ABSTRACT
The arteriovenous fistulas (AVFs) of the vertebral artery are usually caused by iatrogenic and penetrating traumas. Vertebral AVF is rarely seen after blunt cervical trauma. A 65-year-old male patient applied to the emergency clinic due to falling from a height of about 3 m. In his neurological examination, he had weakness in the left upper limb and tinnitus in the left ear. The cervical computed tomography examination showed a Hangman’s fracture, a C3 vertebra corpus compression fracture, and a C1 anterior arch fracture. There was a separation on the C1-2 transverse foramen due to the fracture, and there was a fracture in the left C3-4 transverse foramen. In cervical magnetic resonance imaging (MRI), the presence of a contusion in the spinal cord at the C2 corpus level was observed. Through an MRI angiography examination of the vertebral artery, it was determined that the left vertebral artery had developed an AVF at the V2-3 segment level. Stabilization surgery was performed with a posterior approach for unstable vertebrae. Then, vertebral AVF was then closed endovascularly using a stent coil. Improvement in neurological deficit was seen after surgery and endovascular treatment. There were no complications related to the procedure. Transverse foramen should be carefully evaluated, especially in the upper cervical trauma. Vertebral artery imaging should be performed before instability surgery in the presence of a separation in the fracture line to determine whether the damage to the vertebral artery is iatrogenic.
Keywords: Blunt neck trauma, endovascular treatment, vertebral arteriovenous fistulas
INTRODUCTION
Cervical traumas often occur due to traffic accidents, falling from a height, sports injuries, and diving. Approximately 25–35% of cervical vertebra fractures in adults are related to the first three vertebrae.[1] Neurological deficits occur in 45–60% of the upper cervical traumas.[2] Vertebral arteries can be damaged directly due to a fracture in the transverse foramen as well as during tension or dislocation during hyperextension due to lateral mass connections.[3] Vascular injury in this area can be seen as minimal intimal injury, intimal flap imaging, pseudoaneurysm, dissection accompanied by intraural hematoma, complete vascular occlusion, extravasation, or arteriovenous fistula (AVF).[4]
A spinal AVF is a rare lesion that is usually detected relatively late.[5] It has been reported that AVF in a vertebral artery typically develops iatrogenically due to percutaneous nerve blog applications and radiation therapy after vascular applications, such as central venous catheterization and diagnostic cerebral angiography.[6] In addition, cases of AVF can occur after penetrating neck injury or cervical spine surgery.[6] A relationship between blunt trauma and AVF is rarer; only two cases have been reported in the literature.[5,6]
CASE REPORT
A 65-year-old male patient applied to the emergency clinic due to falling from a height of about 3 m. He had weakness in the left upper limb and tinnitus in the left ear. In his physical examination, the Glasgow coma score was 15 points, the cranial nerve examination was natural, the proximal and distal muscle group in the left upper extremity had 3/5 motor strength, and there was no motor deficit in the lower extremities.
The cervical computed tomography (CT) examination showed a Hangman’s fracture (Effendi/Levin type 2a, Francis grade 3), a C3 vertebra corpus compression fracture, and a C1 anterior arch fracture. There was a separation on the C1-2 transverse foramen due to the fracture, and there was a fracture in the left C3-4 transverse foramen (Fig. 1).
Figure 1.

(a) Computed tomography (CT) sagittal view; anterior dislocation due to hangman’s fracture and collapse in the C3 corpus. (b) In the coronal 3D image, C1 anterior arc fracture, pedicular dissociation in the transverse foramen. (c) In the coronal plan CT image, C2 vertebral fracture. (d) Cervical fracture. (d) Cervical CT axial plane; Decomposition image in C2 vertebral pedicle and transverse foramen
In cervical magnetic resonance imaging (MRI), the presence of a contusion in the spinal cord at the C2 corpus level was observed. Through an MRI angiography examination of the vertebral artery, it was determined that the left vertebral artery had developed an AVF at the V2-3 segment level (Fig. 2).
Figure 2.

(a) In cervical sagittal T2 magnetic resonance imaging (MRI) examination; image of myelomalesis in the spinal cord, (b) vertebral artery MRI angiographic examination, black arrow; right vertebral artery, white arrow shows filling defect and arteriovenous fistulas (AVF) in the left vertebral artery, and (c) image of MRI angiography AVF in the coronal plane.
The Hangman’s fracture was considered unstable, and stabilization of the unstable spine segment was planned was the first priority. Using a posterior approach, stabilization was achieved with a bilateral C1 lateral mass, a C2 transpedicular, and a C3-4 lateral mass screw. In the early post-operative neurological examination, the GKS was 15 points, and no motor or sensory deficit differences were observed between this examination and the pre-operative examination. X-ray and cervical MRI images from the first post-operative day are shown in Figure 3.
Figure 3.
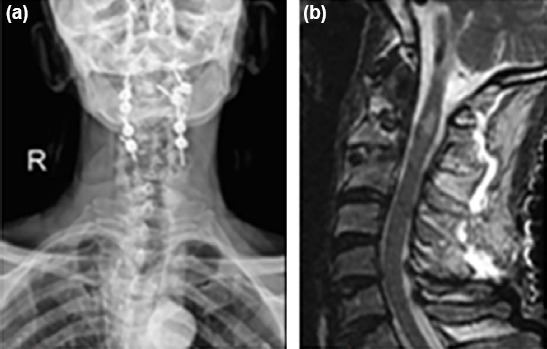
(a) X-ray image after cervical stabilization. (b) Status of cervical contusion at the post-operative C2 vertebra level.
In the early post-operative period, digital subtraction angiography (DSA) and endovascular treatment were recommended to the patient due to the AVF in the left vertebral artery, but the patient refused the treatment.
The patient was discharged without additional neurological deficits and followed up with clinically. In the post-operative one-month clinical examination, there was no increase in the deficit in the left upper extremity. However, the complaint of tinnitus in the left ear has increased. A cervical MRI, a vertebral artery MRI angiography, and a cervical CT angiography were conducted, and an increase in the AVF size or myelomalacia was not observed in the spinal cord (Fig. 4). For this reason, endovascular treatment was recommended again, but the patient did not accept the operation, saying that the tinnitus did not bother him much.
Figure 4.

(a) Magnetic resonance imaging angiography image of arteriovenous fistulas (AVF) 1 month after trauma. (b) Contrast-enhanced computed tomography image of AVF 1 month after trauma.
In the post-operative 3-month control examination, it was observed that the deficit in the patient’s left upper limb had partially improved (Motor strength: 3–4/5). At this time, the patient stated that his complaint of tinnitus disturbed him, and he wanted to be treated. Following confirmation of the treatment, DSA imaging was performed. The AVF on the left vertebral artery was observed during right vertebral artery imaging. Following the treatment planning, the AVF was closed by coil/stent embolization in a second endovascular session. There were no complications during or after this procedure, and the patient’s complaint of tinnitus resolved. DSA images of the AVF on the left vertebral artery before and after the endovascular treatment are shown in Figures 5 and 6, respectively.
Figure 5.

(a) Filling of arteriovenous fistulas (AVF) on the left vertebral artery in the right vertebral artery digital subtraction angiography (DSA) examination. (b) AVF filling in the late venous phase in DSA.
Figure 6.

(a) Digital subtraction angiography (DSA) image of the arterial phase taken from the right vertebral artery after endovascular treatment. (b) Late venous phase DSA image after endovascular treatment.
DISCUSSION
AVF in the vertebral artery usually occurs iatrogenically.[6] In AVF, a high flow shunt is formed from the artery to the vein. Thus, dilation is observed in the vein after arterialization of the vein. In general, it appears as a dural AVF, also known as a pial AVF.[7] This condition can be diagnosed in an MRI examination through the presence of edema in the spinal cortex, flow gaps, and perimedullary venous engorgement. [8] An extradural AVF is less common and usually observed in the cervical region.[7] It occurs between the branches of the vertebral artery and the paravertebral vein, the epidural venous plexus, the internal jugular vein, or the perimedullary vein.[8] In an MR examination, irregularities, dilated venous structures, and myelomalacia can be seen in the related vertebral artery trace.
The Denver criteria can be used to determine the risk of vascular injury in cases of blunt craniocervical trauma (BCT). [3] The CT examination should be evaluated in terms of vertebral artery injuries, especially in blunt cervical traumas, in which the upper cervical region is affected (C1-3 vertebrae) or in fractures that extend to the transverse vertebral foramen or cause subluxation.[3,9] Lebl et al.[10] reported that the risk of injury to the vertebral artery was higher in BCT, where the separation of the transverse foramen was more than 1 mm. In one report, a patient’s vertebral artery was trapped between the broken lines after a hangman’s fracture. [11] In addition, angiographic examination is recommended with facet joint dislocation with or without fracture and type three odontoid fractures in terms of vertebral artery injury.[3] Our patient had C2-3 anterior dislocation due to a hangman’s fracture. At the same time, there were fractures and separation in the left transverse vertebral foramen of more than 1 mm. For these reasons, it was thought that a vertebral artery injury may accompany the upper cervical injury.
DSA is the gold standard in detecting vascular injury due to BCT.[3] DSA is an invasive test that is not available in small hospitals. Advances in CT technology have proved to be the first screening test in the diagnosis of BCTs, especially with 64-slice and higher CT scanners. One study showed 98% sensitivity and 100% specificity compared to DSA.[12] Meanwhile, since MR angiography can be applied with or without contrast, it is useful in cases, where there are contraindications to iodinated contrast matter.[3] In addition, during an MR angiography examination, imaging of the brain and the cervical region to check for ischemia and cord damage, respectively, can be done in the same session. In most vascular injuries, long TE sequences, such as T2W images, may appear as an irregularity or a loss in the normal flow gap.[4] Dietz et al.[13] suggested the use of MR angiography in patients with pulsatile tinnitus. In our case, MRI examination was planned due to the neurological deficit and tinnitus complaint. Non-contrast angiography imaging was performed in the same session. AVF was considered due to the filling defect of the left vertebral artery and the enlargement of the paravertebral veins. However, myelomalacia was observed in the spinal cord at the C2 vertebra level. After this MRI examination, it was concluded that there was AVF in the left vertebral artery at the V2-3 segment. Similar to the two previously reported cases of AVF that developed after BCT, the lesion was at the C1-2 vertebrae level.[5,6]
In general, the risk of vertebral artery injury after spinal surgery is rare.[14] Vertebral artery damage has been reported after the treatment of spinal trauma with an anterior approach.[15] Although no cases of vertebral artery injury due to facet screws applied with posterior approaches to the cervical spine have been reported, Abumi et al.[16] reported that one patient had a vertebral artery injury after transpedicular screw application. Wright et al.[17] reported: a 2.4% risk of vertebral artery injury due to C1-2 transarticular screw fixation. Although the risk of injury in the vertebral artery is low during posterior stabilization surgery, pre-operative vertebral artery integrity must be demonstrated in the upper cervical trauma, which has been shown to be affected by transverse foramen.
Induced venous hypertension and venous stealing due to AVF affect other neighboring structures. Root damage and myelopathy develop due to arterial blood reflux to the spinal pial veins or clogged epidural vein compression.[18] It cannot be precisely said whether the cause of the myelomalacia observed in our patient was a post-traumatic contusion or an epidural venous compression.
Clinical symptoms of AVF are associated with the rate of blood flow in the shunt, the venous drainage pattern, and the chronicity of the mechanical compression.[18] Murmur, heart failure, cervical radiculopathy, and tinnitus can be seen in the iatrogenic AVF clinic.[19] Our case was admitted with complaints of monoparesis of the left arm and tinnitus after falling from a height.
In non-penetrating vertebral AVFs, serial angiographic follow-ups can be performed in asymptomatic low-flow AVF patients.[19] Symptomatic high-flow AVF patients with intracranial hypertension and atrial stealing require occlusion with endovascular therapy after angiographic diagnosis.[19] Excision of the fistula by trapping the proximal and distal ends can be performed surgically.[19] However, in open surgery, difficulties in the exploration of vascular structures may complicate the suturing of the vessel due to an acute post-traumatic inflammatory response and crumbling of the vascular wall. In addition, the fistula canal itself can be hidden by dilated neighboring veins, making open surgery difficult. For these reasons, it has been reported that the morbidity and mortality rates in open surgery are high.[19] In two previously reported cases, the AVFs were closed endovascularly in the early period after trauma.[5,6] In our case, the cervical instability that was primarily due to trauma was treated, and the fistula repair was performed three months after obtaining endovascular treatment consent. No screw malposition was observed in the post-operative imaging. During this period, the patient had no neurological deterioration but an increase in the tinnitus complaint.
After performing the diagnostic DSA procedure, the fistula repair was performed endovascularly using a stent and a coil in different sessions. After the procedure, the patient’s tinnitus complaint improved, and there were no complications related to the procedure.
Conclusion
Vertebral AVF after blunt neck trauma is an extremely rare condition. Transverse foramen should be carefully evaluated, especially in the upper cervical trauma. Vertebral artery imaging should be performed before instability surgery in the presence of a separation in the fracture line to determine whether the damage to the vertebral artery is iatrogenic.
Footnotes
Informed Consent: Written informed consent was obtained from the patient for the publication of the case report and the accompanying images.
Peer-review: Internally peer-reviewed.
Authorship Contributions: Concept: A.Y.; Design: A.Y.; Supervision: A.Y.; Resource: O.U.; Data: O.U.; Analysis: E.D.; Literature search: D.O.K.; Writing: D.O.K.; Critical revision: H.S.I.
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–74. [PubMed] [Google Scholar]
- 2.Caglar Ş, Aydın Z, Tuna H. Traumas in the upper cervical region. In: Aksoy K, editor. Temel Neurosurgery. Vol. 2. Ankara: Turkish Neurosurgery Association; 2005. pp. 1164–73. [Google Scholar]
- 3.Cothren CC, Moore EE. Blunt cerebrovascular injuries. Clinics (Sao Paulo) 2005;60:489–96. doi: 10.1590/s1807-59322005000600011. [DOI] [PubMed] [Google Scholar]
- 4.Kumar Y, Hayashi D. Role of magnetic resonance imaging in acute spinal trauma:A pictorial review. BMC Musculoskelet Disord. 2016;17:310. doi: 10.1186/s12891-016-1169-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heuer GG, Gabel BC, Bhowmick DA, Stiefel MF, Hurst RW, Schuster JM. Symptomatic high-flow arteriovenous fistula after a C-2 fracture. Case report. J Neurosurg Spine. 2008;8:381–4. doi: 10.3171/SPI/2008/8/4/381. [DOI] [PubMed] [Google Scholar]
- 6.Young M, Johnson R, Gordhan A. Acute formation of a blunt trauma-induced vertebral artery arteriovenous fistula treated with endovascular occlusion of vertebral artery. Cureus. 2019;11:e5801. doi: 10.7759/cureus.5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tse GH, Patel UJ, Coley SC, Dyde RA. Cervical cord decompression following embolisation of a giant cervical vertebro-vertebral arteriovenous fistula. Interv Neuroradiol. 2017;23:399–404. doi: 10.1177/1591019917708569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR Am J Roentgenol. 1988;150:405–12. doi: 10.2214/ajr.150.2.405. [DOI] [PubMed] [Google Scholar]
- 9.Mitha AP, Kalb S, Ribas-Nijkerk JC, Solano J, McDougall CG, Albuguergue DC, et al. Clinical outcome after vertebral artery injury following blunt cervical spine trauma. World Neurosurg. 2013;80:399–404. doi: 10.1016/j.wneu.2012.04.029. [DOI] [PubMed] [Google Scholar]
- 10.Lebl DR, Bono CM, Velmahos G, Metkar U, Nguyen J, Harris MB. Vertebral artery injury associated with blunt cervical spine trauma:A multivariate regression analysis. Spine (Phila Pa 1976) 2013;38:1352–61. doi: 10.1097/BRS.0b013e318294bacb. [DOI] [PubMed] [Google Scholar]
- 11.Henkelmann R, Josten C, Glasmacher S, Heyde CE, Spiegl UJA. vertebral artery caught in the fracture gap after traumatic C2/3 spondylolisthesis. Case Rep Orthop. 2017;2017:9179647. doi: 10.1155/2017/9179647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eastman AL, Chason DP, Perez CL, McAnulty AL, Minei JP. Computed tomographic angiography for the diagnosis of blunt cervical vascular injury:Is it ready for primetime?J Trauma. 2006;60:925–9. doi: 10.1097/01.ta.0000197479.28714.62. [DOI] [PubMed] [Google Scholar]
- 13.Dietz RR, Davis WL, Harnsberger HR, Jacobs JM, Blatter DD. MR imaging and MR angiography in the evaluation of pulsatile tinnitus. AJNR Am J Neuroradiol. 1994;15:879–89. [PMC free article] [PubMed] [Google Scholar]
- 14.Peng CW, Chou BT, Bendo JA, Spivak JM. Vertebral artery injury in cervical spine surgery:Anatomical considerations, management, and preventive measures. Spine J. 2009;9:70–6. doi: 10.1016/j.spinee.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Daentzer D, Deinsberger W, Böker DK. Vertebral artery complications in anterior approaches to the cervical spine:Report of two cases and review of literature. Surg Neurol. 2003;59:300–9. doi: 10.1016/s0090-3019(03)00113-7. [DOI] [PubMed] [Google Scholar]
- 16.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976) 2000;25:962–9. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 17.Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation:Results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998;88:634–40. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]
- 18.Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. Am J Roentgenol. 1988;150:405–12. doi: 10.2214/ajr.150.2.405. [DOI] [PubMed] [Google Scholar]
- 19.O'Shaughnessy BA, Bendok BR, Parkinson RJ, Shaibani A, Batjer HH. Transarterial coil embolization of a high-flow vertebrojugular fistula due to penetrating craniocervical trauma:Case report. Surg Neurol. 2005;64:335–40. doi: 10.1016/j.surneu.2004.11.010. [DOI] [PubMed] [Google Scholar]


