Abstract
CASE DESCRIPTION:
Good residual limb skin health is vital to successful prosthetic prescription. Unnatural loading profiles and excessive sweating can lead to skin and soft tissue problems. Perforated liners allow the transport of moisture away from the skin and allow negative pressure (a condition that has been shown to aid wound healing) to act directly on the residuum surface.
AIM:
Assess the effects of perforated prosthetic liner use, particularly with respect to wound healing.
METHOD:
Three patient histories were retrospectively reviewed following prescription of perforated prosthetic liners due to excessive sweating or prolonged residual limb health concerns. Photographic records from patient files were used to document changes in residual limb condition. Patients also provided subjective feedback regarding their experiences.
FINDINGS:
Two cases described active amputees with persistent blistering irritated during exercise. Another case described a patient of low mobility level with a history of residual limb skin infections. All saw their conditions heal and reported a reduction in problematic sweating. Two patients reported cancelling surgical interventions after substantial improvements with the perforated liner.
DISCUSSION:
These findings provide evidence that the use of perforated prosthetic liners allow improvements in residual limb health, while still permitting prosthetic use.
Keywords: Perforated Liner, Residual Limb, Wound Healing, Sweating, Vacuum, Lower Limb Prosthetics
INTRODUCTION
The interface between the residual limb and the prosthetic socket is, arguably, the most crucial part of successful prosthetic prescription.1 Without a comfortably fitting socket, the patient will not wear their prosthesis.
The skin and soft tissue of the residual limb are particularly susceptible to damage. Contrary to historic biomechanical assumptions, there is evidence to suggest that this interface should be considered as an extra joint in the lower limb, with translation and rotation,2,3 which lead to unnatural loading profiles. There may also be scar tissue and, if the amputation aetiology was dysvascular, the tissue is at greater risk of pressure ulcers,4 which cannot heal as well5 and could result in revision surgery or reamputation.6
Another issue that exacerbates the problem is excessive sweating.1,7–10 When questioned about the factors affecting their quality of life and their satisfaction with their prostheses, up 70% of lower limb amputees have reported that they consider sweating a problem7,11 and up to two-thirds claim that sweating adversely affects their activities of daily living (ADL).12
The causes of excessive sweating in amputees are clear. It has been reported that trans-tibial amputees use 10-40% more energy than able-bodied people to walk and perform daily tasks.13,14 They also have a reduced surface area (approximately 10-15% less), which affects the capacity to transfer heat energy and cool down.15 Consequently, the body’s natural response is to produce more perspiration. Furthermore, the use of prosthetic liners, made of silicone, polyurethane or TPE gel, creates an even warmer environment locally, around the residual limb because they often have poor thermal conductivity.16,17 This impermeable18 micro-climate is moist, warm and nutrientrich, making it ideal for bacterial growth. The sweat is stasis on the residuum surface instead of evaporating, which can lead to skin problems, such as dermatitis.19–21
There is evidence that liner material selection can reduce residuum temperatures,22 such as the Alpha SmartTemp liner (WillowWood, Roseburg, OR, USA), which uses Phase Change Material that stores and releases heat energy. However, it is unknown whether this is sufficient to reduce thermal discomfort.23 Regardless, even if sweating is reduced, what perspiration does occur will remain on the skin, so associated problems remain. In light of this, “breathable” prosthetic liners have been developed, which have permeable surfaces to allow the transfer of air and moisture away from the skin, such as Silcare Breathe (Blatchford, Basingstoke, UK) with laser-drilled perforations and SoftSkin Air (Uniprox, Zeulenroda-Triebes, Germany) with micro-pores. This report describes cases of patients with residual limb health conditions who were fitted with perforated liners.
METHODOLOGY
Participants
The case histories in this study were collected retrospectively. Once relevant cases were identified, the patients were approached and they were asked to provide written consent for their case to be described. The inclusion criteria included being over the age of 18, being able to provide informed consent, having a trans-tibial amputation, being a prosthetic limb wearer, having a history of residual limb health issues and having changed to a perforated prosthetic liner.
Perforated liners
There were two types of perforated prosthetic liner used in these cases; one (Silcare Breathe Cushion,a Blatchford, UK) used with elevated vacuum suspension (EVS) or a passive vacuum and the other (Silcare Breathe Locking,b Blatchford, UK) used with a pin-lock. The ‘cushion’ version has a rounded distal cap and is used in conjunction with a suspension sleeve. A distal one-way valve in the socket allows the use of suction suspension or EVS. Laser-drilled perforations are distributed along the length of the liner. There are also perforations in the distal cap. On the pin-lock version, the perforations stop a short distance from the distal end. At the distal cap, a valve opens when the wearer bears load and closes again when the limb is lifted from the ground, creating a small area of passive vacuum in the area distal to the perforations in the wall of the liner, which facilitates the retention of the residuum within the liner.
Data collected
Demographic data were collected from the patients in each case. These included gender, age, K level and any relevant comorbidities. Their prosthetists were asked to describe the patients’ prosthetic prescription, including suspension and ankle/foot technologies, before and after they were fitted with the perforated liner, to identify any potentially compounding factors for consideration.
Photographic evidence of residual limb health conditions was gathered to verify the clinicians’ own patient notes. Since the analysis was performed retrospectively, photos were only available when the clinician, or the amputee themselves, had seen fit to take one. These images were used for a qualitative examination of changes in residual limb health.
FINDINGS
Three case histories were collected, covering different demographics, prosthetic preferences and residual limb health issues. Since the analysis was retrospective and gathered from different centres, the detail included in the patient records was variable between cases (Table 1).
Table 1:
Summary table of the cases described
| Case | Age (years) | Mass (kg) | BMI | K level | Amputation type/side | Residual limb issue | Previous prescription | New prescription |
|---|---|---|---|---|---|---|---|---|
| #1 | 41 | 90 | 28.4 | K3-K4 | Trans-tibial /Right | Distal blisters around scarring | Cushion silicone liner with suction suspension | Pin-lock perforated liner |
| #2 | 45 | 100 | 30.2 | K3-K4 | Trans-tibial /Right | Posterior ulcer/wound | Pin-lock silicone liner with BladeXT foot | 1st: Pin-lock perforated liner |
| 2nd: Cushion perforated liner with suction suspension | ||||||||
| #3 | 50 | 106 | 31.0 | K2-low K3 | Trans-tibial /Right | Distal maceration and infection | Cushion silicone liner with suction suspension and Tres foot | Cushion perforated liner with EVS and K2-specific hydraulic ankle |
Case #1
The patient was a 41-year-old male with a right-sided, trans-tibial amputation caused by a road traffic collision approximately four years prior. He was 90kg in mass, with a body mass index (BMI) of 28.4 and he had been classified as a K3-K4 level walker.
Following limb loss, the patient wished to return to his previously active lifestyle, including regular jogging, walking and cycling. However, exercise, combined with his silicone liner had led to excessive perspiration building up, remaining on the surface of his residuum and collecting distally. The patient reported that this caused relative movement between the residuum and the liner and chaffing. Blisters would develop in and around the scars at the distal end of his residuum, where sweat collected (Figure 1a). Jogging on consecutive days led to prosthetic disuse on the third day because the blisters made limb wearing too painful.
Figure 1:

The condition of the Case #1 patient’s residual limb (a) before being fitted with a perforated liner and (b) after three months of use.
In fact, the patient had booked a surgery to revise the scarring at the distal end of his residuum, in the hope that it would help to reduce blister formation. As a result of sweating issues, the patient was fitted with a locking, perforated liner on 19th June 2017. It was believed that he would prefer the pin-lock version because it removed the necessity to wear a suspension sleeve. At initial fitting, the patient reported finding the liner comfortable to wear and easy to don.
A follow-up appointment was carried out after a month on 24th July 2017. The patient reported that the liner remained comfortable, with good prosthetic control. He had continued jogging and walking and although he felt that his limb felt about the same temperature, there had been considerably less sweat on his limb after doffing the liner, which he described as only a “slight glisten” on the skin. His prosthetist reported no skin breakdown and improvements in the existing blistering had led the patient to postpone his surgery. There was a review appointment after three months in September 2017, at which time the patient was regularly going for 8km jogs, the blistering had healed (Figure 1b) and he had cancelled the surgery.
Case #2
The patient was a 45-year-old male with a right-sided, traumatic, trans-tibial amputation. He was 100kg in mass, with a BMI of 30.2 and he had been classified as a K3-K4 level walker.
Prior to and since his amputation, the patient enjoyed competing in motocross endurance races. For these competitions, he would wear a carbon blade-style prosthesis with a sole plate and pin-lock silicone liner. However, he struggled with excessive sweating on his residual limb and had skin issues since 2014. An ulcer developed on the posterior-distal aspect of his residuum (Figure 2a) and it worsened to the extent that his doctor had mentioned the possibility of further amputation to a trans-femoral level. The ulcer had persisted for over a year before he was initially fitted with a locking, perforated liner on 27th August 2018 (Figure 2b). In that time the patient used “no medicine, no cream, no lotion” and was advised to use “only soap and water” to clean the wound. When asked what the dermatology clinic advised him, the patient explained “they said the white heavy skin that look like a callous around the wound (Figure 2b), was from moisture. They told me I would have to take my leg off for 3 to 5 months for it to completely heal”, which was impractical for him as he was in full-time employment.
Figure 2:

The condition of the Case #2 patient’s residual limb (a) approximately one year before being fitted with a perforated liner, (b) at the point of fitting, and after (c) 4 weeks of use, (d) 7 weeks of use (the point of changing to passive vacuum suspension), (e) 9 weeks of use, (f) 11 weeks of use and (g) 13 weeks of use.
The residual limb condition was monitored at regular intervals over the first three months of perforated liner use at 4, 7, 9, 11 and 13 weeks. When compared to the initial fitting stage (Figure 2b), at 4 weeks (24th September 2018 - Figure 2c), the ulcer had visibly reduced in size and the wound was no longer suppurating. At 7 weeks (15th October 2018 - Figure 2d), Tissue was granulating and the affected area/ulcer had reduced in size. It was at this point that the patient changed to a cushion, perforated liner and Northene socket, copolymer polypropylene frame, passive vacuum adaptive expulsion valve system. Over the following 6 weeks, the ulcer reduced in size considerably (1st and 12th November 2018 - Figure 2e and f), before being considered fully healed 13 weeks after initial fitting (28th November 2018 - Figure 2g).
Since healing, the patient has been fitted with a hydraulic ankle unit for use with his passive vacuum system. He has also continued to compete in motocross endurance events (for which he uses the locking perforated liner), achieving ‘top 5’ finishes against able-bodied competitors.
Case #3
The patient was a 50-year-old male (mass: 106kg, BMI: 31.0), with a right-sided, trans-tibial amputation, classified as a K2 to low K3 level walker. He habitually wore an energy-storing-and-return (ESAR) foot.
The patient had chronic residual limb skin issues for approximately eight years. Excessive perspiration had led to the skin becoming macerated and infected (Figure 3a and b). The patient had reported “being on the brink of revision surgery” to remove the affected skin.
Figure 3:
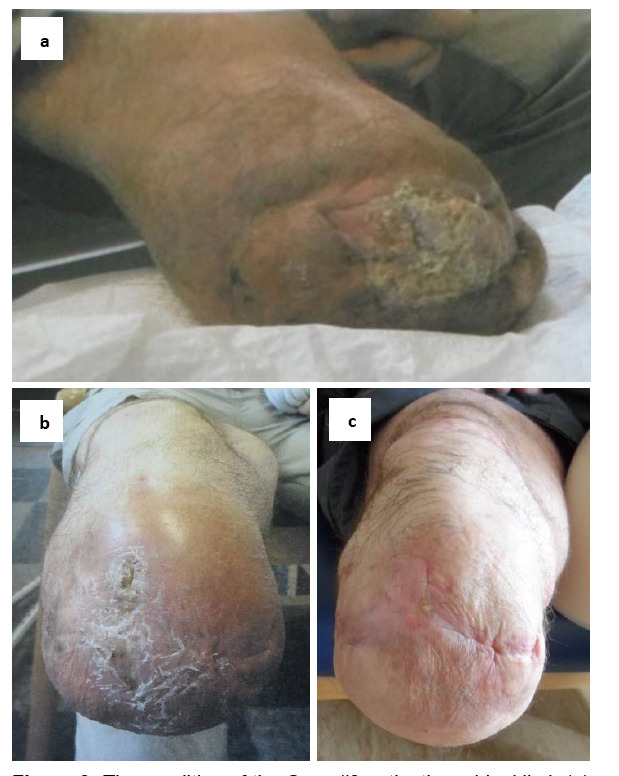
The condition of the Case #3 patient’s residual limb (a) in its worst condition in 2011, (b) in 2013 and (c) in March 2019, after continued use of a perforated liner (since 2016) with elevated vacuum suspension and hydraulic ankle (since August 2017).
He was fitted with a perforated cushion liner, in conjunction with a passive vacuum, in 2016. In 2017 this was upgraded to an EVS system that used the movement of a hydraulic ankle unit to draw greater vacuum levels. After three months of using this prosthetic prescription, the patient reported that he thought it was “doing a great job” of keeping his skin dry; he was wound free and had had no residuum problems. The patient has continued to use this prescription for over a year, during which time his residuum remains in good health (Figure 3c).
DISCUSSION
This research illustrates the health benefits of maintaining a dry residuum/socket interface by the use of perforated liners. While the use of silicone liners is primarily for comfort and impact absorption, providing a close fit and suspension,10 they can create warm, moist environments in which bacteria can thrive. Creating a dry environment mitigates against the risks of skin maceration and infection. Such conditions lead to uncomfortable socket fits and prosthetic abandonment. Also, intuitively, the presence of sweat will lubricate this interface, increasing relative motion between the residuum and the liner. This may affect prosthetic control and/or suspension, potentially reducing swing clearance and become a tripping hazard. Subsequent compensatory movements to improve clearance increase energy expenditure24 and may have a degenerative effect on musculoskeletal health.25–27
In their review of prosthesis thermal discomfort in 2014, Ghoseiri and Safari10 described available options for management of excessive heat and perspiration in the prosthetic socket. They refer to antiperspirants, local ointments and topical sprays to inhibit the physiological process of sweating but cite unpleasant odors and potential allergies as drawbacks.10 An alternative is the use of Botulinum Toxin (Botox) injections but this is described as invasive, requiring repeated treatment to maintain effectiveness and may potentially cause pain and/or side effects10 They ultimately concluded that prosthesis thermal discomfort was still an unresolved problem. Notably, this review was published prior to the commercialisation of perforated prosthetic liners.
The wounds arising from sweating can also have a substantial impact on the economics of healthcare. Treatment and care of patients with skin health conditions, such as pressure ulcers and chronic wounds, cost the UK National Health Service (NHS) up to £3.1 billion per annum.28,29 Although this number is for the population as a whole, amputees will be disproportionately affected, particularly those with vascular comorbidities. These issues can lead to socket adjustments or replacements, which studies have shown constitute a sizeable proportion of clinical appointments,30,31 creating a time and financial burden for limb centres. Additionally, two cases in this analysis reported considering surgical interventions as a result of their skin conditions, which were cancelled after tissue improvements following the use of perforated liners. Other reported treatments to reduce excessive sweating, such as Botox injections32 or daily antiperspirant use,32 can be expensive, inconvenient, produce side effects or have limited effectiveness. If a change in prosthetic liner prescription can provide the desired effect, it may be the most cost-effective approach.
As far as the authors are aware, this is the first published evidence for the effects of “breathable” liners. Some practitioners may be concerned that the perforations in liners may create areas of stress concentration that may increase the rate of deterioration of the liner itself or damage the surrounding skin. Many liner manufacturers offer warranty periods of between six and 12 months, or three months for suspension sleeves. Perforated liners have a six month warranty so although there may be a greater risk of degradation than a non-perforated liner, the longevity is still within typical industry standards for this type of prosthetic component. Although none of these three cases reported any skin issues around the perforations, the manufacturer’s Instructions For Usec warn that “enlarged perforations can trap the skin and cause blisters” and recommend that should the perforations become damaged, the patient should cease the use of the liner.
It should be noted that there might have been other influences present in these cases. Although Cases #1 and #3 didn’t report the use of other wound healing treatments, such as creams or ointments, it is possible that the patients might have used these therapies without reporting such to a member of their treatment team. Han and Ceilley’s33 review of chronic wounds describes many topical therapies and dressings that could assist wound healing but the practicality of these treatments within a prosthetic socket environment is unclear. One of the patients also began using EVS with their perforated liner. EVS has previously been shown to reduce residuum volume fluctuation34–38 and relative movement,34,37,39,40 which reduces interface pressure.41 This, combined with encouraging healthier, more hydrated, more oxygenated tissue,42 might explain why residual limb wounds have been observed to heal faster with EVS,43 without discontinuing prosthetic use.44–46 Negative pressure wound therapy (NPWT) is a widely used technique to aid wound healing47,48 and has been demonstrated to be effective even for diabetic amputees.49 The perforations in the liner allowed the vacuum to be applied directly to the wound surface, potentially further helping healing.
Two of the cases began using hydraulic ankles with their perforated liners. These devices significantly reduce interface pressures, loading rates and deep tissue trauma,50 which may also have contributed to improvements in residual limb condition.
The current study was also limited in that the analysis was performed retrospectively, each clinical team had their own methods of monitoring the patients’ skin conditions and there were other prescription changes that may have influenced wound healing (e.g. prosthetic suspension method). Future work will consist of a more regimented, scientifically rigorous analysis with a wider cohort of patients. Patients will be divided into two groups; the control group will use regular silicone liners and the intervention group will use perforated liners. Patients will be monitored at pre-defined, regular intervals. The progress of wound healing will be quantified, using metrics such as wound surface area, as described in Hoskins’ work.46 Compounding factors, such as prosthetic componentry and suspension method will be controlled to isolate the effects of liner perforations only.
DECLARATION OF CONFLICTING INTERESTS
The authors are full time employees of the manufacturer of the prosthetic liners evaluated in this study.
SOURCES OF SUPPORT
Blatchford Clinical Services who documented and provided patient care.
AUTHOR CONTRIBUTION
-
Michael McGrath,
Conceptualization, case collation, writing original, review and editing.
-
Joseph McCarthy,
Conceptualization, case collection, analysis, writing original, review and editing.
-
Ana Gallego,
Analysis, writing original, review and editing.
-
Alan Kercher,
Conceptualization, case collection, analysis, review and editing.
-
Saeed Zahedi,
Analysis, writing original, review and editing.
-
David Moser,
Analysis, writing original, review and editing.
MANUFACTURERS’ DOCUMENTATION
a https://www.blatchford.co.uk/endolite/silcare-breathe-cushion-liner/
b https://www.blatchford.co.uk/endolite/silcare-breathe-locking-liner/
ACKNOWLEDGEMENTS
The authors would like to thank the prosthetists and patients involved in providing the information for the cases in this study.
Footnotes
Canadian Prosthetics & Orthotics Journal (CPOJ) is an international peer-reviewed open-access journal established in Ottawa, Canada in 2019 (ISSN 2561-987X). CPOJ articles are licensed under the Creative Commons Attribution 4.0 United States License. https://jps.library.utoronto.ca/index.php/cpoj/ABOUT-CPOJ https://jps.library.utoronto.ca/index.php/cpoj/COPYRIGHT
All articles are permanently available online to the public without restrictions or subscription fees. All articles are free to be used, cited and distributed on condition that appropriate acknowledgement is included. Authors are the copyright holders of their original contributions.
REFERENCES
- 1.Legro MW, Reiber G, del Aguila M, Ajax MJ, Boone DA, Larsen JA, et al. Issues of importance reported by persons with lower limb amputations and prostheses. J Rehabil Res Dev. 1999; 36(3):155–163. [PubMed] [Google Scholar]
- 2.Tang J, McGrath M, Laszczak P, Jiang L, Bader DL,Moser D,Zahedi S. Characterisation of dynamic couplings at lower limb residuum/socket interface using 3D motion capture. Med Eng Phys. 2015;37(12):1162–1168. 10.1016/j.medengphy.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 3.Tang J, McGrath M, Hale N, Jiang L, Bader D,Laszczak P, et al. A combined kinematic and kinetic analysis at the residuum/socket interface of a knee-disarticulation amputee. Med Eng Phys. 2017;49:131–139. 10.1016/j.medengphy.2017.08.014 [DOI] [PubMed] [Google Scholar]
- 4.Gary Sibbald R, Woo KY. The biology of chronic foot ulcers in persons with diabetes. Diabetes-Metab Res. 2008. May;24(S1):S25–30. 10.1002/dmrr.847 [DOI] [PubMed] [Google Scholar]
- 5.Greenhalgh DG. Wound healing and diabetes mellitus. Clin Plast Surg 2003; 30: 37–45. DOI: 10.1016/S0094-1298(02)00066-4 [DOI] [PubMed] [Google Scholar]
- 6.Dillingham TR, Pezzin LE, Shore AD. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch Phys Med Rehab. 2005; 86(3):480–6. 10.1016/j.apmr.2004.06.072 [DOI] [PubMed] [Google Scholar]
- 7.Hagberg K, Brånemark R. Consequences of non- vascular trans-femoral amputation: A survey of quality of life, prosthetic use and problems. Prosthet Orthot Int. 2001; 25(3):186–94. DOI: 10.1080/03093640108726601 [DOI] [PubMed] [Google Scholar]
- 8.Hachisuka K, Nakamura T, Ohmine S, Shitama H, Shinkoda K. Hygiene problems of residual limb and silicone liners in transtibial amputees wearing the total surface bearing socket. Arch Phys Med Rehab. 2001;82(9):1286–1290. 10.1053/apmr.2001.25154 [DOI] [PubMed] [Google Scholar]
- 9.Meulenbelt HE, Geertzen JH, Jonkman MF, Dijkstra PU. Determinants of skin problems of the stump in lower-limb amputees. Arch Phys Med Rehabil. 2009; 90: 74–81. 10.1016/j.apmr.2008.07.015 [DOI] [PubMed] [Google Scholar]
- 10.Ghoseiri K, Safari MR. Prevalence of heat and perspiration discomfort inside prostheses: Literature review. J Rehabil Res Dev. 2014; 51: 855. DOI: 10.1682/JRRD.2013.06.0133 [DOI] [PubMed] [Google Scholar]
- 11.Berke GM, Fergason J, Milani JR, Hattingh J, McDowell M, Nguyen V, et al. Comparison of satisfaction with current prosthetic care in veterans and servicemembers from Vietnam and OIF/OEF conflicts with major traumatic limb loss. J Rehabil Res Dev. 2010; 47(3). DOI: 10.1682/JRRD.2009.12.0193 [DOI] [PubMed] [Google Scholar]
- 12.Hansen C, Godfrey B, Wixom J, McFadden M. Incidence, severity, and impact of hyperhidrosis in people with lowerlimb amputation. J Rehabil Res Dev. 2015;52(1). 10.1682/JRRD.2014.04.0108 [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez EG. Energy expenditure in below-knee amputees: correlation with stump length. Arch Phys Med Rehabil. 1974;55:111–9. [PubMed] [Google Scholar]
- 14.Gailey RS, Wenger MA, Raya M, Kirk N, Erbs K, Spyropoulos P, et al. Energy expenditure of trans-tibial amputees during ambulation at self-selected pace. . Prosthet Orthot Int. 1994;18(2):84–91. DOI: 10.3109/03093649409164389 [DOI] [PubMed] [Google Scholar]
- 15.Seymour R. Prosthetics and Orthotics: Lower Limb and Spinal. Philadelphia, PA, USA: Lippincott Williams & Wilkins, 2002. [Google Scholar]
- 16.Klute GK, Rowe GI, Mamishev AV, Ledoux WR. The thermal conductivity of prosthetic sockets and liners. Prosthet Orthot Int. 2007;31(3):292–299. 10.1080/03093640601042554 [DOI] [PubMed] [Google Scholar]
- 17.Webber CM, Klittich MR, Dhinojwala A, Davis BL. Thermal conductivities of commercially available prosthetic materials. J Prosthet Orthot. 2014; 26(4):212–5. DOI: 10.1097/JPO.0000000000000043 [DOI] [Google Scholar]
- 18.Hachisuka K, MATSUSHIMA Y, OHMINE S, SHITAMA H, SHINKODA K. Moisture permeability of the total surface bearing prosthetic socket with a silicone liner: is it superior to the patella-tendon bearing prosthetic socket?. J. UOEH. 2001;23(3):225–32. 10.7888/juoeh.23.225 [DOI] [PubMed] [Google Scholar]
- 19.Lake C, Supan TJ. The Incidence of Dermatological Problems in the Silicone Suspension Sleeve User. J Prosthet Orthot. 1997; 9: 97–106. [Google Scholar]
- 20.Meulenbelt HE, Geertzen JH, Dijkstra PU, Jonkman MF. Skin problems in lower limb amputees: an overview by case reports. J Eur Acad Dermatol Venereol. 2007;21(2):147–55. 10.1111/j.1468-3083.2006.01936.x [DOI] [PubMed] [Google Scholar]
- 21.Almassi F, Emadi N, Mousavi B, Masumi M, Souroush MR. Dermatosis contributing factors in bilateral lower limb war-amputees. Pak J Biol Sc. 2010;13(2):78–82. DOI: 10.3923/pjbs.2010.78.82 [DOI] [PubMed] [Google Scholar]
- 22.Wernke MM, Schroeder RM, Kelley CT, Denune JA, Colvin JM. SmartTemp prosthetic liner significantly reduces residual limb temperature and perspiration. J Prosthet Orthot. 2015;27(4):134–9. DOI: 10.1097/JPO.0000000000000070 [DOI] [Google Scholar]
- 23.Williams RJ, Washington ED, Miodownik M, Holloway C. The effect of liner design and materials selection on prosthesis interface heat dissipation. Prosthet Orthot Int. 2018;42(3): 275–279. 10.1177/0309364617729923 [DOI] [PubMed] [Google Scholar]
- 24.Su PF, Gard SA, Lipschutz RD, Kuiken TA. Gait characteristics of persons with bilateral transtibial amputations. J Rehabil Res Dev. 2007;44(4): 491–502. DOI: 10.1682/JRRD.2006.10.0135 [DOI] [PubMed] [Google Scholar]
- 25.Gailey R. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008; 45 15. DOI: 10.1682/JRRD.2006.11.0147 [DOI] [PubMed] [Google Scholar]
- 26.Lloyd CH, Stanhope SJ, Davis IS, Royer TD. Strength asymmetry and osteoarthritis risk factors in unilateral trans-tibial, amputee gait. Gait Posture. 2010;32(3):296–300. 10.1016/j.gaitpost.2010.05.003 [DOI] [PubMed] [Google Scholar]
- 27.Lemaire ED, Fisher FR. Osteoarthritis and elderly amputee gait. Arch Phys Med Rehabil. 1994; 75: 1094–1099. 10.1016/0003-9993(94)90084-1 [DOI] [PubMed] [Google Scholar]
- 28.Posnett J, Franks PJ. The costs of skin breakdown and ulceration in the UK. Skin Breakdown–the silent epidemic. Hull: The Smith and Nephew Foundation. 2007. [Google Scholar]
- 29.Posnett J, Franks P. The burden of chronic wounds in the UK. Diabetic Med 2008; 14: S7–S85. [Google Scholar]
- 30.Datta D, Vaidya SP, Alsindi Z. Analyses of prosthetic episodes in trans-tibial amputees. Prosthet Orthot Int 1999; 23: 9–12. DOI: 10.3109/03093649909071605 [DOI] [PubMed] [Google Scholar]
- 31.Nair A, Hanspal RS, Zahedi MS, Saif M, Fisher K. Analyses of prosthetic episodes in lower limb amputees. Prosthet Orthot Int. 2008;32(1):42–49. DOI: 10.1080/03093640701610615 [DOI] [PubMed] [Google Scholar]
- 32.Charrow A, DiFazio M, Foster L, Pasquina PF, Tsao JW. Intradermal botulinum toxin type A injection effectively reduces residual limb hyperhidrosis in amputees: a case series. Arch Phys Med Rehabil. 2008;89(7):1407–1409. 10.1016/j.apmr.2007.11.054 [DOI] [PubMed] [Google Scholar]
- 33.Han G, Ceilley R. Chronic wound healing: a review of current management and treatments. Adv Ther. 2017;34(3):599–610. DOI: 10.1007/s12325-017-0478-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Board WJ, Street GM, Caspers C. A comparison of trans-tibial amputee suction and vacuum socket conditions. Prosthet Orthot Int. 2001;25(3):202–9. 10.1080/03093640108726603 [DOI] [PubMed] [Google Scholar]
- 35.Goswami J, Lynn R, Street G, Harlander M. Walking in a vacuum-assisted socket shifts the stump fluid balance. Prosthet Orthot Int. 2003;27(2):107–13. DOI: 10.1080/03093640308726666 [DOI] [PubMed] [Google Scholar]
- 36.Gerschutz MJ, Denune JA, Colvin JM, Schober G. Elevated vacuum suspension influence on lower limb amputee's residual limb volume at different vacuum pressure settings. J Prosthet Orthot. 2010;22(4):252–256. DOI: 10.1097/JPO.0b013e3181f903df [DOI] [Google Scholar]
- 37.Klute GK, Berge JS, Biggs W, Pongnumkul S, Popovic Z, Curless B. Vacuum-assisted socket suspension compared with pin suspension for lower extremity amputees: effect on fit, activity, and limb volume. Arch Phys Med Rehabil. 2011;92(10):1570–1575. 10.1016/j.apmr.2011.05.019 [DOI] [PubMed] [Google Scholar]
- 38.Sanders JE, Harrison DS, Myers TR, Allyn KJ. Effects of elevated vacuum on in-socket residual limb fluid volume: Case study results using bioimpedance analysis. J Rehabil Res Dev. 2011;48(10):1231. DOI: 10.1682/JRRD.2010.11.0219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gerschutz MJ, Hayne ML, Colvin JM, Denune JA. Dynamic effectiveness evaluation of elevated vacuum suspension. J Prosthet Orthot. 2015; 27(4):161–5. DOI: 10.1097/JPO.0000000000000077 [DOI] [Google Scholar]
- 40.Darter BJ, Sinitski K, Wilken JM. Axial bone-socket displacement for persons with a traumatic transtibial amputation: The effect of elevated vacuum suspension at progressive body-weight loads. Prosthet Orthot Int 2016; 40: 552–557. 10.1177/0309364615605372 [DOI] [PubMed] [Google Scholar]
- 41.Beil TL, Street GM, Covey SJ. Interface pressures during ambulation using suction and vacuum-assisted prosthetic sockets. J Rehabil Res Dev. 2002; 39: 693. [PubMed] [Google Scholar]
- 42.Rink C, Wernke MM, Powell HM, Gynawali S, Schroeder RM, Kim JY, et al. Elevated vacuum suspension preserves residual-limb skin health in people with lower-limb amputation: Randomized clinical trial. J Rehabil Res Dev. 2016;53(6). 1121–1132. DOI: 10.1682/JRRD.2015.07.0145 [DOI] [PubMed] [Google Scholar]
- 43.Brunelli S, Averna T, Delusso M, et al. Vacuum assisted socket system in transtibial amputees: Clinical report. Orthopädie-Technik Quarterly: English Edition 2009; 2 [Google Scholar]
- 44.Traballesi M, Averna T, Delussu AS, Brunelli S. Transtibial prosthesization in large area of residual limb wound: Is it possible? A case report. Disabil Rehabil Assist Technol. 2009;4(5):373–375. 10.1080/17483100903038568 [DOI] [PubMed] [Google Scholar]
- 45.Traballesi M, Delussu AS, Fusco A, Iosa M, Averna T, Pellegrini R, et al. Residual limb wounds or ulcers heal in transtibial amputees using an active suction socket system. A randomized controlled study. Eur J Phys Rehabil Med. 2012. Dec 1;48(4):613–23. [PubMed] [Google Scholar]
- 46.Hoskins RD, Sutton EE, Kinor D, Schaeffer JM, Fatone S. Using vacuum-assisted suspension to manage residual limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int 2014; 38: 68–74. 10.1177/0309364613487547 [DOI] [PubMed] [Google Scholar]
- 47.Philbeck JT, Whittington KT, Millsap MH, Briones RB, Wight DG, Schroeder WJ. The clinical and cost effectiveness of externally applied negative pressure wound therapy in the treatment of wounds in home healthcare Medicare patients. Ostomy Wound Manag. 1999;45(11):41–50. [PubMed] [Google Scholar]
- 48.Huang C, Leavitt T, Bayer LR, Orgill DP. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg 2014; 51: 301–331. DOI: 10.1067/j.cpsurg.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 49.Armstrong DG, Lavery LA, Diabetic Foot Study Consortium. Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomised controlled trial. Lancet. 005;366(9498):1704–10. 10.1016/S0140-6736(05)67695-7 [DOI] [PubMed] [Google Scholar]
- 50.Portnoy S, Kristal A, Gefen A, Siev-Ner I. Outdoor dynamic subject-specific evaluation of internal stresses in the residual limb: Hydraulic energy-stored prosthetic foot compared to conventional energy-stored prosthetic feet. Gait Posture. 2012;35(1):121–5. 10.1016/j.gaitpost.2011.08.021 [DOI] [PubMed] [Google Scholar]


