Abstract
Context.—
The most common benign hepatic mass-forming lesions often display fairly specific imaging characteristics, whereas less familiar, rarer benign neoplasms and pseudotumors may pose a diagnostic challenge in clinical, radiology, and pathology practice because of either their rarity or their unusual features.
Objective.—
To review a selection of pseudotumors and unusual benign hepatic neoplasms encountered in consultation practices with a focus on nonepithelial tumors.
Data Sources.—
Sources include English-language literature and personal experiences.
Conclusions.—
Several benign conditions (namely, segmental atrophy, infections, immunoglobulin G4 [IgG4]–related sclerosing disease, angiomyolipoma, mesenchymal hamartoma, and various vascular lesions) can lead to formation of hepatic masses. Because of their rarity and underrecognition, such lesions are often diagnostically challenging. Awareness of hepatic pseudotumors and various rare hepatic neoplasms and their potential mimics can forestall misdiagnosis and inappropriate management.
Myriad benign hepatic mass-forming lesions can be found and characterized by their radiologic features. However, despite advances in imaging techniques, the less frequently encountered hepatic tumors may pose a diagnostic challenge because of their less specific imaging findings or their rarity.
Mass-forming hepatic pseudotumors are rare nonneoplastic lesions that can mimic neoplasm clinically. There are several rare hepatic pseudotumors, such as segmental atrophy, infections, immunoglobulin G4 (IgG4)–related sclerosing disease (IgG4-RSD), Rosai-Dorfman disease (RDD), and regenerative hepatic pseudotumor (RHP) that may pose diagnostic dilemmas for clinicians and pathologists alike (Table 1). Similarly, rare, benign hepatic neoplasms, such as hepatic angiomyolipoma, mesenchymal hamartoma, and variants of hemangioma, can be diagnostically challenging because of their atypical imaging characteristics. Awareness of hepatic pseudotumors and various rare hepatic neoplasms and their potential mimics can forestall misdiagnosis and inappropriate management. Therefore, in this review we aim to provide an overview of a selection of pseudotumors and unusual benign hepatic neoplasms (with a focus on nonepithelial lesions).
Table 1.
Summary of Hepatic Pseudotumors
| Pseudotumors | Brief Description and Hallmarks |
|---|---|
| Segmental atrophy | Abnormal vessels Collapsed hepatic parenchyma Elastosis |
| IgG4-related sclerosing disease | Fibroinflammatory process Storiform fibrosis Obliterative phlebitis IgG4-enriched lymphoplasmacytic infiltrate |
| Rosai-Dorfman disease | Fibroinflammatory process Emperipolesis Increased IgG4+ plasma cells Arteries more affected than veins S100 protein highlights the lesional cells |
| Inflammatory pseudotumor-like follicular/fibroblastic dendritic cell sarcoma | Young to middle-aged adults Spindle cells heavily admixed with inflammatory cells Fibrinoid deposits in the vessel wall At least 1 follicular dendritic cell marker is positive (CD21/CD35, CD23) Epstein-Barr virus–encoded early nuclear RNAs in situ hybridization positive |
| Syphilis | High-risk population (human immunodeficiency virus, men who have sex with men) Fibroinflammatory process Plasma cell–rich fibroblastic proliferation with abscesses Granulomas, Kupffer cell hyperplasia, and portal edema with pericholangitis or cholangitis in the surrounding liver Positive Treponema pallidum immunohistochemistry |
| Regenerative hepatic pseudotumor | Sinusoidal dilatation Vascular thrombosis Bile ductular proliferation No or focal elastosis |
| Echinococcosis (hydatid disease) | Infection with the tapeworm Echinococcus Zoonotic infection Hepatic echinococcosis involves the liver in 2 basic patterns:
|
Abbreviation: IgG4, immunoglobulin G4.
PSEUDOTUMORS
Segmental Atrophy
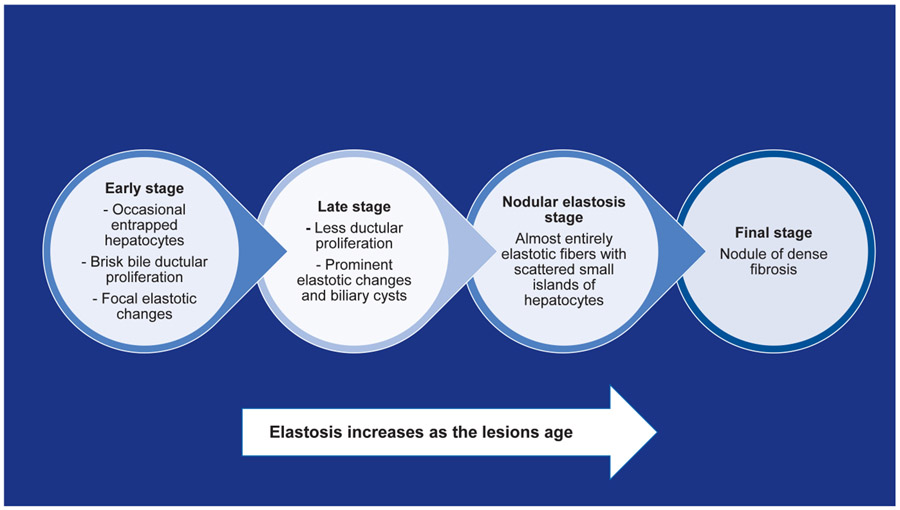
Segmental atrophy (SA) of the liver is a rare and underrecognized benign entity with only a few reported series. SA can present as a mass lesion, posing a diagnostic challenge for radiologists and pathologists alike. Clinicopathologic characteristics remain poorly described, and radiologists, hepatologists, and surgeons are often unaware and ill-prepared to deal with this clinical entity. The etiology of SA is not precisely known, and it is not entirely clear why these lesions develop. Some speculate that they result from a form of vascular injury, such as local thrombosis of a vessel feeding a smaller subsegment of the liver, leading to ischemic parenchymal extinction and loss of hepatocytes. SA was originally described by Singhi et al,1 wherein they described the clinicopathologic features of 18 cases. SA predominantly arises in middle-aged adults, with a slight female predominance. Although exceedingly rare, SA has been reported in children.2 Data from an unpublished study showed that SA has a strong association with longstanding cardiovascular disease and is rarely associated with connective tissue disorders.3 The lesions are often subcapsular and can range in size from 1.7 to 10 cm.1,3 Histologically, depending on the stage of the lesion, SA displays a morphologic spectrum. In the early stages, there are occasional entrapped hepatocytes, a brisk bile ductular proliferation, and focal elastotic changes. As the lesions age, the bile ductular proliferation decreases, and elastosis increases. In the final stages, SA demonstrates nodules of dense fibrosis (Figure 1).
Figure 1.
Segmental atrophy stages.
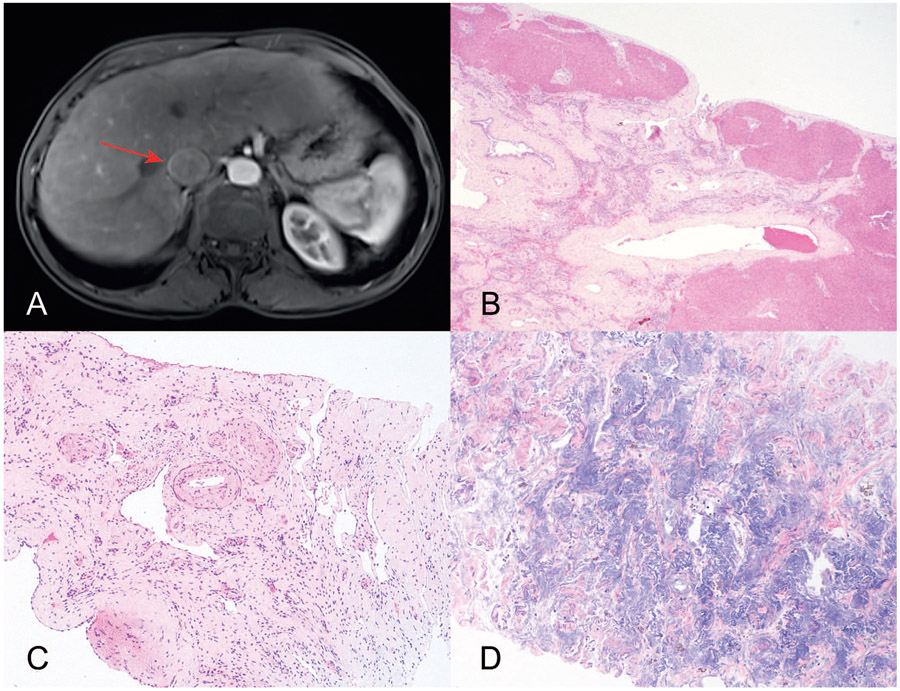
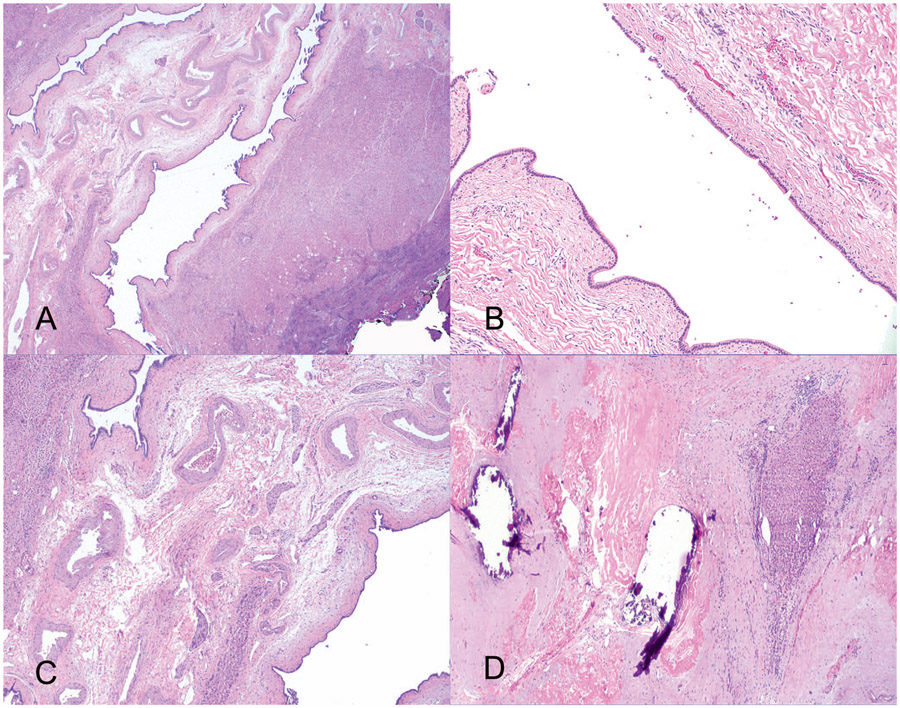
The most striking histologic feature in SA is the presence of abnormally thick-walled blood vessels throughout the lesion (Figure 2). Other salient features include dilated bile ducts and biliary cysts. The biliary cysts, if large, can sometimes be clinically concerning for mucinous cystic neoplasm or intraductal papillary neoplasm of bile ducts (Figure 3). A simple hepatic cyst or a solitary bile duct cyst secondary to a limited form of ductal plate malformation is another potential differential diagnosis because of their morphologic similarity to the biliary retention cyst in SA. Regenerative hepatic pseudotumor is another recently described pseudotumor caused by vascular flow changes, but it differs from segmental atrophy morphologically. The vascular changes in regenerative hepatic pseudotumor are associated with reactive parenchymal changes, including sinusoidal dilation, patchy bile ductular proliferation, and portal vein abnormalities, but, unlike SA, elastosis is absent or only focally present.4 In Table 2, we have listed the potential differential diagnosis of segmental atrophy based on the suggestion of the contributing pathologists at the time of consultation. However, in practice, the noted entities are often easily distinguishable from SA, except perhaps in limited samples.
Figure 2.
Segmental atrophy (SA). A, Magnetic resonance image shows an abnormal appearance of the inferior right hepatic lobe/portions of segment 6 near the gallbladder fossa (arrow), with a subtle area of focal capsular retraction concerning for cholangiocarcinoma. B, Histologic examination shows a subcapsular lesion showing residual entrapped hepatocytes, inflammation, and bile ductular proliferation. C, SA at its later stages shows increased elastosis as well as thick-walled blood vessels. D, Elastin stain highlights the elastic fibers (hematoxylin-eosin, original magnifications ×2 [B] and ×10 [C]; elastin, original magnification ×400 [D]).
Figure 3.
Segmental atrophy (SA). This is an 11-cm subcapsular lesion clinically concerning for mucinous cystic neoplasm or intraductal papillary neoplasm of bile ducts. A and B, At low magnification, a retention-type biliary cyst, lined with bland biliary-type epithelium without ovarian-type stroma, dominates the histology at least focally suggesting other types of cystic biliary tract disease. C and D, Adjacent to the cyst and in other areas of the lesion, classic features of SA with thick-walled blood vessels and elastosis are seen (hematoxylin-eosin, original magnifications ×2 [A], ×10 [B], ×100 [C], and ×200 [D]).
Table 2.
Differential Diagnosis of Segmental Atrophy
Cystic changes predominate
|
Elastosis predominates
|
Awareness of multiple stages of SA and recognizing its various morphologies allow for accurate diagnosis.
IgG4-Related Sclerosing Disease
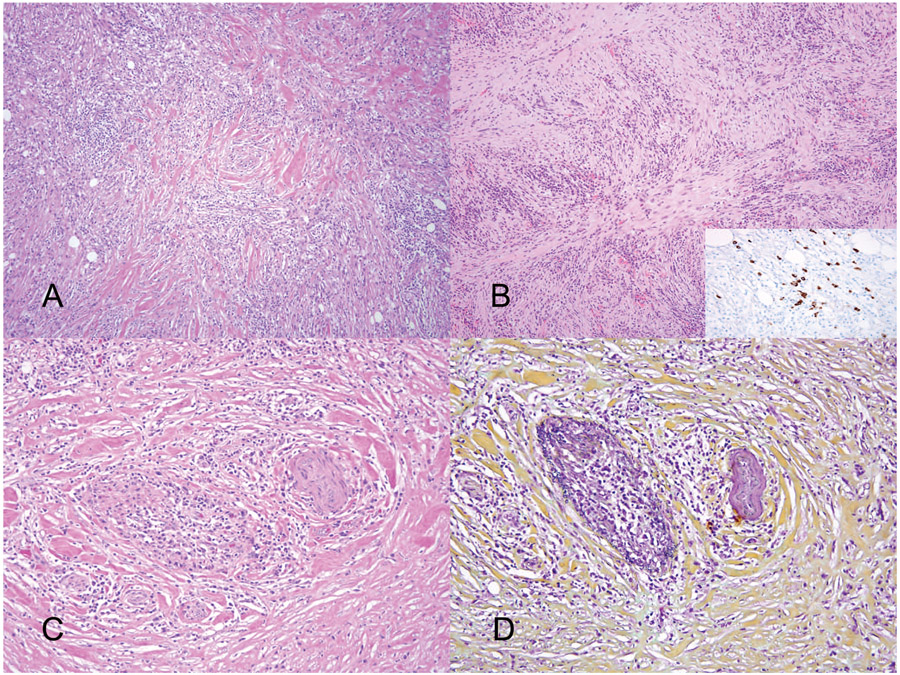
IgG4-RSD is a chronic fibroinflammatory disease affecting various organs, including salivary glands, thyroid, pancreas, bile ducts, and, less commonly, liver. Previously, the manifestations in each organ system were classified as unrelated diseases (eg, type 1 autoimmune pancreatitis, Riedel thyroiditis, Küttner tumor [submandibular gland], and Mikulicz disease [salivary and lacrimal glands]). However, affected patients often had lesions in multiple organs and expressed high levels of serum IgG4, which led to the unification of these diseases under the IgG4-RSD umbrella.5 Although there are clinical diagnostic criteria for IgG4-RSD (such as serum IgG4 levels >135 mg/dL), histologic evaluation remains the gold standard for the diagnosis. Normal IgG4 levels do not exclude the diagnosis of IgG4-related disease because serum IgG4 concentrations are normal in approximately 10% to 40% of patients with IgG4-RSD.6,7 Histologically, hepatic IgG4-RSD can range from mild nonspecific portal inflammation to sclerosing cholangitis and inflammatory pseudotumor. Classic histologic appearance based on Boston consensus criteria includes storiform fibrosis, obliterative phlebitis, and IgG4-enriched lymphoplasmacytic infiltrate.7 Immunohistochemistry can support the diagnosis when there are increased IgG4+ cells for which the cut points vary in different organs (Figure 4). For the liver or bile ducts, the suggested cut points are greater than 50 IgG4+ cells per high-power field (HPF) for surgical resection specimens and greater than 10 IgG4+ cells per HPF for biopsies.7 Another supporting immunohistochemistry finding is an IgG4/IgG ratio of greater than 40%. This can be problematic in practice because the IgG immunostain typically shows high background staining. The current recommendations are to count 3 HPFs with the highest density of IgG4+ plasma cells and use these same 3 fields for IgG+ counts to generate the IgG4/IgG ratio.8 Although immunohistochemistry can support the diagnosis, one should not be overly reliant on IgG immunohistochemistry for the diagnosis. Multiple studies have shown that elevated serum IgG4 and increased numbers of IgG4+ plasma cells can be seen in the setting of biliary tract carcinomas, primary sclerosing cholangitis, and RDD.9,10 Thus, an undersampled bile duct carcinoma or primary sclerosing cholangitis may be misdiagnosed as IgG4-RSD if a pathologist is overly reliant on the IgG4+ cell count. While steroid-responsive, IgG4-RSD conveys risk for progressive fibrosis and eventually cirrhosis. RDD is a key differential diagnosis of IgG4-RSD because of the presence of vasculopathy and increased IgG4+ plasma cells. RDD is a rare non–Langerhans cell histiocytic proliferation that can manifest in nodal and extranodal sites. Involvement of the gastrointestinal tract and especially liver is exceedingly rare. Emperipolesis, although nonspecific, is a helpful diagnostic feature. In general, arteries are more likely to be affected in RDD in contrast to obliterative phlebitis of IgG4-RSD, and immunostaining with S100 protein is a useful tool for confirming the diagnosis (Figure 5).11
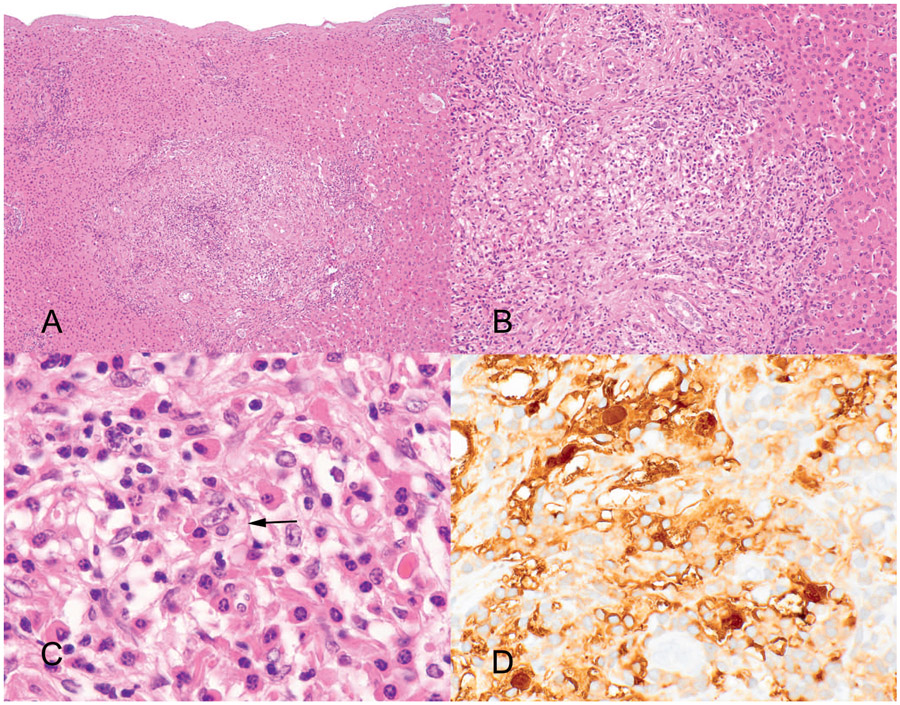
Figure 4.
Immunoglobulin G4 (IgG4)–related sclerosing disease. A, Low magnification shows a fibroinflammatory lesion with areas of storiform fibrosis. B, Numerous plasma cells express IgG4 on immunostain (inset). C and D, Obliterative phlebitis is characterized by a damaged vein adjacent to an artery, as highlighted on (D) Movat stain (hematoxylin-eosin, original magnifications ×2 [A] and ×10 [B and C]; IgG4 immunostain, original magnification ×400 [B, inset]; original magnification ×400 [D]).
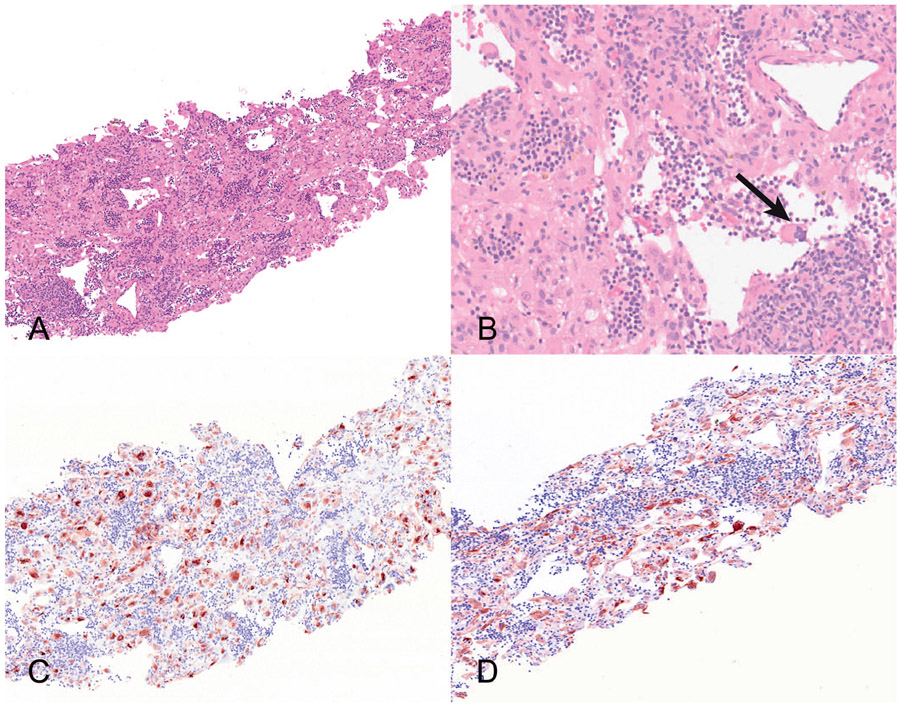
Figure 5.
Rosai-Dorfman disease (RDD) involving the liver. A, Low magnification shows a fibroinflammatory process predominantly centered within the portal tracts. B, Higher magnification shows a mixed inflammatory infiltrate rich in histiocytes and plasma cells. C, Emperipolesis is indicated by the arrow. D, Strong S100 protein reactivity with prominent emperipolesis. The ingested lymphocytes appear pale within the stained cytoplasm of the lesional histiocytes. The nuclei of the RDD cells express S100 protein (hematoxylin-eosin, original magnifications ×10 [A], ×100 [B], and ×200 [C]; S100 immunostain, original magnification ×400 [D]).
Inflammatory myofibroblastic tumor displays overlapping features with those of IgG4-RSD and is often replete with IgG4+ plasma cells. Most cases, but not all, can be separated with the use of immunohistochemistry for ALK1 and ROS1 and searching for obliterative phlebitis. A subset of cases requires application of a next-generation sequencing–based assay that covers known inflammatory myofibroblastic tumor fusions to confirm the diagnosis.12
A rare subset of inflammatory Epstein-Barr virus-driven lesions has been reported in the liver and spleen as “inflammatory pseudotumor-like follicular/fibroblastic dendritic cell sarcoma (IPT-like FDCS).” Such tumors arise in young to middle-aged adults and are characterized by spindle cells in an inflammatory background. The blood vessels in the tumors frequently have fibrinoid material deposited in their walls (Figure 6). It is not clear whether these lesions are in fact follicular dendritic cell neoplasms because CD23 can be absent. These tumors can recur, sometimes multiple times, but are overall believed to be indolent.13
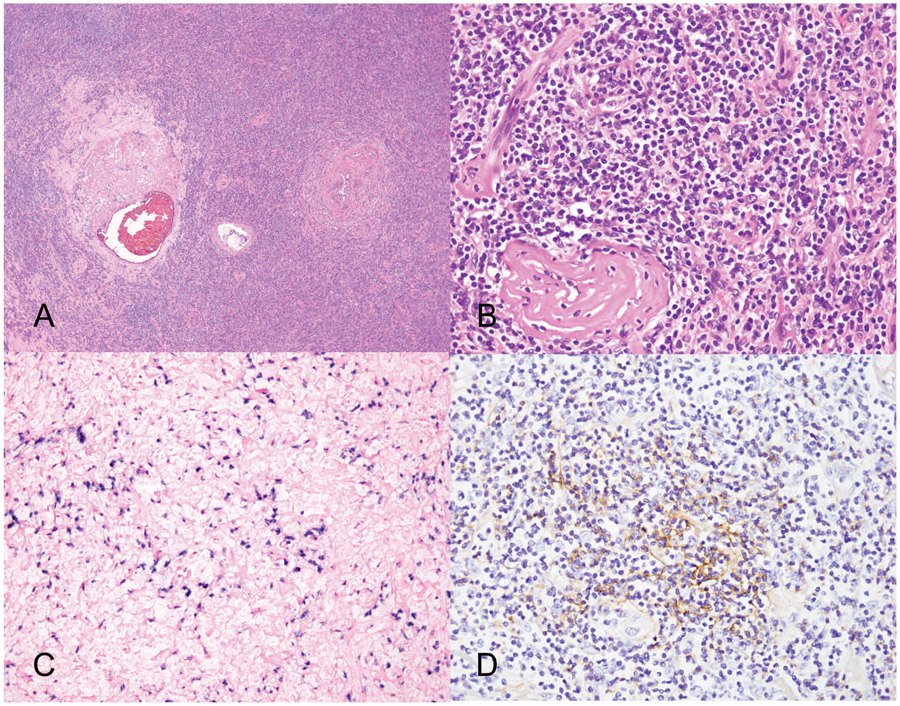
Figure 6.
Inflammatory pseudotumor-like follicular/fibroblastic dendritic cell sarcoma. A and B, The lesion is composed of spindle cells heavily admixed with lymphocytes, histiocytes, and plasma cells. Note the fibrinoid deposits in the wall of blood vessels. C, Immunostaining for CD21 shows focal, patchy staining. D, The spindle cells showed strong nuclear in situ labeling for Epstein-Barr virus–encoded early nuclear RNAs (EBER), whereas the background inflammatory cells are uniformly negative (hematoxylin-eosin, original magnifications ×10 [A] and ×200 [B]; CD21 immunostain, original magnification ×200 [C]; EBER in situ hybridization, original magnification ×200 [D]).
Syphilis
A variety of infections can present as hepatic pseudotumors. Although rare, syphilis is an important infectious cause of inflammatory pseudotumor and should always be considered in the differential diagnosis, especially when evaluating biopsies from high-risk populations, such as human immunodeficiency virus (HIV) patients and men who have sex with men.14 The presumed mechanism of hepatic infection in HIV patients is from portal invasion of organisms after anorectal infection as a result of portal venous drainage of the rectum.11 The liver can be involved in all stages of syphilis. Late syphilis can present with mass lesions formed by gummas or inflammatory pseudotumors mimicking neoplasms, particularly metastases.15,16 Gummas are rarely encountered but are characterized by a central zone of coagulative necrosis and a surrounding rim of fibroinflammatory tissue. When hepatic syphilis presents as an inflammatory pseudotumor, histologic clues include the presence of a plasma cell–rich fibroblastic proliferation with abscesses, granulomas, Kupffer cell hyperplasia, and portal edema with pericholangitis or cholangitis in the surrounding liver (Figure 7). The differential diagnosis in such cases revolves around the entities discussed in the section above concerning IgG4-related disease.
Figure 7.
Syphilis presenting as a liver pseudotumor. A, Low magnification shows a fibroinflammatory process. B, Higher magnification shows the abundance of plasma cells in the inflammatory infiltrate. C, Scattered mild lobular lymphocytic and neutrophilic inflammation in the background liver. D, Treponema pallidum immunostain reveals the presence of spiral organisms (hematoxylin-eosin, original magnifications ×2 [A] and ×10 [B and C]; original magnification ×400 [D]). Images courtesy of Lysandra Voltaggio, MD.
Immunohistochemistry for Treponema pallidum can be a powerful tool in the diagnosis of syphilis. However, a negative stain does not exclude the diagnosis when the morphology and clinical circumstances support it. Typically, when the immunostain is positive, the organisms are concentrated in the areas of the mass lesion and not the background liver. Therefore, a negative immunostain may represent an undersampled mass lesion.14 Congenital syphilis can present with diffuse sinusoidal fibrosis or a giant cell hepatitis pattern.
Echinococcosis (Hydatid Disease)
Hydatid disease is the most common cause of hepatic cysts worldwide and is caused by infection with the larval stage of the tapeworm Echinococcus. It is a zoonotic infection in which humans are infected by exposure to contaminated feces of primary or intermediate hosts. Although not endemic in the United States, cases are occasionally encountered in the United States and central Europe.17,18 The cysts are slow-growing and therefore are often asymptomatic for years.19 Hepatic echinococcosis involves the liver in 2 basic patterns. Echinococcus granulosus is the most common and causes slow-growing cystic lesions that can attain sizes of up to 30 cm in diameter and is most commonly encountered in individuals raising sheep. The cysts often contain several daughter cysts. Echinococcus multilocularis is the alveolar form, which is transmitted by contact with wild animals and has a more aggressive clinical course; it can invade and destroy infected liver, induce a tumorlike growth, and mimic malignancy.20 The cysts are often multilocular, and the cystic cavities contain thick, pasty material. The cysts of E granulosus, if well preserved, are composed of 3 structural components: innermost germinal membrane, a middle hyalinized laminated layer, and an outer layer of hyalinized fibrosis. Echinococcus multilocularis, on the other hand, can show a range of findings, from small cysts to necrotizing granulomatous inflammation without well-formed cyst walls. Trichrome stains, periodic acid–Schiff stain, or Grocott methenamine silver stains can highlight the degenerating parasite forms (Figure 8). Relatively recently, Reinehr et al18 developed an algorithm for not only diagnosing echinococcosis but also using a combination of morphologic and immunohistochemical criteria to discriminate between cystic echinococcosis (CE) and alveolar echinococcosis (AE). Six morphologic criteria that discriminated between cystic and alveolar echinococcosis were: size of smallest (CE/AE, >2/≤2 mm) and largest cyst (CE/AE, >25/≥25 mm), thickness of laminated layer (CE/AE, >0.15/≤0.15 mm) and pericystic fibrosis (CE/AE, >0.6/≤0.6 mm), striation of laminated layer (CE/AE, moderate-strong/weak), and number of cysts (CE/AE, ≤9/>9). Immunostaining with either of 2 novel antibodies (mAbEm2G11 [E multilocularis specific] and mAbEmG3 [reactive in AE and CE]) showed specificity equal to the authors’ routine morphologic criteria.18
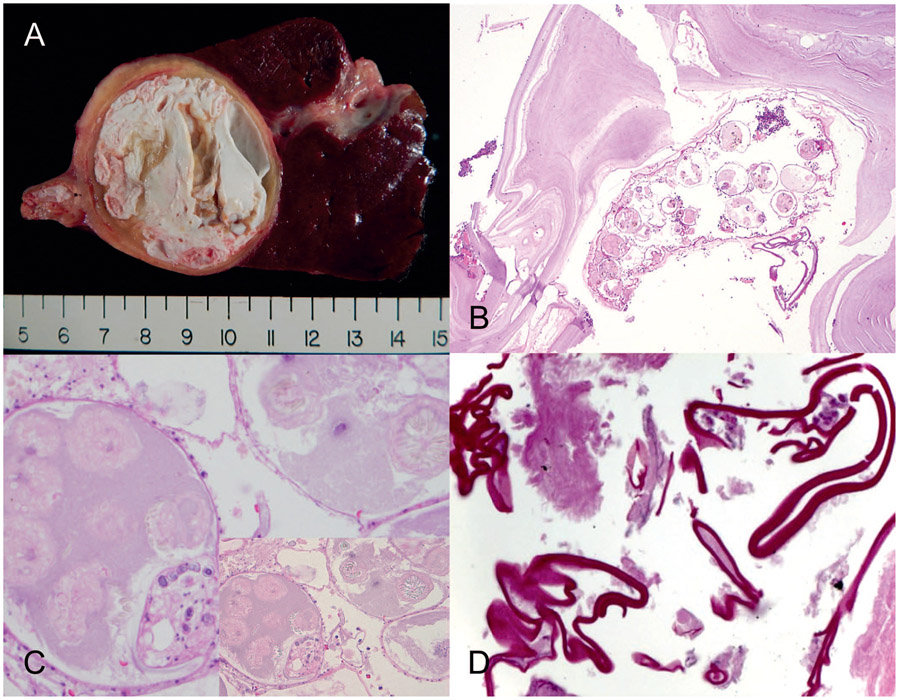
Figure 8.
Echinococcosis granulosus. A, The wedge resection shows a unilocular cystic lesion with a fibrous rim filled with grungy white material. B, Histologic sections showed predominantly acellular hyalinized material and remnants of degenerated parasites with smaller daughter cysts. C, Higher magnification shows refractile hooklets, which are best seen with the condenser down and with refracted light (inset). D, Periodic acid–Schiff stain highlighting the cyst wall (hematoxylin-eosin, original magnifications ×10 [B] and ×200 [C]; original magnification ×200 [D]). Images courtesy of Michael Feely, DO.
RARE BENIGN NEOPLASMS
Hepatic Angiomyolipoma
Hepatic angiomyolipoma (AML) is a rare benign neoplasm, and liver is the second most frequent site of involvement after the kidney. AML has a strong predilection for adult females.21 In contrast to renal examples, most hepatic AMLs are sporadic and only rarely associated with tuberous sclerosis (TS).22 However, tested hepatic AMLs nearly invariably harbor TSC2 mutations as the driver mutation.23 AMLs show differentiation along the lines of perivascular epithelioid cells and are considered part of the perivascular epithelioid cell family.24 Grossly, they often present as nonencapsulated, well-circumscribed solitary lesions in a background of noncirrhotic liver. As the name implies, they are composed of varying amounts of smooth muscle–type cells, adipose tissue (can be fat poor or fat predominant), and blood vessels. The myoid component is the most specific for diagnosis. About 40% of cases show extramedullary hematopoiesis (Figure 9).24 The presence of clusters of foamy macrophages can be a useful diagnostic clue in difficult cases.23 AMLs are easy to recognize when all 3 components are present but can be confused with many entities when only 1 component is present. For example, myoid cells, either epithelioid or spindled, can be the only cell type, which can cause confusion with hepatic adenoma, hepatocellular carcinoma, malignant melanoma, smooth muscle tumors, and metastatic gastrointestinal stromal tumor. Almost half of the cases in a study by Tsui et al25 were initially misdiagnosed as carcinomas or sarcomas. Fortunately, the mimics can be reliably excluded when histology is combined with immunohistochemistry. HMB-45 and Melan-A are positive in AMLs, whereas cytokeratin, HepPar1, and other hepatocellular markers are negative. However, there are important pitfalls of which to be aware. When hepatic epithelioid AML resembles hepatocellular adenoma and hepatocellular carcinoma, immunohistochemistry can be deceptive. AML can show an absence of liver fatty acid-binding protein, and the presence of fat can mimic the appearance for HNF1α-inactivated hepatocellular adenoma. Diffuse glutamine synthetase (unrelated to CTNNB1 mutation) staining can be seen in epithelioid AML and can be mistaken for the pattern of staining characteristic of β-catenin–activated hepatocellular adenoma or hepatocellular carcinoma.23 Another important pitfall is the expression of CD117 in AML, mimicking metastatic gastrointestinal stromal tumor.26 Most AMLs are considered benign and are associated with an excellent prognosis with infrequently reported malignant behavior. The criteria for malignancy in hepatic AML are not well established. Size >5 cm and mitoses ≥1 in 50 HPFs were the only features that predicted malignant behavior in 1 large study.27 Folpe et al28 advocated a 3-tiered system of benign, malignant, and uncertain malignant potential based on 7 high-risk features, including size >5 cm, high nuclear grade, hypercellularity, mitotic rate of >1 per 50 HPFs, necrosis, infiltration into surrounding normal parenchyma, and vascular invasion.28 The reliability of these criteria is uncertain because many AMLs show similar features and behave indolently.
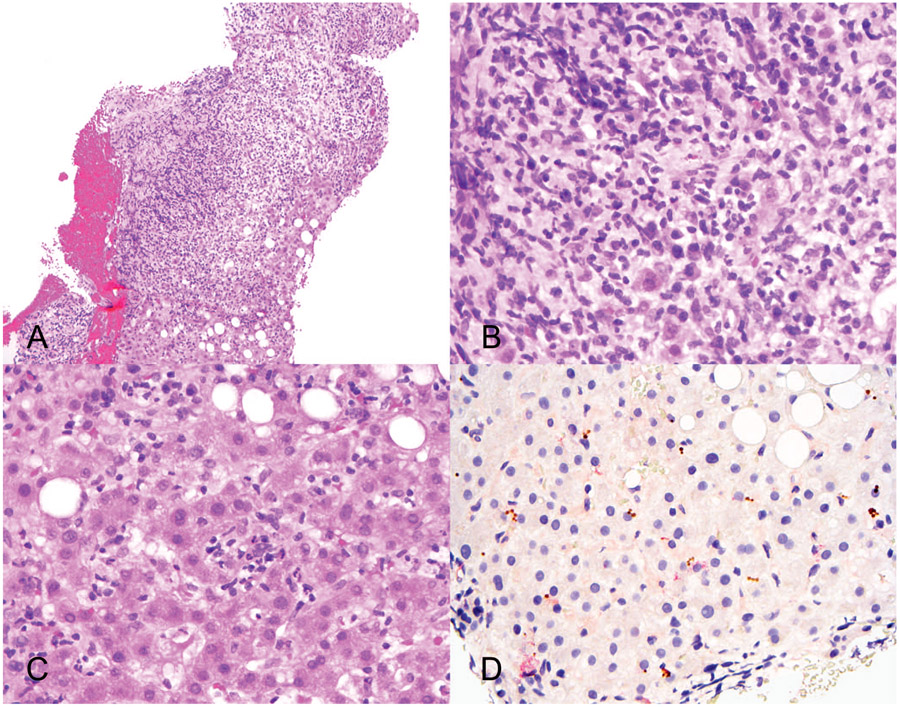
Figure 9.
Fat-poor angiomyolipoma. A, Low magnification shows a richly vascular lesion composed of epithelioid cells with abundant eosinophilic cytoplasm. B, Extramedullary hematopoiesis (arrow). C and D, Immunostains for HMB-45 and Melan-A (hematoxylin-eosin, original magnifications ×10 [A] and ×100 [B]; HMB-45 and Melan-A, original magnification ×200 [C and D]). Images courtesy of Richard Kirsch, MD.
Occasionally, AML can be richly inflammatory29,30 and mimic inflammatory myofibroblastic tumor or an inflammatory pseudotumor. However, the core feature of plump eosinophilic cells remains.
Mesenchymal Hamartoma
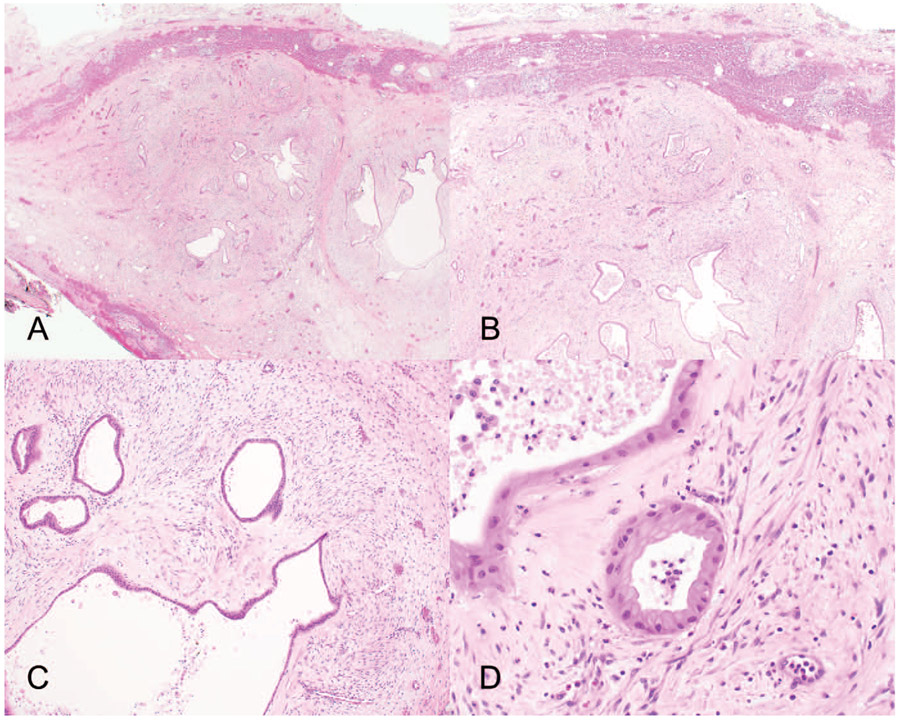
Mesenchymal hamartoma (MH) is rare (5% of pediatric liver tumors) but is the second most common pediatric hepatic tumor after hepatoblastoma. Although itself benign, on rare occasions it can progress to embryonal sarcoma and shares molecular alterations with those of embryonal sarcoma.31 MH is associated with Beckwith-Wiedemann syndrome and shows frequent genetic alterations of chromosome 19 involving a region called MHLB1 (evidence for its neoplastic nature).32.33 In addition, recently identified germ-line and somatic mutations in DICER1 in the absence of chromosomal translocations involving 19q13.4 suggest that MH is a component of the DICER1 syndrome phenotype.34 Like hepatoblastoma and germ cell tumors, MH can result in elevated serum α-fetoprotein levels, causing diagnostic confusion.32 Grossly, MH can present as a solid or cystic lesion. Histologically, MH is a biphasic lesion composed of epithelial and mesenchymal components characterized by numerous dilated bile ducts in a loose mesenchymal stroma somewhat resembling fibroadenoma of the breast. Interspersed islands of normal-appearing hepatocytes are also seen. Extramedullary hematopoiesis is commonly present. Cytologic atypia and mitoses are absent in both components (Figure 10). The prognosis of MH is excellent after complete excision. Incomplete excision may be associated with malignant transformation to embryonal sarcoma.35 Surgery is often curative, but there are rare reports of symptomatic unresectable examples requiring liver transplantation.36
Figure 10.
Mesenchymal hamartoma. A and B, Low magnifications show a biphasic lesion composed of numerous bile ducts in a loose mesenchymal stroma with interspersed islands of normal hepatocytes. C, Higher magnification shows both epithelial and mesenchymal components. D, Both components have bland nuclei with no cytologic atypia or mitoses (hematoxylin-eosin, original magnifications ×10 [A and B], ×100 [C], and ×200 [D]).
Hepatic Vascular Lesions
Benign vascular neoplasms of the liver are common; cavernous hemangioma is the most common benign hepatic tumor overall.37 Vascular hepatic neoplasms often present with characteristic enhancement patterns radiologically.38 The 2 hemangioma variants that can occasionally present diagnostic challenges because of their rarity and their unusual features are sclerosed hemangioma and anastomosing hemangioma, discussed here.
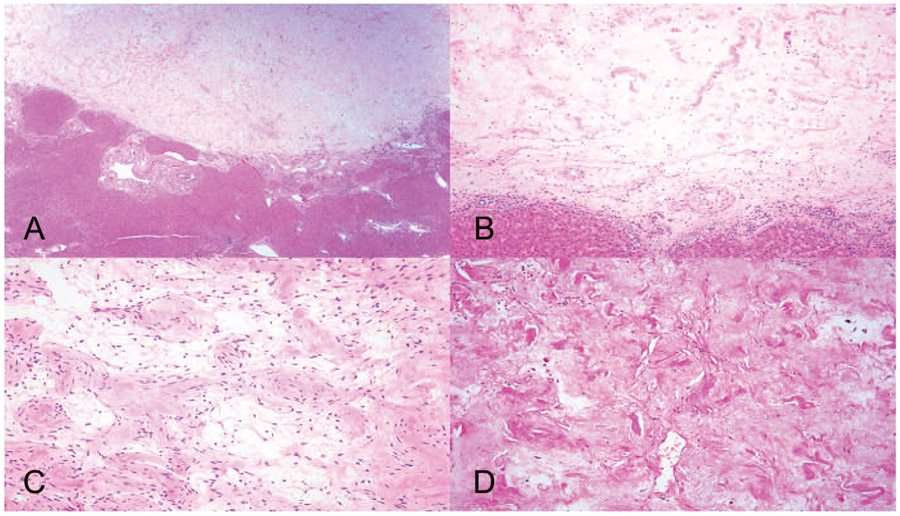
Sclerosed Hemangioma
Hepatic sclerosed hemangioma is a rare benign vascular lesion. It is a hemangioma that has undergone degeneration and scarring. Despite recent radiologic advances, when the scarring is extensive, hepatic sclerosed hemangioma can mimic malignancy radiographically.39 Histologically, scattered small vascular channels in a sclerotic background are seen. In later stages, the lesions become fully sclerotic, and the vascular channels undergo near-complete obliteration, leaving only ghostly remnants (Figure 11).40 Focal scars (eg, healed granulomatous lesions) and segmental atrophy can be included in the differential diagnosis, but even when the involutional changes of hepatic sclerosed hemangioma are extensive, an underlying vascular architecture can still be identified. Focal scars are typically avascular and may contain residual foreign body–type giant cells or fungal spores. Segmental atrophy can be distinguished by an elastin stain, which is negative in sclerosed hemangioma.
Figure 11.
Sclerosed hemangioma. A, Hemangioma with predominant sclerosis and near-complete obliteration of the vascular spaces. B, Higher magnification of remnant vessels. C, Ghostly remnants of vascular spaces. D, Negative elastin stain (hematoxylin-eosin, original magnifications ×10 [A], ×100 [B], and ×200 [C]; original magnification ×400 [D]).
Anastomosing Hemangioma
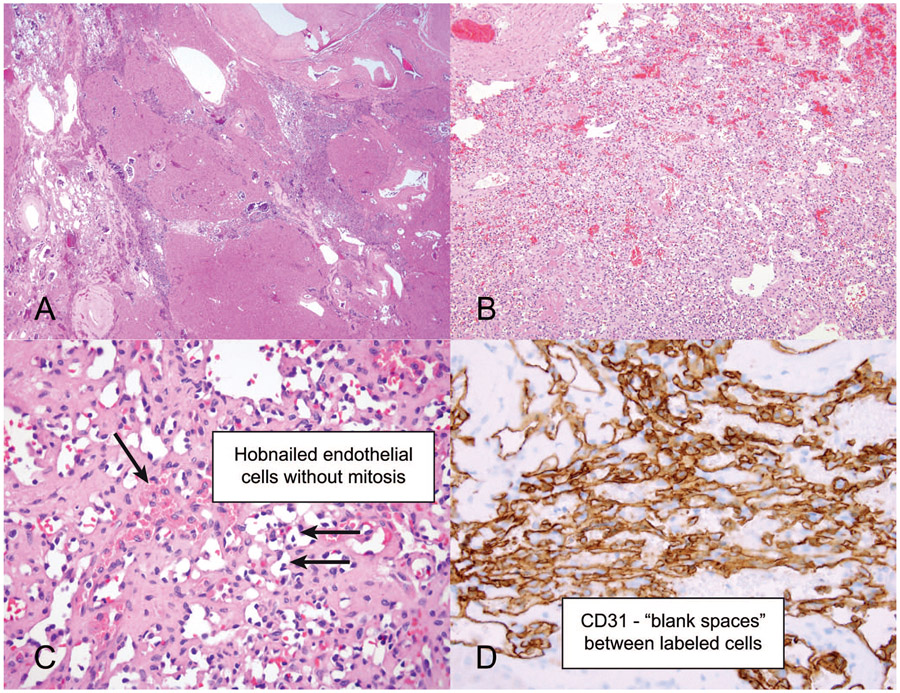
Anastomosing hemangioma, also called hepatic small vessel neoplasm, is a rare distinctive benign hepatic vascular tumor that may be mistaken for angiosarcoma. These lesions are grossly well demarcated but histologically can have an infiltrative pattern mimicking angiosarcoma. Despite the infiltrative pattern, they lack the high-grade cytologic atypia of angiosarcoma. Anastomosing hemangioma is thought to be a benign neoplasm rather than reactive because it harbors GNAQ/GNA14 mutations.41,42 Although there are limited available follow-up data, there are no reports of metastasis or recurrence to date. Grossly the tumor appears well circumscribed, with a gray-brown focally spongy appearance. Histologically, the tumor shows an infiltrative pattern with interconnecting vascular channels. Cytologically, anastomosing hemangioma may demonstrate mild cytologic atypia, usually in the supporting stroma rather than in the endothelial cells themselves, hobnailed endothelial cells, extramedullary hematopoiesis, and hyaline globules, but endothelial cell mitoses are absent. Immunohistochemistry for vascular markers is often useful because it highlights the anastomosing pattern by featuring blank spaces in between the labeled cells (Figure 12).43 Awareness of this rare entity is essential to avoid overdiagnosis as angiosarcoma and unnecessary aggressive treatment.
Figure 12.
Anastomosing hemangioma. A, Infiltrative vascular lesion at low magnification. B, Medium power shows an anastomosing vascular lesion. C, Higher magnification shows scattered hyaline globules and hobnailed endothelial cells without mitosis. D, CD31 immunostain highlighting the anastomosing pattern and blank spaces between the labeled cells (hematoxylin-eosin, original magnifications ×2 [A], ×10 [B], and ×100 [C]; original magnification ×400 [D]).
SUMMARY
The more common hepatic lesions often display specific imaging characteristics. The less familiar, rare benign tumors may pose diagnostic challenges. Here we discussed a selection of unusual benign liver lesions, focusing on nonepithelial tumors. When appropriate, pseudotumors and other rare benign lesions should be considered in the differential diagnosis to avoid misdiagnosis and overtreatment.
Footnotes
The authors have no relevant financial interest in the products or companies described in this article.
Contributor Information
Naziheh Assarzadegan, Department of Pathology, University of Michigan, Ann Arbor.
Elizabeth Montgomery, Department of Pathology, University of Miami Miller School of Medicine, Miami, Florida.
References
- 1.Singhi AD, Maklouf HR, Mehrotra AK, et al. Segmental atrophy of the liver: a distinctive pseudotumor of the liver with variable histologic appearances. Am J Surg Pathol. 2011;35(3):364–371. doi: 10.1097/PAS.0b013e31820b0603 [DOI] [PubMed] [Google Scholar]
- 2.Bedada AG, Sreekumaran MI, Azzie G. Segmental atrophy of the liver in a child: case report and review of the literature. S Afr J Child Health. 2019;13(2): 100–101. doi: 10.7196/SAJCH.2019.v13i2.1574 [DOI] [Google Scholar]
- 3.Assarzadegan N, Estevez-Castro R, Hutchings D, et al. Segmental atrophy (pseudotumor) of the liver: a marker of cardiovascular disease that mimics neoplasia. Mod Pathol. 2020;33(suppl 2):1500. [Google Scholar]
- 4.Torbenson M, Yasir S, Anders R, et al. Regenerative hepatic pseudotumor: a new pseudotumor of the liver. Hum Pathol. 2020;99:43–52. doi: 10.1016/j.humpath.2020.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Divatia M, Kim SA, Ro JY. IgG4-related sclerosing disease, an emerging entity: a review of a multi-system disease. Yonsei Med J. 2012;53(1):15–34. doi: 10.3349/ymj.2012.53.1.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masaki Y, Kurose N, Yamamoto M, et al. Cutoff values of serum IgG4 and histopathological IgG4+ plasma cells for diagnosis of patients with IgG4-related disease. Int J Rheumatol. 2012;2012:580814. doi: 10.1155/2012/580814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181–1192. doi: 10.1038/modpathol.2012.72 [DOI] [PubMed] [Google Scholar]
- 8.Chen JH, Deshpande V. IgG4-related disease and the liver. Gastroenterol Clin North Am. 2017;46(2):195–216. doi: 10.1016/j.gtc.2017.01.001 [DOI] [PubMed] [Google Scholar]
- 9.Mendes FD, Jorgensen R, Keach J, et al. Elevated serum IgG4 concentration in patients with primary sclerosing cholangitis. Am J Gastroenterol. 2006;101(9):2070–2075. doi: 10.1111/j.1572-0241.2006.00772.x [DOI] [PubMed] [Google Scholar]
- 10.Harada K, Nakanuma Y. Cholangiocarcinoma with respect to IgG4 reaction. Inti Hepatol. 2014;2014:803876. doi: 10.1155/2014/803876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alruwaii ZI, Zhang Y, Larman T, Miller JA, Montgomery EA. Rosai-Dorfman disease of the digestive system-beware vasculopathy: a clinicopathologic analysis. Am J Surg Pathol. 2019;43(12):1644–1652. doi: 10.1097/PAS.0000000000001343 [DOI] [PubMed] [Google Scholar]
- 12.Taylor MS, Chougule A, MacLeay AR, et al. Morphologic overlap between inflammatory myofibroblastic tumor and IgG4-related disease: lessons from next-generation sequencing. Am J Surg Pathol. 2019;43(3):314–324. doi: 10.1097/PAS.0000000000001167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheuk W, Chan JK, Shek TW, et al. Inflammatory pseudotumor-like follicular dendritic cell tumor: a distinctive low-grade malignant intra-abdominal neoplasm with consistent Epstein-Barr virus association. Am J Surg Pathol. 2001; 25(6):721–731. doi: 10.1097/00000478-200106000-00003 [DOI] [PubMed] [Google Scholar]
- 14.Hagen CE, Kamionek M, McKinsey DS, Misdraji J. Syphilis presenting as inflammatory tumors of the liver in HIV-positive homosexual men. Am J Surg Pathol. 2014;38(12):1636–1643. doi: 10.1097/PAS.0000000000000264 [DOI] [PubMed] [Google Scholar]
- 15.Shim HJ. Tertiary syphilis mimicking hepatic metastases of underlying primary peritoneal serous carcinoma. World J Hepatol. 2010;2(9):362–366. doi: 10.4254/wjh.v2.i9.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeRoche TC, Huber AR. The great imitator: syphilis presenting as an inflammatory pseudotumor of liver. Int J Surg Pathol. 2018;26(6):528–529. doi: 10.1177/1066896917745665 [DOI] [PubMed] [Google Scholar]
- 17.Taxy JB, Gibson WE, Kaufman MW. Echinococcosis: unexpected occurrence and the diagnostic contribution of routine histopathology. Am J Surg Pathol. 2017;41(1):94–100. doi: 10.1097/PAS.0000000000000742 [DOI] [PubMed] [Google Scholar]
- 18.Reinehr M, Micheloud C, Grimm F, et al. Pathology of echinococcosis: a morphologic and immunohistochemical study on 138 specimens with focus on the differential diagnosis between cystic and alveolar echinococcosis. Am J Surg Pathol. 2020;44(1):43–54. doi: 10.1097/PAS.0000000000001374 [DOI] [PubMed] [Google Scholar]
- 19.Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20(3):795–817. doi: 10.1148/radiographics.20.3.g00ma06795 [DOI] [PubMed] [Google Scholar]
- 20.Eckert J, Conraths FJ, Tackmann K. Echinococcosis: an emerging or re-emerging zoonosis? Int J Parasitol. 2000;30(12–13):1283–1294. doi: 10.1016/s0020-7519(00)00130-2 [DOI] [PubMed] [Google Scholar]
- 21.Talati H, Radhi J, Popovich S, Marcaccio M. Hepatic epithelioid angiomyolipoma: case series. Gastroenterology Res. 2010;3(6):293–295. doi: 10.4021/gr273w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goodman ZD, Ishak KG. Angiomyolipomas of the liver. Am J Surg Pathol. 1984;8(10):745–750. doi: 10.1097/00000478-198410000-00003 [DOI] [PubMed] [Google Scholar]
- 23.Yan Z, Grenert JP, Joseph NM, et al. Hepatic angiomyolipoma: mutation analysis and immunohistochemical pitfalls in diagnosis. Histopathology. 2018;73(1):101–108. doi: 10.1111/his.13509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nonomura A, Mizukami Y, Kadoya M. Angiomyolipoma of the liver: a collective review. J Gastroenterol. 1994;29(1):95–105. doi: 10.1007/BF01229084 [DOI] [PubMed] [Google Scholar]
- 25.Tsui WM, Colombari R, Portmann BC, et al. Hepatic angiomyolipoma: a clinicopathologic study of 30 cases and delineation of unusual morphologic variants. Am J Surg Pathol. 1999;23(1):34–48. doi: 10.1097/00000478-199901000-00004 [DOI] [PubMed] [Google Scholar]
- 26.Makhlouf HR, Remotti HE, Ishak KG. Expression of KIT (CD117) in angiomyolipoma. Am J Surg Pathol. 2002;26(4):493–497. doi: 10.1097/00000478-200204000-00012 [DOI] [PubMed] [Google Scholar]
- 27.Bleeker JS, Quevedo JF, Folpe AL. “Malignant” perivascular epithelioid cell neoplasm: risk stratification and treatment strategies. Sarcoma. 2012;2012:541626. doi: 10.1155/2012/541626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Folpe AL, Mentzel T, Lehr HA, Fisher C, Balzer BL, Weiss SW. Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature. Am J Surg Pathol. 2005;29(12):1558–1575. doi: 10.1097/01.pas.0000173232.22117.37 [DOI] [PubMed] [Google Scholar]
- 29.Kojima M, Nakamura S, Ohno Y, Sugihara S, Sakata N, Masawa N. Hepatic angiomyolipoma resembling an inflammatory pseudotumor of the liver: a case report. Pathol Res Pract. 2004;200(10):713–716. doi: 10.1016/j.prp.2004.08.001 [DOI] [PubMed] [Google Scholar]
- 30.Shi H, Cao D, Wei L, Sun L, Guo A. Inflammatory angiomyolipomas of the liver: a clinicopathologic and immunohistochemical analysis of 5 cases. Ann Diagn Pathol. 2010;14(4):240–246. doi: 10.1016/j.anndiagpath.2010.03.002 [DOI] [PubMed] [Google Scholar]
- 31.Martins-Filho SN, Putra J. Hepatic mesenchymal hamartoma and undifferentiated embryonal sarcoma of the liver: a pathologic review. Hepat Oncol. 2020;7(2):HEP19. doi: 10.2217/hep-2020-0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cajaiba MM, Sarita-Reyes C, Zambrano E, Reyes-M–gica M. Mesenchymal hamartoma of the liver associated with features of Beckwith-Wiedemann syndrome and high serum alpha-fetoprotein levels. Pediatr Dev Pathol. 2007;10(3):233–238. doi: 10.2350/06-07-0128.1 [DOI] [PubMed] [Google Scholar]
- 33.Rakheja D, Margraf LR, Tomlinson GE, Schneider NR. Hepatic mesenchymal hamartoma with translocation involving chromosome band 19q13.4: a recurrent abnormality. Cancer Genet Cytogenet. 2004;153(1):60–63. doi: 10.1016/j.cancergencyto.2003.12.004 [DOI] [PubMed] [Google Scholar]
- 34.Apellaniz-Ruiz M, Segni M, Kettwig M, et al. Mesenchymal hamartoma of the liver and DICER1 syndrome. N Engl J Med. 2019;380(19):1834–1842. doi: 10.1056/NEJMoa1812169 [DOI] [PubMed] [Google Scholar]
- 35.Stringer MD, Alizai NK. Mesenchymal hamartoma of the liver: a systematic review. J Pediatr Surg. 2005;40(11):1681–1690. doi: 10.1016/j.jpedsurg.2005.07.052 [DOI] [PubMed] [Google Scholar]
- 36.Hernández JC, Alfonso C, González L, et al. Solid mesenchymal hamartoma in an adult: a case report. J Clin Pathol. 2006;59(5):542–545. doi: 10.1136/jcp.2004.024398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bioulac-Sage P, Laumonier H, Laurent C, Blanc JF, Balabaud C. Benign and malignant vascular tumors of the liver in adults. Semin Liver Dis. 2008;28(3):302–314. doi: 10.1055/s-0028-1085098 [DOI] [PubMed] [Google Scholar]
- 38.Choi HH, Manning MA, Mehrotra AK, Wagner S, Jha RC. Primary hepatic neoplasms of vascular origin: key imaging features and differential diagnoses with radiology-pathology correlation. AJR Am J Roentgenol. 2017;209(6):W350–W359. doi: 10.2214/AJR.17.18100 [DOI] [PubMed] [Google Scholar]
- 39.Doyle DJ, Khalili K, Guindi M, Atri M. Imaging features of sclerosed hemangioma. AJR Am J Roentgenol. 2007;189(1):67–72. doi: 10.2214/AJR.06.1076 [DOI] [PubMed] [Google Scholar]
- 40.Makhlouf HR, Ishak KG. Sclerosed hemangioma and sclerosing cavernous hemangioma of the liver: a comparative clinicopathologic and immunohisto-chemical study with emphasis on the role of mast cells in their histogenesis. Liver. 2002;22(1):70–78. doi: 10.1046/j.0106-9543.2001.01604.x [DOI] [PubMed] [Google Scholar]
- 41.Joseph NM, Brunt EM, Marginean C, et al. Frequent GNAQ and GNA14 mutations in hepatic small vessel neoplasm. Am J Surg Pathol. 2018;42(9):1201–1207. doi: 10.1097/PAS.0000000000001110 [DOI] [PubMed] [Google Scholar]
- 42.Bean GR, Joseph NM, Gill RM, Folpe AL, Horvai AE, Umetsu SE. Recurrent GNAQ mutations in anastomosing hemangiomas. Mod Pathol. 2017;30(5):722–727. doi: 10.1038/modpathol.2016.234 [DOI] [PubMed] [Google Scholar]
- 43.Lin J, Bigge J, Ulbright TM, Montgomery E. Anastomosing hemangioma of the liver and gastrointestinal tract: an unusual variant histologically mimicking angiosarcoma. Am J Surg Pathol. 2013;37(11):1761–1765. doi: 10.1097/PAS.0b013e3182967e6c [DOI] [PubMed] [Google Scholar]