1. Introduction
Older adults comprise a significant portion of thoracic patients, with 34.9% of new lung cancer cases among adults aged 65–74 years and 36.2% among those 75 years and older [1]. Older adults are at higher risk of frailty than their younger counterparts. Frailty has been associated with poor surgical outcomes such as complications, readmissions, and discharge to a higher level of care [2,3].
Gait speed is a brief, feasible measure that can identify frail patients with high sensitivity [4–7]. Slower gait speeds have been shown to be predictive of hospitalizations and worse survival in both the community and among people with cancer [8,9]. Gait speed has been well-studied in research settings, but there are less data regarding the implementation of gait speed in clinical settings—especially thoracic surgery clinics [10–14]. This study aimed to investigate the feasibility and acceptability of medical assistants (MAs) measuring four-meter gait speed (4MGS) as part of their routine vital sign assessment.
2. Material and Methods
2.1. Study Design and Population
The study was approved by the Institutional Review Board and informed consent was waived. We examined all new patients presenting to a single thoracic surgeon’s clinic from January–July 2021. This surgeon’s clinic also participated in a geriatric-thoracic surgery collaboration, in which patients aged 70 or above presenting with a lung nodule or patients aged 65 and above presenting with esophageal cancer or mesothelioma were also evaluated by a board-certified geriatrician. The MAs were trained in 4MGS measurement and were instructed to record 4MGS on all new patients. Details of 4MGS measurement are in Supplemental 1. Additionally, the geriatrician emailed the MAs the day before the clinic reminding them to measure 4MGS in the patients he would be evaluating.
2.2. Data Collection and Analysis
Patient demographics, comorbidities, and 4MGS measurements were obtained through a divisional database. To investigate the burden and acceptability of 4MGS measurement, we administered a brief survey six months after the study to all MAs (Supplemental 2). The survey consisted of six questions regarding how easy it was to learn, measure, and record 4MGS scored on a Likert scale (graded from 1 [not easy] to 5 [very easy]). Additionally, there were four open-ended questions where the MAs could list any feedback.
To quantify feasibility, we measured the proportion of patients with 4MGS measured out of the number of eligible patients. We additionally compared clinical characteristics between those who had a 4MGS measurement and those who did not. Differences in continuous variables were analyzed using Wilcoxon Rank Sum tests and differences between categorical variables were analyzed using Fisher’s exact (when smallest samples size <10) or Chi-square tests; p < 0.05 was considered a statistically significant difference. All analyses were conducted using StataSE 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC.).
3. Results
One hundred nine patients were eligible for 4MGS measurement in the thoracic surgeon’s clinic during the seven month study period. The cohort had a median age of 67 years (interquartile range [IQR] 59–74; Table 1). Twenty-one patients (19.3%) seen by the surgeon were also assessed by the geriatrician. Sixty-nine patients (63.3%) had 4MGS recorded. The median 4MGS was 0.94 m/s (IQR 0.80–1.11 m/s). Female patients (60.9% vs. 30.1% male, p = 0.01) and patients seen by the geriatrician (85.7% vs. 58.0% not seen by the geriatrician, p = 0.02) were more likely to have completed 4MGS (Supplemental 3). The remainder of the demographic and clinical characteristics were similar between the patients who completed 4MGS and those who did not.
Table 1.
Characteristics of cohort stratified by gait speed.
| Total | With Gait Speed | Without Gait Speed | |
|---|---|---|---|
| 109 | 69 (63.3%) | 40 (36.7%) | |
| Age, median (IQR) | 67 (59–74) | 69 (60–74) | 66 (50–71) |
| Sex, n (%) | |||
| Female | 56 (51.4%) | 42 (60.9%) | 14 (35.0%) |
| Male | 53 (48.6%) | 27 (39.1%) | 26 (65.0%) |
| Body Mass Index, median (IQR) | 26.50 (23.3–30.6) | 26.26 (22.3–30.6) | 26.73 (24.1–30.3) |
| Charlson Comorbidity Index, median (IQR) | 4 (2–7) | 4 (3–6) | 4 (2–7.5) |
| Race, n (%) | |||
| American Indian/Alaska Native | 1 (0.9%) | 0 (0%) | 1 (2.5%) |
| Asian | 2 (1.8%) | 1 (1.4%) | 1 (2.5%) |
| African American | 6 (5.5%) | 4 (5.8%) | 2 (5.0%) |
| White | 94 (86.2%) | 61 (88.4%) | 33 (82.5%) |
| Other | 2 (1.8%) | 1 (1.4%) | 1 (2.5%) |
| Declined | 4 (3.7%) | 2 (2.9%) | 2 (5.0%) |
| Ethnicity, n (%) | |||
| Hispanic | 2 (1.8%) | 0 (0%) | 2 (5.0%) |
| Non-Hispanic | 101 (92.7%) | 66 (95.7%) | 35 (87.5%) |
| Unavailable | 6 (5.5%) | 3 (4.3%) | 3 (7.5%) |
| Evaluated by Geriatrician, n (%) | 21 (19.3%) | 18 (26.1%) | 3 (7.5%) |
IQR = interquartile range.
There was a 100% response rate on the survey. Overall, 4MGS seemed easy to learn (7/7 or 100% responding with a 4 or 5), to administer (6/7 or 85.7% responding with a 4 or 5), and was well-accepted by the patients (7/7 or 100% responding with a 4 or 5) (Fig. 1). Fewer MAs reported that it was easy to remember to administer (2/7 or 28.6% responding with a 4 or 5). Common responses to what would help MAs remember included, providing reminders within the patient’s medical record and including the test on the vital sheet.
Fig. 1.
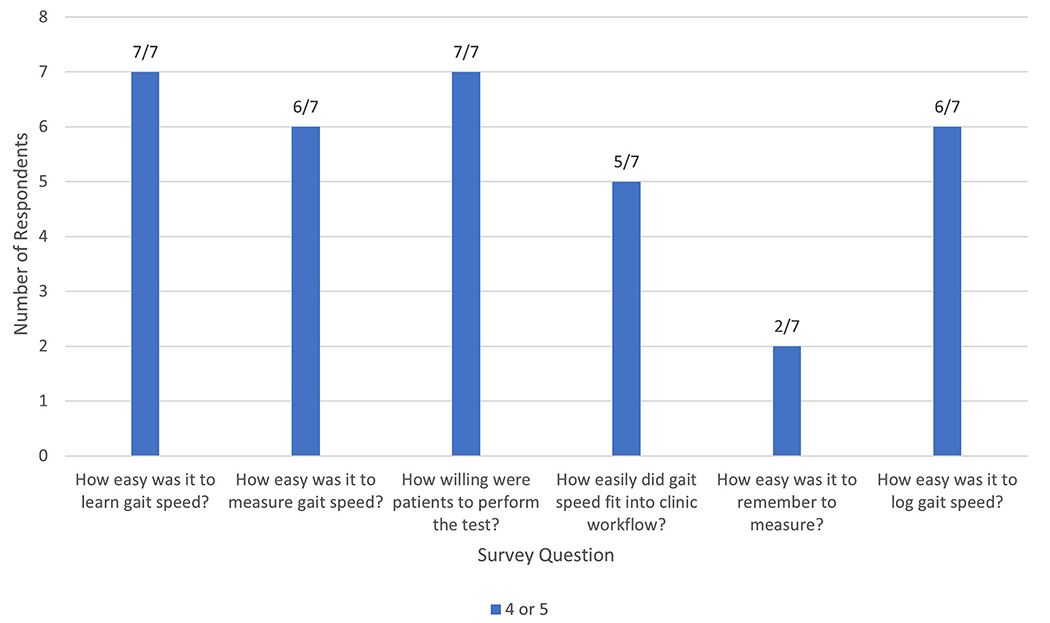
Survey of clinical staff to measure the burden and acceptability of 4MGS measurement.
Responses ranged from 1 (not easy/willing) to 5 (very easy/willing).
4. Discussion
Our study demonstrates the integration of 4MGS as a functional vital sign in a thoracic surgery clinic. It was moderately feasible for the MAs to measure, and the main barrier was remembering to complete the test.
Few studies have investigated the implementation of gait speed in a thoracic surgery setting. A number of cardiac surgery centers started measuring gait speed in 2011 for incorporation in the Society of Thoracic Surgeons Adult Cardiac Surgery Database, but details regarding methods of implementation are limited [15]. Bohannon et al. investigated the feasibility of gait speed measurement in a home care setting and found that their providers measured and documented gait speed in all patients [6]. Tucker et al. examined the feasibility of emergency room (ER) nurses measuring gait speed in older adults, with 60% of eligible patients completing the test [13]. The factors that explain these differences in implementation need to be explored, including varying resources and motivations across settings for measurement of physical function.
Our MAs reported that 4MGS was acceptable to patients and easy to learn, measure, and record. Our findings suggest that one critical support for implementing 4MGS entails a reminder system that alerts staff when and for whom to administer the test. This is supported by our observation that patients seen by the geriatrician had a higher completion rate than patients not seen by the geriatrician. The higher rate was likely due to the reminder emails sent by the geriatrician to MAs the day before the patients’ visits.
Utilizing factors known to improve implementation as well as staff feedback [14], we were able to make changes after the study period aimed at increasing rates of 4MGS measurement. To improve the ease of recording, we included a place to record 4MGS on the sheet where the MAs record their vitals. Additionally, we began including reminders for 4MGS on the clinic whiteboard to which MAs refer when rooming patients. We also worked closely with the MA director to make 4MGS measurement part of routine training.
Our study has limitations. For instance, we measured 4MGS once rather than taking the average of multiple trials. While this does increase the accuracy of the measurement, this must be balanced with the additional burden of repeated measurements. Moreover, we were unable to track the reasons why 4MGS was not measured in each patient. Although subject to recall bias, the survey administered to MAs provided important general responses regarding the acceptability and challenges in measuring 4MGS.
Our experience with 4MGS shows successes and challenges in its implementation as a vital sign measured by MAs in a thoracic surgery clinic, and we will continue to evaluate uptake and sustainability.
Supplementary Material
Acknowledgements
We would like to thank the thoracic surgery clinic staff at Brigham and Women’s Hospital for their hard work on this study and all other studies in the division.
CD was supported by the Harvard Translational Research in Aging Training Program (NIA T32AG023480); Brigham Research Institute (CD); The Boston Claude D. Pepper Older Americans Independence Center (National Institute on Aging of the National Institute of Health: P30 AG031679) (CD). AD was supported through the Jack Mitchell Thoracic Oncology Research Fellowship.
Footnotes
Declaration of Competing Interest
None.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jgo.2023.101481.
References
- [1].SEER Cancer Stat Facts. Lung and bronchus cancer. Bethesda, MD: National Cancer Institute; 2023. https://seer.cancer.gov/statfacts/html/lungb.html. [Google Scholar]
- [2].Lin HS, Watts JN, Peel NM, Hubbard RE. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr 2016;16(1):157. 10.1186/sl2877-016-0329-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tepas JJ. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg 2013;206(5):818. 10.1016/j-amjsurg.2013.07.029. [DOI] [PubMed] [Google Scholar]
- [4].Peel NM, Kuys SS, Klein K. Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci 2013;68(1):39–46. 10.1093/gerona/glsl74. [DOI] [PubMed] [Google Scholar]
- [5].Barthuly AM, Bohannon RW, Gorack W. Gait speed is a responsive measure of physical performance for patients undergoing short-term rehabilitation. Gait Posture 2012;36(1):61–4. 10.1016/j-gaitpost.2012.01.002. [DOI] [PubMed] [Google Scholar]
- [6].Bohannon RW. Measurement of gait speed of older adults is feasible and informative in a home-care setting. J Geriatr Phys Ther 2009;32(1):22–3. 10.1519/00139143-200932010-00005. [DOI] [PubMed] [Google Scholar]
- [7].Clegg A, Rogers L, Young J. Diagnostic test accuracy of simple instruments for identifying frailty in community-dwelling older people: a systematic review. Age Ageing 2015;44(1):148–52. 10.1093/ageing/aful57. [DOI] [PubMed] [Google Scholar]
- [8].Cesari M, Kritchevsky SB, Penninx BWHJ, et al. Prognostic value of usual gait speed in well-functioning older people - results from the Health, Aging and Body Composition Study. J Am Geriatr Soc 2005;53(10):1675–80. 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- [9].Liu MA, DuMontier C, Murillo A, et al. Gait speed, grip strength, and clinical outcomes in older patients with hematologic malignancies. Blood. 2019;134(4):374–82. 10.1182/blood.2019000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Katlic MR, Coleman J, Khan K, Wozniak SE, Abraham JH. Sinai abbreviated geriatric evaluation: development and validation of a practical test. Ann Surg 2019;269(1):177–83. 10.1097/SLA.0000000000002597. [DOI] [PubMed] [Google Scholar]
- [11].Bohannon RW, Wang YC. Four-meter gait speed: normative values and reliability determined for adults participating in the NIH toolbox study. Arch Phys Med Rehabil 2019;100(3):509–13. 10.1016/j.apmr.2018.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Karpman C, Lebrasseur NK, Depew ZS, Novotny PJ, Benzo RP. Measuring gait speed in the out-patient clinic: methodology and feasibility. Respir Care 2014;59 (4):531–7. 10.4187/respcare.02688. [DOI] [PubMed] [Google Scholar]
- [13].Tucker PW, Evans DD, Clevenger CK, Ardisson M, Hwang U. Feasibility of nurses measuring gait speed in older community-dwelling emergency department patients. Geriatr Nurs N Y N 2016;37(6):453–7. 10.1016/j.gerinurse.2016.06.015. [DOI] [PubMed] [Google Scholar]
- [14].Orkaby AR, James K, Leuchtenburg J, Solooki E, Gaziano JM, Driver JA. Taking prevention to the next step: implementation of a brief, sustainable frailty assessment in a cardiology clinic. BMJ Open Qual 2021;10(1):e001140. 10.1136/bmjoq-2020-001140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Afilalo J, Kim S, O’Brien S, et al. Gait speed and operative mortality in older adults following cardiac surgery. JAMA Cardiol 2016;1(3):314–21. 10.1001/jamacardio.2016.0316. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


