Abstract
Obsessive-compulsive disorder is an impairing psychiatric condition affecting 1-2% of adults and youth. Cognitive-behavioral therapy with exposure and response prevention (CBT) is an efficacious intervention but requires specialty training and access is often limited. While certain factors are associated with treatment access, one key barrier that has not been explored is the geographic availability of OCD treatment providers. Using integrated geographically-referenced data, we examined the geographic distribution of OCD CBT specialty providers across the state of Texas, with particular attention to the relationship to neighborhood socioeconomic disadvantage, insurance status, and rural versus urban status. We found that specialist providers are almost exclusively located inside the highly urbanized parts of the state, primarily in more affluent areas, and often only accept self-pay. The characteristics of the areas located the furthest away from specialty OCD care include a high proportion of persons identifying as Hispanic; a high proportion of non-English speakers, households with income below poverty; households with no vehicles; and persons with no health insurance. Average household income decreased as distances from specialist providers increased. Broadly, findings confirm that OCD CBT specialty providers are clustered in large socially advantaged areas and that economic disadvantage remains a significant barrier to care. As inadequate or inappropriate treatment of OCD is likely to result in sustained and impairing symptoms, this is of great concern.
Keywords: Obsessive-compulsive disorder, Cognitive-behavioral therapy, Exposure and response prevention, Barriers, Treatment Access, Geographic Information System, Social determinants of health
INTRODUCTION
Obsessive-compulsive disorder (OCD) affects approximately 1-2% of individuals and contributes to considerable impairment and duress [1, 2]. Evidence-based treatment strategies, namely cognitive-behavioral therapy (CBT) and pharmacotherapy with serotonin reuptake inhibitors (SRI), have been established as effective [3-5]. Evidence supports CBT monotherapy as the first-line intervention for mild/moderate cases and combined with SRIs for more severe presentations [6, 7]. Nevertheless, diagnosis is frequently delayed, and specialist CBT treatment is difficult to access, especially for those who must use insurance or live in rural locations [8-10]. As a result, many individuals do not receive treatment or if they do, it is inconsistent with best-practice as the underutilization of CBT and the difficulty that many patients have in accessing CBT has been documented in international samples[11].
Despite established clinical recommendations and patient preference for CBT [12, 13], many patients are unable to access care [14]. Inadequate intervention is associated with chronic symptom presentation as well as increased risk for further psychopathology [15]. Studies on barriers to OCD treatment have revealed both attitudinal (e.g., stigma, shame) and practical barriers (e.g., treatment availability, cost) faced by those with OCD [8, 10, 16, 17]. Ability to access treatment is impacted by sociodemographic factors: non-Hispanic White individuals are less likely to experience barriers related to transportation/scheduling of sessions or choosing their provider compared to other racial/ethnic groups [18], and African Americans are more likely than non-Hispanic White Americansto report barriers related to cost, stigma, and transportation, especially when uninsured [16]. One key barrier that has not been explored is the geographic availability of OCD treatment providers, which is associated with sociodemographic factors in other behavioral health conditions [19-21].
Given that residential neighborhoods have both direct and indirect effects on health [22, 23], detecting likely geographic disparities in patient access to care, or the incidence or prevalence of disease endpoints, for that matter, is valuable for health planning and resource allocation. Furthermore, in the U.S., renewed attention is directed toward the significance of the social determinants of health (SDoH) in health disparities [24-26]. SDoH may be assessed across three major domains, proximal, intermediate, and distal. While proximal and distal operate at the individual and policy levels, respectively, the intermediate determinants include the socio-environmental context within which individuals experience their routine/daily activities (e.g., neighborhood social environment). Therefore, examining the influence of neighborhood-level socioeconomic disadvantage, separately from individual SES, continues to attract significant attention [27]. Increasingly, researchers are using the area deprivation index (ADI), developed and validated by Singh [28], to assess neighborhood socioeconomic disadvantage. ADI has been used to examine disease risk factors [29], predict healthcare utilization [30], and understand healthcare disparities [28]. However, although studies have examined geographic-based disparities in access to mental health care in general [31], none are focused on OCD care access. Further, we are not aware of any work that used ADI specifically to measure socioeconomic-based disparities in OCD care access.
This study was designed to document geographic access to specialized CBT for OCD. CBT was chosen given the focused specialty training and the status of CBT as the patient-preferred first-line treatment for OCD [3, 6, 7]. The primary goal was to examine the geographic distribution of OCD CBT specialty providers across the state of Texas, with particular attention given to how the OCD CBT locations overlay on a measure of neighborhood socioeconomic disadvantage, and rural versus urban areas of Texas. Furthermore, we examined the relationships between the measure of socioeconomic disadvantage in the neighborhoods where the OCD providers are located and two aspects of their practice: (1) the payment types accepted by the providers (e.g., self-pay versus commercial insurance) and (2) the provider age expertise (e.g., child/adolescent and adult). Finally, we sought to examine the proportion of individuals who were within varied distances from an OCD specialty provider.
METHODS
We used ArcGIS Pro (Esri Corporation, Redlands, California) to integrate geospatial and other non-geographic data and to operationalize and ascertain spatially referenced neighborhood characteristics. GISs are “automated systems for the capture, storage, retrieval, analysis, and display of spatial (and spatially referenced) data” [32]. GIS mapping has been used in the healthcare sector for different purposes, including efforts to describe and understand the changing landscape of health care and access [33-35]. For this study, we followed the following geoanalytic processes.
OCD providers:
The websites of several professional organizations for clinicians specializing in OCD treatment were searched. This included the International OCD Foundation, Association for Behavioral and Cognitive Therapy, and Anxiety and Depressive Disorders Association. Clinician data including location, specialty, and insurance acceptance was sourced directly from organization resource listings. Per these professional organizations and the clinicians’ websites (when one existed), data regarding insurance acceptance and treatment specialization within OCD was collected. Individual clinician credentials and insurance acceptance were not independently reviewed by the study team. The addresses of all the Texas specialist providers were geocoded using ArcGIS World Geocoding Service (Esri, Redlands, CA), and assembled into their respective neighborhoods, defined as the US Census Bureau census tract. The census tract geographic level is a small (optimum population of 4,000 residents or 1,600 housing units) and relatively permanent statistical subdivision of a county designed to be relatively homogeneous in terms of population characteristics, economic status, and living conditions.
For context, we assessed the concentration of specialist providers in the rural versus urban parts of Texas. The US Census classifies urbanized centers into two types of Core Based Statistical Areas (CBSA); including metropolitan statistical areas (MSAs) and micropolitan statistical areas (μSAs). MSAs and μSAs have one urbanized area plus adjacent territory that has a high degree of social and economic integration with the core as measured by commuting ties. For MSAs, the urbanized area is 50,000 or more population while μSAs have at least 10,000 but less than 50,000 population [36, 37]. Any areas outside of these two CBSA categories are generally rural areas. Specifically, we also assessed the concentration of specialist providers specifically within the boundary of Texas-Mexico border area, formally defined as the area within 100 kilometers (or 62 miles) of the Rio Grande, it includes 32 Texas border counties [26].
The area deprivation index (ADI)
Simultaneously, the ArcGIS Pro application (Esri, Redlands, CA) was used to integrate geographically-referenced data in order to operationalize the ADI. The ADI is a composite measure of “neighborhood” socioeconomic disadvantage that is based on 17 U.S. Census variables from the following four categories: poverty, housing, employment, and education [28] (See Supplementary Table 1 for the ADI source variables). For the current study, we computed the ADI at the census tract geographic level (same as “neighborhood” for the specialist providers). The source variables for our ADI were from the U.S. Census 2012-2016 American Community Survey (ACS) 5-year estimates [38]. We computed the ADI scores for all the census tracts in Texas according to established protocol [28, 39], and for analysis purposes, we used the quartile classification method to create a four-class categorical measure of the state’s ADI data. Subsequently, we assigned the ADI score and the quartile-based class of any census tract to the specialist providers that were located inside the tract. Higher ADI scores represent greater disadvantage; therefore, census tracts were eventually assembled into either the least deprived group (Q1) or more deprived group (Q2 to Q4). This classification was purposeful because we intended to observe any differences between the very least deprived neighborhoods and others.
Health insurance plans
Insurance acceptance was sourced with the clinician location and specialty data in the manner described above. Insurance categorization was split into two categories: (1) self-pay only (i.e., does not accept any insurance) and (2) accepts some type of insurance. The latter was then further broken down into two sub-categories: (2a) accepts private insurance only and (2b) accepts both public and private insurance. Medicare and Medicaid were considered to be public insurances. All other insurances were considered to be private insurances. No listed clinicians reported to only accept public insurance.
Drive time catchment areas to Texas’ specialist providers
Using the Network Analyst Extension in ArcGIS Pro 2.6 (Esri, Redlands, CA) and Esri’s street network dataset, we delineated the boundaries of the areas (catchment areas) within which we expect Texans to drive to any of the 94 specialist providers based on typical weather and road conditions. We created a series of five concentric drive time rings around each facility, using varying travel time increments up to 120 minutes (2 hours) drive time to any facility. The drive time catchment areas were: 0 – 15 (immediate vicinity); 15 – 30 (short drive); 30 – 75 (manageable drive); 75 – 120 (long drive); and >120 minutes (tiring drive). We expect the drive times that we used and the accompanying descriptions to reflect how Texas residents may feel about their driving experience in general, especially because Texas is an auto centric state. The catchment delineation produced five mutually exclusive geographic zones that span the entire state. After these zones were established, we used the “Enrich” analysis tool in ArcGIS Pro 2.6 to produce summary estimates of selected characteristics for each catchment area. We used the default data allocation method in Esri’s Business Analyst Software as a Service (SaaS) mapping solution to address this challenge—the method allocates data to user-created geographic features (e.g., our catchment areas) by automatically applying population weights to the computation of the necessary estimates in real time. We tabulated data on 20 variables across the following domains: population, sociodemographic, socioeconomic, and health insurance status. Estimates were based on the US Census Bureau 2015-2019 American Community Survey (ACS) 5-year estimates [38], except for race/ethnicity estimates that were based on Esri’s population estimates for 2021. These steps are similar to our earlier approach [35].
Statistical analysis
First, frequency distributions were computed for: the major OCD specialty programs (offered vs. not offered); the proportion of all specialist providers in each ADI quartile group; and the frequency of insurance types accepted by the specialist providers. We also computed the mean (sd.) ADI score for each quartile group, first for all the census tracts in Texas, and thereafter for only the census tracts that contained specialist providers. To examine the relationships between the type of payments that specialist providers accepted and the ADI groups that they belonged to, we used cross tabulations to evaluate the differences in proportions, using the chi-square tests. Statistical significance was defined as p<0.05. Analyses were performed in Stata version 14.2.
RESULTS
Geographic distribution of specialist providers across Texas
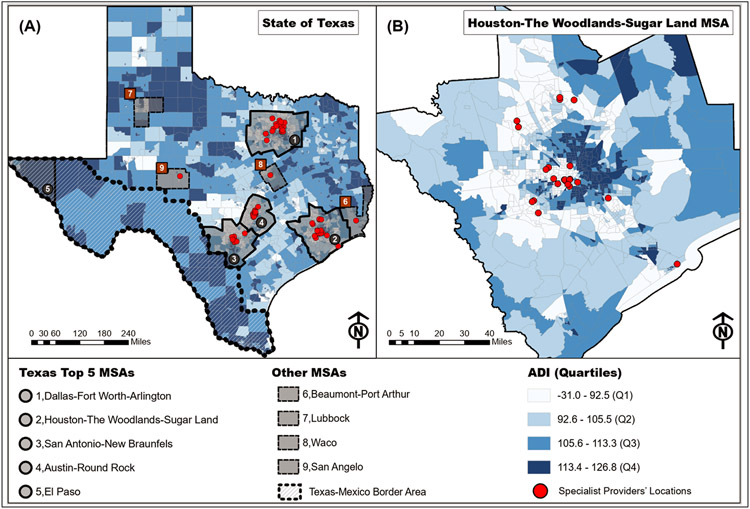
Across Texas, we identified 94 locations that provide OCD specialty programs. Individual clinics may practice more than one specialty program (see Table 1 for more details). The specialist providers are almost exclusively located inside the highly urbanized parts of the state; areas that generally have higher population density when compared with the rest of Texas. For context, 91 of the 94 centers were located inside the top four Texas MSAs: Dallas-Fort Worth-Arlington MSA, Houston-The Woodlands-Sugar Land MSA, San Antonio-New Braunfels MSA, and Austin-Round Rock MSA. Notably, there were no specialist providers inside the El Paso MSA; the fifth most-populous Texas MSA, whereas three smaller MSAs each contained one specialist provider. Similarly, no specialist providers were located in the southern parts of the state, along the Texas-Mexico border. The geographic distribution of the specialist providers is shown in Figure 1. Also, no specialist providers were located in non-CBSA areas of the state; meaning there were no clinics in rural Texas.
Table 1:
Texas Specialist providers: population served, specialty services, and treatments provided. 2019 data. a
| Population Served | ||
|---|---|---|
| Children | 48 | 51.1% |
| Adolescents | 73 | 77.7% |
| Adults | 87 | 92.6% |
| Specialty Services | ||
| BDD | 36 | 38.3% |
| Hoarding | 22 | 23.4% |
| Skin Picking | 51 | 54.3% |
| Trichotillomania | 52 | 55.3% |
| PANDAS/PANS | 16 | 17.0% |
| Tics/Tourette’s | 29 | 30.9% |
| Perfectionism | 66 | 70.2% |
| Scrupulosity | 55 | 58.5% |
| Violent/Sexual Obsession | 86 | 91.5% |
| ASD | 13 | 13.8% |
| OCD | 93 | 98.9% |
| Treatment | ||
| CBT | 89 | 94.7% |
| Medication | 4 | 4.3% |
| ACT | 41 | 43.6% |
| Family Therapy | 31 | 33.0% |
| Teletherapy | 30 | 31.9% |
| Skills Training | 42 | 44.7% |
| Home Visits | 32 | 34.0% |
| Intensive Treatment Options | 17 | 18.1% |
The websites of several professional organizations for clinicians specializing in OCD treatment were searched. This included the International OCD Foundation, Association for Behavioral and Cognitive Therapy, and Anxiety and Depressive Disorders Association.
Figure 1:
Specialist providers and area deprivation index (ADI) at the census tract level. (A) Distribution of ADI categories across the state of Texas with select CBSA boundaries overlay and the location of specialist providers. (B) A zoomed-in version of map (A) shows how Specialist providers are generally located inside low ADI census tracts.
OCD clinic locations and area deprivation index
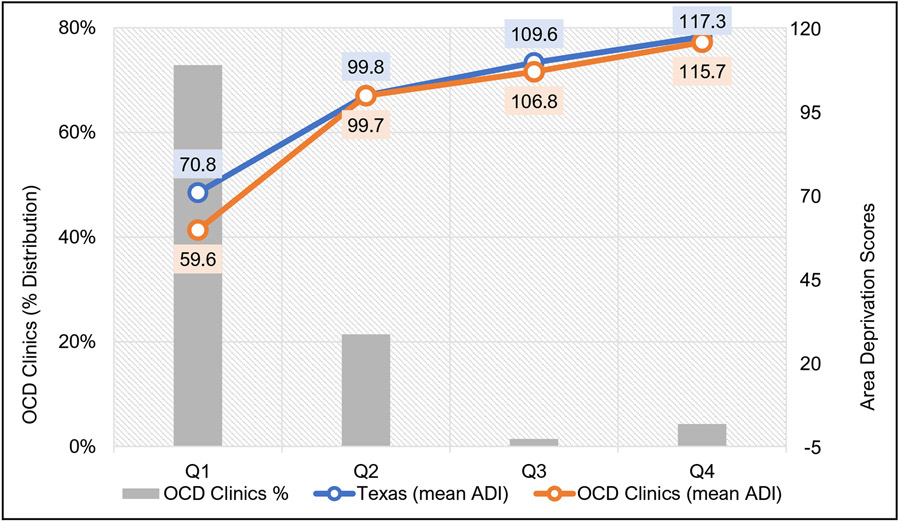
Figure 1 provides a visual representation of the 94 specialist providers’ locations when overlaid on the census tract level ADI categories (Q1 – Q4) across Texas. The specialist providers were located inside 70 census tracts out of the 5,220 Texas census tracts used for this analysis (i.e., 1.3%). Although Texas has a total of 5,265 CTs, 12 are “water only.” We also excluded CTs with less than 100 residents; these generally represent areas like campuses, airports, etc. When examined across ADI categories, 51 (72.9%) of the 70 specialist providers’ CTs were in the least derived category (Q1). Whereas 15 (21.4%), 1 (1.4%) and 3 (4.3%) tracts were located in the Q2, Q3, and Q4 groups, respectively. Also, the mean ADI scores for the specialist providers’ CTs are generally lower than the state’s mean scores, especially in Q1. (Figure 2).
Figure 2:
Distribution of Specialist providers across Texas: Clinic presence based on neighborhood socioeconomic deprivation (Quartiles)
Payment types accepted and Specialist providers’ locations neighborhood area deprivation index
Out of 89 specialist providers for which information about payment types accepted was available, 44 (49.4%) accepted self-pay only, while 45 (50.6%) accepted either private or public insurance. Specialist providers accepting self-pay only were significantly higher (88.6%) in the lower ADI census tracts (Q1; least deprived neighborhoods) compared with providers that accepted insurance payments; for those, 67% were located in the lower ADI census tracts (see Table 2).
TABLE 2:
Relationship between the ADI and the payment type accepted by specialist providers (N = 94a)
| Payment Type | Accepting insurance c | Self-pay only | P-valueb | ||
|---|---|---|---|---|---|
| Q1 | 30 | 67% | 39 | 88.6% | 0.013 |
| Q2 - Q4 | 15 | 33% | 5 | 11.4% | |
Note: Payment information was missing for 5 specialist providers (5.3%).
The Chi-square statistic is significant at the .05 level.
Private insurance only (N=35); public and private insurance (N=10). Of note the distribution of specialists accepting private only versus those accepting private/public did not differ between the two ADI groups.
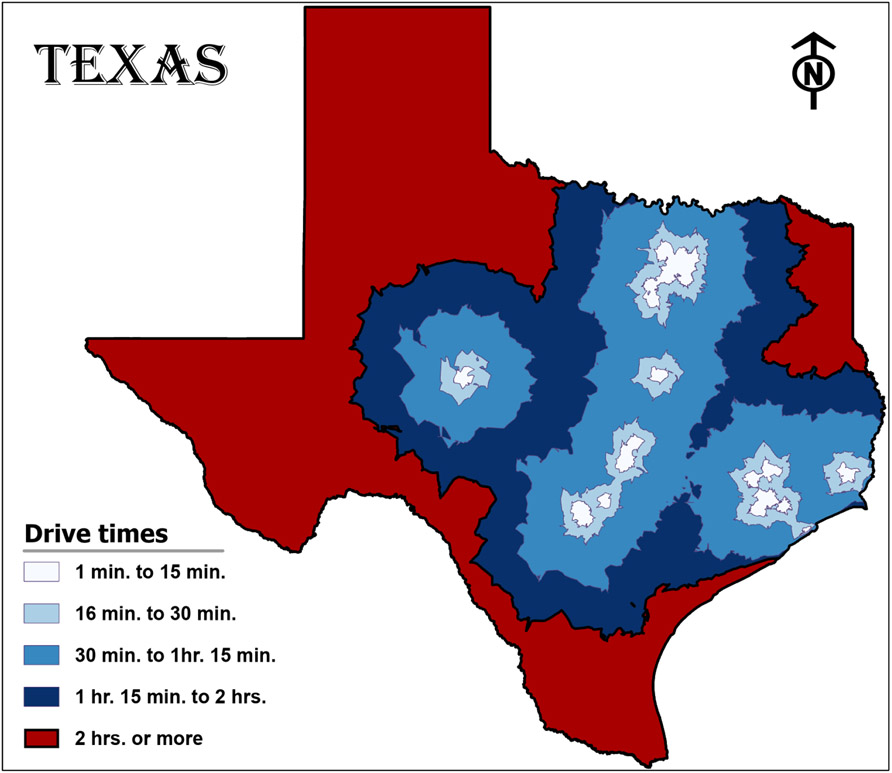
Drive time catchment area to Specialist providers
Detailed breakdown of the population characteristics for the drive time catchment areas that we created is shown in Table 3. Briefly, about one-third (35.52%) of Texas’ population is located inside the immediate vicinity (0 – 15 min. drive time), followed by the 16 – 30 min drive time (28.05%). The tiring drive catchment area (>120 min. drive time) contains the third largest population; about 5 million (16.62%). Notably, the characteristics that seem to be disproportionately high in the tiring drive catchment area, when compared with the other catchment areas, include Hispanic population (67.84%); persons speaking Spanish but not English language (3.50% of 18 – 64 y.o. and 1.72% of 65+ y.o.); households with income below poverty (20.57%); households with no vehicles (3.14% of homeowners); and persons with no health insurance (8.47%, and 9.53% for 19 – 34 y.o. and 35 – 64 y.o., respectively). Also, average household income decreased as distances from specialist providers increased, resulting in about $35,000 difference between the immediate vicinity catchment area and the tiring drive catchment area. Figure 3 shows the map of the drive time catchment areas and Table 3 contains more details on their characteristics.
TABLE 3:
Population characteristics calculated separately for each drive time ring.
| Immediate vicinity 0 – 15 min. |
Short drive 15 – 30 min. |
Manageable drive 30 – 75 min. |
Long drive 75 – 120 min. |
Tiring drive > 120 min. |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Population | ||||||||||
| 1. Total Population | 10,646,315 | 8,405,344 | 3,891,331 | 2,045,613 | 4,980,621 | |||||
| 2. Total Households | 4,010,207 | 2,801,090 | 1,411,658 | 752,670 | 1,640,096 | |||||
| 3. Civilian Population Age 18+ | 8,089,901 | 6,186,130 | 3,017,193 | 1,585,835 | 3,653,502 | |||||
| Sociodemographic | ||||||||||
| 4. Hispanic Population | 3888643 | (36.53) | 3183321 | (37.87) | 1007257 | (25.88) | 629079 | (30.75) | 3379095 | (67.84) |
| 5. NH White Pop | 4083483 | (38.36) | 3204281 | (38.12) | 2303920 | (59.21) | 1158159 | (56.62) | 1264574 | (25.39) |
| 6. NH Black Pop | 1441926 | (13.54) | 1371634 | (16.32) | 412134 | (10.59) | 190832 | (9.33) | 212120 | (4.26) |
| 7. NH Asian Pop | 967274 | (9.09) | 446631 | (5.31) | 64148 | (1.65) | 23907 | (1.17) | 60575 | (1.22) |
| 8. NH Others | 255827 | (2.40) | 192409 | (2.29) | 97358 | (2.50) | 42656 | (2.09) | 61303 | (1.23) |
| 9. 18-64 speak Span/No English | 174694 | (1.86) | 137923 | (1.89) | 22414 | (0.68) | 13451 | (0.73) | 154182 | (3.50) |
| 10. 65+speak Span/No English | 30012 | (0.32) | 25314 | (0.35) | 3669 | (0.11) | 3975 | (0.22) | 75731 | (1.72) |
| Socioeconomic | ||||||||||
| 11. Average household income | $101,784.00 | $94,582.00 | $83,342.00 | $74,358.00 | $67,014.00 | |||||
| 12. HHs: Income below poverty | 447172 | (12.14) | 298556 | (11.71) | 162839 | (13.27) | 106080 | (15.42) | 317087 | (20.57) |
| 13. HHs: Public assistance income | 48011 | (1.30) | 38188 | (1.50) | 16705 | (1.36) | 10912 | (1.59) | 25328 | (1.64) |
| 14. Unemployed population 16+ y.o | 326997 | (5.80) | 271469 | (6.45) | 112085 | (6.44) | 58023 | (6.17) | 168026 | (7.57) |
| 15. Homeowner HHs: No vehicle | 35803 | (1.83) | 28476 | (1.67) | 18393 | (2.12) | 11698 | (2.47) | 31194 | (3.14) |
| 16. Renter HHs: No vehicle | 181444 | (10.53) | 78655 | (9.34) | 36187 | (10.05) | 25654 | (11.94) | 64899 | (11.87) |
| Insurance | ||||||||||
| 17. Pop <19: No health insurance | 256337 | (2.56) | 250818 | (3.21) | 92895 | (2.73) | 55493 | (2.95) | 181554 | (3.88) |
| 18. Pop 19-34: No health insurance | 633154 | (6.33) | 478565 | (6.12) | 181520 | (5.32) | 114723 | (6.09) | 395938 | (8.47) |
| 19. Pop 35-64: No health insurance | 693515 | (6.93) | 575627 | (7.36) | 233130 | (6.84) | 139156 | (7.39) | 445590 | (9.53) |
| 20. Pop 65+: No health insurance | 24315 | (0.24) | 19250 | (0.25) | 4737 | (0.14) | 1874 | (0.10) | 12944 | (0.28) |
Note: NH = Non-Hispanic; HHs = Households; Pop = Population.
Figure 3:
Four concentric drive time rings around specialist providers’ locations in varying travel time increments from 1 minute drive time to 2 hours. Areas outside the concentric rings are > 2hr drive time.
DISCUSSION
Cognitive-behavioral therapy for OCD is an effective treatment but numerous barriers limit access. This report examined geographic access to CBT for OCD in Texas with regards to how specialty treatment locations are related to neighborhood socioeconomic, rural/urban, payer type, and provider age expertise. Broadly, findings confirm clinical experience indicating that CBT providers are clustered in large socially advantaged areas within large cities and are largely self-pay. The vast majority of OCD specialists were located in the four largest cities in Texas with no representation in rural areas, smaller cities, or on the Mexican border.
While COVID-19 has normalized use of telepsychiatry services, some individuals do not desire or find this approach appropriate for their condition, and technical issues such as insufficient internet connectivity are also a potential concern. Others may not think to contact a clinic outside of their immediate surroundings relative to a local provider. Indeed, mental health access is broadly problematic in Texas where many counties have very few general mental health providers, let alone OCD specialists. Collectively, this may severely limit treatment access, which is of concern as, like other conditions [40], inadequate or inappropriate treatment of OCD is likely to result in sustained and impairing symptoms [8-10]. This issue may be even more pronounced for those that only speak Spanish (or another non-English language), with very few providers available, thus perpetuating service disparities for sufferers of minority status.
Despite the availability of specialty practices, about half of clinics were self-pay and did not accept insurance. Most specialty practices were located in more affluent areas, especially those that only accept self-pay status. Indeed, cost remains a significant barrier to care for mental health intervention access [41, 42], and our data indicate that individuals with OCD in Texas are likely to experience this barrier. Further, insurance reimbursement rates are often insufficient to cover costs for practitioners compelling providers to limit 3rd party contracting. Scalable but effective interventions to improve access are clearly warranted, especially focusing on less affluent, rural, and non-English speaking areas and populations. To expand the reach of best-practice treatments for OCD, experts and professionals could engage with policymakers and advocates to implement stronger dissemination efforts, relying on professional training, digitally administered interventions and training programs, and other cost-effective solutions
We highlight two study limitations. First, we relied on self-reported clinical expertise without independent verification. Second, our analysis was limited to Texas, and did not consider specialist OCD treatment in neighboring states. On balance, we anticipate this pattern of findings to be relevant across the U.S.
Overall, conducting our ADI analysis at the census tract (neighborhood level) is an important contribution to the epidemiology of OCD care in Texas. Over the last decade, scholars have argued for and validated the importance of examining the impact of “place-based” socioenvironmental factors on health outcomes [43, 44]. In fact, we are not aware of any previous studies that examined OCD care access in Texas as we have done here. Our study provides evidence that geospatial analysis can be a powerful tool for determining neighborhood level correlates of OCD care access. Understanding health disparities through spatial processes provides the ability to understand spatial and spatially-driven structures that influence the exposure-disease relationships. The utility of geospatial analytics and processes in this regard provides insight into neighborhood-level drivers of disease outcomes that may otherwise remain unknown. On the other hand, when used optimally, findings of locally varying relationships may provide information to effectuate holistic policy prescriptions that are often operationalized in geographical space [45].
Supplementary Material
Highlights.
CBT is efficacious for OCD but access is often limited.
We examined the geographic distribution of OCD specialty providers in Texas.
Specialist providers are almost exclusively located in affluent urbanized areas.
Average household income decreased as distance from specialist providers increased.
Economic disadvantage remains a significant barrier to care.
Acknowledgements
We are grateful to several colleagues across the authors’ home departments and centers at the Baylor College of Medicine for their support during the COVID-19 pandemic.
Funding
OS work on this paper was supported by Fulbright and the Leifur Eiriksson Foundation. Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number P50HD103555 for use of the Clinical and Translational Core facilities. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethics approval and consent to participate
The protocol for this study did not require institutional review board review nor approval as it leveraged publicly available data without engaging any individuals in procedures.
Consent for publication
This manuscript does not contain any individual person’s data in any form.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
Ms. Christian, Mr. Smarason and Dr. Schneider report no disclosures. Dr. Goodman has received research support from Brainsway, Biohaven Pharmaceutics and the NIH; Medtronic donated devices to a research project; and he received consulting fees from Biohaven and Neurocrine Biosciences. Dr. Storch reports personal fees from Elsevier, personal fees from Wiley, personal fees from Springer, personal fees from American Psychological Association, personal fees from Jessica Kingsley, personal fees from Lawrence Erlbaum, personal fees from Oxford, grants from Greater Houston Community Foundation, grants from ReBuild Texas, grants from NIH, grants from Texas Higher Education Coordinating Board, personal fees from Biohaven Pharmaceutics and Levo Therapeutics, personal fees from International OCD Foundation, outside the submitted work. He holds stock in NView.
Given their role as an Editorial Board Member (EAS), and Associate Editor (WKG), Eric Storch and Wayne Goodman had no involvement in the peer-review of this article and had no access to information regarding its peer-review.
REFERENCES
- 1.Markarian Y, et al. , Multiple pathways to functional impairment in obsessive–compulsive disorder. Clinical Psychology Review, 2010. 30(1): p. 78–88. [DOI] [PubMed] [Google Scholar]
- 2.Ruscio AM, et al. , The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry, 2010. 15(1): p. 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGuire JF, et al. , A meta-analysis of cognitive behavior therapy and medication for child obsessive–compulsive disorder: Moderators of treatment efficacy, response, and remission. Depression and Anxiety, 2015. 32(8): p. 580–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Öst L-G, et al. , Cognitive behavioral treatments of obsessive–compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clinical Psychology Review, 2015. 40: p. 156–169. [DOI] [PubMed] [Google Scholar]
- 5.de Vries YA, et al. , Initial severity and antidepressant efficacy for anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder: An individual patient data meta-analysis. Depression and Anxiety, 2018. 35(6): p. 515–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geller DA, March JS, and American Academy of Child and Adolescent Psychiatry Committee on Quality Issues, Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 2012. 51(1): p. 98–113. [DOI] [PubMed] [Google Scholar]
- 7.National Institute for Health and Clinical Excellence, Obsessive-compulsive disorder: core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder. 2005. [Google Scholar]
- 8.García-Soriano G, et al. , Factors associated with non-treatment or delayed treatment seeking in OCD sufferers: a review of the literature. Psychiatry Research, 2014. 220(1-2): p. 1–10. [DOI] [PubMed] [Google Scholar]
- 9.Poyraz CA, et al. , Factors associated with the duration of untreated illness among patients with obsessive compulsive disorder. Comprehensive Psychiatry, 2015. 58: p. 88–93. [DOI] [PubMed] [Google Scholar]
- 10.Marques L, et al. , Barriers to treatment and service utilization in an internet sample of individuals with obsessive–compulsive symptoms. Depression and Anxiety, 2010. 27: p. 470–475. [DOI] [PubMed] [Google Scholar]
- 11.Brakoulias V, et al. , Treatments used for obsessive–compulsive disorder—An international perspective. Human Psychopharmacology: Clinical and Experimental, 2019. 34(1): p. e2686. [DOI] [PubMed] [Google Scholar]
- 12.Lewin AB, et al. , The importance of considering parent's preferences when planning treatment for their children–the case of childhood obsessive-compulsive disorder. J Child Psychol Psychiatry, 2014. 55(12): p. 1314–6. [DOI] [PubMed] [Google Scholar]
- 13.Patel SR and Simpson HB, Patient Preferences for OCD treatment. The Journal of Clinical Psychiatry, 2010. 71(11): p. 1434–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartz C, et al. , Treatment-seeking in OCD community cases and psychological treatment actually provided to treatment-seeking patients: A systematic review. Journal of Obsessive-Compulsive and Related Disorders, 2013. 2(4): p. 448–456. [Google Scholar]
- 15.Fineberg NA, et al. , Early intervention for obsessive compulsive disorder: An expert consensus statement. European Neuropsychopharmacology, 2019. [DOI] [PubMed] [Google Scholar]
- 16.Williams MT, et al. , Barriers to treatment among African Americans with obsessive-compulsive disorder. Journal of anxiety disorders, 2012. 26(4): p. 555–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gentle M, Harris LM, and Jones MK, The Barriers to Seeking Treatment for Obsessive-Compulsive Disorder in an Australian Population. Behaviour Change, 2014. 31 (4): p. 258–278. [Google Scholar]
- 18.Glazier K, et al. , Stigma and shame as barriers to treatment for Obsessive-Compulsive and Related Disorders. Journal of Depression and Anxiety, 2015. 4(3): p. 191. [Google Scholar]
- 19.Sharma R, et al. , Geographic Distribution of California Mental Health Professionals in Relation to Sociodemographic Characteristics. Cultur Divers Ethni Minor Psychol, 2017. 23(4): p. 595–600. [DOI] [PubMed] [Google Scholar]
- 20.Kim G, et al. , Geographic variation in mental health care disparities among racially/ethnically diverse adults with psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology, 2017. 52(8): p. 939–948. [DOI] [PubMed] [Google Scholar]
- 21.Andrilla CHA, et al. , Geographic Variation in the Supply of Selected Behavioral Health Providers. American Journal of Preventive Medicine, 2018. 54(6, Supplement 3): p. S199–S207. [DOI] [PubMed] [Google Scholar]
- 22.Adler NE and Rehkopf DH, U.S. Disparities in Health: Descriptions, Causes, and Mechanisms. Annual Review of Public Health, 2008. 29(1): p. 235–252. [DOI] [PubMed] [Google Scholar]
- 23.Macintyre S and Ellaway A, Neighborhoods and health: an overview. Neighborhoods and health, 2003. 20: p. 42. [Google Scholar]
- 24.Adler NE, et al. , Addressing social determinants of health and health disparities: A vital direction for health and health care. NAM Perspectives, 2016. [Google Scholar]
- 25.Haskins J, Healthy People 2030 to create objectives for health of nation: Process underway for next 10-year plan. 2017, American Public Health Association. [Google Scholar]
- 26.Organization, W.H., Our cities, our health, our future: acting on social determinants for health equity in urban settings. Report to the WHO Commission on Social Determinants of Health from the Knowledge Network on Urban Settings. Our cities, our health, our future: acting on social determinants for health equity in urban settings. Report to the WHO Commission on Social Determinants of Health from the Knowledge Network on Urban Settings., 2008. [Google Scholar]
- 27.Robert SA, Socioeconomic position and health: the independent contribution of community socioeconomic context. Annual review of sociology, 1999. 25(1): p. 489–516. [Google Scholar]
- 28.Singh GK, Area deprivation and widening inequalities in US mortality, 1969–1998. American journal of public health, 2003. 93(7): p. 1137–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wardle J, et al. , Socioeconomic disparities in cancer-risk behaviors in adolescence: baseline results from the Health and Behaviour in Teenagers Study (HABITS). Preventive medicine, 2003. 36(6): p. 721–730. [DOI] [PubMed] [Google Scholar]
- 30.Butler DC, et al. , Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health services research, 2013. 48(2pt1): p. 539–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sturm R, Ringel JS, and Andreyeva T, Geographic disparities in children’s mental health care. Pediatrics, 2003. I12(4): p. e308–e308. [DOI] [PubMed] [Google Scholar]
- 32.Clarke KC, McLafferty SL, and Tempalski BJ, On epidemiology and geographic information systems: a review and discussion of future directions. Emerging infectious diseases, 1996. 2(2): p. 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Delmelle EM, et al. , Modeling travel impedance to medical care for children with birth defects using Geographic Information Systems. Birth Defects Research Part A: Clinical and Molecular Teratology, 2013. 97(10): p. 673–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McLafferty SL, GIS and health care. Annual review of public health, 2003. 24(1): p. 25–42. [DOI] [PubMed] [Google Scholar]
- 35.Salciccioli KB, et al. , A model for geographic and sociodemographic access to care disparities for adults with congenital heart disease. Congenital heart disease, 2019. 14(5): p. 752–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Management, U.O.o. and Budget, 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas: Notice. Federal Register, 2010. 75(123): p. 37246–52. [Google Scholar]
- 37.America, T.A.N. and I. ESRI, US Core Based Statistical Areas. 2006. [Google Scholar]
- 38.Census. American Community Survey Information Guide. 2017. [cited 2019 April 20]; Available from: https://www.census.gov/content/dam/Census/programs-surveys/acs/about/ACS_Information_Guide.pdf. [Google Scholar]
- 39.Knighton AJ, et al. , Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. eGEMs, 2016. 4(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Swindle RW JR, Cronkite RC, and Moos RH, Risk factors for sustained nonremission of depressive symptoms: a 4-year follow-up. The Journal of nervous and mental disease, 1998. 186(8): p. 462–469. [DOI] [PubMed] [Google Scholar]
- 41.Salloum A, et al. , Barriers to access and participation in community mental health treatment for anxious children. Journal of Affective Disorders, 2016. 196: p. 54–61. [DOI] [PubMed] [Google Scholar]
- 42.Rowan K, McAlpine DD, and Blewett LA, Access and cost barriers to mental health care, by insurance status, 1999–2010. Health affairs, 2013. 32(10): p. 1723–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cummins S., et al. , Understanding and representing ‘place’in health research: a relational approach. Social science & medicine, 2007. 65(9): p. 1825–1838. [DOI] [PubMed] [Google Scholar]
- 44.Janssen I, et al. , Influence of individual-and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. The American journal of clinical nutrition, 2006. 83(1): p. 139–145. [DOI] [PubMed] [Google Scholar]
- 45.Kearns R, Moon G, From medical to health geography: novelty, place and theory after a decade of change. Prog Hum Geogr:2002: 26(5), 605–625. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.