Abstract
The objective of this study was to review the prevalence and features of the beta thalassaemia trait in Jamaican populations. Screening of 221,306 newborns over the last 46 years has given an indication of the distribution and prevalence of beta thalassaemia genes, and screening of 16,612 senior school students in Manchester parish, central Jamaica, has provided their haematological features. The prevalence of the beta thalassaemia trait predicted from double heterozygotes was 0.8% of 100,000 babies in Kingston, 0.9% of 121,306 newborns in southwest Jamaica, and 0.9% of school students in Manchester. Mild beta+ thalassaemia variants (-88 C>T, -29 A>G, -90 C>T, polyA T>C) accounted for 75% of Kingston newborns, 76% of newborns in southwest Jamaica, and 89% of Manchester students. Severe beta+ thalassaemia variants were uncommon. Betao thalassaemia variants occurred in 43 patients and resulted from 11 different variants of which the IVSII-849 A>G accounted for 25 (58%) subjects. Red cell indices in IVSII-781 C>G did not differ significantly from HbAA, and this is probably a harmless polymorphism rather than a form of beta+ thalassaemia; the removal of 6 cases in school screening had a minimal effect on the frequency of the beta thalassaemia trait. Red cell indices in the beta+ and betao thalassaemia traits followed established patterns, although both were associated with increased HbF levels. The benign nature of beta+ thalassaemia genes in Jamaica means that cases of sickle cell-beta+ thalassaemia are likely to be overlooked, and important clinical questions such as the role of pneumococcal prophylaxis remain to be answered.
Keywords: Beta thalassaemia, Newborn screening, Jamaica, Sickle cell disease
Introduction
The current HbVar database (Giardine et al. 2021) lists over 300 variants associated with beta thalassaemia, but most reports are of single-family pedigrees, and there is limited information on their prevalence and distribution in populations. Studies in Jamaica over the last 46 years have screened 221,306 at birth and 16,612 senior school students; the former provide information on the relative prevalence and distribution of the trait, and the latter have allowed a description of red cell indices in some of the more common variants. The types and prevalence of variants causing beta thalassaemia in the Jamaican population provide useful information on the nearly 3 million Jamaican residents but also on the large Jamaican diaspora.
Material and methods
Ascertainment of subjects
Two populations were established by newborn screening. Victoria Jubilee Hospital (VJH) is the main Government maternity hospital serving the corporate area of Kingston where, between June 1973 and December 1981, a total of 100,000 consecutive non-operative deliveries were screened by methods to detect sickle cell disease (Serjeant et al. 1974; Serjeant et al. 1986). Newborn screening in southwest Jamaica commenced in March 2008 with a phased introduction of screening in 13 hospitals by March 2014. Results up to December 31, 2016, have been published (Mason et al. 2016a; Serjeant et al. 2019), and further data to a total of 121,306 deliveries screened up to December 31, 2019, provided the molecular basis of haemoglobin variants (Serjeant et al. 2022). A third population (Mason et al. 2016b), established by the screening of 16,612 students mostly aged 15–19 years attending 15 secondary schools in Manchester parish in central Jamaica over a 6-year period (academic years 2007–2013), provided information on some red cell characteristics. All students received preliminary lectures on sickle cell disease and its genetics, were given explanatory letters for their parents, and were invited to attend for free, voluntary blood tests at sites in the schools determined by the school staff.
Laboratory methods
The diagnostic methods inevitably changed over the 46-year period. Screening at Victoria Jubilee Hospital, which commenced in 1973, used liquid blood samples, taken as the umbilical cord was cut, which were analysed by haemoglobin electrophoresis on cellulose acetate with confirmation of all variant bands by agar gel (Serjeant et al. 1974). For deliveries in southwest Jamaica, which commenced in 2008, blood spots were collected from the umbilical cord, dried, and analysed by electrophoresis until high-pressure liquid chromatography (HPLC) became available which was used for the later 80% of samples. Bands of HbS or HbC with less than 25% HbA were investigated by family studies or sequencing of DNA if family studies were incomplete or inconsistent. For newborns, the prevalence of molecular variants was derived from subjects with sickle cell-beta+ thalassaemia and sickle cell-betao thalassaemia in the Jamaican Cohort and in southwest Jamaica from parental studies.
For screening of school students, a 5 ml EDTA blood sample was taken by venipuncture, haematological indices measured in electronic cell counters, and rapid haemolysates analysed by electrophoresis (Mason et al. 2016b). Haemoglobin bands in the position of HbS were confirmed by slide sickling tests and in the position of HbC by agar gel electrophoresis at pH 6.2. Samples, considered candidates for the beta thalassaemia trait (HbAA phenotype, mean cell haemoglobin ≤ 26 pg, and red cell distribution width coefficient of variation (RDW[CV]) below 18), had estimations of HbA2, which, if ≥ 3.5%, proceeded to DNA analysis. This was performed at the University of Heidelberg, Germany, by Sanger sequencing of the β-globin gene including the promoter region following PCR-amplification using primers as published (Vetter et al. 1997). In the first 3355 of 16,612 (20.2%) students, HbA2 was estimated by the less accurate microcolumn method, and when the more accurate HPLC technology became available, the apparent prevalence of values ≥ 3.5% rose from 0.66 to 0.96% (Mason et al. 2016a). The primary purpose of this screening was to determine haemoglobin genotype, and since measurement of fetal haemoglobin (HbF) and HbA2 levels was limited to candidates for the beta thalassaemia trait, this would have introduced a bias. More valid distributions for HbF and HbA2 were therefore extracted from the HbAA controls of the Jamaican cohort study and, when matched to the same age distribution, yielded multiple observations in each individual: simultaneous estimates for HbF and HbA2 were available in 151 individuals and for HbF alone in an additional 27 subjects. The latter values were measured by alkali denaturation for HbF (Betke et al. 1959) and elution of the HbA2 band after electrophoresis as previously described (Mason et al. 1982; Serjeant et al. 1978).
Statistical methods
Values are expressed as counts, median, and means with standard deviations and stratified by gender. The distribution of HbF which is skewed was normalised by natural logarithmic transformation before being expressed as geometric means with 95% confidence intervals. Differences in means between groups were assessed by analysis of variance (ANOVA) with post hoc comparisons by Scheffe’s test. For variables where the variances were heteroscedastic, the Kruskal-Wallis procedure was used to compare distributions with post hoc comparisons done with the Wilcoxon rank-sum test. Analyses were performed with Stata Statistical Software: Release 17 (College Station, TX: StataCorp LLC).
Results
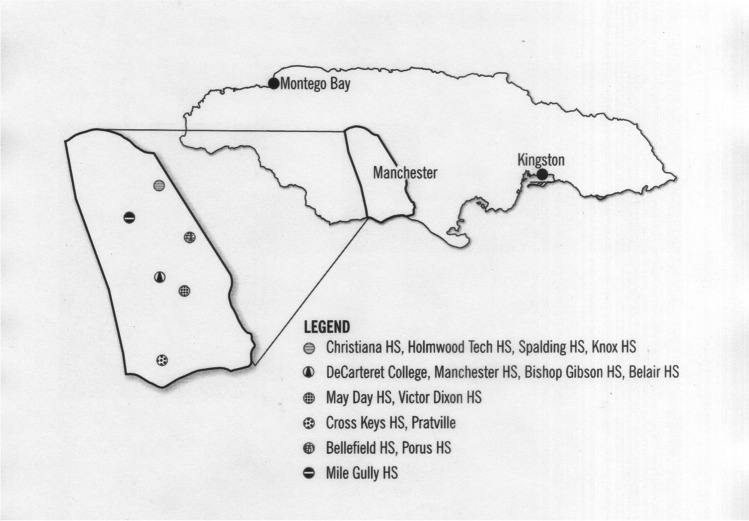
An outline map of Jamaica provides orientation for the two major cities and for the parish of Manchester along with the distribution of the 15 participating schools (Fig. 1). Of these, six served the parish capital Mandeville, four were in the north of the parish, two in the south, two in the east, and one in the centre of the parish. The population of the island is 2.8 million (estimated at July 2023), and the racial breakdown is 76% West African origin, 15% African-European, 3% East Indian (from India), 3% Caucasian, and 1% Chinese (World Population Review quoting Statistical Institute of Jamaica 2023).
Fig. 1.
Jamaica illustrating the site of Manchester parish and the participating schools
Benign beta+ thalassaemia variants accounted for 256/321 (80%) overall, 33/44 (75%) newborns in Kingston, 85/112 (76%) newborns in southwest Jamaica, and 130/146 (89%) of the students in the Manchester Project (Table 1). The variants -88 C>T and -29 A>G were most common, and severe beta+ thalassaemia characterised by 5–10% HbA, when inherited with HbS, were uncommon. Betao thalassaemia variants occurred in 43 (14%) of the combined populations, of which IVSII-849 A>G accounted for 25 (58%) and 10 other molecular variants were identified. The frequency for the beta thalassaemia gene of 0.0048169 in southwest Jamaica was significantly greater (p < 0.01) than the 0.003010 derived from the prevalence of sickle cell-beta+ thalassaemia in the Victoria Jubilee population (Serjeant et al. 1986) consistent with a greater prevalence of beta thalassaemia gene in southwest Jamaica.
Table 1.
Beta thalassaemia mutations in the three populations
| Victoria Jubilee | Manchester | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variant | Newborn screening | Newborn screening | School screening | Total | ||||||||
| HGVS nomenclature | Sβ+thal. | Sβo thal. | Sβ+thal. | Sβothal. | Cβ+thal. | Cβo thal. | Aβthal. | Sβ+thal. | Sβothal. | |||
| Mild β+ | ||||||||||||
| -90 C>T | HBB: c.-140C>T | 3 | 11 | 14 | ||||||||
| -88 C>T | HBB: c.-138C>T | 10 | 31 | 7 | 60 | 4 | 112 | |||||
| -87 C>A | HBB: c.-137C>A | 1 | 2 | 3 | ||||||||
| -29 A>G | HBB: c.-79A>G | 20 | 26 | 12 | 36 | 4 | 98 | |||||
| -28 A>G | HBB: c.-78A>G | 3 | 3 | |||||||||
| PolyA T>C | HBB: c.*110T>C | 2 | 4 | 1 | 6 | 13 | ||||||
| Cd24 T>A | HBB: c.75T>A | 1 | 1 | |||||||||
| Cd129 GCC→GTC | HBB: c.389C>T | 2 | 2 | |||||||||
| IVSI-108 T>C | HBB: c.93-23T>C | 2 | 2 | |||||||||
| IVSI-110 G>A | HBB: c.93-21G>A | 2 | 2 | |||||||||
| IVSII-781 C>G | HBB: c.316-70C>G | 6 | 6 | |||||||||
| Subtotal | 33 | 65 | 20 | 130 | 8 | 256 | ||||||
| Severe β+ | ||||||||||||
| IVSI-5 G>A | HBB: c.92+5G>A | 3 | 1 | 3 | 7 | |||||||
| IVSII-5 G>C | HBB: c.315+5G>C | 1 | 1 | 2 | ||||||||
| IVSII-654 C>T | HBB: c.316-197C>T | 1 | 1 | 2 | ||||||||
| Subtotal | 0 | 4 | 2 | 4 | 1 | 11 | ||||||
| βo | ||||||||||||
| IVS1-2 T>C | HBB: c.92+2T>C | 1 | 1 | |||||||||
| IVSII-1 G>A | HBB: c.315+1G>A | 2 | 2 | 1 | 5 | |||||||
| IVSII-849 A>G | HBB: c.316-2A>G | 4 | 9 | 1 | 10 | 1 | 25 | |||||
| Cd17 AAG→TAG | HBB: c.52 A>T | 1 | 1 | |||||||||
| Cd30 (-1) G>C† | HBB: c.92G>C | 3 | 1 | 4 | ||||||||
| Cd43 GAG→TAG | HBB: c.130 G>T | 1 | 1 | |||||||||
| Cd47 +A | HBB: c.143_144+A | 1 | 1 | |||||||||
| Cd106/107 +G | HBB: c.321_322+G | 2 | 2 | |||||||||
| Single HbS gene | 1 | 1 | ||||||||||
| 1393 bp deletion** | 1 | 1 | ||||||||||
| FS6 –A | HBB: c.20delA | 1 | 1 | |||||||||
| Undetermined | 2 | 2 | 0 | 0 | 2 | 0 | 4 | 1 | 0 | 11 | ||
| Subtotal | 2 | 13 | 0 | 16 | 2 | 3 | 16 | 1 | 1 | 54 | ||
| Grand total | 35 | 13 | 69 | 16 | 24 | 3 | 150 | 10 | 1 | 321 | ||
Apparent CC syndromes for Victoria Jubilee and for Manchester students were not fully characterized and remain phenotypes
Eight subjects manifested 2 variants. (i) -88 C>T and IVSI-108 T>C, (ii) -88 C>T and IVSII-814 G>T, (iii) -29 A>G and -1 T>C, (iv) -29 A>G and -90 C>T, (v) -29 A>G and IVSI-108 T>C, (vi) IVSI-5 G>A and IVSI-108 T>C, (vii–viii) IVSII-849 A>G and IVSI-108 T>C
**HBB NG_000007.3:g.70060_7145de l139 †Hb Monroe
Red cell indices (Table 2) did not differ between the common variants for mild beta+ thalassaemia (-88 C>T, -29 A>G, -90 C>T, PolyA T>C). Compared to HbAA controls, the -88 C>T and -29 A>G variants did not deviate consistently in total haemoglobin, but had higher red cell counts and lower MCV, all significant at the p < 0.001 level in both genders; the -90 C>T and the PolyA T>C showed similar trends but at lower levels of significance possibly because of smaller numbers of cases. The IVSII-781 C>G variant differed from the other beta+ variants and did not differ from the HbAA genotype except for a modest elevation of HbA2 which could have resulted from the sampling protocol. Compared to the normal controls, the most common betao thalassaemia variant, IVSII-849 A>G, tended to have lower haemoglobin and lower MCV and higher red cell counts in males but not females, the latter because of a small number of cases.
Table 2.
Selected red cell indices depicted as mean, SD (median) in beta thalassaemia trait and normal AA phenotypes with significance of differences
| Phenotype | (n) | Hb (g/dL) | RBC (×1012/L) | MCV (fL) | p value deviation from HbAA | ||
|---|---|---|---|---|---|---|---|
| Hb | RBC | MCV | |||||
| Males | |||||||
| HbAA | 5720 | 14.5, 1.2 (14.5) | 5.1, 0.4 (5.1) | 84.0, 5.7 (85) | - | - | - |
| -29 A>G | 19 | 13.6, 0.8 (13.5) | 5.8, 0.5 (5.7) | 70.8, 3.7 (70) | 0.12 | <0.001 | <0.001 |
| -88 C>T | 26 | 13.6, 1.1 (14.0) | 5.8, 0.5 (5.7) | 71.5, 4.0 (71) | 0.017 | <0.001 | <0.001 |
| -90 C>T | 5 | 13.6, 1.5 (14.1) | 6.0, 0.4 (5.7) | 71.2, 8.1 (70) | 0.8 | 0.002 | 0.0024 |
| Poly A T>C | 3 | 13.8, 0.9 (14.1) | 6.0, 0.6 (6.1) | 71.3, 0.3 (70) | 0.9 | 0.052 | 0.005 |
| IVSII-781 C>G | 2 | 14.9, 1.5 (14.9) | 5.8, 0.4 (5.8) | 79.5, 3.6 (80) | 1.0 | 0.6 | 0.13 |
| IVSII-849 A>G | 8 | 12.7, 1.5 (12.6) | 6.2, 0.4 (6.3) | 62.7, 3.5 (63) | 0.003 | <0.001 | <0.001 |
| Females | |||||||
| HbAA | 7219 | 12.5, 1.2 (12.6) | 4.5, 0.4 (4.5) | 83.0, 7.1 (84) | - | - | - |
| -29 A>G | 16 | 12.0, 0.6 (12.1) | 5.2, 0.4 (5.0) | 71.4, 3.0 (72) | 0.014 | <0.001 | <0.001 |
| -88 C>T | 32 | 12.2, 0.8 (12.3) | 5.0, 0.4 (5.0) | 73.7, 3.9 (74) | 0.056 | <0.001 | <0.001 |
| -90 C>T | 6 | 12.2, 1.0 (12.5) | 5.5, 0.7 (5.5) | 69.9, 3.2 (69) | 0.4 | <0.001 | <0.001 |
| Poly A T>C | 2 | 12.1, 0.8 (12.1) | 5.2, 0.0 (5.2) | 72.8, 5.9 (73) | 0.4 | 0.33 | 0.051 |
| IVSII-781 C>G | 3 | 12.3, 0.5 (12.2) | 4.7, 0.3 (4.7) | 82.1, 2.3 (81) | 0.5 | 0.9 | 0.5 |
| IVSII-849 A>G | 2 | 10.9, 0.1 (10.9) | 5.4, 0.3 (5.4) | 64.0, 0.0 (64) | 0.04 | 0.1 | 0.018 |
Hb total haemoglobin, RBC red cell count, MCV mean cell volume
HbF levels were significantly elevated in the 4 beta+ thalassaemia traits and in the betao thalassaemia traits but did not deviate from normal in the IVSII-781 C>G variant (Table 3). Elevations of HbA2 showed a similar pattern, although levels were increased in the IVSII-781C>G variant.
Table 3.
HbF (geometric means) and HbA2 (means, SD) in beta thalassaemia trait compared with cohort HbAA phenotypes with significance of differences
| Phenotype | n | HbF (95% CI) | p value deviation from HbAA | n | HbA2 mean (SD) | p value deviation from HbAA |
|---|---|---|---|---|---|---|
| Males | ||||||
| HbAA | 87 | 0.27 (0.24, 0.31) | - | 71 | 2.82 (0.43) | - |
| Mild β+ thalassaemia | 41 | 2.34 (1.71, 3.21) | <0.001 | 53 | 5.67 (0.44) | 0.001 |
| IVSII-781 C>G | 1 | 0.90 | 0.104 | 2 | 3.5 (0) | 0.047 |
| IVSII-849 A>G | 6 | 0.64 (0.48, 0.86) | 0.006 | 8 | 5.43 (0.92) | 0.001 |
| Females | ||||||
| HbAA | 94 | 0.31 (0.27, 0.35) | - | 80 | 2.84 (0.30) | - |
| Mild β+ thalassaemia | 42 | 2.94 (2.25, 3.85) | <0.001 | 55 | 5.27 (0.64) | 0.001 |
| IVSII-781 C>G | 1 | 0.90 | 0.146 | 3 | 3.57 (0.06) | 0.009 |
| IVSII-849 A>G | 2 | 1.94 (0.73, 5.18) | 0.001 | 2 | 5.45 (0.21) | 0.001 |
Discussion
The great majority of the beta thalassaemia genes in Jamaica are of the mild β+ thalassaemia type, and it is likely that the overall prevalence for beta thalassaemia is less than 1%. Differentiation of beta thalassaemia variants is technically feasible in the newborn period but cumbersome for community-based programmes, and the current values are extrapolated from the relative prevalences of HbS- and HbC-beta thalassaemia syndromes. Analysis of the Victoria Jubilee data, based on cases of sickle cell-β+ and sickle cell-βo thalassaemia, predicted relative gene frequencies of 0.00556 and 0.00236 for a combined total of 0.00792 or approximately 0.8%. Similar calculations on babies born in southwest Jamaica showed the beta thalassaemia trait in 112/121,306 (0.92%). The most reliable estimate of the frequency of the beta thalassaemia trait should come from the school screening programme, but the prevalence may have been underestimated in the first 20% as indicated in the “Methods” section. Despite this potential error, the beta thalassaemia gene frequency was higher in southwest Jamaica, consistent with previous observations that the clinic operating in Montego Bay in the west of the island served approximately one tenth of the national database known to the Sickle Cell Unit, yet accounted for one-third of the cases of sickle cell-beta+ thalassaemia (unpublished data). The overall prevalence of the beta thalassaemia trait in Jamaica is therefore of the order of 0.9% and may be marginally lower if the variant IVSII-781 C>G is excluded.
The analysis of red cell indices confirmed major differences between the mild beta+ thalassaemia mutations and the small number with betao mutations, and it is unlikely that these were significantly biased by the lack of data on iron deficiency and on the frequency of alpha thalassaemia. Although potential weaknesses of the study, an arbitrary formula was derived using RDW[CV] which will have excluded a major contribution from iron deficiency, but this could not be confirmed within the context of the study. Although the alpha globin gene number was not available, there is no reason for the ratio to diverge from the 30% prevalence of heterozygous alpha thalassaemia reported in the Jamaican population (Serjeant 2022).
There is an extensive literature on the beta thalassaemia trait in different racial groups (Weatherall and Clegg 1981) but only limited data on populations of predominantly West African ancestry. An early paper comparing the features of Jamaican βo and β+ thalassaemia trait (Millard et al. 1977) preceded identification of the DNA molecular basis, and the current data with identification of the molecular substitution confirms the red cell indices and increased HbF levels, although the mechanism of the latter is currently unknown. The IVSII-781 C>G variant, sometimes assumed to be a form of beta thalassaemia, did not have thalassaemic red cell indices, and the elevated HbA2 was probably a feature of the sampling procedure. On balance, it seems likely that the IVSII-781 C>G variant is a harmless polymorphism rather than a form of beta thalassaemia.
The assignment of perceived severity of beta thalassaemia genes into mild β+, severe β+, or βo types was complicated by discrepancies between clinical course and that predicted from the molecular substitution. For example, the variant Codon 129 GCC→GTC (Hb La Desirade) produces no HbA when inherited with HbS suggesting severity, yet the features of HbS/Hb La Desirade were clinically and haematologically mild (Merault et al. 1986), so it has been classed as a mild β+ mutation. The syndrome HbS-βo thalassaemia is uncommon in Jamaica and clinically unpredictable. The absence of HbA might be expected to cause a severe clinical course, but it is highly variable and often benign possibly because of other interacting genes. Transfusion-dependent beta thalassaemia among people of West African origin is rare in Jamaica but might be expected to occur once in every 200,000 births.
Since sickle cell-beta+ thalassaemia in Jamaica results predominantly from mild molecular variants, it becomes important to know more of the clinical features and pathology. These are currently not well documented, partly because their benign course ensures that many cases do not present to medical attention so that it is perceived to be uncommon. In Jamaica, this syndrome was detected in 35 babies screened at Victoria Jubilee Hospital in Kingston for a prevalence of 0.035% and in 65 babies in southwest Jamaica for a prevalence of 0.054%. There are no data to answer even simple questions such as whether the 15–25% HbA of most cases (Sweeting et al. 1997; Donaldson et al. 2000) allows normal splenic function to persist beyond the high-risk period for pneumococcal sepsis, casting doubt on the role of pneumococcal prophylaxis.
Author contributions
GRS and BES conceived the study; KPM, FG, R-A G, GRS, and LW conducted the blood collection and analysis; MR performed the statistical analysis; AEK and MH performed the DNA analyses. All authors read and approved the manuscript.
Funding
This work was funded in part by the National Health Fund of Jamaica, grant HPP70.
Declarations
Ethical approval
The study was approved by the Ministry of Health and the Ministry of Education of the Jamaican Government and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Betke K, Marti HR, Schlicht I. Estimation of small percentages of foetal haemoglobin. Nature. 1959;185:1877–1878. doi: 10.1038/1841877a0. [DOI] [PubMed] [Google Scholar]
- Donaldson A, Old J, Fisher C, Serjeant BE, Serjeant GR. Jamaican Sβ+ thalassaemia: mutations and haematology. Br J Haematol. 2000;108:290–294. doi: 10.1046/j.1365-2141.2000.01829.x. [DOI] [PubMed] [Google Scholar]
- Giardine BM, Joly P, Pissard S, Wajcman H, Chui DHK, Hardison RC, Patrinos GP. Clinically relevant updates of the HbVar database of human hemoglobin variants and thalassemia mutations. Nucleic Acids Res. 2021;49:D1192–D1196. doi: 10.1093/nar/gkaa959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason K, Gibson F, Gardner R, Warren L, Fisher D, Happich M, Kulozik A, Hambleton I, Serjeant B, Serjeant G. Newborn screening for sickle cell disease; Jamaican experience. West Ind Med J. 2016;65:18–26. doi: 10.7727/wimj.2015.492. [DOI] [PubMed] [Google Scholar]
- Mason K, Gibson F, Higgs D, Fisher C, Thein SL, Clark B, Kulozik A, Happich M, Serjeant B, Serjeant G. Haemoglobin variant screening in Jamaica: meeting student’s request. Br J Haematol. 2016;172:634–636. doi: 10.1111/bjh.13531. [DOI] [PubMed] [Google Scholar]
- Mason KP, Grandison Y, Hayes RJ, Serjeant BE, Serjeant GR, Vaidya S, Wood WG. Post-natal decline of fetal haemoglobin in homozygous sickle cell disease: relationship to parental HbF levels. Br J Haematol. 1982;52:455–463. doi: 10.1111/j.1365-2141.1982.tb03915.x. [DOI] [PubMed] [Google Scholar]
- Merault G, Keclard L, Garin J, Poyart C, Blouquit Y, Arous N, Galacteros F, Feingold J, Rosa J. Hemoglobin La Desirade αA2β2 129 (H7) Ala→Val: a new unstable hemoglobin. Hemoglobin. 1986;10:593–605. doi: 10.3109/03630268609036564. [DOI] [PubMed] [Google Scholar]
- Millard DP, Mason K, Serjeant BE, Serjeant GR. Comparison of the haematological features of the βo and β+ thalassaemia traits in Jamaican Negroes. Br J Haematol. 1977;36:161–170. doi: 10.1111/j.1365-2141.1977.tb00636.x. [DOI] [PubMed] [Google Scholar]
- Serjeant BE, Forbes M, Williams LL, Serjeant GR. Screening cord bloods for detection of sickle cell disease in Jamaica. Clin Chem. 1974;20:666–669. doi: 10.1093/clinchem/20.6.666. [DOI] [PubMed] [Google Scholar]
- Serjeant BE, Mason KP, Serjeant GR. The development of HbA2 in normal Negro infants and in sickle cell disease. Br J Haematol. 1978;39:259–265. doi: 10.1111/j.1365-2141.1978.tb01096.x. [DOI] [PubMed] [Google Scholar]
- Serjeant GR. Phenotypic variation in sickle cell disease: the role of beta globin haplotype, alpha thalassemia and fetal hemoglobin in HbSS. Expert Rev Hematol. 2022;15:107–116. doi: 10.1080/17474086.2022.2040984. [DOI] [PubMed] [Google Scholar]
- Serjeant GR, Serjeant BE, Forbes M, Hayes RJ, Higgs DR, Lehmann H. Haemoglobin gene frequencies in the Jamaican population: a study of 100,000 newborns. Br J Haematol. 1986;64:253–262. doi: 10.1111/j.1365-2141.1986.tb04117.x. [DOI] [PubMed] [Google Scholar]
- Serjeant GR, Serjeant BE, Mason K, Happich M, Kulozik A. Beta thalassemia mutations in Jamaica: geographic variation in small communities. Hemoglobin. 2019;42:294–296. doi: 10.1080/03630269.2018.1540354. [DOI] [PubMed] [Google Scholar]
- Serjeant GR, Serjeant BE, Mason KP, Gibson F, Gardner R-A, Warren L, Hambleton IR, Thein SL, Happich M, Kulozik AE (2022) Newborn screening for abnormal haemoglobins in Jamaica: practical issues in an island programme. J Med Screen. 10.1177/09691413221111209 [DOI] [PubMed]
- Sweeting I, Serjeant BE, Thomas PW, Serjeant GR. Microchromatographic quantitation of HbA levels in phenotypes of sickle cell-β+ thalassemia. J Chromatogr. 1997;700:269–274. doi: 10.1016/S0378-4347(97)00270-3. [DOI] [PubMed] [Google Scholar]
- Vetter B, Schwarz C, Kohne E, Kulozik AE. Beta-thalassaemia in the immigrant and non-immigrant German populations. Br J Haematol. 1997;97:266–272. doi: 10.1046/j.1365-2141.1997.342674.x. [DOI] [PubMed] [Google Scholar]
- Weatherall DJ, Clegg JB. Thalassaemia syndromes. 3. Oxford, UK: Blackwell Scientific Publications; 1981. [Google Scholar]
- World Population Review quoting Statistical Institute of Jamaica 2023. Accessed from internet on 16 Jun 2023