Abstract
Ischemic heart disease and subsequent myocardial infarction (MI) is one of the leading causes of mortality in the United States and around the world. In order to explore the pathophysiological changes after myocardial infarction and design future treatments, research models of MI are required. Permanent ligation of the left coronary artery (LCA) in mice is a popular model to investigate cardiac function and ventricular remodeling post MI. Here we describe a less invasive, reliable, and reproducible surgical murine MI model by permanent ligation of the LCA. Our surgical model comprises of an easily reversible general anesthesia, endotracheal intubation that does not require a tracheotomy, and a thoracotomy. Electrocardiography and troponin measurement should be performed to ensure MI. Echocardiography at day 28 after MI will discern heart function and heart failure parameters. The degree of cardiac fibrosis can be evaluated by Masson’s trichrome staining and cardiac MRI. This MI model is useful for studying the pathophysiological and immunological alterations after MI.
Introduction
Cardiovascular disease is a major public health concern that claims 17.9 million lives each year, accounting for 31 percent of global mortality1. The most prevalent type of cardiovascular anomaly is coronary heart disease, and myocardial infarction (MI) is one of the major manifestations of coronary heart disease2. MI is usually caused by thrombotic occlusion of a coronary artery due to the rupture of a vulnerable plaque3. The resulting ischemia causes profound ionic and metabolic changes in the affected myocardium, as well as a rapid decrease in systolic function. MI results in the death of cardiomyocytes, which can further lead to ventricular dysfunction and heart failure4.
Research on MI in patients is limited due to the scarcity of tissues obtained from patients with MI5. As such, murine models of MI are useful in both studying disease mechanisms as well as developing potential therapeutic targets. Currently available murine models of MI includeirreversible ischemia models (LCA and ablation methods) and reperfusion models (ischemia/reperfusion, I/R)6. Permanent ligation of the left coronary artery (LCA) in mice is the most used method, and it imitates the pathophysiology and immunology of MI in patients7, 8, 9. Permanent MI can also be induced by ablation methods, which involve electrical damage or cryoinjury. Ablation methods are able to generate uniformsized infarction at the precise location10. On the other hand, scar formation, infarct morphology, and molecular signaling mechanisms may vary among the ablation methods10, 11. The murine I/R method is another important MI model as it represents the clinical scenario of reperfusion therapy12. The I/R model is associated with challenges such as a variable infarct size, difficulty in distinguishing responses of initial injury, and reperfusion6.
Although widely used, LCA ligation methods are associated with low survival rates and post-operative pain13. This protocol demonstrates the murine surgical MI model of LCA ligation that involves the preparation and intubation of mice, LCA ligation, post-operative care, and validation of MI. Rather than using an invasive tracheotomy14, this method employs endotracheal intubation. The animal is intubated by illuminating the oropharynx using a laryngoscope, making the procedure easier, safer, and less traumatic15. The mouse is kept on ventilator support and under isoflurane anesthesia throughout the procedure. Further, echocardiography and Masson’s trichrome staining are performed to evaluate heart function and cardiac fibrosis after MI, respectively. Overall, this method provides a reliable and reproducible surgical murine model of MI that can be used to study pathophysiology and inflammation after MI.
Protocol
The present study protocol was reviewed and approved by the Institutional Animal Care and Use Committee (IACUC) of the University of Pittsburgh. Eight (sham n = 4 and MI n = 4) 1-year-old female C57BL/6J mice weighing 24-30 g were used for these experiments. Approximately 100% and at least 80% of mice survived in the first 24 h and 28 days, respectively.
1. Preparation and endotracheal intubation of the mice
Preheat a bead sterilizer (see Table of Materials) to 250 °C and place autoclaved surgical instruments in it for a few minutes.
Anesthetize the mouse in an induction chamber with 3% isoflurane and 1 L/min oxygen for 5 min.
Ensure the depth of anesthesia in the mouse by checking the response to a firm toe pinch.
Weigh the mouse to estimate the dosage of the pre-operative analgesic drug, buprenorphine (0.1 mg/kg). Inject the drug intraperitonially.
Trim the fur on the left side of the thorax using an electric razor.
Disinfect the surgical site with povidone-iodine and 70% ethanol thereafter three times.
Place the mouse in the supine position on an inclined board. Secure the head and limbs of the mouse using an elastic band attached to the upper incisors and adhesive tape, respectively. Apply sterile ophthalmic lubricant on the eyes to prevent dryness while under anesthesia.
Open the jaw and gently pull the tongue out of the oral cavity.
Identify the opening of the larynx by illuminating the oropharynx using a laryngoscope (see Table of Materials).
Cut off about 0.5 cm from a 24 G catheter needle and insert the blunt needle into the plastic shield. Direct the blunt needle with the plastic shield into the trachea. Take out the needle, leaving the plastic shield into the trachea.
Set the ventilator (see Table of Materials) to a respiratory rate of 137 beats per min (optimized for the mice used in this study) and tidal volume 0.18 cc. Connect the respirator tubes to the catheter shield and confirm correct intubation by looking for a synchronized chest movement with the ventilator.
Disconnect the respirator tube from the catheter shield and place the animal in the supine position on a preheated temperature-controlled surgical board. Reconnect the mouse to the ventilator.
Table of material
| Name of Material/ Equipment | Company | Catalog Number | Comments/Description |
|---|---|---|---|
| 22 G catheter needle | Exel INT | 26741 | Thoracentesis |
| 24 G catheter needle | Exel INT | 26746 | Endotracheal intubation |
| 4-0 nylon suture | Covetrus | 29263 | Suturing of muscles and skin |
| 8-0 nylon suture | S&T | 3192 | Ligation of LAD |
| Anesthetic Vaporizers | Vet equip | VE-6047 | Anesthetic support |
| Animal physiology monitor | Fujifilm | VEVO 3100 | Monitor heart rate,respiration rate and body temperature |
| Betadine solution | PBS animal health | 11205 | Antispetic |
| Buprenorphine | Covetrus | 55175 | Analgesic |
| Disecting microscope | OMANO | OM2300S-V7 | Binocular |
| Electric razor | Wahl | 79300-1001M | Shaving |
| Electrode gel | Parker Laboratories | W60698L | Electrically conductive gel |
| Ethanol | Decon Laboratories | 22-032-601 | Disinfectant |
| Forceps | FST | 11065-07 | Stainless Steel |
| Gauze | Curity | CAR-6339-PK | Sterile |
| Heat lamp | Satco | S4998 | Post surgery care |
| Heating pad | Kent scientific | Surgi-M | Temperature control |
| Hot Bead sterilizer | Germinator 500 | 11503 | Sterilization of surgical instrument |
| Isoflurane | Covetrus | 29405 | Anesthesia |
| Masson’s trichrome staining kit | Thermoscientific | 87019 | Measurement of cardiac Fibrosis |
| Micro Needle Holder | FST | 12500-12 | Stainless Steel |
| Micro scissors | FST | 15000-02 | Stainless Steel |
| Ophthalmic ointment | Dechra | Puralube Vet | Sterile occular lubricant |
| Scanning Gel | Parker Laboratories | Aquasonic 100 | Aqueous ultrasound transmission gel |
| Scissors | FST | 14060-11 | Stainless Steel |
| Small Animal Laryngoscope | Penn-Century | Model LS-2-M | Illuminating the oropharynx |
| Small animal ventilator | Harvard apparatus | 557058 | Ventilator support |
| Surgical light | Cole parmer | 41723 | Illuminator Width (in): 7 |
| Vevo 3100 preclinical imaging platforn | Fujifilm | VEVO 3100 | Echocardiography |
| VevoLAB software | Fujifilm | VevoLAB 3.2.6 | Echocardiography data analysis |
2. Permanent ligation of the left coronary artery
-
Disinfect the surgical site with povidone-iodine and 70% alcohol. Apply a sterile drape having a quarter-sized hole in the center to secure the surgical site. Gently lift the skin using a pair of forceps and make a small (1.5-2 cm) cutaneous transverse incision along the line between the left pectoralis major and minor muscles using a pair of surgical scissors.
NOTE: Scissors were used to make the incision as it provides the required control over the depth and direction of the cut.
Separate the underlying pectoralis muscles with forceps and dissecting scissors. The muscles were separated using retractors attached to elastic bands.
Make an incision in the third intercostal space with a pair of micro scissors following the natural angle of the ribcage. At this phase, extreme caution must be exercised to prevent injury to the heart and lungs.
Gently stretch the ribs apart using retractors to expose the left ventricle. Move the pericardial fat aside and locate the LCA, which runs from the edge of the left atrium towards the apex of the heart.
-
Pass an 8-0 nylon suture under the LCA with the help of a needle holder. Ligate the LCA with a double knot followed by a second knot (a modified surgeon’s knot).
NOTE: Blanching of the lower left ventricle confirms a successful LCA ligation. In addition to this, troponin measurement, ECG monitoring (ST elevation), echo/in vivo cardiac-gated MRI, or micro-CT images are also advised to confirm the comparable MI lesions.
Remove the retractors and insert a 22 G catheter needle into the chest cavity. Remove the needle, leaving the tip of the plastic shield in the thoracic cavity. Close the ribcage using a 4-0 nylon suture.
Connect a syringe to the 22 G plastic shield and slowly remove excess air trapped in the thoracic cavity by gently pressing the chest to establish a negative air pressure. Remove the plastic shield.
Close the skin with a 4-0 nylon suture.
Switch off the isoflurane supply. At this stage, the mouse is on the ventilator supplying oxygen.
3. Post-operative care
-
Switch off the ventilator once spontaneous breathing starts.
NOTE: The procedure takes about 30-35 min per animal from preparation of the mice up to this step.
Keep the mouse under a heat lamp and monitor it until it is awake. The animal should not be left unattended until it has recovered enough consciousness to maintain sternal recumbency.
After surgery, place the animal is in a separate cage and return it to the original cage with other animals only after it fully recovers.
Monitor the mouse daily for any sign of pain or discomfort.
Continue intraperitoneal injection of buprenorphine (0.1 mg/kg) every 6-8 hours for an additional 2 days following the surgery.
4. Echocardiographic Evaluation
NOTE: Echocardiography was performed to evaluate the parameters of heart failure on day 28 after MI.
After 28 days following the surgery, anesthetize the mice with 3% isoflurane and 1 L/min oxygen, apply sterile ophthalmic lubricant on the eyes, and remove chest hair using hair removal cream. Disinfect the chest area with povidone-iodine and 70% ethanol three times.
Secure the anesthetized mice atop the imaging platform (see Table of Materials) in the supine position and maintain a steady level of anesthesia throughout the procedure using a nose cone connected to the anesthetic system (1%-2% isoflurane and 1 L/min oxygen).
Tape the four paws to the ECG electrodes with electrode gel (see Table of Materials). Monitor the temperature of the animal by inserting a rectal probe (see Table of Materials).
Apply the scanning gel (see Table of Materials) to the chest, place the transducer vertically, lower it to the parasternal line (parallel to the thorax), and rotate 35° anticlockwise to obtain the parasternal long axis view of the left ventricle.
Tap the B-mode imaging button on the imaging software (see Table of Materials) to get a complete long axis view of the heart. Adjust the gate size and brightness and save the images using Save Clip or Save Frame for later measurements16.
Switch to M-mode (motion-mode) and place the M-mode axis at the level of the papillary muscle. Adjust the gate size and tap the M-mode Start button. Save the images using Save Clip or Save Frame16, 17.
As the 4D mode image acquisition process is automated, verify that the ECG and respiration signals are active (Figure 1) before acquiring the data.
Start acquiring the data in B-Mode. Open the 4D scan panel and initiate the 3D motor. Set the image parameters in the 4D scan panel and tap the Scan button to begin the scanning. After reviewing the images in the 2D view, load the images into 4D mode using the Load into 4D button.
Figure 1: Active ECG and respiration signals during the echocardiographic evaluation.
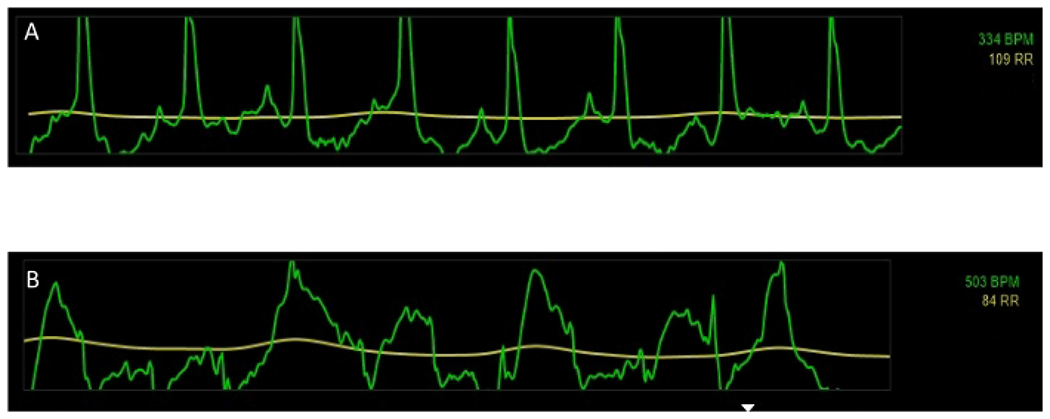
Representative active ECG and respiration signals during the echocardiographic evaluation of (A) sham and (B) MI mice. Green = ECG signals, yellow = respiration signals.
Representative Results
Figure 1 demonstrates the representative active ECG and respiration signals during the echocardiographic evaluation of sham (Figure 1A) and MI (Figure 1B) mice. Verification of active ECG and respiration signals are important before acquiring the echocardiographic data. Figure 2 shows echocardiographic measurement of cardiac functional parameters following 28 days after LCA ligation. Figure 2 shows M-mode images of the para sternal short axis view of sham (Figure 2A) and MI (Figure 2B) hearts. Figure 2B shows defective heart wall movement following LCA ligation. Indicators of heart failure, such as increased LV mass (Figure 2C), decreased ejection fraction (Figure 2D), and decreased cardiac output (Figure 2E), were observed in the MI group as compared to the sham group.
Figure 2: Echocardiographic evaluation of cardiac functional parameters following LCA ligation on day 28 after the surgery.
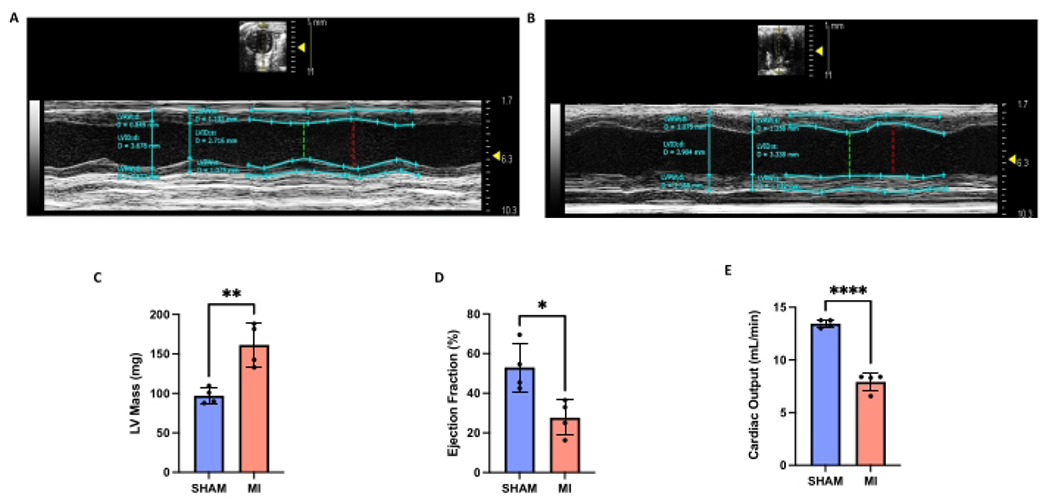
Representative parasternal short axis (PSAX) M-mode echocardiographic images of (A) sham and (B) MI mice. Assessment of (C) left ventricular mass (mg), (D) ejection fraction (%), and (E) cardiac output (mL/min) of sham and mice with MI. LVAW;d = left ventricular anterior wall thickness in diastole; LVAW;s = left ventricular anterior wall thickness in systole; LVPW;d = left ventricular posterior wall thickness in diastole; LVPW;s = left ventricular posterior wall thickness in systole; LVID;d = left ventricular internal diameter in diastole; LVID;s = left ventricular internal diameter in systole. Data are shown as Mean ± SD. * P < 0.05, ** P < 0.01, **** P < 0.0001.
All the animals were euthanized according to standard protocols using an excessive dose of CO2 gas. The hearts were fixed and frozen in optimal cutting temperature (OCT) compound. Masson’s trichrome staining18 was performed for three different ventricle sections (lower, middle, and upper) and images were taken using a research slide scanner under 10x magnification to examine the degree of cardiac fibrosis. Figure 3 shows increased collagen staining (blue) in the infarcted heart, indicating augmented fibrosis.
Figure 3: Assessment of fibrosis after LCA ligation on day 28 after the surgery.
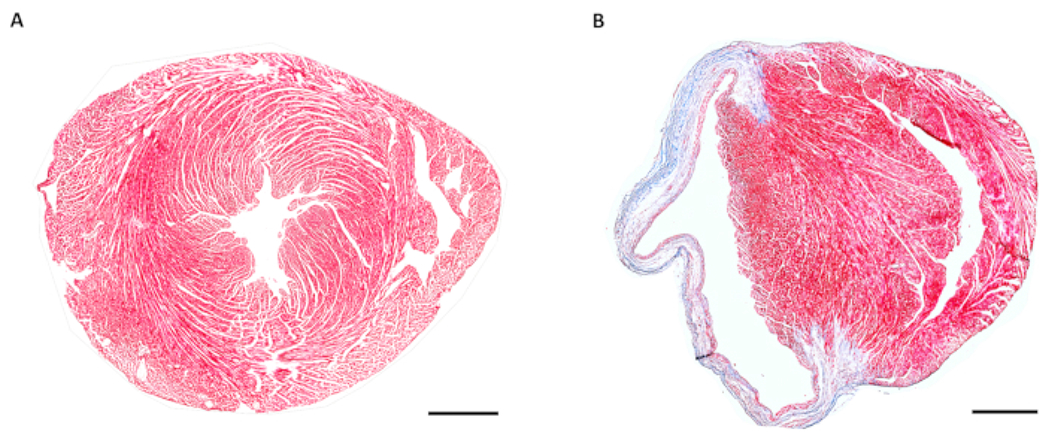
Representative images showing Masson’s trichrome staining of (A) sham and (B) MI hearts 28 days after the surgery. The fibrotic regions in the infarcted heart are characterized by collagen deposition and stained blue after Masson’s trichrome staining. Scale bar = 500 μm.
Discussion
The murine model of MI is gaining popularity in cardiovascular research laboratories, and this study describes a reproducible and clinically relevant MI model. This protocol improves the LCA ligation process in several ways. To begin with, the use of injectable pre-operative anesthetics such as xylazin/ketamine or sodium pentobarbital14, 15 is avoided. Only isoflurane anesthesia was used, which helps enhance animal survival rates (>80% survival 28 days after surgery), minimize drug-induced complications, and has minimal cardiac effects as compared to other agents19. However, isoflurane does also slow the heart, albeit at a lower degree compared to other anesthetic agents20. This protocol involves less invasive endotracheal intubation avoiding tracheostomy21, which reduces post-operative pain and discomfort. Previous murine LCA ligation studies have recommended making a mid-neck incision to improve the visualization of endotracheal intubation; however, the current protocol uses a laryngoscope instead to illuminate the oropharynx15. Lugrin et al. recently demonstrated a murine LCA MI model without thoracentesis14; however, the current protocol includes an effective thoracentesis, which will help remove excess blood and air from the chest cavity, preventing pneumothorax19. In addition, this method uses sterile gauze for bleeding management in place of a cauterizer, as using a cauterizer to reduce bleeding can result in iatrogenic burns and may alter inflammatory readings21.
One of the critical steps in this surgical model is identification and ligation of the LCA. The location of the coronary artery may vary depending on mouse strains and genotypes9. In most cases, the artery is not visible under a microscope. From experience, ligating the myocardial tissue 2-4 mm below the edge of the left atrium results in efficient blanching of the left ventricular wall. Furthermore, the procedure can be simply modified to induce temporary myocardial ischemia followed by reperfusion (I/R) by removing the ligation22. This animal model mimics the restoration of coronary blood flow in MI patients following percutaneous coronary intervention23, 24. Since the permanent LCA occlusion model differs from the I/R model in several aspects, such as the size of the infarcted area, location of the infarct, and infiltration of inflammatory cells, researchers must be cautious while selecting the relevant model depending on the study7, 14, 25.
There are multiple approaches to ensure successful ligation of the LCA and subsequent development of MI. Observing immediate blanching of the lower left ventricle is the earliest confirmation of successful LCA ligation. Apart from this, the extent and location of the myocardial infarct can be visualized by staining the whole heart with Evan’s blue or 2,3,5-triphenyl tetrazolium chloride (TTC)26. Measurement of circulating cardiac troponin can further validate the myocardial tissue injury21. Electrocardiography can be used as a non-invasive method of confirming elevation of the ST segment after MI17. The degree of cardiac fibrosis associated with MI can be evaluated by Masson’s trichrome staining and cardiac MRI27, 28, 29. Echocardiography can be used to evaluate the parameters of heart failure on days 1 and 28 after MI. To examine cardiac remodeling following the MI, Masson’s trichome staining and echocardiography can be utilized17. It is also possible to use qPCR and immunoblot to further investigate and confirm the expression of the genes and proteins implicated in fibrosis, inflammation, and heart failure after MI14.
The major limitation of LCA ligation is the high incidence of mortality, which could be due to post-operative cardiac arrhythmias, ventricular rupture, hemorrhage, pneumothorax, and post-operative discomfort19, 30. However, a successful thoracentesis, minimizing the non-target tissue damage, and proper post-operative pain and temperature management may help reduce the death of the animal. As with any other surgical model, exact reproducibility is another limitation of this surgical model. Researchers can, however, reproduce MI, control infarct size, and improve post-surgery survival by rigorous practice and experience.
Acknowledgments
This work was supported by National Institute of Health grants (R01HL143967, R01HL142629, R01AG069399, and R01DK129339), AHA Transformational Project Award (19TPA34910142), AHA Innovative Project Award (19IPLOI34760566), and ALA Innovation Project Award (IA-629694) (to PD).
Footnotes
A complete version of this article that includes the video component is available at http://dx.doi.org/10.3791/64387.
Disclosures
The authors do not have any conflicts of interest to disclose.
References
- 1.Virani SS et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 143 (8), e254–e743 (2021). [DOI] [PubMed] [Google Scholar]
- 2.Mendis S. et al. World Health Organization definition of myocardial infarction: 2008-09 revision. International Journal of Epidemiology. 40 (1), 139–146 (2011). [DOI] [PubMed] [Google Scholar]
- 3.Frangogiannis NG Pathophysiology of myocardial infarction. Comprehensive Physiology. 5 (4), 1841–1875 (2011). [DOI] [PubMed] [Google Scholar]
- 4.Smit M, Coetzee A, Lochner A The pathophysiology of myocardial ischemia and perioperative myocardial infarction. Journal of Cardiothoracic and Vascular Anesthesia. 34 (9), 2501–2512 (2020). [DOI] [PubMed] [Google Scholar]
- 5.Johny E. et al. Platelet mediated inflammation in coronary artery disease with Type 2 Diabetes patients. Journal of Inflammation Research. 14, 5131 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin TP et al. Preclinical models of myocardial infarction: from mechanism to translation. British Journal of Pharmacology. 179 (5), 770–791 (2022). [DOI] [PubMed] [Google Scholar]
- 7.De Villiers C, Riley PR Mouse models of myocardial infarction: comparing permanent ligation and ischaemia-reperfusion. Disease Models & Mechanisms. 13 (11), dmm046565 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vasamsetti SB et al. Apoptosis of hematopoietic progenitor-derived adipose tissue-resident macrophages contributes to insulin resistance after myocardial infarction. Science Translational Medicine. 12 (553), eaaw0638 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernandez B. et al. The coronary arteries of the C57BL/6 mouse strains: implications for comparison with mutant models. Journal of Anatomy. 212 (1), 12–18 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Amerongen MJ, Harmsen MC, Petersen AH, Popa ER, van Luyn MJ Cryoinjury: a model of myocardial regeneration. Cardiovascular Pathology. 17 (1), 23–31 (2008). [DOI] [PubMed] [Google Scholar]
- 11.Lam NT, Sadek HA Neonatal heart regeneration: comprehensive literature review. Circulation. 138 (4), 412–423 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heusch G, Gersh BJ The pathophysiology of acute myocardial infarction and strategies of protection beyond reperfusion: a continual challenge. European Heart Journal. 38 (11), 774–784 (2017). [DOI] [PubMed] [Google Scholar]
- 13.Srikanth G, Prakash P, Tripathy N, Dikshit M, Nityanand S Establishment of a rat model of myocardial infarction with a high survival rate: A suitable model for evaluation of efficacy of stem cell therapy. Journal of Stem Cells & Regenerative Medicine. 5 (1), 30–36 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lugrin J, Parapanov R, Krueger T, Liaudet L Murine myocardial infarction model using permanent ligation of left anterior descending coronary artery. Journal of Visualized Experiments. (150), e59591 (2019). [DOI] [PubMed] [Google Scholar]
- 15.Muthuramu I, Lox M, Jacobs F, De Geest B Permanent ligation of the left anterior descending coronary artery in mice: a model of post-myocardial infarction remodelling and heart failure. Journal of Visualized Experiments. (94), e52206 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pistner A, Belmonte S, Coulthard T, Blaxall BC Murine echocardiography and ultrasound imaging. Journal of Visualized Experiments. (42), e2100 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L. et al. Assessment of cardiac morphological and functional changes in mouse model of transverse aortic constriction by echocardiographic imaging. Journal of Visualized Experiments. (112), e54101 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vasamsetti SB et al. Sympathetic neuronal activation triggers myeloid progenitor proliferation and differentiation. Immunity. 49 (1), 93–106 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reichert K. et al. Murine left anterior descending (LAD) coronary artery ligation: an improved and simplified model for myocardial infarction. Journal of Visualized Experiments. (122), e55353 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alwardt CM, Redford D, Larson DF General anesthesia in cardiac surgery: a review of drugs and practices. The Journal of Extra-Corporeal Technology. 37 (2), 227–235 (2005). [PMC free article] [PubMed] [Google Scholar]
- 21.Kolk MV et al. LAD-ligation: a murine model of myocardial infarction. Journal of Visualized Experiments. (32), e1438 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu Y, Yin X, Wijaya C, Huang M-H, McConnell BK Acute myocardial infarction in rats. Journal of Visualized Experiments. (48), e2464 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kalogeris T, Baines C, Krenz M, Korthuis R Chapter six-cell biology of ischemia/reperfusion injury. International Review of Cell and Molecular Biology, Academic Press,. 229–317 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scofield SL, Singh K Confirmation of myocardial ischemia and reperfusion injury in mice using surface pad electrocardiography. Journal of Visualized Experiments. (117), e54814 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yan X. et al. Temporal dynamics of cardiac immune cell accumulation following acute myocardial infarction. Journal of Molecular and Cellular Cardiology. 62, 24–35 (2013). [DOI] [PubMed] [Google Scholar]
- 26.Xu Q. et al. Protective effects of fentanyl preconditioning on cardiomyocyte apoptosis induced by ischemia-reperfusion in rats. Brazilian Journal of Medical and Biological Research. 50 (2), e5286 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leuschner F. et al. Rapid monocyte kinetics in acute myocardial infarction are sustained by extramedullary monocytopoiesis. Journal of Experimental Medicine. 209 (1), 123–137 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leuschner F. et al. Silencing of CCR2 in myocarditis. European Heart Journal. 36 (23), 1478–1488 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dutta P. et al. E-selectin inhibition mitigates splenic HSC activation and myelopoiesis in hypercholesterolemic mice with myocardial infarction. Arteriosclerosis, Thrombosis, and Vascular Biology. 36 (9), 1802–1808 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jiang C. et al. A modified simple method for induction of myocardial infarction in mice. Journal of Visualized Experiments. (178), e63042 (2021). [DOI] [PubMed] [Google Scholar]


