Abstract
Objective:
Individuals who experience gambling harms report that sustained recovery involves changing both gambling behaviors and psychological symptoms, as well as building a meaningful life. However, there is limited understanding about the effect of cognitive behavioral (CB) techniques on psychological symptoms and quality of life. The purpose of the current study was to examine the effect of CB techniques for gambling-related harms on broader recovery outcomes such as psychological symptoms and quality of life.
Method:
A systematic article search was conducted to identify randomized controlled trials of CB techniques with nonactive and minimal treatment control groups that assessed psychological symptoms or quality of life as outcomes. Random effects meta-analysis was used to examine the effect of CB techniques relative to nonactive and minimal treatment control groups.
Results:
A total of nine studies representing 658 participants was included. Eight studies reported outcomes on depression and anxiety, three on substance use, and six on quality of life. CB techniques significantly reduced anxiety (g = −0.44) and depression (g = −0.35) at posttreatment, but not substance use. CB techniques also significantly increased quality of life at posttreatment (g = 0.40). There was a large amount of heterogeneity suggesting the magnitude of effects could vary significantly in future randomized trials.
Conclusions:
Future studies should examine the longitudinal associations between gambling harms, psychological symptoms, and quality of life, and to assess whether changes in gambling harms throughout treatment precede or are a consequence of changes in psychological symptoms and quality of life.
Keywords: efficacy, treatment, problem gambling, gambling disorder
Gambling-related harms occur when individuals experience adverse consequences due to engagement in gambling (Langham et al., 2015). Many individuals who experience these harms meet criteria for the DSM-5 psychiatric diagnosis of gambling disorder (American Psychiatric Association, 2013), but others will experience harms without meeting diagnostic criteria (Langham et al., 2015; Weinstock et al., 2017). Regardless of the label, gambling harms constitute a significant public health concern (Wardle et al., 2019) and often co-occur with other psychological symptoms (Dowling et al., 2015; Lorains et al., 2011; Petry et al., 2005).
Among individuals seeking treatment for gambling harms, approximately 23% reported a mood disorder, 18% an anxiety disorder, 56% nicotine use disorder, 21% alcohol use disorder, and 7% drug use disorder (Dowling et al., 2015). The temporal relation between gambling harm and co-occurring psychological symptoms is not well understood, as there is evidence that psychological symptoms precede the onset of gambling harms (Kessler et al., 2008) and that gambling harms precede psychological symptoms (Afifi et al., 2016; Sundqvist & Rosendahl, 2019). However, it is well established that co-occurring psychological symptoms increase the complexity of clinical presentations (Peter et al., 2016; Pfund et al., 2017; Pietrzak & Petry, 2005).
Emerging research suggests that individuals with lived experiences of gambling harms believe that sustained recovery involves changing both gambling behaviors and psychological symptoms, as well as building a meaningful life beyond gambling (Pickering et al., 2020). In a review of gambling treatment outcomes, Pickering and colleagues (2017) identified 63 different outcome measures that spanned gambling-specific constructs, co-occurring psychological symptoms, and quality of life. Yet few studies have identified the effect of treatment on outcomes beyond gambling-specific constructs. A comprehensive review that explored this question identified only six randomized controlled trials of integrated treatments that included components targeting gambling and co-occurring psychological symptoms (Dowling et al., 2016). These integrated treatments involved psychosocial interventions, typically cognitive-behavioral (CB) techniques, and pharmacotherapy either in isolation or combination (Echeburúa et al., 2011; Grant et al., 2014; Grant & Potenza, 2006; Hollander et al., 2005; Korman et al., 2008; Toneatto et al., 2009). Since then, other randomized controlled trials have been published on integrated treatments (Bücker et al., 2018, 2021), but the small number of studies on those treatments proves challenging for quantifying the effect of treatment on psychological symptoms and quality of life recovery outcomes. To increase the potential pool of studies to review, it would be advantageous to review the parallel literature that examines the effect of treatments that do not necessarily incorporate treatment components targeting psychological symptoms (i.e., “nonintegrated treatments”) and determine whether nonintegrated treatments affect psychological symptoms and quality of life.
To date, almost a dozen systematic reviews and/or meta-analyses have been conducted on the efficacy of nonintegrated treatments for gambling harms (e.g., Cowlishaw et al., 2012; Petry et al., 2017; Pfund et al., 2020). The most recent meta-analysis indicated that CB techniques targeting gambling significantly reduced gambling disorder symptom severity and gambling behaviors relative to nonactive and minimally treated controls at posttreatment (Pfund et al., 2022). However, questions remain about the effect of nonintegrated CB techniques on psychological symptoms and quality of life.
There is a strong theoretical rationale to believe that CB techniques would affect psychological symptoms and quality of life in addition to gambling behavior and gambling harms. CB techniques are based on social cognitive theory where individuals are considered the agents of change (Bandura, 2001), and the change targets (Pfund & Ginley, 2019) include cognitions (e.g. “I feel lucky”) and behaviors (e.g. withdrawing money on a debit card to gamble). As a person changes their cognitions and behaviors, they may experience reductions in gambling harms and gambling behavior and an increase in self-efficacy around their ability to cope in a range of challenging situations (Bandura, 2001) that may then correspond to changes in psychological symptoms and quality of life (Sander & Peters, 2009; Schluter et al., 2019). The CB techniques may also be tailored in ways that include conversations about changing psychological symptoms and quality of life in the context of gambling harms and gambling behavior (American Psychological Association, 2006).
The aim of the present study was to systematically review the literature on randomized controlled trials of CB techniques for gambling harms and estimate the effect of these techniques on other psychological symptoms and quality of life. Results of the present systematic review and meta-analysis can increase understanding about the effect of gambling treatments on the spectrum of recovery outcomes and inform the design of future randomized controlled trials.
Method
We reported how we determined our sample size, all data exclusions (if any), all manipulations, and all measures in the study. The current study was part of a larger preregistered meta-analysis (PROSPERO ID = CRD42022288058) of 29 studies on the effect of CB techniques on gambling disorder severity and gambling behavior (Pfund et al., 2022). The current study presented new results from a subset of the 29 total studies that reported psychological functioning and well-being outcomes. The current study’s methods were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Page et al., 2021) and A Measurement Tool to Assess Systematic Reviews-2 (Shea et al., 2017) guidelines. No deviations were made from the preregistered protocol.
Search Strategy
Searches were conducted in seven databases (i.e., Academic Search Complete, Embase, Google Scholar, PsycINFO, PubMed, ScienceDirect, and Web of Science Core Collection) and two clinical trial registries (i.e., Clinicaltrials.gov and International Standard Randomised Controlled Number) during July 2022. Reference lists of six past meta-analyses were also searched to identify additional articles (Augner et al., 2022; Bergeron et al., 2022; Cowlishaw et al., 2012; Gooding & Tarrier, 2009; Pfund et al., 2020; Sagoe et al., 2021).
Inclusion and Exclusion Criteria
Studies were included if they involved: (a) participants aged 18 years of age and older; (b) participants with problem gambling or gambling disorder as determined by an assessment with some validity evidence; (c) a treatment used CB techniques or a treatment that described key CB elements/objectives (e.g., cognitive restructuring, imaginal desensitization, relapse prevention, or stimulus control); (d) the treatment was not explicitly integrated and did not explicitly include components targeting both gambling and co-occurring psychological symptoms; (e) random assignment to two or more conditions with an inactive (i.e., no treatment, waitlist) or minimal treatment (i.e., assessment only, psychoeducation) condition; and (f) assessed psychological symptoms (i.e., anxiety, depression, alcohol use, drug use, nicotine use) or quality of life outcomes. Studies were excluded if they involved: (a) planned study protocols; (b) participants taking pharmacotherapy as part of the study protocol or as part of their medical care unrelated to the study that would directly affect outcomes; and (c) secondary analysis.
Study Identification
Two doctoral level clinical psychologists (RAP and SCP) screened studies at the title and abstract level. Two clinical psychology graduate students (SAK, DPF) then independently determined if articles were eligible based on inclusion and exclusion criteria at the full-text level. The interrater reliability at the title and abstract level was ᴋ = 0.93, and the interrater reliability at the full-text level was ᴋ = 0.94. All discrepancies were resolved through discussion.
Data Extraction
The outcomes of interest in the present study included psychological symptoms and quality of life outcomes. Psychological symptoms included anxiety, depression, and substance use because these symptoms are the most commonly co-occurring with gambling-related harms (Dowling et al., 2015; Lorains et al., 2011). Two authors (SAK, DPF) independently extracted outcomes to verify their accuracy.
Risk of Bias Assessment
The Cochrane Risk of Bias tool was used to assess for potential bias in randomized controlled trials (Higgins & Green, 2011). This tool requires authors to rate trials on several design features that might threaten the validity of results. In the current study, bias was assessed for the random sequence generation, allocation concealment, masking of outcome assessors, and completeness of outcome data. Selective outcome reporting was not rated because many trials are still not prospectively registered (Page & Higgins, 2016). Each domain was assigned high risk of bias, low risk of bias, or unclear risk of bias. Two authors (RAP, SAK) independently rated risk of bias using a codebook, and discrepancies were resolved through discussion. The interrater reliability for risk of bias ratings was ᴋ = 0.96.
Data Analysis Plan
When information needed to conduct meta-analysis was not reported in the original publication, authors were contacted with requests for data. Data were requested from the authors of five studies, and the authors of three studies responded. A remaining two studies were only partially analyzed because they did not report sufficient information to calculate effect sizes.
All meta-analyses were conducted in Comprehensive Meta-Analysis software. To examine the effect of CB techniques on recovery outcomes relative to nonactive controls, Hedges’s g effect sizes were computed. Hedges’s g was selected because it was expected that some studies might comprise small sample sizes, and Hedges’s g corrects for small sample sizes (Hedges & Olkin, 1985). If there were multiple indicators of outcomes, the Hedges’s g value, variance, and standard errors were averaged (Borenstein et al., 2009). The Q-statistic tested heterogeneity in the individual study effect sizes (Hedges & Olkin, 1985), and the I2 and τ2 statistics estimated the magnitude of heterogeneity between studies (Higgins et al., 2003). Prediction intervals (PI) were calculated to describe the effects of treatment in future settings and whether effects corresponded to benefit, null effects, or deterioration (IntHout et al., 2016).
Results
Study Identification
Figure 1 displays a flowchart of the study identification process. After screening articles at the title and abstract level and the full-text level, nine studies reported outcomes related to psychological symptoms and quality of life and were deemed eligible for review. Of these 9 unique studies, seven (78%) reported sufficient information to conduct meta-analysis.
Figure 1.
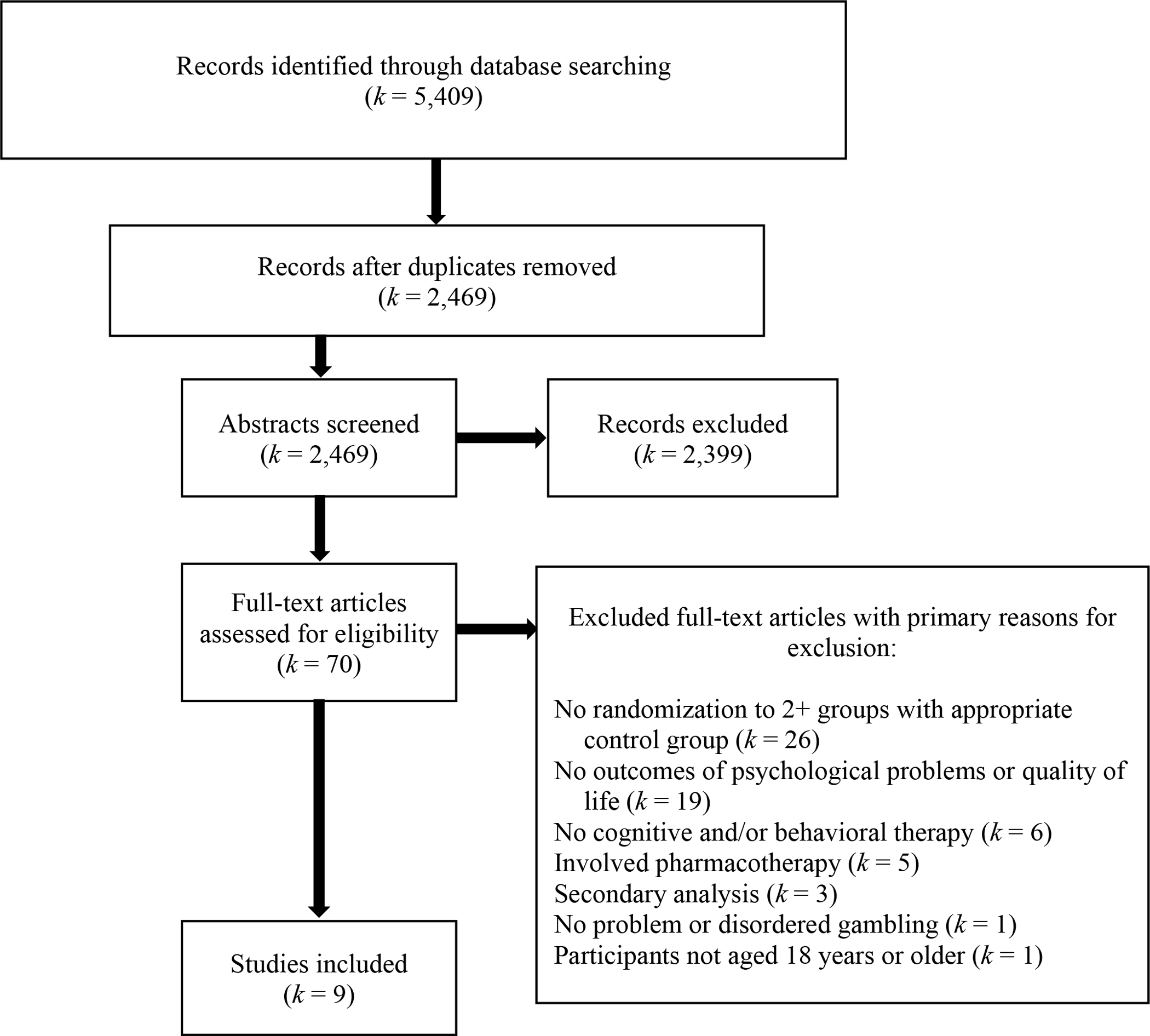
Study flowchart for identification of studies to be reviewed.
Study and Sample Characteristics
Table 1 presents the nine studies included in the systematic review and meta-analysis. Across the nine studies, a total of 658 participants were included. The mean age of participants was 44 years, and 62% of participants identified as male. The years of publication among the studies ranged from 2007 to 2018.
Table 1.
Relevant Studies, Study Conditions, Assessment Time Points, and Outcomes
| Study | Total N | Relevant study conditions | Posttreatment outcomes (months since baseline) | Follow-up Outcomes (months since termination) | Outcomes and Type of Measurement |
|---|---|---|---|---|---|
|
| |||||
| Boudreault et al. (2018) | 62 | CBT WB (31) Waitlist (31) |
Y (2.75) | N | Anxiety (BAI) Depression (BDI) Alcohol use (SAADQ) Quality of life (LSQ) |
| Carlbring & Smit (2008) | 66 | Internet CBT (34) Waitlist (32) |
Y (3) | N | Anxiety (HADS-A) Depression (HADS-D) Quality of life (QOLI) |
| Carlbring et al. (2010) | 96 | Group CBT (50) Waitlist (46) |
Y (3) | N | Anxiety (BAI) Depression (BDI-2) Alcohol use (# drinks/gambling day, # intoxicated gambling days) |
| Casey et al. (2017) | 115 | Internet CBT (60) Waitlist (55) |
Y (1.5) | N | Anxiety (DASS-A) Depression (DASS-D) Alcohol use (AUDIT) Quality of life (QOLI, SWLS) |
| Dowling et al. (2007) | 56 | CBT (14) Group CBT (17) Waitlist (25) |
Y (3) | N | Anxiety (STAI) Depression (BDI-2) |
| Grant et al. (2009) | 68 | CBT (33) GA referral (35) |
Y (2) | N | Anxiety (HAS) Depression (HRSD) Quality of life (QOLI) |
| Oei et al. (2010) | 102 | MI + CBT (37) Group MI + CBT (37) Waitlist (28) |
Y (1.5) | N | Quality of life (SWLS) |
| Oei et al. (2018) | 55 | CBT WB (23) Waitlist (32) |
Y (1.75) | N | Anxiety (DASS-A) Depression (DASS-D) Quality of life (SWLS, WHOQOL) |
| Wong et al. (2015) | 38 | Group CBT (18) Supportive counseling (20) |
Y (2.5) | N | Anxiety (DASS-A) Depression (DASS-D) |
Notes. AUDIT = Alcohol Use Disorders Identification Test; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; DASS-A = Depression Anxiety Stress Scale – Anxiety; DASS-D = Depression Anxiety Stress Scale – Depression; SAADQ = Short Alcohol Dependence Data Questionnaire; HAS = Hamilton Anxiety Scale; HADS – A = Hospital Anxiety and Depression Scale–Anxiety; HRSD = Hamilton Rating Scale for Depression; QOLI = Quality of Life Inventory; STAI = State Trait Anxiety Inventory; SWLS = Satisfaction with Life Scale; WHOQOL = World Health Organization Quality of Life
Highlighted rows indicate outcomes that could not be analyzed due to insufficient reporting of statistical information.
Measurement of Recovery Outcomes Across Included Studies
Table 1 also reports the spectrum of recovery outcomes assessed in each study, and how each outcome was measured. All measures used to assess these outcomes were self-report. All nine studies (100%) assessed outcomes at posttreatment, which ranged from 1.5 to 3 months after baseline. No studies assessed any outcome beyond the posttreatment assessment.
Eight studies (89%) reported anxiety outcomes, and seven (78%) reported sufficient information to conduct meta-analysis on the effect of CB techniques on anxiety. Anxiety was assessed using a range of measures, including the anxiety subscale of the Depression Anxiety Stress Scale (k = 3), the Beck Anxiety Inventory (k = 2), the Hamilton Anxiety Scale (k = 1), the anxiety subscale of the Hospital Anxiety and Depression Scale (k = 1), and the State Trait Anxiety Inventory (k = 1).
Likewise, eight studies (89%) reported depression outcomes, and seven (78%) reported sufficient information to conduct meta-analysis on the effect of CB techniques on depression. Depression was assessed using a range of measures, including the depression subscale of the Depression Anxiety Stress Scale (k = 3), either the first or second version of the Beck Depression Inventory (k = 3), the Hamilton Rating Scale for Depression (k = 1), and the depression subscale of the Hospital Anxiety and Depression Scale (k = 1).
Three studies (33%) reported substance use outcomes, and two (22%) reported sufficient information to conduct meta-analysis on the effect of CB techniques on substance use. All three studies focused on alcohol use, and these outcomes were assessed with the Alcohol Use Disorders Identification Test (k = 1), the Short Alcohol Dependence Data Questionnaire (k = 1), and alcohol use behavior (k = 1). No studies reported drug use or nicotine use outcomes.
Six studies (67%) reported quality of life outcomes, and four (44%) reported sufficient information to conduct meta-analysis on the effect of CB techniques on quality of life. Quality of life was often assessed with multiple measures within studies. The measures included the Quality of Life Inventory (k = 4), the Satisfaction with Life Scale (k = 2), the Life Satisfaction Questionnaire (k = 1), and the World Health Organization Quality of Life Scale (k = 1).
Effect of CB Techniques on Psychological Symptoms and Quality of Life
Table 2 presents a summary of the meta-analysis results across the psychological symptoms and quality of life outcomes. Figure 2 displays a forest plot of the Hedges’s g values for the effect of CB techniques on anxiety at posttreatment relative to control. CB techniques significantly reduced anxiety at posttreatment relative to control (g = −0.44, 95% CI [−0.70, −0.18], p < .001, τ2 = 0.05, 42%). However, the effects on anxiety could vary considerably in future trials (95% PI = −1.69, 0.81).
Table 2.
Effect of Cognitive-Behavioral Techniques on Psychological Symptoms and Quality of Life at Posttreatment with Confidence Intervals and Prediction Intervals
| Outcome | k | n | Hedges’s g | p | 95% CI | 95% PI |
|---|---|---|---|---|---|---|
|
| ||||||
| Anxiety | 7 | 409 | −0.44 | 0.001 | −0.70, −0.18 | −1.69, 0.81 |
| Depression | 7 | 408 | −0.35 | 0.04 | −0.69, −0.01 | −1.98, 1.28 |
| Alcohol use | 2 | 89 | −0.40 | 0.07 | −0.82, 0.03 | - |
| Quality of life | 4 | 245 | 0.43 | 0.002 | 0.16, 0.70 | −0.99, 1.85 |
Note. The 95% Prediction Interval could not be calculated for alcohol use due to the small number of studies comprised in the analysis.
Figure 2.

Forest plot of Hedges’s g Values for Cognitive-Behavioral Techniques versus Non-Active or Minimal Treatment Conditions on Anxiety
Notes. CBT = cognitive-behavioral therapy; MI = motivational interviewing
Figure 3 displays a forest plot of the Hedges’s g values for the effect of CB techniques on depression at posttreatment relative to control. CB techniques significantly reduced depression at posttreatment relative to control (g = −0.35, 95% CI [−0.69, −0.01], p =.04, τ2 = 0.14, I2 = 66%). However, the effects on depression could vary considerably in future trials (95% PI = −1.98, 1.28).
Figure 3.

Forest plot of Hedges’s g Values for Cognitive-Behavioral Techniques versus Non-Active or Minimal Treatment Conditions on Depression
Notes. CBT = cognitive-behavioral therapy; MI = motivational interviewing
Figure 4 displays a forest plot of the Hedges’s g values for the effect of CB techniques on substance use at posttreatment relative to control. CB techniques did not significantly reduce substance use at posttreatment relative to control (g = −0.40, 95% CI [−0.82, 0.03], p = .07). Due to the small number of studies, it was not possible to estimate heterogeneity of the effects.
Figure 4.
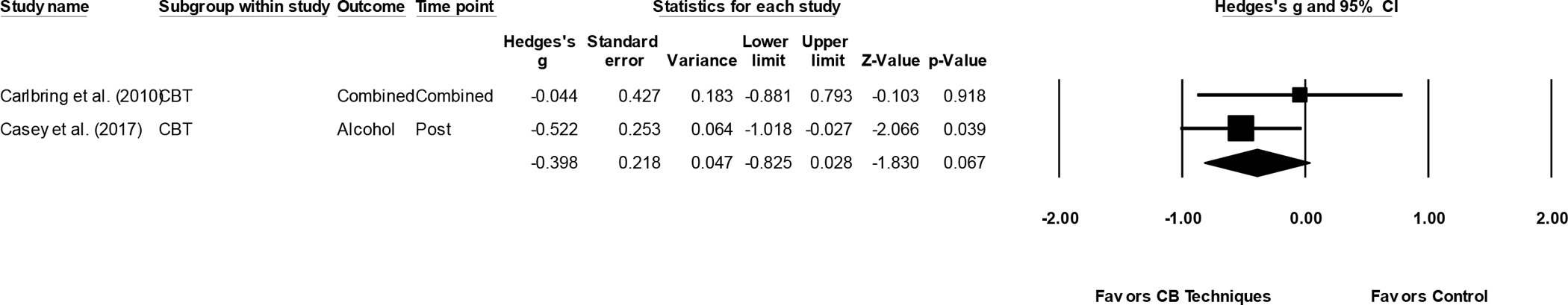
Forest plot of Hedges’s g Values for Cognitive-Behavioral Techniques versus Non-Active or Minimal Treatment Conditions on Substance Use
Notes. CBT = cognitive-behavioral therapy
Figure 5 displays a forest plot of the Hedges’s g values for the effect of CB techniques on quality of life at posttreatment relative to control. CB techniques significantly increased quality of life at posttreatment relative to control (g = 0.43, 95% CI [0.16, 0.70], p = .002, τ2 = 0.01, I2 = 11%). However, the effects on quality of life could vary considerably in future trials (95% PI = −0.99, 1.85).
Figure 5.
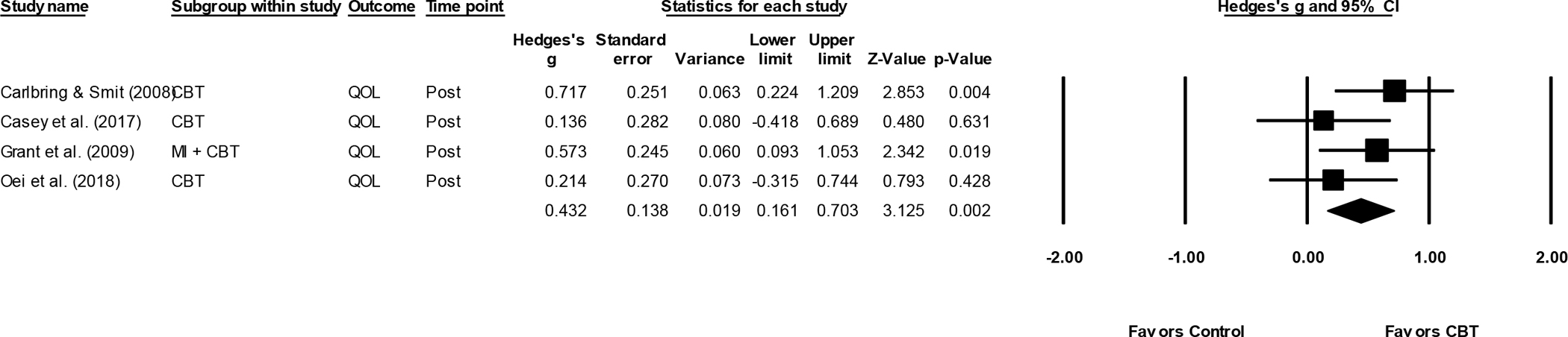
Forest plot of Hedges’s g Values for Cognitive-Behavioral Techniques versus Non-Active or Minimal Treatment Conditions on Quality of Life
Notes. CBT = cognitive-behavioral therapy; MI = motivational interviewing; QOL = quality of life
Risk of Bias Assessment
Table 3 presents the ratings for risk of bias on randomization sequence generation, allocation concealment, masking of assessors, and outcome data. Across the nine studies, no studies (0%) had low risk of bias across all four risk of bias domains. Five studies (56%) adequately described an appropriate method to generate the randomization sequence. Seven studies (78%) inadequately described a method to conceal the allocation sequence to the study team or used an inappropriate method to conceal the allocation sequence. No studies (0%) used an adequate method to mask outcome assessors. Five studies (56%) reported incomplete outcome data.
Table 3.
Risk of Bias Assessment for All Studies Included in the Systematic Review and Meta-Analysis
| Study | Randomization Sequence Generation | Allocation Concealment | Masking of Assessors | Outcome Data |
|---|---|---|---|---|
|
| ||||
| Boudreault et al. (2018) | + | ? | − | + |
| Carlbring & Smit (2008) | + | + | − | + |
| Carlbring et al. (2010) | + | + | − | − |
| Casey et al. (2017) | + | − | − | − |
| Dowling et al. (2007) | ? | ? | − | + |
| Grant et al. (2009) | ? | ? | − | + |
| Oei et al. (2010) | + | ? | ? | ? |
| Oei et al. (2018) | ? | ? | − | − |
| Wong et al. (2015) | ? | ? | − | + |
Note. + = low risk of bias; − = high risk of bias; ? = unclear risk of bias
Discussion
The aim of the present systematic review and meta-analysis was to determine the effect of nonintegrated CB techniques on psychological symptoms and quality of life relative to minimal or no treatment control conditions. Notably, as reported previously (Pfund et al., 2022), a larger set of identified studies were found to reduce gambling behavior and harms. Specifically, these studies reported that CB techniques reduced gambling symptoms and gambling behavior at posttreatment with moderate-to-large effect sizes. As for psychological symptoms and quality of life outcomes, CB techniques significantly decreased anxiety and depression and significantly increased quality of life at posttreatment. Although the present study did not test social cognitive theory, the results suggested that changes in gambling harms and gambling behavior may correspond to changes in psychological symptoms and quality of life. There is currently limited understanding of the directionality of these changes (Petry et al., 2016; Sander & Peters, 2009).
By contrast, the results indicated that CB techniques did not significantly reduce substance use outcomes at posttreatment. One possible explanation is that only two studies reported substance use outcomes, and the small number of studies in the analysis prevented the detection of a significant reduction in these outcomes. Another possible explanation is that the treatments in the present study did not address multiple behavior targets. Studies on samples of individuals who experience gambling harms and use substances suggests that treatment effects may be enhanced when treatment discusses the change of multiple health behaviors (e.g., gambling and alcohol use) rather than a single behavior (Rash et al., 2011) or integrates components that target multiple outcomes (see Dowling et al., 2016 for a comprehensive review of integrated treatments).
These results also indicated that CB techniques might not reliably affect psychological symptoms and quality of life for everyone. Specifically, there was a large amount of heterogeneity in posttreatment effect sizes, and the prediction intervals suggested that treatment effects on psychological symptoms and quality of life in future trials may result in some participants experiencing large improvements while other participants might not change and some might even deteriorate. The span of possible outcomes for those receiving treatment raises questions about how heterogeneity in CB techniques might differentially affect psychological symptoms and quality of life. For example, some CB techniques focused on imaginal desensitization of gambling scenarios (Grant et al., 2009), while others focused on correcting cognitive distortions and building coping skills, and others involved combinations of techniques (Dowling et al., 2007). The small number of studies asking this question prevented us from exploring how different CB components affected outcomes. Future studies might consider using treatment dismantling designs to understand what technique is contributing to what outcome.
Despite the promise of CB techniques in affecting psychological symptoms and quality of life outcomes, these results should be interpreted with caution due to the small number of studies and participants comprising the effect size estimates. As first suggested by Walker and colleagues (2006), future randomized trials should regularly assess psychological symptoms and quality of life. High comorbidity between gambling disorder and psychiatric disorders is the rule rather than the exception (Dowling et al., 2015; Lorains et al., 2011), and the lack of assessment limits understanding of treatment effects on psychological symptoms and quality of life. Many more randomized controlled trials are needed to comprehensively understand these effects.
Unfortunately, the high risk of bias present in the randomized controlled trials indicated the need to interpret the results with caution. This set of trials representing the effect of CB techniques on psychological symptoms and quality of life is characterized by inadequate descriptions of methods to conceal allocation to study conditions, a lack of masking outcome assessors (due to reliance on self-report measurements only), and incomplete outcome data. The impact of study bias on treatment efficacy could not be examined due to the small number of studies in the meta-analysis. However, it is important to recognize how these sources of bias in study design might affect the estimates of treatment effects. For example, meta-analyses indicate that clinician ratings of depression produce higher treatment effects than self-report measurements (Cuijpers et al., 2010). Such evidence raises questions about whether the effect sizes produced in the current meta-analysis are underestimated. Future trials should supplement self-report measures of psychological symptoms and quality of life with clinician interviews.
A limitation of the present meta-analysis was the narrow scope of substance use outcomes. For example, the assessments of substance use were restricted to alcohol use, and this restriction limited understanding of treatment effects on drug use and nicotine use. Furthermore, the assessments of substance use were primarily restricted to substance use symptoms, which limited understanding of the treatment effects on substance use behavior (i.e., frequency, intensity, duration). This distinction between substance use symptoms versus behavior is important considering the most recent meta-analysis indicated that CB techniques exerted greater effects on gambling symptoms than gambling behavior (Pfund et al., 2022). Thus, questions remain about differential treatment effects on substance use symptoms versus behaviors.
Another limitation was the lack of follow-up assessments. No studies in the present review assessed psychological symptoms of quality of life beyond the posttreatment assessment. It may be the case that reductions in gambling behaviors at posttreatment corresponded to subsequent reductions in psychological symptoms and increases in quality of life. Although it may also be the case that improvement in psychological systems and better quality of life led to reductions in gambling behaviors. Future studies should use longitudinal designs to understand the associations among reductions in gambling harms, reductions in psychological symptoms, and improvements in quality of life.
In conclusion, there is promise that CB techniques may abate psychological symptoms and improve quality of life. However, future work is needed given the high risk of bias present in existing randomized controlled trials, as well as the lack of longitudinal assessments in prior trials. The successful implementation of more rigorous methods to reduce risk of bias in randomized controlled trials is needed to test the effect of nonintegrated treatments on psychological symptoms and quality of life outcomes.
Public Health Significance Statement.
This review suggested that cognitive-behavioral techniques may impact psychological functioning and quality of life in addition to gambling behavior and harms. This review also highlighted the need to conduct more rigorous randomized controlled trials that incorporate assessments of psychological functioning and quality of life among individuals experiencing gambling harms.
Acknowledgments
This work was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health award numbers L30AA029551 and T32AA018108. This work was also supported by the Tennessee Department of Mental Health and Substance Abuse Services. The content is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the state of Tennessee.
Footnotes
All authors declare no conflicts of interest.
This study was preregistered on PROSPERO (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=288058).
CrediT Taxonomy:
Rory A. Pfund – conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, visualization, writing – original draft, writing – review and editing
Shelby A. King – data curation, investigation, writing – original draft, writing – review and editing
David P. Forman – data curation, investigation, writing – original draft, writing – review and editing
James M. Zech – data curation, writing – original draft, writing – review and editing
Meredith K. Ginley – conceptualization, supervision, writing – review and editing
Samuel C. Peter – conceptualization, writing – review and editing
Nicholas W. McAfee – conceptualization, writing – review and editing
Katie Witkiewitz – funding acquisition, resources, software, supervision, writing – review and editing
James P. Whelan – funding acquisition, resources, software, supervision, writing – review and editing
References
- Afifi TO, Nicholson R, Martins SS, & Sareen J (2016). A longitudinal study of the temporal relation between problem gambling and mental and substance use disorders among young adults. The Canadian Journal of Psychiatry, 61(2), 102–111. 10.1177/0706743715625950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed., p. 223). American Psychiatric Association. [Google Scholar]
- American Psychological Association. (2006). Evidence-based practice in psychology. American Psychologist, 61(4), 271–285. 10.1037/0003-066X.61.4.271 [DOI] [PubMed] [Google Scholar]
- Augner C, Vlasak T, Aichhorn W, & Barth A (2022). Psychological online interventions for problem gambling and gambling disorder—A meta-analytic approach. Journal of Psychiatric Research, 151, 86–94. [DOI] [PubMed] [Google Scholar]
- Bandura A (2001). Social cognitive theory: An agentic perspective. Annual Review of Psychology, 52, 1–26. [DOI] [PubMed] [Google Scholar]
- Bergeron P-Y, Giroux I, Chrétien M, & Bouchard S (2022). Exposure Therapy for Gambling Disorder: Systematic Review and Meta-Analysis. Current Addiction Reports, 9, 179–194. 10.1007/s40429-022-00428-5 [DOI] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (2009). Introduction to meta-analysis. John Wiley & Sons. [Google Scholar]
- Boudreault C, Giroux I, Jacques C, Goulet A, Simoneau H, & Ladouceur R (2018). Efficacy of a Self-Help Treatment for At-Risk and Pathological Gamblers. Journal of Gambling Studies, 34(2), 561–580. 10.1007/s10899-017-9717-z [DOI] [PubMed] [Google Scholar]
- Bücker L, Bierbrodt J, Hand I, Wittekind C, Moritz S, Bucker L, Bierbrodt J, Hand I, Wittekind C, & Moritz S (2018). Effects of a depression-focused internet intervention in slot machine gamblers: A randomized controlled trial. PloS One, 13, e0198859–e0198859. 10.1371/journal.pone.0198859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bücker L, Gehlenborg J, Moritz S, & Westermann S (2021). A randomized controlled trial on a self-guided Internet-based intervention for gambling problems. Scientific Reports, 11, 1–13. 10.1038/s41598-021-92242-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P, Jonsson J, Josephson H, & Forsberg L (2010). Motivational interviewing versus cognitive behavioral group therapy in the treatment of problem and pathological gambling: A randomized controlled trial. Cognitive Behaviour Therapy, 39(2), 92–103. 10.1080/16506070903190245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P, & Smit F (2008). Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. Journal of Consulting and Clinical Psychology, 76(6), 1090–1094. 10.1037/a0013603 [DOI] [PubMed] [Google Scholar]
- Casey LM, Oei TPS, Raylu N, Horrigan K, Day J, Ireland M, & Clough BA (2017). Internet-Based Delivery of Cognitive Behaviour Therapy Compared to Monitoring, Feedback and Support for Problem Gambling: A Randomised Controlled Trial. Journal of Gambling Studies, 33(3), 993–1010. 10.1007/s10899-016-9666-y [DOI] [PubMed] [Google Scholar]
- Cowlishaw S, Merkouris S, Dowling N, Anderson C, Jackson A, & Thomas S (2012). Psychological therapies for pathological and problem gambling. The Cochrane Database of Systematic Reviews, 11, CD008937–CD008937. 10.1002/14651858.CD008937.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Li J, Hofmann SG, & Andersson G (2010). Self-reported versus clinician-rated symptoms of depression as outcome measures in psychotherapy research on depression: A meta-analysis. Clinical Psychology Review, 30(6), 768–778. 10.1016/j.cpr.2010.06.001 [DOI] [PubMed] [Google Scholar]
- Dowling NA, Cowlishaw S, Jackson AC, Merkouris SS, Francis KL, & Christensen DR (2015). Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. The Australian and New Zealand Journal of Psychiatry, 49(6), 519–539. 10.1177/0004867415575774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling NA, Merkouris SS, & Lorains FK (2016). Interventions for comorbid problem gambling and psychiatric disorders: Advancing a developing field of research. Addictive Behaviors, 58, 21–30. 10.1016/j.addbeh.2016.02.012 [DOI] [PubMed] [Google Scholar]
- Dowling N, Smith D, & Thomas T (2007). A comparison of individual and group cognitive-behavioural treatment for female pathological gambling. Behaviour Research and Therapy, 45, 2192–2202. 10.1016/j.brat.2006.11.003 [DOI] [PubMed] [Google Scholar]
- Echeburúa E, Gómez M, Freixa M, Echeburua E, Gomez M, Freixa M, Echeburúa E, Gómez M, & Freixa M (2011). Cognitive-behavioural treatment of pathological gambling in individuals with chronic schizophrenia: A pilot study. Behaviour Research & Therapy, 49, 808–814. 10.1016/j.brat.2011.08.009 [DOI] [PubMed] [Google Scholar]
- Gooding P, & Tarrier N (2009). A systematic review and meta-analysis of cognitive-behavioural interventions to reduce problem gambling: Hedging our bets? Behaviour Research & Therapy, 47, 592–607. 10.1016/j.brat.2009.04.002 [DOI] [PubMed] [Google Scholar]
- Grant JE, Donahue CB, Odlaug BL, Kim SW, Miller MJ, & Petry NM (2009). Imaginal desensitisation plus motivational interviewing for pathological gambling: Randomised controlled trial. The British Journal of Psychiatry, 195, 266–267. 10.1192/bjp.bp.108.062414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JE, Odlaug BL, Chamberlain SR, Potenza MN, Schreiber LRN, Donahue CB, & Kim SW (2014). A randomized, placebo-controlled trial of N-acetylcysteine plus imaginal desensitization for nicotine-dependent pathological gamblers. The Journal of Clinical Psychiatry, 75(01), 39–45. 10.4088/JCP.13m08411 [DOI] [PubMed] [Google Scholar]
- Grant J, & Potenza MN (2006). Escitalopram treatment of pathological gambling with co-occurring anxiety: An open-label pilot study with double-blind discontinuation. International Clinical Psychopharmacology, 21(4), 203–209. [DOI] [PubMed] [Google Scholar]
- Hedges LV, & Olkin I (1985). Statistical methods for meta-analysis. Academic Press. [Google Scholar]
- Higgins JPT, & Green S (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analyses. BMJ, 327, 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander E, Pallanti S, Allen A, Sood E, & Rossi NB (2005). Does sustained-release lithium reduce impulsive gambling and affective instability versus placebo in pathological gamblers with bipolar spectrum disorders? Am J Psychiatry, 137–145. [DOI] [PubMed] [Google Scholar]
- IntHout J, Ioannidis JPA, Rovers MM, & Goeman JJ (2016). Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open, 6, e010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josephson H, Carlbring P, Forsberg L, & Rosendahl I (2016). People with gambling disorder and risky alcohol habits benefit more from motivational interviewing than from cognitive behavioral group therapy. PeerJ, 2016(3). 10.7717/peerj.1899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Hwang I, LaBrie R, Petukhova M, Sampson NA, Winters KC, & Shaffer HJ (2008). DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine, 38(9), 1351–1360. 10.1017/S0033291708002900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korman L, Collins J, Littman-Sharp N, Skinner W, McMain S, & Mercado V (2008). Randomized control trial of an integrated therapy for comorbid anger and gambling. Psychotherapy Research, 18, 454–465. 10.1080/10503300701858362 [DOI] [PubMed] [Google Scholar]
- Langham E, Thorne H, Browne M, Donaldson P, Rose J, & Rockloff M (2015). Understanding gambling related harm: A proposed definition, conceptual framework, and taxonomy of harms. BMC Public Health, 16(1), 80. 10.1186/s12889-016-2747-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorains FK, Cowlishaw S, & Thomas SA (2011). Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction, 106, 490–498. 10.1111/j.1360-0443.2010.03300.x [DOI] [PubMed] [Google Scholar]
- Oei TPS, Raylu N, & Casey LM (2010). Effectiveness of group and individual formats of a combined motivational interviewing and cognitive behavioral treatment program for problem gambling: A randomized controlled trial. Behavioural and Cognitive Psychotherapy, 38(2), 233–238. 10.1017/S1352465809990701 [DOI] [PubMed] [Google Scholar]
- Oei TPS, Raylu N, & Lai WW (2018). Effectiveness of a Self Help Cognitive Behavioural Treatment Program for Problem Gamblers: A Randomised Controlled Trial. Journal of Gambling Studies, 34(2), 581–595. 10.1007/s10899-017-9723-1 [DOI] [PubMed] [Google Scholar]
- Page MJ, & Higgins JPT (2016). Rethinking the assessment of risk of bias due to selective reporting: A cross-sectional study. Systematic Reviews, 5, 1–8. 10.1186/s13643-016-0289-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, … Moher D (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peter SC, Whelan JP, Ginley MK, Pfund RA, Wilson KK, & Meyers AW (2016). Disordered gamblers with and without ADHD: The role of coping in elevated psychological distress. International Gambling Studies, 16(3), 455–469. 10.1080/14459795.2016.1231211 [DOI] [Google Scholar]
- Petry NM, Ginley MK, & Rash CJ (2017). A systematic review of treatments for problem gambling. Psychology of Addictive Behaviors, 31, 951–961. 10.1037/adb0000290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NMN, Rash CCJ, & Alessi SM (2016). A randomized controlled trial of brief interventions for problem gambling in substance abuse treatment patients. Journal of Consulting and Clinical Psychology, 84, 874–886. 10.1037/ccp0000127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Stinson FS, & Grant BF (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 66(5), 564–574. 10.4088/jcp.v66n0504 [DOI] [PubMed] [Google Scholar]
- Pfund RA, Forman DP, King SA, Zech JM, Ginley MK, Peter SC, McAfee NW, & Whelan JP (2022). Efficacy of cognitive-behavioral techniques for problem gambling and gambling disorder: A systematic review and meta-analysis. Manuscript under review. [DOI] [PMC free article] [PubMed]
- Pfund RA, Peter SC, Whelan JP, Meyers AW, Ginley MK, & Relyea G (2020). Is more better? A meta-analysis of dose and efficacy in face-to-face psychological treatments for problem and disordered gambling. Psychology of Addictive Behaviors, 34(5), 557–568. 10.1037/adb0000560 [DOI] [PubMed] [Google Scholar]
- Pfund RA, Whelan JP, Greenburg JE, Peter SC, Wilson KK, & Meyers AW (2017). Psychological distress as an indicator of co-occurring psychopathology among treatment-seeking disordered gamblers. Journal of Gambling Studies, 33(3), 907–918. 10.1007/s10899-016-9645-3 [DOI] [PubMed] [Google Scholar]
- Pfund R, & Ginley MK (2019). Assessment and treatment of gambling behavior. Journal of Health Service Psychology, 45(3), 81–89. 10.1007/BF03544684 [DOI] [Google Scholar]
- Pickering D, Keen B, Entwistle G, & Blaszczynski A (2017). Measuring treatment outcomes in gambling disorders: A systematic review. Addiction, 113, 411–426. 10.1111/add.13968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering D, Spoelma MJ, Dawczyk A, Gainsbury SM, & Blaszczynski A (2020). What does it mean to recover from a gambling disorder? Perspectives of gambling help service users. Addiction Research and Theory, 28, 132–143. 10.1080/16066359.2019.1601178 [DOI] [Google Scholar]
- Pietrzak RH, & Petry NM (2005). Antisocial personality disorder is associated with increased severity of gambling, medical, drug and psychiatric problems among treatment-seeking pathological gamblers. Addiction, 100(8), 1183–1193. 10.1111/j.1360-0443.2005.01151.x [DOI] [PubMed] [Google Scholar]
- Rash CJ, Weinstock J, & Petry NM (2011). Drinking patterns of pathological gamblers before, during, and after gambling treatment. Psychology of Addictive Behaviors, 25(4), 664–674. 10.1037/a0025565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagoe D, Griffiths MD, Erevik EK, Høyland T, Leino T, Lande IA, Sigurdsson ME, & Pallesen S (2021). Internet-based treatment of gambling problems: A systematic review and meta-analysis of randomized controlled trials. Journal of Behavioral Addictions, 10, 546–565. 10.1556/2006.2021.00062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander W, & Peters A (2009). Pathological gambling: Influence of quality of life and psychological distress on abstinence after cognitive-behavioral inpatient treatment. Journal of Gambling Studies, 25(2), 253–262. 10.1007/s10899-009-9128-x [DOI] [PubMed] [Google Scholar]
- Schluter MG, Kim HS, Poole JC, Hodgins DC, McGrath DS, Dobson KS, & Taveres H (2019). Gambling-related cognitive distortions mediate the relationship between depression and disordered gambling severity. Addictive Behaviors, 90, 318–323. 10.1016/j.addbeh.2018.11.038 [DOI] [PubMed] [Google Scholar]
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, & Henry DA (2017). AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ, 358, 1–9. 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundqvist K, & Rosendahl I (2019). Problem gambling and psychiatric comorbidity—Risk and temporal sequencing among women and men: Results from the Swelogs Case–Control Study. Journal of Gambling Studies, 35(3), 757–771. 10.1007/s10899-019-09851-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toneatto T, Brands B, & Selby P (2009). A randomized, double-blind, placebo-controlled trial of naltrexone in the treatment of concurrent alcohol use disorder and pathological gambling. The American Journal on Addictions, 18(3), 219–225. 10.1080/10550490902787007 [DOI] [PubMed] [Google Scholar]
- Walker M, Toneatto T, Potenza MN, Petry N, Ladouceur R, Hodgins DC, El-Guebaly N, Echeburua E, & Blaszczynski A (2006). A framework for reporting outcomes in problem gambling treatment research: The Banff, Alberta Consensus. Addiction, 101, 504–511. 10.1111/j.1360-0443.2005.01341.x [DOI] [PubMed] [Google Scholar]
- Wardle H, Reith G, Langham E, & Rogers RD (2019). Gambling and public health: We need policy action to prevent harm. BMJ, l1807. 10.1136/bmj.l1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock J, April LM, & Kallmi S (2017). Is subclinical gambling really subclinical? Addictive Behaviors, 73, 185–191. 10.1016/j.addbeh.2017.05.014 [DOI] [PubMed] [Google Scholar]
- Wong DFK, Chung CLP, Wu J, Tang J, Lau P, & Wan JPC (2015). A Preliminary Study of an Integrated and Culturally Attuned Cognitive Behavioral Group Treatment for Chinese Problem Gamblers in Hong Kong. Journal of Gambling Studies, 31(3), 1015–1027. 10.1007/s10899-014-9457-2 [DOI] [PubMed] [Google Scholar]


