Abstract
BACKGROUND:
Lab-based simulators can help to reduce variability in prosthetics research. However, they have not yet been used to investigate the effects of sweating at the residuum-liner interface. This work sought to create and validate a simulator to replicate the mechanics of residual limb perspiration. The developed apparatus was used to assess the effects of perspiration and different liner designs.
METHODOLOGY:
By scanning a cast, an artificial residuum was manufactured using a 3D-printed, transtibial bone model encased in silicone, moulded with pores. The pores allowed water to emit from the residuum surface, simulating sweating. Dry and sweating cyclic tests were performed by applying compressive and tensile loading, while measuring the displacement of the residuum relative to the socket. Tests were conducted using standard and perforated liners.
FINDINGS:
Although maximum displacement varied between test setups, its variance was low (coefficient of variation <1%) and consistent between dry tests. For unperforated liners, sweating increased the standard deviation of maximum displacement approximately threefold (0.04mm v 0.12mm, p<0.001). However, with the perforated liner, sweating had little effect on standard deviation compared to dry tests (0.04mm v 0.04mm, p=0.497).
CONCLUSIONS:
The test apparatus was effective at simulating the effect of perspiration at the residual limb. Moisture at the skin-liner interface can lead to inconsistent mechanics. Perforated liners help to remove sweat from the skin-liner interface, thereby mitigating these effects.
Keywords: Sweating, Residual limb, Socket interface, Simulator, Lower limb prosthetics, Amputation
INTRODUCTION
Excessive sweating commonly affects lower limb amputees1 and impacts their daily life.2 Increased energy expenditure during everyday activities compared to able-bodied people3 and reduced skin surface area4 for cooling both contribute to this issue. Prosthetic liners worn on the residuum can also amplify sweating at the residuum-liner interface, as they have poor thermal conductivity5 and little permeability.6
The socket and residual limb are often considered a single entity with a rigid connection. However, in practice, there is relative movement at this interface,7,8 which sweating can worsen, affecting prosthetic suspension.9
Technologies have been developed to regulate residuum temperature or manage perspiration.10–13 One such technology uses perforations in the liner to allow sweat to transfer away from the skin. Previous evaluations of this technology have reported higher scores in patient-reported outcome measures,13 fewer skin health problems12,13 and a noticeable reduction in the perspiration on the limb.12,13
Due to the inherent heterogeneity and variability of amputees,14 some researchers have emulated the residual limb using simulators and test machines, in lieu of human participants.15,16 These can recreate realistic interface mechanics in prosthetic sockets,17–20 in a highly reproducible and repeatable manner. These methods have not yet been used to examine effects of perspiration at the residuum-liner interface.
Objectives
This research sought to achieve the following objectives; design, construct and evaluate a test apparatus to recreate the impact of sweat at the residuum-liner interface, identify how displacement during loading is affected by the presence of moisture, and evaluate the efficacy of a liner designed for perspiration management.
METHODOLOGY
Manufacture
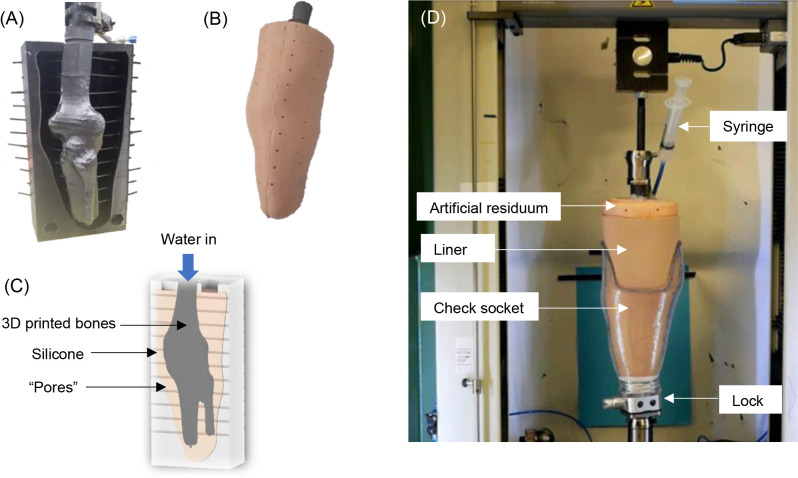
This research followed a similar artificial residuum manufacturing method to McGrath et al.17 A transtibial residuum cast was scanned and a pin-lock check socket was created. A transtibial bone model of an extended knee was also scanned so that the bones and residuum could be scaled in size to match one another. The scaled bone model and two halves of a negative residuum mould were created using additive manufacture. The soft tissue was simulated by moulding silicone (Smooth-On, Inc., PA, USA; density = 1.08 g/cm3) around the bone model.
During moulding, 3mm diameter plastic straws were used to create pores in the silicone, evenly spaced along the length and around the circumference, with one at the distal end (Figure 1A). The 3mm diameter was the minimum that could be consistently 3D printed.
Figure 1:
(A) The 3D printed bones held in place in the negative residuum mould with 3mm straws to create “pores” (B) the moulded silicone artificial residuum with pores visible along its surface (C) an annotated cross-section diagram of the artificial residuum (D) the artificial residuum set up on the test machine.
Water was applied, via a syringe and rubber tubing, into the proximal opening between silicone and bone. Once in the central canal, applying compression forced the water through the pores to the outer surface. The proximal hole was sealed with the rubber tubing in place, using a silicone adhesive. The residuum and its cross-section are shown in Figures 1B and 1C, respectively. A female pyramid tube adaptor was fixed to the proximal end of the bone model allowing rigid attachment to a universal test machine (LR10K Plusi, Lloyd Instruments, UK – Figure 1D).
Protocol
The residuum was fitted with a pin-lock liner (Comfort linerii, Blatchford Ltd, UK) and attached to the check socket. Since this simulator sought to mimic both stance and swing phase, for simplicity, it was vertically-oriented on the test machine (Figure 1D).
Tests were load controlled. A single cycle increased to a maximum 800N compression, reversed to a maximum 100N tension, then returned to 0N. 800N is a typical maximum force applied by an adult of approximately 70-80kg during walking.21 100N is a liberal estimate of the combined peak gravitational and centripetal forces on the limb during swing phase.
The outcome measurement was displacement, recorded by the actuator of the test machine. The measurement was zeroed before any compression occurred, so the output reflected the change in displacement of the proximal attachment of the residual limb, from its initial position, due to the loading pattern.
For sweating tests, 20ml of water was added, based on an approximation calculated from reported amputee sweating rates22 and the residuum surface area. Following each sweating test, the liner was removed to note the quantity of water remaining inside and the residuum was heated for eight hours in an oven at 40°C to ensure the evaporation of any residual water. The order of testing for dry and sweating tests was randomised.
Repeatability
Tests were 50 seconds long, performing 50 cycles at a frequency of 1Hz to simulate a 120 steps per minute walking cadence. Of typical walking bouts, 75% consist of fewer than 40 steps and 60% last under 30 seconds,23 so each simulator test would represent the majority of these bouts.
Reproducibility
It was possible that deconstruction/reassembly of the setup would create differences in the exact fit of the liner on the residuum or the residuum in the socket. This replicates the real-world conditions of doffing and donning a prosthesis day-to-day. Three dry tests of 50 cycles each were performed and the simulator was deconstructed and reconstructed between tests, to quantify this effect.
Liners
The protocol was used to evaluate perforated liners (Silcare Breathe Lockingiii, Blatchford Ltd, UK). These liners have perforations along the length (columns of 150), circumference (eight columns) and at the distal end (60) to allow sweat removal. The perforated and unperforated liners were made with the same silicone, the same fabric (polyamide and lycra) and the same thickness profile (7mm distally, 2.9mm proximally), so the only difference was the perforations. The order of liner testing was random.
Data processing
The first five recorded cycles of each test were excluded from data analysis to account for any human error during setup e.g. the pin ratcheting further into the lock. The remaining 45 cycles were checked to ensure at least 780N compression. Displacement values were compared between tests by magnitude (mean values) and variability (standard deviation (SD), coefficient of variation (CV)). Shapiro-Wilk tests evaluated data normality. The Brown-Forsythe test for homogeneity of variance determined whether datasets had equal variances. This test was chosen for its robustness with non-normal distributions. For normal data, t-tests compared mean displacements. For non-parametric data, Wilcoxon tests were used if group variances were homogenous, otherwise Kruskal-Wallis tests were employed. Statistical significance was defined as p≤0.05.
RESULTS
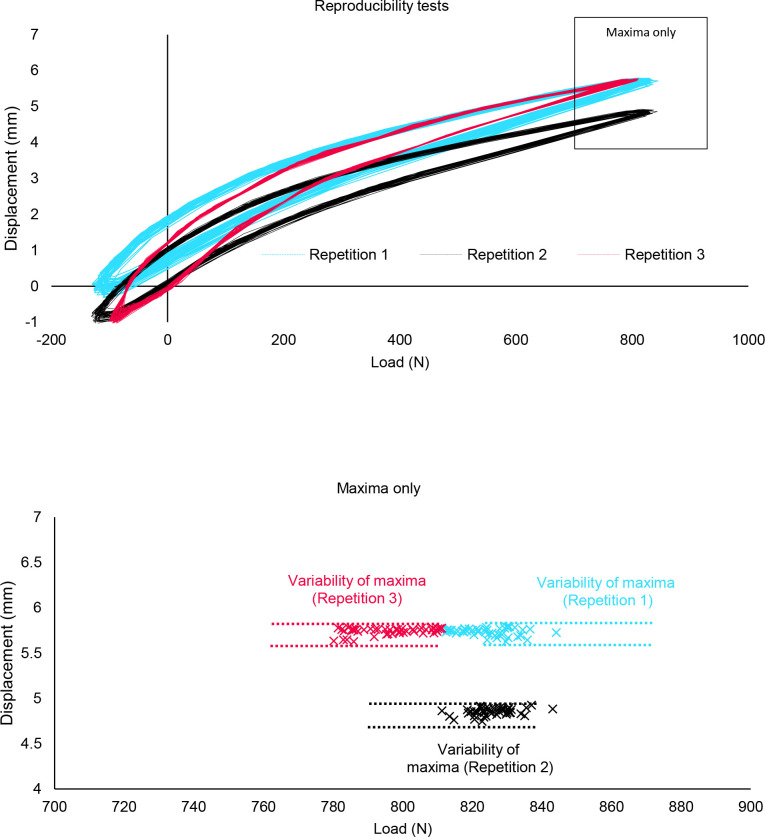
Reproducibility
Hysteresis curves for the three reproducibility tests are shown in Figure 2. Measurements showed that absolute displacement was sensitive to the simulator setup. Maximum values for each repetition (mean±SD; 5.73±0.04mm, 4.85±0.04mm, 5.78±0.04mm, respectively) showed a statistically significant difference (p<0.001). Minimum values for each test (-0.07±0.13mm, -0.86±0.10 mm, -0.95±0.06mm, respectively) also showed a statistically significant difference (p<0.001).
Figure 2:
(Top) The displacement v load curves for the three reproducibility tests. Positive load and displacement indicate compression, negative load and displacement indicate tension. N.B. Not all curves pass through the origin due to the exclusion of the first five cycles. (Bottom) The maximum displacements of each of the cycles, for each reproducibility test. The variability of these maxima, within each test, is annotated.
Repeatability
The CVs for maximum displacements were 0.7%, 0.8% and 0.6% for Repetitions 1, 2 and 3, respectively. The Brown-Forsythe test indicated no significant difference in the variances of these tests (p=0.42). Variability of maximum displacement was chosen to compare between further tests.
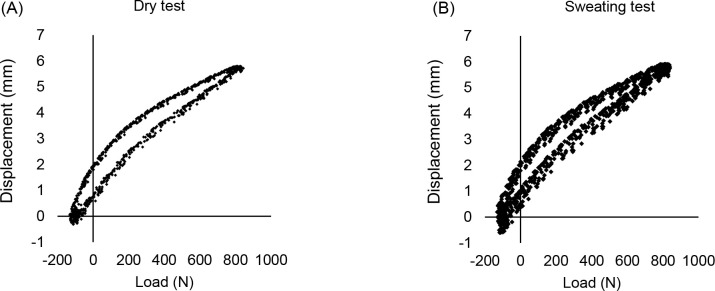
Sweating
Figure 3A and 3B show the hysteresis curves of a dry test and a sweating test for a standard liner. Maximum displacement increased with each cycle of the sweating test. The SD of maximum displacement of the sweating test (0.12mm) was significantly higher than for the dry test (0.04mm, p<0.001).
Figure 3:
(A) The hysteresis curve of a dry test with the standard liner (B) the hysteresis curve of a ‘sweating’ test with the standard liner.
After the sweating test approximately 50% of the water applied was poured out from the bottom of the liner. This did not include any water that may have been remaining on the artificial residuum or in its pores.
Liners
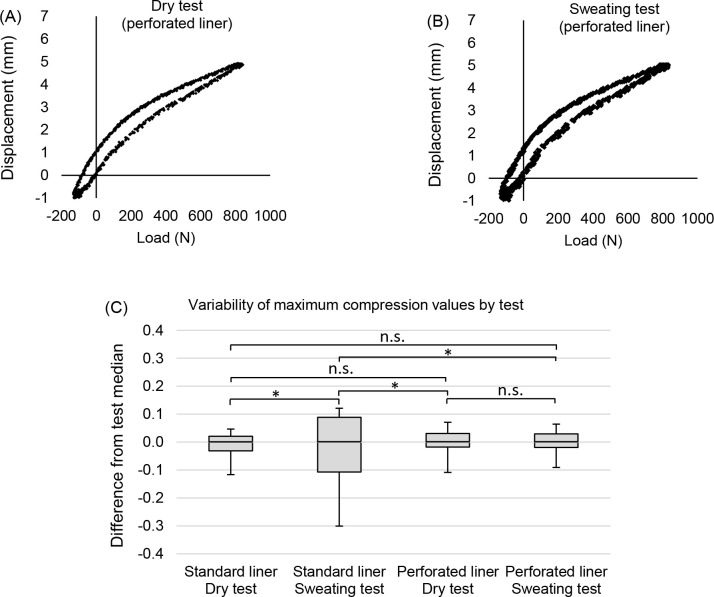
Figure 4A and 4B show the differences in hysteresis curves between a dry test and a sweating test for a perforated liner. The sweating test retained a high degree of repeatability (CV=0.7%), comparable to the dry tests. The variability of the sweating test (SD=0.04mm) and the dry test (SD=0.04mm) were not significantly different (p=0.497).
Figure 4:
(A) The hysteresis curve of a dry test with the perforated liner (B) the hysteresis curve of a sweating test with the perforated liner (C) A box-and-whisker plot of the maximum displacement values from the dry and sweating tests with the standard and perforated liners (normalised by median). The box indicates the interquartile range and the whiskers indicate the maximum and minimum values. The lines at the top of the plot show where comparisons of variability were made. Asterisks (*) indicate a significant difference (p<0.05) in variance between tests.
Figure 4C, shows the interquartile ranges for all tests, normalised by medians. The variability of the sweating test with the perforated liner (SD = 0.04mm) was significantly less than with the standard liner (SD=0.12mm, p<0.001).
After the test, the volume of water poured out from the liner was approximately 5% of the volume originally applied. This did not include any water that may have been (A) remaining on the surface of the residuum, (B) in its pores, (C) absorbed by the outer liner fabric, or (D) expelled from the socket at the distal end, via the lock, which could not be accurately quantified.
DISCUSSION
A simulator was successfully constructed to mimic the interface dynamics of a sweating residual limb. Tests demonstrated that moisture at the residuum-liner interface leads to greater variability in the displacement of the residual limb, relative to the socket, when loaded to replicate walking. When a perforated prosthetic liner was used to allow moisture to transport away from the interface, the variability of displacement was equivalent to that of dry tests, under the same walking load pattern.
For simplicity and the constraints of the test equipment, the simulator was mounted vertically on the test machine. While axial displacement is the largest in magnitude7,24 and widest-researched,20,25–28 the other five degrees-of-freedom (anterior-posterior and medial-lateral translation, as well as rotation about each of the three axes), are also likely to be affected.7,28 Regardless, the results demonstrated a sufficient mechanism to identify the influence of perspiration at the liner interface.
In terms of repeatability, the simulator had CVs<1% between strides. Even between reproducibility tests, which were statistically different, differences in maximum displacement were approximately 1mm, and therefore unlikely to be perceptible by a wearer. Consistent suspension is important with suspension method25–30 and socket fit/design31–34 affecting prosthetic performance.
The effect of sweating was illustrated in Figure 3. Variability (SD) increased approximately threefold (p<0.001); maximum displacement increasing with each progressive cycle. This movement contributes to skin damage35 and explains why sweat affects gait quality.9 A review of gait stability in non-amputees observed that inconsistent gait parameters were the strongest distinguishing factor between fallers and non-fallers,36 with similar observations reported for transtibial amputees.37
The effect of using a perforated liner was investigated (Figure 4). While variability increased 194% with the standard liner during sweating tests, there was no significant difference in variability of the dry and sweating tests with the perforated liner (p=0.497). Notably, even when sweating, the perforated liner retained the consistent mechanics of a dry interface.
Limitations
The scope of the simulator was to develop a method to distribute liquid across the residuum-liner interface. This simplified some characteristics of the residual limb, such as the size and distribution of sweat pores and the heterogeneity of the soft tissue. Nor was it designed to account for the rate of sweat production; the liquid was present from the first loading cycle. Similarly, other conditions associated with sweating (e.g. increased temperature) were not considered in the design.
There were limitations of this simplified design. By adding the liquid at the top there was no way to ensure that all of the water had been pushed to the surface. Furthermore, during the ‘sweating’ test with the perforated liner, water was observed being emitted from the perforations but was not evenly across the liner, perhaps implying that the perspiration was not distributed evenly across the residuum surface. The variable pore length due to residuum geometry and the effect of gravity likely had an impact.
Another potential limitation was the coefficient of friction (CF) between the materials used. The CF between human skin and silicone is between 0.35 and 1.16, with a mean value of 0.6138. The CF of the silicone used to create the artificial residuum is not reported by the manufacturer. However, by keeping it constant between tests, relative comparisons can be made.
An alternative might have been to perform in-vitro experiments with animal specimens. The advantages would have been closer approximations of the mechanical and frictional properties of human tissue. The drawbacks would have been losing the geometry of a residual limb in a socket and less control over the quantity of liquid at the interface.
Finally, it should be noted that these same results may not be generalizable to other liner designs. Differences in the size, profile and distribution of perforations, as well as liner profile and the external fabric may all have an effect on the efficiency of sweat removal.
CONCLUSION
In conclusion, the test apparatus was effective at simulating perspiration at the residual limb with reproducible results. Perforated liners remove perspiration from the residuum-liner interface, helping to maintain consistent mechanical behaviour. Minimising unwanted movement reduces the risk of soft tissue injury.
DECLARATION OF CONFLICTING INTERESTS
Some of the authors are full time employees of the manufacturer of the prosthetic liners evaluated in this study
AUTHOR CONTRIBUTION
Michael McGrath: Conceptualisation, manufacturer, data collection, data analysis, writing original, review and editing
KC Davies: Writing original, review and editing
Ana Gallego: Conceptualisation, manufacturer, data collection, review and editing
Piotr Laszczak: Conceptualisation, review and editing
Jinghua Tang: Review and editing
Saeed Zahedi: Review and editing
David Moser: Review and editing
SOURCES OF SUPPORT
Some of the authors are employees of Blatchford Products Ltd.
ETHICAL APPROVAL
Ethical approval was not needed for this study.
MANUFACTURERS’ DOCUMENTATION
ii) https://www.blatchfordus.com/products/comfort-liner/
iii) https://www.blatchfordus.com/products/silcare-breathe-locking-liner/
ACKNOWLEDGEMENTS
The authors wish to thank Simon Jarvis, the engineer who ran the universal test machine for the experiments in this research.
Footnotes
Canadian Prosthetics & Orthotics Journal (CPOJ) is an international peer-reviewed open-access journal established in Ottawa, Canada in 2021 (ISSN 2561-987X). CPOJ articles are licensed under the Creative Commons Attribution 4.0 United States License. https://jps.library.utoronto.ca/index.php/cpoj/ABOUT-CPOJ https://jps.library.utoronto.ca/index.php/cpoj/COPYRIGHT
All articles are permanently available online to the public without restrictions or subscription fees. All articles are free to be used, cited and distributed on condition that appropriate acknowledgement is included. Authors are the copyright holders of their original contributions.
REFERENCES
- 1.Ghoseiri K, Safari MR. Prevalence of heat and perspiration discomfort inside prostheses: Literature review. J Rehabil Res Dev. 2014;51:855. Doi: 10.1682/JRRD.2013.06.0133 [DOI] [PubMed] [Google Scholar]
- 2.Hagberg K, Brånemark R. Consequences of non-vascular transfemoral amputation: a survey of quality of life, prosthetic use and problems. Prosthet Orthot Int. 2001;25:186-94. Doi: 10.1080/03093640108726601 [DOI] [PubMed] [Google Scholar]
- 3.Gailey RS, Wenger MA, Raya M, Kirk N, Erbs K, Spyropoulos P, et al. Energy expenditure of trans-tibial amputees during ambulation at self-selected pace. Prosthet Orthot In. 1994;18:84-91. Doi: 10.3109/03093649409164389 [DOI] [PubMed] [Google Scholar]
- 4.Seymour R. Prosthetics and orthotics: lower limb and spinal. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2002 [Google Scholar]
- 5.Klute GK, Rowe GI, Mamishev AV, Ledoux WR. The thermal conductivity of prosthetic sockets and liners. Prosthet Orthot Int. 2007;31:292-9. Doi: 10.1080/03093640601042554 [DOI] [PubMed] [Google Scholar]
- 6.Hachisuka K, Matsushima Y, Ohmine S, Shitama H, Shinkoda K. Moisture permeability of the total surface bearing prosthetic socket with a silicone liner: is it superior to the patella-tendon bearing prosthetic socket? J UOEH. 2001;23:225-32. Doi: 10.7888/juoeh.23.225 [DOI] [PubMed] [Google Scholar]
- 7.Tang J, McGrath M, Laszczak P, Jiang L, Bader DL, Moser D, et al. Characterisation of dynamic couplings at lower limb residuum/socket interface using 3D motion capture. Med Eng Phys. 2015;37:1162-8. Doi: 10.1016/j.medengphy.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 8.Tang J, McGrath M, Hale N, Jiang L, Bader D, Laszczak P, et al. A combined kinematic and kinetic analysis at the residuum/socket interface of a knee-disarticulation amputee. Med Eng Phys. 2017;49:131-9. Doi: 10.1016/j.medengphy.2017.08.014 [DOI] [PubMed] [Google Scholar]
- 9.Legro MW, Reiber G, del Aguila M, Ajax MJ, Boone DA, Larsen JA, et al. Issues of importance reported by persons with lower limb amputations and prostheses. J Rehabil Res Dev. 1999;36:155-63 [PubMed] [Google Scholar]
- 10.Wernke MM, Schroeder RM, Kelley CT, Denune JA, Colvin JM. Smart Temp prosthetic liner significantly reduces residual limb temperature and perspiration. J Prosthet Orthot. 2015;27:134-9. Doi: 10.1097/JPO.0000000000000070 [DOI] [Google Scholar]
- 11.Caldwell R, Fatone S. Technique for perforating a prosthetic liner to expel sweat. J Prosthet Orthot. 2017;29:145-7. Doi: 10.1097/JPO.0000000000000136 [DOI] [Google Scholar]
- 12.McGrath M, McCarthy J, Gallego A, Kercher A, Zahedi S, Moser D. The influence of perforated prosthetic liners on residual limb wound healing: a case report. Can Prosthet Orthot J. 2019;2. Doi: 10.33137/cpoj.v2i1.32723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davies KC, McGrath M, Stenson A, Savage Z, Moser D, Zahedi S. Using perforated liners to combat the detrimental effects of excessive sweating in lower limb prosthesis users. Can Prosthet Orthot J. 2020;3. Doi: 10.33137/cpoj.v3i2.34610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steer J, Grudniewski P, Browne M, Worsley P, Sobey A, Dickinson A. Predictive prosthetic socket design part 2: personspecific concept design using multi-objective genetic algorithms. Biomech Model Mechanobiol. 2020;19:1347-1360. Doi: 10.1007/s10237-019-01258-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton M. Novel approaches to evaluating and characterizing force sensor performance at body-device interfaces. [dissertation on the Internet]. University of Toronto; 2019. [citied 2021 March 10]. Available from: http://hdl.handle.net/1807/98045 [Google Scholar]
- 16.Hamilton M, Behdinan K, Andrysek J. Evaluating the effects of load area and sensor configuration on the performance of pressure sensors at simulated body-device interfaces. IEEE Sens J. 2020. Doi: 10.1109/JSEN.2020.2970964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGrath MP, Gao J, Tang J, Laszczak P, Jiang L, Bader D, et al. Development of a residuum/socket interface simulator for lower limb prosthetics. Proc Inst Mech Eng [H]. 2017;231:235-42. Doi: 10.1177/0954411917690764 [DOI] [PubMed] [Google Scholar]
- 18.Gholizadeh H, Lemaire ED, Salekrostam R. Mechanical Evaluation of Unity Elevated Vacuum Suspension System. Can Prosthet Orthot J. 2019;2. Doi: 10.33137/cpoj.v2i2.32941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Armitage LE. Measurement of factors affecting fit at the prosthetic socket-residual limb interface in people with transtibial amputation. [dissertation on the Internet]. University of New SouthWales; 2020; [citied 2021 March 10]. Available from: https://unsworks.unsw.edu.au/fapi/datastream/unsworks:63952/SOURCE02?view=true [Google Scholar]
- 20.Wernke MM, Schroeder RM, Haynes ML, Nolt LL, Albury AW, Colvin JM. Progress toward optimizing prosthetic socket fit and suspension using elevated vacuum to promote residual limb health. Adv Wound Care. 2017;6:233-9. Doi: 10.1089/wound.2016.0719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirtley C. Clinical gait analysis: theory and practice. Elsevier Health Sciences; 2006 [Google Scholar]
- 22.Hasegawa H, Makino H, Fukuhara K, Mikami Y, Kimura H, Adachi N. Thermoregulatory responses of lower limb amputees during exercise in a hot environment. J Therm Biol. 2020;91:102609. Doi: 10.1016/j.jtherbio.2020.102609 [DOI] [PubMed] [Google Scholar]
- 23.Orendurff MS, Schoen JA, Bernatz GC, Segal AD. How humans walk: bout duration, steps per bout, and rest duration. J Rehabil Res Dev. 2008;45:1077. Doi: 10.1682/jrrd.2007.11.0197 [DOI] [PubMed] [Google Scholar]
- 24.Swanson EC, McLean JB, Allyn KJ, Redd CB, Sanders JE. Instrumented socket inserts for sensing interaction at the limbsocket interface. Med Eng Phys. 2018;51:111-8. Doi: 10.1016/j.medengphy.2017.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Darter BJ, Sinitski K, Wilken JM. Axial bone-socket displacement for persons with a traumatic transtibial amputation: The effect of elevated vacuum suspension at progressive bodyweight loads. Prosthet Orthot Int. 2016;40:552-7. Doi: 10.1177/0309364615605372 [DOI] [PubMed] [Google Scholar]
- 26.Gerschutz MJ, Hayne ML, Colvin JM, Denune JA. Dynamic Effectiveness Evaluation of Elevated Vacuum Suspension. J Prosthet Orthot. 2015;27:161-5. Doi: 10.1097/JPO.0000000000000077 [DOI] [Google Scholar]
- 27.Klute GK, Berge JS, Biggs W, Pongunumkul S, Popovic Z, Curless B. Vacuum-assisted socket suspension compared with pin suspension for lower extremity amputees: effect on fit, activity, and limb volume. Arch Phys Med Rehabil. 2011;92:1570-1575 [DOI] [PubMed] [Google Scholar]
- 28.Board WJ, Street GM, Caspers C. A comparison of trans-tibial amputee suction and vacuum socket conditions. Prosthet Orthot Int. 2001;25:202-209. Doi: 10.1080/03093640108726603 [DOI] [PubMed] [Google Scholar]
- 29.Kahle JT, Highsmith MJ. Transfemoral sockets with vacuumassisted suspension comparison of hip kinematics, socket position, contact pressure, and preference: ischial containment versus brimless. Arch Phys Med Rehabil. 2013;50:1241. DOI: 10.1682/JRRD.2013.01.0003 [DOI] [PubMed] [Google Scholar]
- 30.Brunelli S, Delussu AS, Paradisi F, Pellergrini R, Traballesi M. A comparison between the suction suspension system and the hypobaric Iceross Seal-In® X5 in transtibial amputees. Prosthet Orthot Int. 2013;37:436-44. Doi: 10.1177/0309364613476531 [DOI] [PubMed] [Google Scholar]
- 31.Yiğiter K, Şener G, Bayar K. Comparison of the effects of patellar tendon bearing and total surface bearing sockets on prosthetic fitting and rehabilitation. Prosthet Orthot Int. 2002;26:206-12. Doi: 10.1080/03093640208726649 [DOI] [PubMed] [Google Scholar]
- 32.Eshraghi A, Osman NAA, Karimi MT, Gholizadeh H, Ali S, Abas WABW. Quantitative and qualitative comparison of a new prosthetic suspension system with two existing suspension systems for lower limb amputees. Am J Phys Med Rehabil. 2012;91:1028-38. Doi: 10.1097/PHM.0b013e318269d82a [DOI] [PubMed] [Google Scholar]
- 33.Gholizadeh H, Abu Osman NA, Eshraghi A, Ali S, Wan Abas WAB, Pirouz G. Transtibial prosthetic suspension: less pistoning versus easy donning and doffing. J Rehabil Res Dev. 2012;49:1321-30. Doi: 10.1682/jrrd.2011.11.0221 [DOI] [PubMed] [Google Scholar]
- 34.Convery P, Murray K. Ultrasound study of the motion of the residual femur within a trans-femoral socket during gait. Prosthet Orthot Int. 2000;24:226-32. Doi: 10.1080/03093640008726552 [DOI] [PubMed] [Google Scholar]
- 35.Dudek NL, Marks MB, Marshall SC, Chardon JP. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehabil. 2005;86:659-63. Doi: 10.1016/j.apmr.2004.09.003 [DOI] [PubMed] [Google Scholar]
- 36.Hamacher D, Singh N, Van Dieen J, Heller M, Taylor W. Kinematic measures for assessing gait stability in elderly individuals: a systematic review. J R Soc Interface. 2011;8:1682-98. Doi: 10.1098/rsif.2011.0416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hordacre BG, Barr C, Patritti BL, Crotty M. Assessing gait variability in transtibial amputee fallers based on spatial-temporal gait parameters normalized for walking speed. Arch Phys Med Rehabil. 2015;96:1162-5. Doi: 10.1016/j.apmr.2014.11.015 [DOI] [PubMed] [Google Scholar]
- 38.Zhang M, Mak A. In vivo friction properties of human skin. Prosthet Orthot Int. 1999;23:135-41. Doi: 10.3109/03093649909071625 [DOI] [PubMed] [Google Scholar]