Abstract
Background
Antibiotics are the greatest risk factor for Clostridioides difficile infection (CDI). Risk for CDI varies across antibiotic types and classes. Optimal prescribing and stewardship recommendations require comparisons of risk across antibiotics. However, many prior studies rely on aggregated antibiotic categories or are underpowered to detect significant differences across antibiotic types. Using a large database of real-world data, we evaluate community-associated CDI risk across individual antibiotic types.
Methods
We conducted a matched case–control study using a large database of insurance claims capturing longitudinal health care encounters and medications. Case patients with community-associated CDI were matched to 5 control patients by age, sex, and enrollment period. Antibiotics prescribed within 30 days before the CDI diagnosis along with other risk factors, including comorbidities, health care exposures, and gastric acid suppression were considered. Conditional logistic regression and a Bayesian analysis were used to compare risk across individual antibiotics. A sensitivity analysis of antibiotic exposure windows between 30 and 180 days was conducted.
Results
We identified 159 404 cases and 797 020 controls. Antibiotics with the greatest risk for CDI included clindamycin and later-generation cephalosporins, and those with the lowest risk included minocycline and doxycycline. We were able to differentiate and order individual antibiotics in terms of their relative level of associated risk for CDI. Risk estimates varied considerably with different exposure windows considered.
Conclusions
We found wide variation in CDI risk within and between classes of antibiotics. These findings ordering the level of associated risk across antibiotics can help inform tradeoffs in antibiotic prescribing decisions and stewardship efforts.
Keywords: antibiotics, case–control study, CDI, Clostridioides difficile infection, outpatient, risk factors, stewardship
Antibiotic exposure is the primary risk factor for clostridioides difficile infection, but the level of risk varies across different antibiotics. This study estimates and compares the risk for community-associated clostridioides difficile infection across 27 different individual antibiotics.
Graphical Abstract
Graphical Abstract.
Clostridioides difficile infection (CDI) is a common cause of health care–associated infections, contributing to excess morbidity, mortality, and health care costs [1–3]. In addition to hospital settings, cases of community-associated CDI (CA-CDI) have also become more common [4–6]. Thus, while exposure to health care settings remains a major risk factor for CDI [7–9] for both health care– and community-associated CDI, multiple other risk factors have been described. These risk factors include advanced age [3], gastric acid suppression [10–13], frailty [14], low albumin [15, 16], multiple comorbidities [17], and, most importantly, prior antibiotic use [18–20]. In fact, before the identification of the causative agent for CDI, the disease was commonly called antibiotic-associated colitis [21, 22].
Almost all antibiotics have been associated with an increased risk of developing CDI [23]. However, some antibiotics impart more risk than others. In general, clindamycin, later-generation cephalosporins, and fluoroquinolones are considered high-risk antibiotics for developing CDI [24]. In contrast, tetracyclines are considered lower-risk antibiotics [25]. Given the public health importance of CDI, many antibiotic stewardship efforts have focused on reducing CDI rates by reducing inappropriate antibiotic prescribing [26]. Because some antibiotics confer more risk for CDI than others, preferentially prescribing lower-risk antibiotics has been proposed as an approach to reduce CDI rates [25, 27, 28].
Most studies comparing CDI risks for different antibiotics have been underpowered to differentiate levels of risk between individual antibiotics. Thus, several meta-analyses have pooled results from smaller studies [20, 29–31]. In general, confidence intervals around the risk estimates for different antibiotics tend to overlap, except for the lowest- and highest-risk antibiotics. These meta-analyses are further challenged by pooling different study populations and including different time periods for capturing antibiotic exposure. Estimating the risk attributable to different antibiotic exposures is especially challenging for patients with significant health care exposures, which often entail multiple overlapping risk factors for CDI. An alternative approach is to estimate CDI risk by focusing on CDI cases without recent hospitalizations or long-term-care exposures. The recent increase in CA-CDI may provide such an opportunity.
The objective of this study was to evaluate the risk for CA-CDI across different antibiotics to better inform antibiotic prescribing. We directly compared the associated risk levels between multiple types of antibiotics by conducting a case–control study of CA-CDI cases and controls without CDI using a large data set of commercial insurance claims across the United States. We also evaluated the impact of different lengths of time before CDI to capture antibiotic exposure.
METHODS
Data
We used the Merative MarketScan Research Databases including the Commercial, Medicare, and Multi-State Medicaid databases. The Commercial and Medicare databases covered the years 2001–2021, and the Medicaid database covered 2014–2018. These databases contain demographic and enrollment information, along with inpatient, outpatient, and emergency department visits and outpatient prescription drug claims. Across the study period, these databases represent >245 million distinct enrollees.
Study Population
We conducted a matched case–control study comparing prior exposures between CA-CDI cases and matched controls without CDI. We included both adult and pediatric patients. Case patients diagnosed with CA-CDI were identified using the following criteria: (1) CDI diagnosed (using International Classification of Diseases, Ninth/Tenth Revision, Clinical Modification [ICD-9-CM/ICD-10-CM] codes) in either an outpatient setting, as the principal diagnosis for a hospital admission, or during a hospitalization lasting ≤2 days, (2) no prior inpatient stay within 12 weeks before the CDI diagnosis, (3) continuous enrollment with medication coverage for ≥180 days before the index diagnosis, and (4) no prior CDI diagnoses. Each CDI case was then randomly matched to 5 enrollees without CDI of the same age, sex, insurance type, and covering the same enrollment period before diagnosis (ie, 180 days before the corresponding CDI diagnosis date). Each match was unique, and control patients were only matched to a single case. Controls were assigned the same index date associated with their matched cases’ index CDI diagnosis; this date was used as the index date to identify prior antibiotic exposure.
To account for possible lags in the diagnosis of CDI in outpatient settings relative to the actual infection date (eg, patient presented with diarrhea, was treated empirically, and received diagnosis only after lab results were returned), we sought to identify empiric treatment of CDI before the recorded diagnosis. We implemented the following adjustment to correct for potential lags in diagnosis. For patients who received treatment for CDI (ie, received a prescription for oral vancomycin, fidaxomicin, or metronidazole) within 30 days before the index CDI diagnosis, we shifted the index CDI date to either (1) the date of a health care visit for diarrhea, if it occurred within 30 days on or before the treatment date, or (2) the date on which the CDI treatment was received, if no diarrhea diagnosis was recorded.
Statistical Analysis
We used a conditional logistic regression model to estimate the likelihood of having CA-CDI as a function of individual types of antibiotic exposures and other patient risk factors. We created separate indicator variables for each of the antibiotic types considered, based on exposure within 30 days before index. Patients who received >1 type of antibiotic during this exposure period had separate indicators for each antibiotic received, regardless of whether the antibiotics were received concurrently or sequentially. We used the prescription fill date and number of days supplied to compute the time from index date to the most recent antibiotic exposure. For example, a patient who received a 7-day supply of an antibiotic filled 35 days before index would be included as having a time since last exposure of 28 days.
Our aim was to focus on those antibiotics for which CA-CDI risk could be estimated with a reasonable degree of precision. Thus, 27 individual antibiotic types were selected for which ≥50 case and control observations had exposure within 30 days before index. Supplementary Table 1 lists each of the individual antibiotics that were considered along with their class. Antibiotics with 20–50 case observations were included in our analytical model, but their effect sizes were not reported in our primary results. All remaining types of antibiotics with <20 case observations were not considered individually, but were instead aggregated into a single category, called “other antibiotics,” sharing a single indicator in the model representing other antibiotic exposure within 30 days. Finally, antibiotics that met these inclusion criteria but had been discontinued (eg, gatifloxacin), were primarily used for treatment of H. pylori (eg, amoxicillin/clarithromycin), or were primarily used in inpatient settings (eg, ceftriaxone) were included in the model but are not presented in the primary tables (Supplementary Table 2).
We also controlled for patient comorbidities using the Elixhuaser comorbidity indicators [32], computed using all health care visits that occurred within 180 days before the index date, and separate indicators were included for each of the comorbidities. Receipt of a proton-pump inhibitor (PPI) within 90 days before index was also included in the model. Finally, to account for differences in potential health care exposures before infection, the total number of health care visit dates in the prior 90 days was calculated and included in the model. Note, patient age, sex, date of diagnosis, and insurance type were all accounted for in the study design during the matching process, as each of these variables was identically matched between cases and controls.
A Bayesian analysis was implemented using an improper uniform prior on the regression coefficients. Given the large sample size and a lack of strong beliefs regarding the relationships between antibiotics, we utilized an improper uniform prior. We computed point estimates using the posterior mean and 95% credible intervals (CIs). We also directly compared antibiotics by computing the posterior probabilities that the odds ratio of exposure to one type of antibiotic was greater than the odds ratio of exposure to another type of antibiotic.
Sensitivity Analysis
The existing literature evaluating CDI risk has often used a range of exposure windows to capture prior antibiotic exposure. Studies have found that antibiotics within 30 [33], 45 [34], 60 [35], 90 [12, 13, 36], and 180 days [6, 37] may be associated with increased risk for CDI. To evaluate the effect that differing exposure windows may have on the estimates for CDI risk, we conducted a sensitivity analysis where alternative exposure windows of 60, 90, 120, 150, and 180 days before the index date were considered. We then repeated the analysis using each of these alternative exposure windows, hypothesizing that longer exposure windows would shift effect estimates toward the null value (ie, odds ratio of 1) as more patients with unassociated exposures would be labeled exposed.
RESULTS
We identified 159 404 cases of CA-CDI and 797 020 controls. Table 1 provides a description of our study population in terms of demographic characteristics. In general, the study population reflects a similar age distribution to surveillance reports of CA-CDI events [38, 39]. Compared with controls, CA-CDI case patients were more likely to have received a PPI (20.02% vs 8.93%), to have received any antibiotic within 30 days (49.42% vs 9.87%), to have more comorbidities (2.38 vs 0.91), and to have had more health care visits in the 90 days prior (9.81 vs 3.48).
Table 1.
Study Population Characteristics of CA-CDI Cases and Matched Controls
| Characteristic | CA-CDI Cases, No. (%) |
Controls, No. (%) |
|---|---|---|
| No. | 159 404 | 797 020 |
| Age group | ||
| <18 y | 12 460 (7.82) | 62 300 (7.82) |
| 18–26 y | 10 228 (6.42) | 51 140 (6.42) |
| 27–44 y | 26 739 (16.77) | 133 695 (16.77) |
| 45–64 y | 58 693 (36.82) | 293 465 (36.82) |
| >65 y | 51 284 (32.17) | 256 420 (32.17) |
| Female sex | 103 691 (65.05) | 518 455 (65.05) |
| Medicaid | 20 956 (13.15) | 104 780 (13.15) |
| PPI within prior 90 d | 31 909 (20.02) | 71 150 (8.93) |
| Any antibiotic within 30 d | 78 784 (49.42) | 78 629 (9.87) |
| Mean/median number of comorbidities | 2.38/2 | 0.91/0 |
| Mean/median number of visits before index | 9.81/6 | 3.48/1 |
Abbreviations: CA-CDI, community-associated Clostridioides difficile infection; PPI, proton-pump inhibitor.
Table 2 provides summary counts of each antibiotic evaluated along with the number of cases and controls who received the antibiotic and the univariate odds ratios for the odds of occurrence among cases relative to controls. The 5 most commonly prescribed antibiotics among cases were clindamycin, amoxicillin/clavulanate, ciprofloxacin, cephalexin, and cefdinir. Among control patients, the most common antibiotics were amoxicillin, azithromycin, amoxicillin/clavulanate, ciprofloxacin, and cephalexin. The top 5 antibiotics in terms of unadjusted odds ratios were clindamycin, cefixime, cefpodoxime, cefdinir, and cefuroxime. The only antibiotic with an unadjusted odds ratio <1 was minocycline.
Table 2.
Comparison of Counts of Antibiotic Exposure Within 30 Days Before Index Between CA-CDI Cases and Controls, Along With Unadjusted Odds Ratios for CDI and Adjusted Odds Ratios and 95% Credible Intervals From the Conditional Logistic Regression Model; Additional Covariates and Antibiotics With <50 Cases Among the Control Population Can be Found in Supplementary Table 2.
| Antibiotic Class | Antibiotic Name | Count Among CA-CDI Cases (n = 181 041) |
Count Among Controls (n = 905 205) |
Unadjusted Odds Ratio | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Lincosamides | Clindamycin | 11 054 | 2615 | 22.64 | 25.39 (24.11–26.72) |
| Cephalosporins | Cephalexina | 5494 | 6301 | 4.48 | 2.88 (2.74–3.02) |
| Cefdinirc | 5455 | 2379 | 11.84 | 11.02 (10.39–11.69) | |
| Cefuroximeb | 2460 | 1190 | 10.48 | 9.59 (8.79–10.45) | |
| Cefpodoximec | 324 | 114 | 14.24 | 9.17 (6.99–12.04) | |
| Cefadroxila | 253 | 308 | 4.11 | 2.84 (2.27–3.54) | |
| Cefprozilc | 244 | 289 | 4.23 | 2.97 (2.4–3.68) | |
| Cefiximec | 243 | 79 | 15.4 | 12.04 (8.84–16.38) | |
| Cefaclorb | 62 | 60 | 5.17 | 4.16 (2.66–6.52) | |
| Fluoroquinolones | Ciprofloxacin | 10 672 | 6853 | 8.27 | 6.83 (6.56–7.1) |
| Levofloxacin | 4246 | 4349 | 4.99 | 2.49 (2.35–2.64) | |
| Moxifloxacin | 969 | 661 | 7.37 | 4.71 (4.14–5.37) | |
| Penicillins | Amoxicillin/clavulanate | 12 738 | 7056 | 9.72 | 8.53 (8.23–8.85) |
| Amoxicillin | 6079 | 12 365 | 2.52 | 1.96 (1.88–2.04) | |
| Penicillin | 797 | 1412 | 2.83 | 1.8 (1.59–2.03) | |
| Ampicillin | 178 | 220 | 4.05 | 2.6 (2–3.39) | |
| Dicloxacillin | 148 | 106 | 6.99 | 5.91 (4.37–7.99) | |
| Sulfonamides | Sulfamethoxazole/trimethoprim | 5289 | 5881 | 4.62 | 2.16 (2.05–2.27) |
| Trimethoprim | 135 | 301 | 2.24 | 1.01 (0.76–1.36) | |
| Macrolides | Azithromycin | 4499 | 11 811 | 1.93 | 1.31 (1.26–1.37) |
| Clarithromycin | 692 | 1125 | 3.08 | 1.83 (1.62–2.07) | |
| Erythromycin | 218 | 357 | 3.06 | 1.53 (1.21–1.93) | |
| Tetracyclines | Doxycycline | 2005 | 6273 | 1.61 | 0.96 (0.89–1.02) |
| Minocycline | 283 | 1462 | 0.97 | 0.79 (0.67–0.93) | |
| Tetracycline | 114 | 348 | 1.64 | 1.21 (0.92–1.6) | |
| Other | Nitrofurantoin | 2798 | 4117 | 3.44 | 1.77 (1.65–1.89) |
| Linzolid | 167 | 52 | 16.07 | 3.58 (2.36–5.44) |
Abbreviation: CA-CDI, community-associated Clostridioides difficile infection.
First-generation cephalosporin.
Second-generation cephalosporin.
Third-generation cephalosporin.
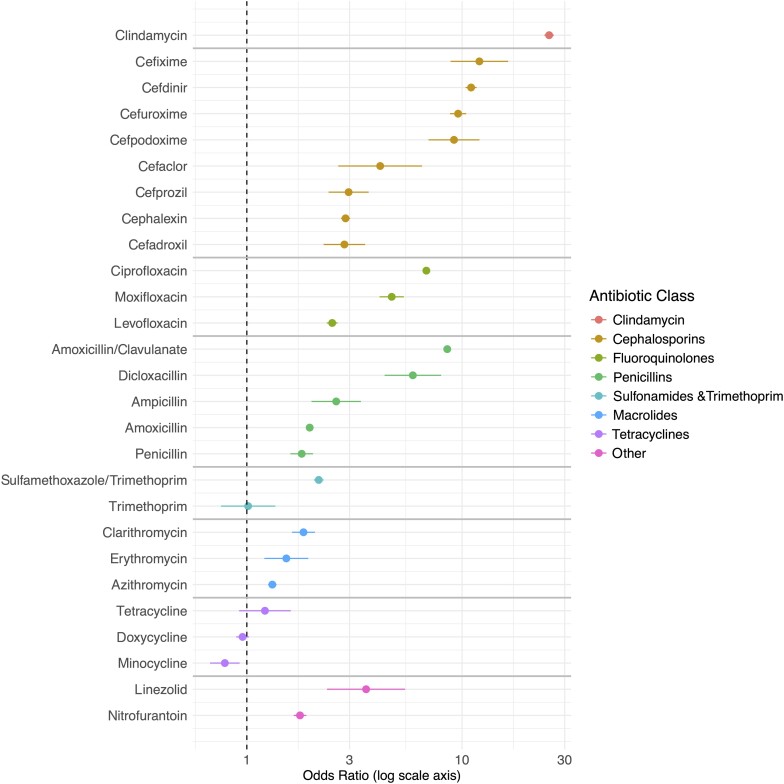
Adjusted odds ratios and 95% credible intervals for each antibiotic from the logistic regression model are also presented in Table 2 (estimates for the remaining risk factors and antibiotics with low counts are presented in Supplementary Table 2). Clindamycin (25.39; 95% CI, 24.11–26.72) was associated with the greatest level of risk for CDI. The later-generation cephalosporins of cefixime, cefdinir, cefuroxime, and cefpodoxime along with the penicillin amoxicillin/clavulanate had odds ratios ranging from 8.53 to 12.04. The fluoroquinolones of ciprofloxacin and moxifloxacin, dicloxacillin, and later-generation cephalosporin cefaclor had odds ratios ranging from 4.16 to 6.83. Linezolid, the later-generation cephalosporin cefprozil, first-generation cephalosporins cephalexin and cefadroxil, ampicillin, levofloxacin, and sulfamethoxazole/trimethoprim had odds ratios between 2.15 and 3.58. The remaining penicillins, macrolides, and nitrofurantoin had odds ratios between 1.31 and 1.96. Trimethoprim, doxycycline, and tetracycline had odds ratios that were not statistically significant, while minocycline had a significant protective effect (0.79; 95% CI, 0.67–0.93).
From Figure 1, which compares estimated odds ratios and 95% credible intervals, one can see that there is significant variation in risk both between antibiotic classes and within classes. On average, clindamycin and cephalosporins, particularly later-generation cephalosporins, provided the highest risk, while fluoroquinolones and penicillins provided moderate risk, macrolides and sulfonamides provided lower risk, and the tetracyclines provided almost no risk. However, within classes there remained considerable variation between antibiotic types. For example, amoxicillin/clavulanate had a risk level similar to that of later-generation cephalosporins at 8.53 (95% CI, 8.23–8.85), which was >4 times the associated risk level of amoxicillin without clavulanate (1.96; 95% CI, 1.88–2.04). Ciprofloxacin had a risk level closer to that of later-generation cephalosporins (6.83; 95% CI, 6.56–7.10), while levofloxacin had a risk level similar to first-generation cephalosporins (2.49; 95% CI, 2.35–2.64). Cefeximine (12.04; 95% CI, 8.84–16.38) had >4 times the risk level of cefadroxil (2.84; 95% CI, 2.27–3.54).
Figure 1.
Visual comparison of effect estimates across antibiotic types, grouped by antibiotic class. Point estimates are depicted by the circle and 95% credible intervals by the line segments. Exact values can be found in Table 2.
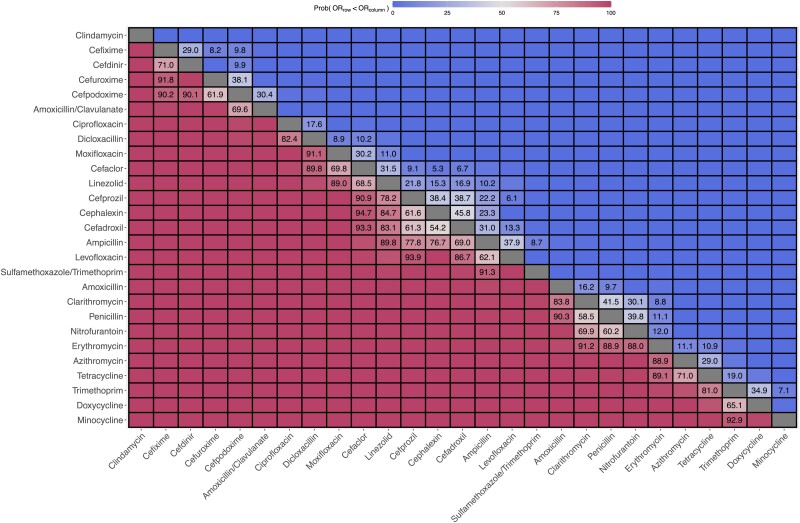
For each pair of antibiotics, Figure 2 provides a probabilistic comparison that one antibiotic is associated with a greater risk for CDI than another antibiotic. Specifically, Figure 2 shows the posterior probability that the increase in odds of CDI due to taking one antibiotic (represented along the rows) is less than the increase due to taking a different antibiotic (represented along the columns). Specific values are reported for all probability values between 5% and 95%. Across nearly all 27 antibiotics considered, we were able to probabilistically differentiate and order their level of associated risk at a 95% level. Clindamycin exhibits the highest level of risk, reflected by posterior probability values >95% that the odds ratio for clindamycin was greater than the odds ratio of any other antibiotic type considered. In contrast, the posterior probability that the odds ratio for minocycline is less than another antibiotic type is >95% across all antibiotic types other than trimethoprim.
Figure 2.
Posterior probabilities of the pairwise comparisons of odds ratios across antibiotic types. The values represent the posterior probability that the odds ratio of the antibiotic in the row is less than the odds ratio of the antibiotic in the column. For example, the posterior probability that the odds ratio for cefixime is less than that of cefdinir is roughly 29.0%, while the posterior probability that the odds ratio for cefdinir is less than that of cefixime is roughly 71.0%. Results are ordered by effect size based on the 30-day exposure window. Only exact probability values between 5% and 95% are reported; Supplementary Figure 1 provides complete values for all cells <5% and >95%.
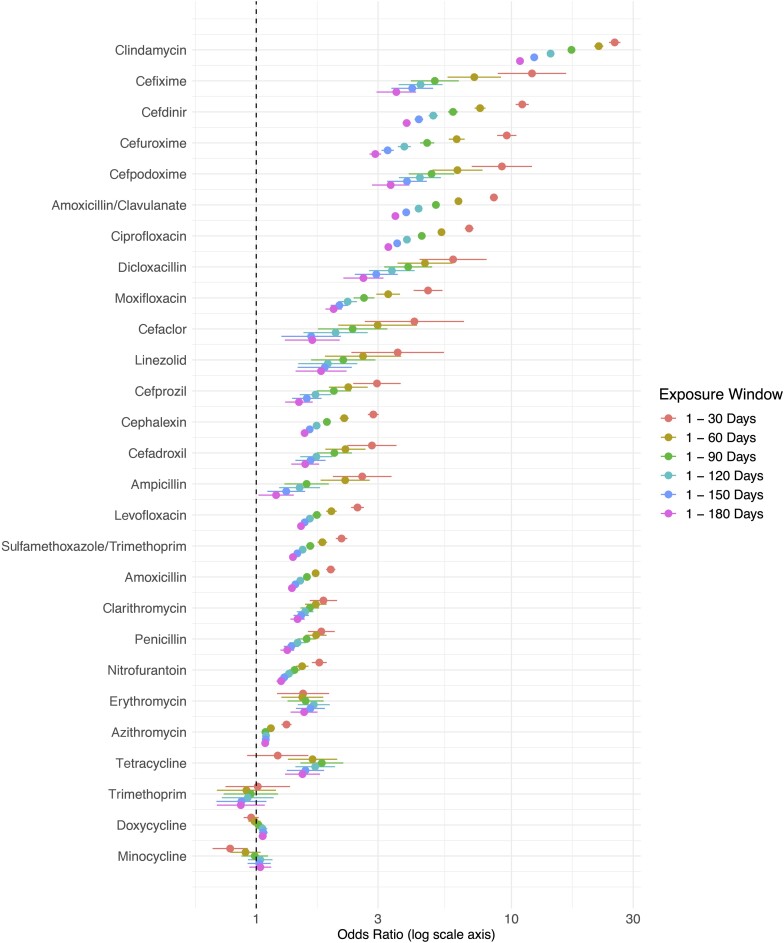
We conducted a sensitivity analysis using different windows to capture antibiotic exposures. Figure 3 provides a summary of the results from the sensitivity analysis where alternative exposure windows are considered. The results in Figure 3 are ordered based on the estimated risk level. Supplementary Table 3 provides the exact estimates and credible intervals for each of these models. Supplementary Figures 1–6 provide posterior pairwise comparisons of odds ratios across antibiotics using exposure windows from 30 to 180 days, respectively.
Figure 3.
Results of sensitivity analysis for effect estimates across antibiotic types using different exposure windows to capture prior antibiotic exposure. Exact values are reported in Supplementary Table 3. Results are ordered by effect size based on the 30-day exposure window. In general, effect estimates move toward the null value of 1 as the exposure window increases.
Two notable features emerge from the sensitivity analysis. First, the ordering of types of antibiotics in terms of risk is generally preserved—an antibiotic that exhibited a higher level of risk than another antibiotic using a 30-day window generally remained higher risk when using a 90-day window. Second, within antibiotic types there is a fairly dramatic decrease in the estimated effect for longer exposure windows. This shift occurs in a monotonic fashion, with larger exposure windows producing odds ratios closer to 1, across nearly all antibiotics. This shift is often so dramatic that the estimated effect for one antibiotic using a given window may trade places with another antibiotic using a different window. For example, cefdinir had a larger effect than amoxicillin/clavulanate at each time period; however, the risk for amoxicillin/clavulanate using a 30-day window (8.53; 95% CI, 8.23–8.85) was greater than cefdinir when using a 60-day window (7.53; 95% CI, 7.17–7.92). Thus, comparisons across antibiotics require consistent exposure windows.
DISCUSSION
In this study, we compared the risk for CA-CDI associated with 27 different antibiotics. Given our large study population, we were able to derive comparable risk estimates for each of these antibiotics while controlling for other antibiotic exposures and a range of additional risk factors. Although our case–control design does not provide exact relative risk estimates for the population, we provide comparable estimates of risk levels across antibiotic types and classes. We found considerable variation of risk across antibiotic classes and across individual antibiotics within classes. These findings have important implications for clinical prescribing decisions and illustrate some of the potential tradeoffs when choosing between different antibiotics in terms of CDI-related risk.
In general, our results are consistent with prior investigations. We found that clindamycin is deserving of its high-CDI-risk reputation. Also consistent with other reports, we found that tetracyclines are associated with the lowest levels of risk. However, most prior reports of CDI risk estimates lack power to produce nonoverlapping risk estimates [20, 29–31]. A recent study that evaluated risk across 18 different individual antibiotics among a large population of nursing home residents [36] produced many effect estimates with overlapping confidence intervals. In contrast, our study population was sufficiently large to produce effect estimates, credible intervals, and posterior probabilities, allowing for direct inference on the ordering of risk associated with the 27 antibiotics considered.
Similar to some prior studies, we demonstrated that the risk associated with first-generation cephalosporins is substantially lower than most later-generation cephalosporins. Prior meta-analyses have shown that point estimates between these classes were different, but we demonstrated a clear delineation in risk among individual first- and later-generation cephalosporins. In addition, we found that macrolides were associated with a relatively low risk level, almost comparable to that of tetracyclines. Interestingly, amoxicillin/clavulanate was similar in risk to later-generation cephalosporins and was associated with substantially more risk than amoxicillin without clavulanate. While much interest has been focused on the risks of CDI associated with fluroquinolones [40, 41], we found that the risks associated with fluroquinolones were in between the risks associated with first- and later-generation cephalosporins.
We also considered how risk estimates for different antibiotics may change depending on the period used to capture antibiotic exposure. Existing literature has been largely inconsistent when considering different exposure windows; 30- to 90-day windows are commonly used [12, 13, 33–36], but longer windows have also been considered [6, 37]. Our findings raise important questions about the comparability of results across different studies and settings. We found that for most antibiotics, the risk estimates varied by a large degree when different exposure windows were considered. Comparing the 30-day vs 90-day exposure window results in quite a dramatic shift for many antibiotics: Clindamycin went from an odds ratio of 25.39 (95% CI, 24.11–26.72) to 17.19 (95% CI, 16.58–17.81), cefixime went from 12.04 (95% CI, 8.84–16.38) to 5.01 (95% CI, 4.03–6.22), and amoxicillin/clavulanate went from 8.53 (95% CI, 8.23–8.85) to 5.06 (95% CI, 4.92–5.20). Comparing results between studies that rely on different exposure windows (eg, 30 vs 90 days) may lead to inconsistent findings and inaccurate assessments of the relative ranking of risk across antibiotics. This may be especially problematic for meta-analyses that incorporate studies with differing exposure windows and different sets or groupings of antibiotics.
Our study also has important considerations for future efforts to model the risk of CDI. First, our results suggest that crude class-based risk models may be too broad to capture distinctions between antibiotics in a given class. Indeed, we found that the variability within some classes in terms of associated risk level may exceed the variation between classes. Thus, attempts to define risk models in terms of simple high- vs low-risk classes may obscure important and meaningful differences within a class. Risk categories may need to ignore antibiotic classes and instead focus on individual types of antibiotics. Even when considering the distinction between first- vs later-generation cephalosporins, individual type must be considered as both cefprozil and cefaclor (both later-generation cephalosporins) had risk levels comparable to first-generation cephalosporins. Second, our findings highlight the importance of understanding the exposure window both when modeling risk and considering potential tradeoffs. Future work is needed to further assess the time-since exposure and the associated level of risk for CDI; some antibiotics may be associated with increased risk for differing periods of time. Similarly, the risk for different antibiotics associated with CDI recurrence is an important topic that needs further exploration.
Our study also suggests extensions for future work. First, a number of antibiotics were accounted for in our model but were not reported in our primary results due to a low number of exposures (Supplementary Table 2). One notable antibiotic worthy of future consideration is the later-generation cephalosporin cefditoren. Preliminary results (Supplementary Table 2) suggest that cefditoren may have a risk level similar to that of clindamycin (39.29; 95% CI, 16.58–93.07). However, this estimate may be imprecise due to the limited number of cases. Second, our study utilized a relatively simple modeling approach (eg, assumed additive effects across antibiotics) in order to evaluate risk across the widest range of antibiotics while considering different exposure windows. However, more complex modeling approaches may also be considered. For example, the duration of antibiotic exposure and time since last exposure, along with multiplicative interactions or comparisons of combination vs sequential antibiotic exposures when patients received multiple antibiotics, may also be modeled. Finally, individual risk levels may vary for different types of antibiotics across different subpopulations. We found only minor changes when the analysis was restricted to adult patients (Supplementary Figure 7), although the effect for 2 antibiotics increased when restricting the analysis to adults. Future studies may need to be conducted in specific age groups or other important subpopulations for CDI.
Our study has a number of limitations. First, we relied on administrative claims data to identify health care visits and diagnoses of CDI. We did not have lab data or clinic notes to conclusively identify CDI or the timing of symptom onset. We also could not identify stewardship practices at individual institutions that may have changed over the study period. Second, we relied on outpatient claims submitted for reimbursement to identify antibiotic exposure. Enrollees may have had differences in medication coverage, and the comprehensiveness of coverage may also have caused some enrollees to pay out-of-pocket for medications. Thus, the number of individuals exposed to antibiotics may be underidentified. However, this limitation likely biases effect estimates toward the null value, as some exposed patients will be labeled unexposed. Finally, we did not have access to antibiotics associated with inpatient stays. For this reason, we focused on CA-CDI cases and excluded analysis of any patients who were hospitalized within 12 weeks before index. Consequently, we were not able to analyze the full spectrum of antibiotic risk, in particular, the types of antibiotics more likely to be used in inpatient rather than outpatient settings. In addition, our results may be less generalizable to populations with frequent exposure to long-term care or hospital settings. Given that patients over age 65 represent a disproportionate number of CDI cases, future work should be conducted to capture the antibiotic exposures represented in long-term care settings.
Despite our limitations, we were able to define precise and comparable levels of relative risk for a wide range of antibiotics used in outpatient settings. These findings not only help inform strategies to reduce risk for CDI based on prescribing, but also help inform CDI risk modeling in general. Future risk estimates will need to carefully control for exposure windows (ie, the risk since starting an antibiotic) when making comparisons across antibiotics. Future work should also examine the risk for CDI recurrence.
Supplementary Material
Acknowledgments
Author contributions. Miller, Segre, and Polgreen conceived the research question and study design; Miller and Arakkal curated the data and developed the study cohorts; Miller, Arakkal, Sewell, and Tholany performed the analysis; all authors contributed to and revised the final manuscript.
Data availability. The data used for this study were from the Merative MarketScan Research Databases. These data used for this study are from a proprietary administrative health care claims database maintained by Merative and can be obtained by researchers through an agreement with Merative.
Patient consent. This study did not include factors requiring patient consent. The University of Iowa Human Subjects Office considers the MarkertScan database to be exempt from human subjects research review due to the deidentified nature of these retrospective administrative data.
Financial support. Support for this work was provided by a cooperative agreement from the Centers for Disease Control and Prevention (CDC)—award number U01 CK000594 (A.M., A.A., D.S., A.S., and P.P. received support from this grant).
Contributor Information
Aaron C Miller, University of Iowa, Carver College of Medicine, Iowa City, Iowa, USA.
Alan T Arakkal, University of Iowa, College of Public Health, Iowa City, Iowa, USA.
Daniel K Sewell, University of Iowa, College of Public Health, Iowa City, Iowa, USA.
Alberto M Segre, Department of Computer Science, University of Iowa, Iowa City, Iowa, USA.
Joseph Tholany, University of Iowa, Carver College of Medicine, Iowa City, Iowa, USA.
Philip M Polgreen, University of Iowa, Carver College of Medicine, Iowa City, Iowa, USA.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
References
- 1. Desai K, Gupta SB, Dubberke ER, Prabhu VS, Browne C, Mast TC. Epidemiological and economic burden of Clostridium difficile in the United States: estimates from a modeling approach. BMC Infect Dis 2016; 16:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kwon JH, Olsen MA, Dubberke ER. The morbidity, mortality, and costs associated with Clostridium difficile infection. Infect Dis Clin North Am 2015; 29:123–34. [DOI] [PubMed] [Google Scholar]
- 3. Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med 2015; 372:825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guh AY, Kutty PK. Clostridioides difficile infection. Ann Intern Med 2018; 169:ITC49–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Evans CT, Safdar N. Current trends in the epidemiology and outcomes of Clostridium difficile infection. Clin Infect Dis 2015; 60(Suppl 2):S66–71. [DOI] [PubMed] [Google Scholar]
- 6. Kuntz JL, Chrischilles EA, Pendergast JF, Herwaldt LA, Polgreen PM. Incidence of and risk factors for community-associated Clostridium difficile infection: a nested case-control study. BMC Infect Dis 2011; 11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Durovic A, Widmer AF, Tschudin-Sutter S. New insights into transmission of Clostridium difficile infection-narrative review. Clin Microbiol Infect 2018; 24:483–92. [DOI] [PubMed] [Google Scholar]
- 8. Gerding DN, Johnson S, Peterson LR, Mulligan ME, Silva J Jr. Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol 1995; 16:459–77. [DOI] [PubMed] [Google Scholar]
- 9. Kim KH, Fekety R, Batts DH, et al. Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic-associated colitis. J Infect Dis 1981; 143:42–50. [DOI] [PubMed] [Google Scholar]
- 10. Inghammar M, Svanström H, Voldstedlund M, et al. Proton-pump inhibitor use and the risk of community-associated Clostridium difficile infection. Clin Infect Dis 2021; 72:e1084–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jimenez J, Drees M, Loveridge-Lenza B, Eppes S, delRosario F. Exposure to gastric acid-suppression therapy is associated with health care- and community-associated Clostridium difficile infection in children. J Pediatr Gastroenterol Nutr 2015; 61:208–11. [DOI] [PubMed] [Google Scholar]
- 12. Dial S, Delaney JA, Schneider V, Suissa S. Proton pump inhibitor use and risk of community-acquired Clostridium difficile-associated disease defined by prescription for oral vancomycin therapy. CMAJ 2006; 175:745–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dial S, Delaney JA, Barkun AN, Suissa S. Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease. JAMA 2005; 294:2989–95. [DOI] [PubMed] [Google Scholar]
- 14. Rao K, Micic D, Chenoweth E, et al. Poor functional status as a risk factor for severe Clostridium difficile infection in hospitalized older adults. J Am Geriatr Soc 2013; 61:1738–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tabak YP, Johannes RS, Sun X, Nunez CM, McDonald LC. Predicting the risk for hospital-onset Clostridium difficile infection (HO-CDI) at the time of inpatient admission: HO-CDI risk score. Infect Control Hosp Epidemiol 2015; 36:695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shah K, Curtin BF, Chu C, Hwang D, Flasar MH, von Rosenvinge E. Characteristics of Clostridium difficile infection in patients hospitalized with myelodysplastic syndrome or acute myelogenous leukemia. World J Clin Oncol 2017; 8:398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harris AD, Sbarra AN, Leekha S, et al. Electronically available comorbid conditions for risk prediction of healthcare-associated Clostridium difficile infection. Infect Control Hosp Epidemiol 2018; 39:297–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guh AY, Adkins SH, Li Q, et al. Risk factors for community-associated Clostridium difficile infection in adults: a case-control study. Open Forum Infect Dis 2017; 4:XXX–XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Furuya-Kanamori L, Stone JC, Clark J, et al. Comorbidities, exposure to medications, and the risk of community-acquired Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2015; 36:132–41. [DOI] [PubMed] [Google Scholar]
- 20. Deshpande A, Pasupuleti V, Thota P, et al. Community-associated Clostridium difficile infection and antibiotics: a meta-analysis. J Antimicrob Chemother 2013; 68:1951–61. [DOI] [PubMed] [Google Scholar]
- 21. Bartlett JG. Antibiotic-associated pseudomembranous colitis. Rev Infect Dis 1979; 1:530–9. [DOI] [PubMed] [Google Scholar]
- 22. Fekety R, Silva J, Toshniwal R, et al. Antibiotic-associated colitis: effects of antibiotics on Clostridium difficile and the disease in hamsters. Rev Infect Dis 1979; 1:386–97. [DOI] [PubMed] [Google Scholar]
- 23. Kelly CP, Pothoulakis C, LaMont JT. Clostridium difficile colitis. N Engl J Med 1994; 330:257–62. [DOI] [PubMed] [Google Scholar]
- 24. Owens RC Jr, Donskey CJ, Gaynes RP, Loo VG, Muto CA. Antimicrobial-associated risk factors for Clostridium difficile infection. Clin Infect Dis 2008; 46(Suppl 1):S19–31. [DOI] [PubMed] [Google Scholar]
- 25. Tariq R, Cho J, Kapoor S, et al. Low risk of primary Clostridium difficile infection with tetracyclines: a systematic review and metaanalysis. Clin Infect Dis 2018; 66:514–22. [DOI] [PubMed] [Google Scholar]
- 26. Gerding DN, Muto CA, Owens RC Jr. Measures to control and prevent Clostridium difficile infection. Clin Infect Dis 2008; 46(Suppl 1):S43–49. [DOI] [PubMed] [Google Scholar]
- 27. Ritchie ND, Irvine SC, Helps A, Robb F, Jones BL, Seaton RA. Restrictive antibiotic stewardship associated with reduced hospital mortality in gram-negative infection. QJM 2017; 110:155–61. [DOI] [PubMed] [Google Scholar]
- 28. Lawes T, Lopez-Lozano JM, Nebot CA, et al. Effect of a national 4C antibiotic stewardship intervention on the clinical and molecular epidemiology of Clostridium difficile infections in a region of Scotland: a non-linear time-series analysis. Lancet Infect Dis 2017; 17:194–206. [DOI] [PubMed] [Google Scholar]
- 29. Brown KA, Khanafer N, Daneman N, Fisman DN. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother 2013; 57:2326–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Slimings C, Riley TV. Antibiotics and hospital-acquired Clostridium difficile infection: update of systematic review and meta-analysis. J Antimicrob Chemother 2014; 69:881–91. [DOI] [PubMed] [Google Scholar]
- 31. Slimings C, Riley TV. Antibiotics and healthcare facility-associated Clostridioides difficile infection: systematic review and meta-analysis 2020 update. J Antimicrob Chemother 2021; 76:1676–88. [DOI] [PubMed] [Google Scholar]
- 32. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998; 36:8–27. [DOI] [PubMed] [Google Scholar]
- 33. Brown KA, Fisman DN, Moineddin R, Daneman N. The magnitude and duration of Clostridium difficile infection risk associated with antibiotic therapy: a hospital cohort study. PLoS One 2014; 9:e105454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dial S, Kezouh A, Dascal A, Barkun A, Suissa S. Patterns of antibiotic use and risk of hospital admission because of Clostridium difficile infection. CMAJ 2008; 179:767–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Webb BJ, Subramanian A, Lopansri B, et al. Antibiotic exposure and risk for hospital-associated Clostridioides difficile infection. Antimicrob Agents Chemother 2020; 64:e02169–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Brown KA, Langford B, Schwartz KL, Diong C, Garber G, Daneman N. Antibiotic prescribing choices and their comparative C. difficile infection risks: a longitudinal case-cohort study. Clin Infect Dis 2021; 72:836–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Miller AC, Sewell DK, Segre AM, Pemmaraju SV, Polgreen PM. Risk for Clostridioides difficile infection among hospitalized patients associated with multiple healthcare exposures prior to admission. J Infect Dis 2021; 224:684–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Centers for Disease Control and Prevention . Emerging infections program healthcare-associated infections—community interface report: Clostridioides difficile infection. 2019. Available at: https://www.cdc.gov/hai/eip/Annual-CDI-Report-2019.html. Accessed February 28, 2023.
- 39. Centers for Disease Control and Prevention . Emerging infections program healthcare-associated infections—community interface report Clostridioides difficile infection. 2018. Available at: https://www.cdc.gov/hai/eip/Annual-CDI-Report-2018.html. Accessed February 28, 2023.
- 40. Tischendorf J, Brunner M, Knobloch MJ, et al. Evaluation of a successful fluoroquinolone restriction intervention among high-risk patients: a mixed-methods study. PLoS One 2020; 15:e0237987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Claeys KC, Hopkins TL, Vega AD, Heil EL. Fluoroquinolone restriction as an effective antimicrobial stewardship intervention. Curr Infect Dis Rep 2018; 20:7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.