Abstract
Importance:
Agitation is common in mechanically ventilated ICU patients, but little is known about physician attitudes regarding agitation in this setting.
Objectives:
To characterize physician attitudes regarding agitation in mechanically ventilated ICU patients.
Design, Setting, and Participants:
We surveyed critical care physicians within a multicenter health system in Western Pennsylvania, assessing attitudes regarding agitation during mechanical ventilation and use of and confidence in agitation management options. We used quantitative clinical vignettes to determine whether agitation influences confidence regarding readiness for extubation. We sent our survey to 332 critical care physicians, of whom 80 (24%) responded and 69 were eligible (had cared for a mechanically ventilated patient in the preceding three months).
Main Outcomes and Measures:
Respondent confidence in patient readiness for extubation (0–100%, continuous) and frequency of use and confidence in management options (1–5, Likert).
Results:
Of 69 eligible responders, 61 (88%) agreed agitation is common and 49 (71%) agreed agitation is a barrier to extubation, but only 27 (39%) agreed their approach to agitation is evidence-based. Attitudes regarding agitation did not differ much by practice setting or physician demographics, though respondents working in medical ICUs were more likely (p=0.04) and respondents trained in surgery or emergency medicine were less likely (p=0.03) than others to indicate that agitation is an extubation barrier. Fifty-three (77%) respondents reported they frequently use non-pharmacologic measures to treat agitation, and 42 (70%) of those who reported they used non-pharmacologic measures during the prior 3 months indicated confidence in their effectiveness. In responses to clinical vignettes, confidence in patient’s readiness for extubation was significantly lower if the patient was agitated (p<0.001) or tachypneic (p<0.001), but the presence of both agitation and tachypnea did not reduce confidence compared with tachypnea alone (p=0.24).
Conclusions and Relevance:
Most critical care physicians consider agitation during mechanical ventilation a common problem and agreed that agitation is a barrier to extubation. Treatment practice varies widely.
Keywords: Psychomotor Agitation, Airway Extubation, Cross-Sectional Studies, Practice Patterns, Physicians
Introduction
Every year, more than 10 million patients worldwide require mechanical ventilation for acute respiratory failure.1 Up to 70% of these patients develop agitation, most often due to delirium, a syndrome of acute brain dysfunction characterized by fluctuating disturbances in attention and cognition.2 During mechanical ventilation, both agitation and delirium interfere with care and are associated with a variety of undesirable outcomes, including delays in extubation and ICU discharge and increases in mortality, cost, and long-term cognitive impairment.3–6
Agitation during mechanical ventilation is often managed with sedatives and analgesics,7,8 yet some sedation practices, most notably deep sedation and use of benzodiazepines, are associated with persistent delirium9–11 and prolonged mechanical ventilation.10 Current guidelines from the Society for Critical Care Medicine recommend light sedation,8 but this management goal can be difficult to achieve when a patient is agitated. Indeed, the potentially competing goals of minimizing agitation while maintaining light sedation, as well as the lack of clear evidence regarding effective treatments for agitation during mechanical ventilation, contributes to variability in sedation practices and in clinical decision-making in response to agitation. During the liberation phase of mechanical ventilation, for example, agitation—which is often accompanied by tachypnea—may lead clinicians to defer extubation. Little is known, however, about critical care physicians’ attitudes regarding agitation in this setting.
We therefore conducted a survey to better understand attitudes and approaches to agitation during mechanical ventilation. We hypothesized that most critical care physicians view agitation as a barrier to liberation from mechanical ventilation and are less likely to extubate a patient who is agitated than one who is not. We also expected that preferences regarding the treatment of agitation during mechanical ventilation would vary widely.
Methods
In October 2019, we used a commercially available, web-based survey tool (Qualtrics) to survey critical care physicians across the UPMC Health System, a large, nonprofit, multihospital system located primarily in western Pennsylvania, USA. We sent an email invitation, including a cover letter, and up to two follow-up emails to 332 potential respondents (i.e., critical care physicians) identified using health system directories. We offered no incentives. The University of Pittsburgh Institutional Review Board reviewed the study (“Provider perceptions regarding agitation during mechanical ventilation”) as STUDY19090111 and approved it on 10/1/2019 as exempt under 45 CFR 46.101(b) (2).12 In this survey study, no individual patient data or personal identifiers were collected, and all research was conducted in accordance with the most recent (2013) revision of the Declaration of Helsinki.13
We sought to examine attitudes toward agitation during invasive mechanical ventilation and variation in the management of agitation. Our systematic approach to survey development included (1) formulating the research questions, (2) determining whether a survey was an appropriate tool to help answer the questions, (3) conducting a literature review to determine if previous surveys on this topic had been developed and validated, (4) drafting survey items, (5) having content experts review the survey items for face and content validity, clarity, and relevance, (6) revising the items, (7) piloting the survey, and (8) revising the items again prior to deployment of the survey. To assess and improve face and content validity, we pilot tested a draft survey with two critical care physicians who practice outside the UPMC Health System and revised the survey based on their feedback. The final survey assessed respondents’ demographics, their attitudes regarding agitation during mechanical ventilation, and their use of and confidence in management options. We measured attitudes using a 5-point Likert scale. We measured use of and confidence in management options using a 4-point Likert scale. We also used clinical vignettes to determine whether agitation influences critical care physicians’ confidence regarding readiness for extubation. Specifically, the outcome measured with these vignettes was self-reported confidence in a patient’s readiness for extubation, measured as a percentage (range, 0% to 100%) and analyzed as a continuous variable. The order of the vignettes, which are shown in Table 1, was randomized, and all respondents viewed all vignettes, allowing each respondent to serve as their own comparator. The full survey is available online as supplementary material.
Table 1.
Case vignettes regarding confidence in extubation readiness
| When answering the questions that follow, imagine a patient with acute respiratory failure who is receiving invasive mechanical ventilation (i.e., they are intubated) in the ICU. You are assessing the patient 30 minutes after a spontaneous breathing trial (SBT) started. |
| The patient is on pressure support ventilation (PSV) with 5 cm H2O inspiratory pressure, 5 cm H2O PEEP, and 40% FiO2. Their SpO2 is 96%, and they have a strong cough and no secretions. |
| Given the following findings (RR indicates respiratory rate), please indicate your level of confidence that the patient is ready for extubation: |
| • RR 18/min, Riker SAS 4 (alert and calm) |
| • RR 18/min, Riker SAS 5 (agitated) |
| • RR 18/min, Riker SAS 6 (very agitated) |
| • RR 33/min, Riker SAS 4 (alert and calm) |
| • RR 33/min, Riker SAS 5 (agitated) |
| • RR 33/min, Riker SAS 6 (very agitated) |
|
|
| For each of the 6 vignettes, respondents were asked to rate their confidence that the patient was ready for extubation using a 0–100 slider. |
We excluded respondents who reported they had not provided care for a mechanically ventilated adult in the three months preceding the survey as this study was focused specifically on agitation during mechanical ventilation. For descriptive purposes, we considered responses of “strongly agree” and “somewhat agree” to indicate agreement with our attitudinal questions, responses of “very often” and “always” to indicate frequent use of a given therapy, and responses of “moderate confidence” and “high confidence” to indicate confidence in the effectiveness of a therapy. Survey questions without responses were treated as missing and were not imputed.
We used Stata (version 16.1) for statistical analysis. We used Fisher’s exact tests to assess associations between categorical respondent characteristics (e.g., ICU type and primary specialty) and attitudinal responses. We used Wilcoxon signed-rank tests to determine whether confidence regarding readiness for extubation differed by respiratory rate or presence/absence of agitation and report sign test p values, median difference in confidence, and non-parametric 95% confidence intervals for this difference, which we generated via bootstrapping with one thousand samples. We considered a two-sided alpha of 0.05 to indicate significance.
Results
From the 332 individuals invited to participate, we received 80 (24%) responses, but we excluded 11 respondents who had not cared for a mechanically ventilated patient in the previous three months. We therefore analyzed data from 69 (21%) respondents, whose characteristics are shown in Table 2. All 69 respondents completed all applicable survey questions, leaving no incomplete responses. Most respondents were trained in internal medicine, though nearly half worked in general medical/surgical ICUs. Six different hospitals were represented, with some respondents providing care in more than one; the most common primary hospital was UPMC Presbyterian, UPMC’s largest referral and teaching hospital. Half of the respondents reported five or more years of critical care-specific practice.
Table 2.
Respondent characteristics
| Characteristics | Total (N=69) |
|---|---|
| Male, n (%) | 45 (65%) |
| Years of critical care experience, median [IQR] | 5 [2–14] |
| Training background, n (%) | |
| Internal Medicine | 49 (71%) |
| Emergency Medicine | 15 (22%) |
| Surgery | 3 (4%) |
| Anesthesia | 1 (1%) |
| Neurology | 1 (1%) |
| ICU type, n (%) | |
| General | 33 (48%) |
| Medical | 26 (38%) |
| Trauma | 5 (7%) |
| Surgical | 3 (4%) |
| Neurological | 2 (3% |
| Primary hospital, n (%) | |
| UPMC Presbyterian | 44 (64%) |
| UPMC Mercy | 9 (13%) |
| UPMC Magee-Women’s | 5 (7%) |
| UPMC Shadyside | 5 (7%) |
| UPMC East | 4 (6%) |
| UPMC Hamot | 1 (1%) |
| Other | 1 (1%) |
Agitation was recognized as a problem by nearly all respondents; 88% agreed that agitation is common, 71% agreed it is a barrier to extubation, and 65% agreed agitation is harmful to mechanically ventilated patients (Table 3). Notably, only 39% of respondents agreed that their approach to agitation is evidence-based. Attitudes about agitation did not differ much between practice settings or physician demographic groups, though respondents working in medical ICUs were more likely to indicate that agitation is an extubation barrier (Table 3; p=0.04), and respondents trained in surgery or emergency medicine were less likely than those trained in other specialties to indicate that agitation is an extubation barrier (p=0.03).
Table 3.
Critical care physician perspectives regarding agitation during mechanical ventilation
| Somewhat or Strongly Agree | ||||||||
|---|---|---|---|---|---|---|---|---|
| Statement about agitation | All (N=69) | GICU (N=30) | MICU (N=25) | SICU (N=4) | TICU (N=4) | NICU (N=3) | Other (N=3) | P value |
| Agitation is a common problem in my ICU. | 61 (88%) | 26 (87%) | 23 (92%) | 4 (100%) | 3 (75%) | 3 (100%) | 2 (67%) | 0.52 |
| When mechanically ventilated patients experience agitation, it causes them harm. | 45 (65%) | 18 (60%) | 17 (68%) | 4 (100%) | 3 (75%) | 1 (33%) | 2 (67%) | 0.60 |
| Agitation during mechanical ventilation is a barrier to successful extubation. | 49 (71%) | 20 (67%) | 22 (88%) | 3 (75%) | 1 (25%) | 2 (67%) | 1 (33%) | 0.04 |
| My approach to treating agitation during mechanical ventilation is evidence-based. | 27 (39%) | 13 (43%) | 10 (40%) | 2 (50%) | 1 (25%) | 0 (0%) | 1 (33%) | 0.84 |
Abbreviations: GICU, general ICU; MICU, medical ICU; NICU, neurologic ICU; SICU, surgical ICU; TICU, trauma ICU
Results indicate the n (%) who selected a 3 (somewhat agree) or 4 (strongly agree) on a 4-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree).
P values were generated using Fisher’s exact tests that compared critical care physicians’ agreement with each statement across ICU types.
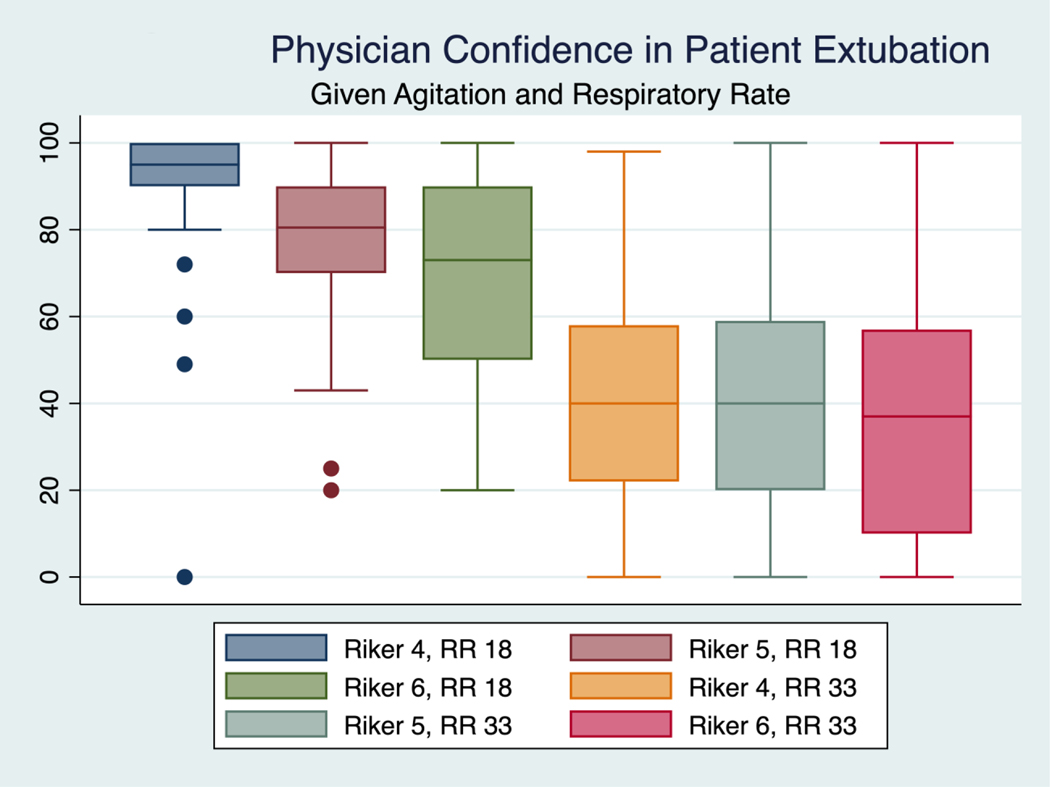
Responses to case vignettes revealed that confidence in the extubation readiness of a non-agitated (indicated by a Riker Sedation-Agitation Scale [SAS] score of 4), non-tachypneic (indicated by a respiratory rate [RR] of 18) patient who passed a spontaneous breathing trial (SBT) was high (Figure 1). When the patient was not tachypneic, confidence in extubation readiness was significantly lower when the vignette included agitation (median difference −11% confident, 95% CI −16% to −6%, p<0.001 for SAS4/RR18 vs. SAS5/RR18; median difference −20% confident, 95% CI −26% to −14%, p<0.001 for SAS4/RR18 vs. SAS6/RR18). Tachypnea (RR33) was also associated with a reduction in confidence (mean difference −50% confident, 95% CI −60% to −40%, p<0.001 for SAS4/RR18 vs. SAS4/RR33; mean difference −27% confident, 95% CI −34% to −19%, p<0.001 for SAS6/RR18 vs. SAS6/RR33). Agitation was not, however, associated with confidence when both vignettes described a tachypneic patient (mean difference −1% confident, 95% CI −8% to 7%, p=0.21 for SAS4/RR33 vs. SAS6/RR33).
Figure 1.
Box-and-whisker plots of respondent critical care physicians’ self-reported confidence in the extubation of standardized vignette patients of varying respiratory rates (RR) and levels of agitation, as measured by the Riker Sedation-Agitation Scale (SAS). Among non-tachypneic patients, any increase in agitation is associated with a significant decrement in extubation confidence (p < 0.001). There are significant differences in extubation confidence between tachypneic and non-tachypneic patients at all levels of agitation. Among tachypneic patients, changes in agitation are not associated with significant changes in extubation confidence.
Use of and confidence in therapies for agitation during mechanical ventilation were highly variable (Table 4). Respondents reported they most often use non-pharmacologic measures, and 70% of those who used non-pharmacologic measures during the 3 months before the survey reported confidence in the strategy. Only a small number of respondents reported they frequently use dexmedetomidine to manage agitation during mechanical ventilation despite the fact that 69% of those who reported using dexmedetomidine in the prior 3 months indicated they are confident in the effectiveness of this medication. Specific antipsychotics, alternatively, were reported to be used frequently by up to one third of respondents—32% reported frequently using quetiapine, 14% reported frequently using olanzapine, and 10% reported frequently using haloperidol—but no more than half of those who reported using any individual antipsychotic indicated confidence in that medication’s effectiveness.
Table 4.
Frequency of use and confidence in different treatments for agitation during mechanical ventilation
| Treatment | Frequently Usea | Confident in Effectivenessb |
|---|---|---|
| Propofol | 32 (46%) | 44 (76%) |
| Fentanyl | 37 (54%) | 36 (63%) |
| Quetiapine | 22 (32%) | 26 (51%) |
| Olanzapine | 12 (17%) | 17 (41%) |
| Non-pharmacologic | 53 (77%) | 42 (70%) |
| Haloperidol | 10 (14%) | 19 (50%) |
| Midazolam | 11 (16%) | 23 (56%) |
| Dexmedetomidine | 4 (6%) | 27 (69%) |
| Lorazepam | 0 (0%) | n/a |
Number (%) of respondents who reported using the treatment “very often” or “always” when treating agitation in an ICU patient receiving mechanical ventilation during the 3 months preceding the survey
Number (%) of respondents (among those who reported using the treatment during the 3 months preceding the survey) who reported moderate or high confidence that the treatment is effective when managing agitation during mechanical ventilation
Reported use of select treatments for agitation during mechanical ventilation varied by specialty training background, but use of most treatments was similar across specialties (Table 5). Emergency Medicine-trained critical care physicians were more likely than others to report frequent use of propofol (p=0.04), whereas Internal Medicine- and Neurology-trained critical care physicians were more likely than others to report frequent use of non-pharmacologic measures (p=0.02).
Table 5.
Frequency of use of different treatments for agitation during mechanical ventilation by specialty training background
| Frequently Usea | ||||||
|---|---|---|---|---|---|---|
| Treatment | IM (N=49) | Surgery (N=3) | Anesthesia (N=1) | EM (N=15) | Neurology (N=1) | P valueb |
| Propofol | 19 (39%) | 2 (67%) | 0 (0%) | 11 (80%) | 0 (0%) | 0.04 |
| Fentanyl | 25 (51%) | 2 (67%) | 0 (0%) | 10 (80%) | 0 (0%) | 0.49 |
| Quetiapine | 16 (80%) | 1 (33%) | 1 (100%) | 4 (27%) | 0 (0%) | 0.68 |
| Olanzapine | 10 (20%) | 0 (0%) | 0 (0%) | 2 (13%) | 0 (0%) | 0.89 |
| Non-pharmacologic | 42 (86%) | 2 (67%) | 0 (0%) | 8 (53%) | 1 (100%) | 0.02 |
| Haloperidol | 8 (16%) | 1 (33%) | 0 (0%) | 1 (7%) | 0 (0%) | 0.58 |
| Midazolam | 10 (20%) | 1 (33%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.20 |
| Dexmedetomidine | 3 (6%) | 0 (0%) | 0 (0%) | 1 (7%) | 0 (0%) | 1.00 |
| Lorazepam | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
Abbreviations: EM, Emergency Medicine; IM, Internal Medicine
Number (%) of respondents who reported using the treatment “very often” or “always” when treating agitation in an ICU patient receiving mechanical ventilation during the 3 months preceding the survey
P values were generated using Fisher’s exact tests that compared critical care physicians’ reported use of treatments for agitation by specialty training background.
Discussion
In this survey of critical care physicians working in six Midwest hospitals in the US, we found that a high percentage of respondents consider agitation during mechanical ventilation to be a common problem and a barrier to extubation. Specifically, 88% of respondents agreed agitation during mechanical ventilation is common, and 65% agreed it is harmful. Additionally, critical care physicians responding to this survey were increasingly less likely to judge a hypothetical patient as ready for extubation the more agitated the patient was, even if all other variables used to judge extubation readiness were optimized. Yet in the face of this common threat to patient recovery, the management of agitation varies widely, and critical care physicians are not very confident about treatment options. These findings highlight a major knowledge gap in the care of mechanically ventilated ICU patients.
Though several survey studies have highlighted the barrier that agitation poses to the delivery of critical care, our study is the first, to our knowledge, to evaluate agitation during mechanical ventilation as a barrier to extubation. Freeman and colleagues found that 99% of critical care clinicians surveyed agreed that an agitated patient is at increased risk of harm,14 and Morandi et al. documented significant variability in worldwide use of treatments for agitation in the ICU.15 We advanced this line of research by using clinical vignettes to show that agitation during mechanical ventilation is quantitively associated with reduced confidence in extubation readiness among clinicians. Using this approach, we found that for a non-tachypneic patient, a 1-point increase in the SAS (i.e., minor agitation) decreases clinician confidence in readiness for extubation by 11 percentage points. This finding highlights the need for evidence-based treatments (pharmacologic or non-pharmacologic) that reduce agitation during recovery from acute respiratory failure.
We found that the percentage of respondents who reported frequently using a specific treatment for agitation varied from 0% for lorazepam to 77% for non-pharmacologic measures. This variability in use may reflect variability in confidence and/or tension between a treatment’s perceived effectiveness and its side effect profile. More than half of respondents, for example, who reported using midazolam were confident it is effective, but less than one in six respondents reported using it frequently, possibly due to its association with delirium.11 Approximately 70% of the respondents who reported using propofol and dexmedetomidine—the two sedatives recommended in Society for Critical Care Medicine (SCCM) clinical practice guidelines8—were confident in the effectiveness of these agents, but fewer than 5% of all respondents reported frequent use of dexmedetomidine, with use possibly limited by cost and/or availability (factors that were not assessed in our survey).
Given the sample size, which is the largest thus reported but still modest, it is difficult to interpret these findings conclusively, although the trends are suggestive that either physician or patient factors influence attitudes and practices. Given the sample size, particularly the relatively minimal crossover between training background and ICU type, we are unable to answer the question of whether training background, practice environment, or both are the primary determinants of attitude. This finding should be evaluated in larger studies.
Confidence in non-pharmacologic therapies—which are also recommended by SCCM guidelines—was relatively high among users, but nearly one-fourth of respondents did not report frequent use of non-pharmacologic measures, a finding that is consistent with studies reporting that most ICUs do not have a consistent protocol to guide non-pharmacologic treatments for agitation.16 Non-users may be motivated by lack of confidence as well as by barriers to implementation.17 Of note, non-pharmacologic treatment of agitation should be understood to include prevention of common causes of agitation, including delirium and discomfort due to pain, bladder distention, air hunger, or immobility. Indeed, prevention of delirium and discomfort remains a key part of agitation management, as recommended in the SCCM PADIS guidelines,8 especially since seminal clinical trials have shown that delirium can be curtailed by non-pharmacologic interventions, most notably early mobilization.18,19
When compared with confidence in guideline-recommended treatments, confidence among users of other treatments—including medications that have been found to be ineffective as delirium treatments (e.g., haloperidol20)—was not much lower. This finding may reflect the lack of clear evidence guiding the treatment of agitation during mechanical ventilation. Importantly, deep pharmacologic sedation is widely recognized to be detrimental10,21 with recent studies finding that depth of sedation is more relevant to post-extubation delirium risk than dose of sedatives.22 The management of agitation during mechanical ventilation frequently involves an implicit or explicit tradeoff between the risks of agitation and the risks of sedation. Though guidelines recommend frequent assessment of sedation level and maintenance of light sedation, they typically do not provide an explicit framework for balancing the competing risks of agitation and moderate-to-deep sedation. Such a framework would likely be helpful in creating confidence in agitation management strategies.
The major strength of this study is its size, as the largest survey of critical care physicians on agitation heretofore published. The most similar survey, which included 25 physicians, focused primarily on nursing attitudes regarding the use of physical restraints to manage agitation.14 Other studies of physician approaches to agitation in the ICU included a unit-level survey of agitation-management practices in Canada (4 physicians),16 whereas most studies have not differentiated between routine sedation and the management of agitation.23–26 Another strength was the use of standardized case vignettes, which allowed us to quantitatively assess the association between agitation and perceived extubation readiness.
Limitations included that our study was conducted within a single health system in one region of the United States. Though previous studies do not suggest this is the case, agitation management may vary geographically, and attitudes about agitation during mechanical ventilation may differ as well. Despite being the largest survey of critical care physicians on agitation to date, the size and demographic breakdown of our respondent pool likely prevent meaningful analysis of differences in attitude or management preferences based on training background, practice duration, primary ICU type, interprofessional team dynamics, or other factors that may influence how a critical care physician might manage agitation. As we did not formally assess inter- and intra-rater reliability, it may be that some variability across respondents was due to test effects or to chance. Also, we did not ask respondents about systematic algorithms or specific non-pharmacologic treatments, but their use and confidence may differ from one non-pharmacologic approach to another. Lastly, nonresponse bias could have affected results, though our response rate was not low for an email-based survey. Reminder emails were the only strategy we used to increase response rate, which might have been higher if compensation was offered.
Conclusions
A very high percentage of critical care physicians consider agitation a common problem for mechanically ventilated patients and agree that agitation is a barrier to extubation. Yet use of and confidence in treatments varies widely, and a minority of critical care physicians consider available treatments to be evidenced based. Prospective studies of agitation are now needed to identify mechanisms and potential treatments, and clinical trials of commonly used agitation treatments are ultimately needed to guide clinicians as they seek to improve patients’ outcomes.
Supplementary Material
Funding:
This work was supported by the National Institutes of Health (grant number 1F32HL158058). The funding source had no role in design of the study, collection, analysis, or interpretation of data, or in preparation of the manuscript.
TDG receives research funding from the National Institutes of Health and Ceribell, served previously as a consultant for Haisco Pharmaceutical Group Co., Ltd., and is on an advisory board for Lungpacer Medical Inc.
Footnotes
Declarations
Financial Disclosures and Conflicts of Interest:
The other authors (NTP, CAO, KMP, PJT, AET) have no conflicts of interest to disclose.
References
- 1.Wunsch H, Linde-Zwirble WT, Angus DC, Hartman ME, Milbrandt EB, Kahn JM. The epidemiology of mechanical ventilation use in the United States. Crit Care Med 2010;38(10):1947–53. DOI: 10.1097/CCM.0b013e3181ef4460. [DOI] [PubMed] [Google Scholar]
- 2.Prendergast NT, Tiberio PJ, Girard TD. Treatment of delirium during critical illness. Annu Rev Med 2022;73:407–421. DOI: 10.1146/annurev-med-042220-013015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association., American Psychiatric Association. DSM-5 Task Force. Diagnostic and statistical manual of mental disorders : DSM-5. 5th ed. Washington, D.C.: American Psychiatric Association, 2013. [Google Scholar]
- 4.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 2004;291(14):1753–62. DOI: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 5.Girard TD, Jackson JC, Pandharipande PP, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med 2010;38(7):1513–20. DOI: 10.1097/CCM.0b013e3181e47be1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lat I, McMillian W, Taylor S, et al. The impact of delirium on clinical outcomes in mechanically ventilated surgical and trauma patients. Crit Care Med 2009;37(6):1898–905. DOI: 10.1097/CCM.0b013e31819ffe38. [DOI] [PubMed] [Google Scholar]
- 7.Arroliga AC, Thompson BT, Ancukiewicz M, et al. Use of sedatives, opioids, and neuromuscular blocking agents in patients with acute lung injury and acute respiratory distress syndrome. Crit Care Med 2008;36(4):1083–8. DOI: 10.1097/CCM.0B013E3181653895. [DOI] [PubMed] [Google Scholar]
- 8.Devlin JW, Skrobik Y, Gelinas C, et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med 2018;46(9):e825–e873. DOI: 10.1097/CCM.0000000000003299. [DOI] [PubMed] [Google Scholar]
- 9.Pandharipande P, Shintani A, Peterson J, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology 2006;104(1):21–6. DOI: 10.1097/00000542-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Shehabi Y, Bellomo R, Kadiman S, et al. Sedation Intensity in the First 48 Hours of Mechanical Ventilation and 180-Day Mortality: A Multinational Prospective Longitudinal Cohort Study. Crit Care Med 2018;46(6):850–859. DOI: 10.1097/CCM.0000000000003071. [DOI] [PubMed] [Google Scholar]
- 11.Shi HJ, Yuan RX, Zhang JZ, Chen JH, Hu AM. Effect of midazolam on delirium in critically ill patients: a propensity score analysis. J Int Med Res 2022;50(4):3000605221088695. DOI: 10.1177/03000605221088695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.45 C.F.R. § 46.1012019.
- 13.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310(20):2191–4. DOI: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 14.Freeman S, Yorke J, Dark P. The management of agitation in adult critical care: Views and opinions from the multi-disciplinary team using a survey approach. Intensive Crit Care Nurs 2019;54:23–28. DOI: 10.1016/j.iccn.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Morandi A, Piva S, Ely EW, et al. Worldwide Survey of the “Assessing Pain, Both Spontaneous Awakening and Breathing Trials, Choice of Drugs, Delirium Monitoring/Management, Early Exercise/Mobility, and Family Empowerment” (ABCDEF) Bundle. Crit Care Med 2017;45(11):e1111–e1122. DOI: 10.1097/CCM.0000000000002640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiu JA, Shergill M, Dhingra V, et al. Variation in the Management of Pain, Agitation, and Delirium in Intensive Care Units in British Columbia. Am J Crit Care 2020;29(2):122–129. DOI: 10.4037/ajcc2020396. [DOI] [PubMed] [Google Scholar]
- 17.Balas MC, Pun BT, Pasero C, et al. Common Challenges to Effective ABCDEF Bundle Implementation: The ICU Liberation Campaign Experience. Crit Care Nurse 2019;39(1):46–60. DOI: 10.4037/ccn2019927. [DOI] [PubMed] [Google Scholar]
- 18.Schaller SJ, Anstey M, Blobner M, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 2016;388(10052):1377–1388. DOI: 10.1016/S0140-6736(16)31637-3. [DOI] [PubMed] [Google Scholar]
- 19.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009;373(9678):1874–82. DOI: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Girard TD, Exline MC, Carson SS, et al. Haloperidol and Ziprasidone for Treatment of Delirium in Critical Illness. N Engl J Med 2018;379(26):2506–2516. DOI: 10.1056/NEJMoa1808217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wongtangman K, Santer P, Wachtendorf LJ, et al. Association of Sedation, Coma, and In-Hospital Mortality in Mechanically Ventilated Patients With Coronavirus Disease 2019-Related Acute Respiratory Distress Syndrome: A Retrospective Cohort Study. Crit Care Med 2021;49(9):1524–1534. DOI: 10.1097/CCM.0000000000005053. [DOI] [PubMed] [Google Scholar]
- 22.Azimaraghi O, Wongtangman K, Wachtendorf LJ, et al. Differential Effects of Gamma-Aminobutyric Acidergic Sedatives on Risk of Post-Extubation Delirium in the ICU: A Retrospective Cohort Study From a New England Health Care Network. Crit Care Med 2022;50(5):e434-e444. DOI: 10.1097/CCM.0000000000005425. [DOI] [PubMed] [Google Scholar]
- 23.Wang J, Peng ZY, Zhou WH, Hu B, Rao X, Li JG. A National Multicenter Survey on Management of Pain, Agitation, and Delirium in Intensive Care Units in China. Chin Med J (Engl) 2017;130(10):1182–1188. DOI: 10.4103/0366-6999.205852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soliman HM, Melot C, Vincent JL. Sedative and analgesic practice in the intensive care unit: the results of a European survey. Br J Anaesth 2001;87(2):186–92. DOI: 10.1093/bja/87.2.186. [DOI] [PubMed] [Google Scholar]
- 25.Martin J, Parsch A, Franck M, Wernecke KD, Fischer M, Spies C. Practice of sedation and analgesia in German intensive care units: results of a national survey. Crit Care 2005;9(2):R117–23. DOI: 10.1186/cc3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salluh JI, Dal-Pizzol F, Mello PV, et al. Delirium recognition and sedation practices in critically ill patients: a survey on the attitudes of 1015 Brazilian critical care physicians. J Crit Care 2009;24(4):556–62. DOI: 10.1016/j.jcrc.2009.04.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.