu ST-segment elevation myocardial infarction programme. Asia Intervent. 2021;7(1):27–34. doi: 10.4244/AIJ-D-21-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Navi B.B., Audebert H.J., Alexandrov A.W., Cadilhac D.A. Grotta JC, PRESTO (prehospital stroke treatment organization) writing group. mobile stroke units: evidence, gaps, and next steps. Stroke. 2022;53(6):2103–2113. doi: 10.1161/STROKEAHA.121.037376. [DOI] [PubMed] [Google Scholar]
- 39.Mission_Delhi_Pilot_Project.pdf [Internet] https://main.icmr.nic.in/sites/default/files/Mission_Delhi_Pilot_Project.pdf [cited 2022 Dec 26]. Available from:
- 40.Sharma S., Padma M.V., Bhardwaj A., Sharma A., Sawal N., Thakur S. Tele-stroke in resource-poor developing country model. Neurol India. 2016 Sep-Oct;64(5):934–940. doi: 10.4103/0028-3886.190243. [DOI] [PubMed] [Google Scholar]
- 41.Bhatia R., Haldar P., Puri I., Padma Srivastava M.V. IMPETUS study investigators. Study protocol: IMPETUS: implementing a uniform stroke care pathway in medical colleges of India: IMPETUS stroke. Ann Indian Acad Neurol. 2022;25(4):640–646. doi: 10.4103/aian.aian_1033_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Directorate general of health services [Internet. https://dghs.gov.in/content/1363_3_NationalProgrammePreventionControl.aspx [cited 2022 Dec 26]. Available from:
- 43.Mellon L., Doyle F., Rohde D., Williams D., Hickey A. Stroke warning campaigns: delivering better patient outcomes? A systematic review. Patient Relat Outcome Meas. 2015;6:61–73. doi: 10.2147/PROM.S54087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mooney M., McKee G., Fealy G., O'Brien F., O'Donnell S., Moser D. A review of interventions aimed at reducing pre-hospital delay time in acute coronary syndrome: what has worked and why? Eur J Cardiovasc Nurs. 2012;11(4):445–453. doi: 10.1016/j.ejcnurse.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 45.Yuan J., Li M., Liu Y., et al. Analysis of time to the hospital and ambulance use following a stroke community education intervention in China. JAMA Netw Open. 2022 May 2;5(5) doi: 10.1001/jamanetworkopen.2022.12674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sun X.G., Zhang N., Wang T., et al. Public and professional education on urgent therapy for acute ischemic stroke: a community-based intervention in Changsha. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2013;34(12):2131–2135. doi: 10.1007/s10072-013-1348-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.