Abstract
Background:
Shifting to online learning during the coronavirus pandemic has increased the number of individuals symptomatic of digital eye strain (DES). This study aimed to determine the frequency and potential risk factors of DES among university staff members and students in this pandemic era.
Methods:
A cross-sectional online survey was conducted during the pandemic, in May and June 2020. The online questionnaire was designed to collect data on DES-related ocular and extraocular manifestations. The survey was sent via social media to the previous year’s students and staff within the Faculty of Medicine, Tanta University, Tanta, Egypt. The responses were downloaded and analyzed.
Results:
Of the 412 participants completing the questionnaire, 34 (8.3%) were university staff members with a mean (standard deviation [SD]) age of 36.7 (6.6) years, and 378 (91.7%) were university students with a mean (SD) age of 20.8 (1.8) years. Participants with DES symptoms numbered 294 (71.4%) before the lockdown, increasing to 366 (88.8%) during the last month, with 84 developing new-onset DES. Most participants reported ocular symptoms associated with DES. After the lockdown, both students and staff had a significant prolongation of nighttime digital screen use and TV watching, an increase in the 4-item Patient Health Questionnaire (PHQ-4) severity scale scores, and anxiety and depression, with a reduced duration of daytime reading (all P < 0.05). Students had a significant prolongation of daytime digital screen use and TV watching and an increase in the frequency of eye lubricant use and mean Perceived Stress Scale (PSS)-4 scores (all P < 0.05). Multiple logistic regression analysis revealed that studenthood and increased nighttime screen use were independent risk factors for DES by odds ratios (95% confidence intervals) of 10.60 (2.12 – 53.00) and 3.99 (1.71 – 9.34), respectively (both P < 0.05).
Conclusions:
Lockdown and closure of the university, with a shift to online learning, increased the exposure of staff and students to digital screens and the number of individuals with DES. Studenthood and prolonged nighttime digital screen use were independent risk factors for DES. Further studies investigating the prevalence and risk factors of DES, comparing similar data during and after the pandemic, may reveal other aspects of DES caused by virtual reality-based training.
Key Words: coronavirus disease 19, online learning, distance education, eyestrain, disease frequency survey, refractive error, university, staffs, students
INTRODUCTION
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2, emerged in Wuhan, China, and spread to the entire country by the end of December 2019 [1]. The World Health Organization declared a pandemic on March 11, 2020, causing enormous global concern [1-3]. Subsequently, different strategies were applied at local and global levels to prevent viral transmission [4].
Closure of schools and universities and shifting to online learning was an essential measure undertaken to prevent large-scale community transmission [5]. Shifting to online learning led to an increased number of individuals complaining of ocular and non-ocular symptoms due to prolonged use of digital screens, a condition called digital eye strain (DES) [6, 7], which was previously known as computer vision syndrome [8].
DES had a variable prevalence in the pre-COVID-19 era, and its overall prevalence increased during the COVID-19 pandemic [9]. The main ocular symptoms of DES include dry eye, eye burning, red eye, blurred vision, diplopia, and watery eye [9, 10]. These symptoms increase with an increased duration of exposure to digital screens [10].
This cross-sectional survey aimed to highlight the magnitude and associated risk factors of DES among university students and staff during the COVID-19 lockdown.
METHODS
We conducted a cross-sectional online survey between May and June 2020. The survey was created and sent via social media to the previous year’s students and staff members of the Faculty of Medicine, Tanta University, Tanta, Egypt, considering that the shift to online learning started in March 2020 [11]. The study protocol was in accordance with the tenets of the Declaration of Helsinki and reviewed and approved by the Medical Ethics Committee of Tanta University (IRB0010038/Approval code: 34009). All Participants provided informed consent.
The received results were sorted according to the inclusion and exclusion criteria. We included for analysis only surveys with complete answers and participant consent. Meanwhile, we excluded any surveys of students aged < 18 years, incomplete surveys, results of automated answering, and answers with contradictory results. We included only students above 18 years of age because they can consent to the inclusion of their results in our study and can provide reliable answers to the survey.
The online questionnaire was designed by two experienced ophthalmology consultants to collect the following data before and after the COVID-19 pandemic: (1) sociodemographic data; (2) DES-related symptoms, which are classified as ocular (dry eye, eye burning, red eye, watery eye, diplopia, and blurred vision) and somatic (neck, wrist, back, shoulder, and finger pain); (3) ocular and systemic comorbidities (refractive error, dry eye, stress, depression, and anxiety); (4) medications used (topical eye drops and systemic medications); and (5) pattern of digital screen use (number and types of screens used, duration of use, screen position, breaks taken while using screens, and room illumination).
We adapted questions on the symptoms of DES from the American Optometric Association (2010) and the American Optometric Association (2011) [12]. DES was diagnosed based on the presence of one or more of the above-mentioned ocular symptoms [13, 14]. The severity of each symptom was classified as none, mild (transient symptoms for a few minutes to hours), moderate (symptoms that persisted for a few hours and subsided with rest or sleep), and severe (symptoms that necessitated medical consultation) [15]. We adapted questions on symptoms of stress, depression, and anxiety from the 4-item Patient Health Questionnaire (PHQ-4) [16] and the Perceived Stress Scale (PSS)-4 questionnaire [17]. After completion of the survey, a statement was automatically delivered to each participant to raise awareness of proper practices during digital screen use.
Responses were downloaded into a Microsoft Excel data sheet (Microsoft Corp., Redmond, WA, USA), and statistical analyses were performed using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). Categorical data are presented as frequencies and percentages. Associations were tested using Pearson’s chi-square test for independence of observations or Fisher’s exact test (if more than 20% of cells in a contingency table had an expected count of less than 5). The Cochran – Armitage trend test was used to assess the associations between categorical and ordinal variables. McNemar and Wilcoxon matched pairs signed rank tests were conducted for two paired nominal variables consisting of two and more than two categories, respectively. Numerical variables were tested for normality of distribution using the Shapiro – Wilk test. Numerical variables following a normal distribution are summarized as mean (standard deviation [SD]). Comparisons between two paired and unpaired samples were performed using the paired and unpaired t-tests, respectively. Simple binomial logistic regression analysis was used to assess the effect of relevant variables (including sociodemographic factors, medication history, comorbidities, pattern of digital screen use, and psychological factors) for individuals with newly developed DES during the COVID-19 pandemic. Backward, stepwise, multiple binomial logistic regression analysis was then performed, including all risk factors with a P-value < 0.2 in the univariate analysis. In simple and multiple regression analyses, P-value, odds ratio (OR), and 95% confidence interval (95% CI) for each risk factor were reported. A P-value ≤ 0.05 was adopted for interpretation of the statistical results.
RESULTS
The target population comprised 753 participants, including 603 medical students and 150 staff members. We received 501 completed questionnaires, representing a response rate of 66.5%. After applying the inclusion and exclusion criteria, only 412 individuals were included in the analysis, of whom 34 (8.3%) were university staff members with a mean (SD) age of 36.7 (6.6) [range, 23.0 – 50.0] years and 378 (91.7%) were university students with a mean (SD) age of 20.8 (1.8) [range, 18.0 – 27.0] years. Information was anonymized by excluding names from the questionnaires. Female participants outnumbered male participants (66% versus 34%). Analysis of the responses revealed 294 (71.4%) participants with DES symptoms before the COVID-19 lockdown, of which 12 stopped experiencing symptoms during the lockdown. The number of participants with DES increased to 366 (88.8%) during the last month, with 84 new-onset DES cases.
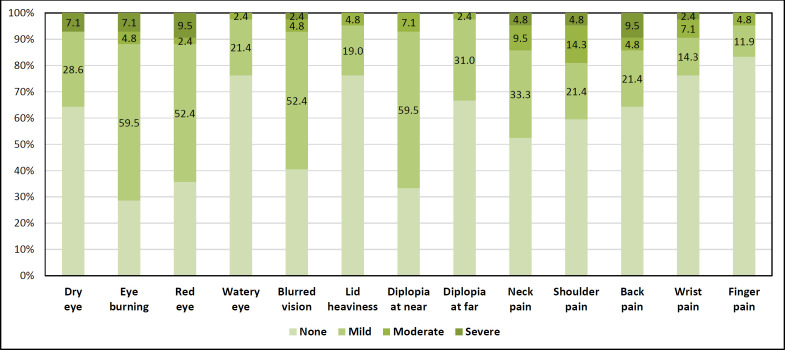
Among individuals with newly developed DES, the most frequent eye symptoms included eye burning (71.4%), diplopia at near (66.6%), red eye (64.3%), blurred vision (59.6%), dry eye (35.7%), diplopia at far (33.4%), lid heaviness (23.8%), and watery eye (23.8%). The most frequently reported somatic symptoms were neck (47.6%), shoulder (40.5%), back (35.7%), wrist (23.8%), and finger (16.7%) pain. The severity of each symptom is shown in Figure 1.
Figure 1.
Frequency and severity of digital eye strain-related symptoms among the participants with newly developed digital eye strain
Both staff and students had a significant prolongation of nighttime digital screen use (both P < 0.001) and TV watching (P < 0.05 and P < 0.001, respectively), as well as a reduced duration of daytime reading (P < 0.05 and P < 0.001, respectively) after the COVID-19 lockdown. In addition, the students had a significant prolongation of daytime digital screen use and TV watching (both P < 0.001) (Table 1).
Table 1.
Duration of digital screen use among the participants before and after the COVID-19 pandemic (total n = 412)
| Parameters | Staff (n = 34) | Student (n = 378) | P 1 | P 2 | P 3 | P 4 | |||
|---|---|---|---|---|---|---|---|---|---|
| Before COVID-19 | After COVID-19 | Before COVID-19 | After COVID-19 | ||||||
| Daytime digital screen use, n (%) | < 2 h | 10 (29.4) | 8 (23.5) | 122 (32.3) | 42 (11.1) | 0.826 a | < 0.001 a | 0.168 b | < 0.001 b |
| 2 – 4 h | 16 (47.1) | 18 (52.9) | 112 (29.6) | 76 (20.1) | |||||
| 4 – 6 h | 8 (23.5) | 8 (23.5) | 86 (22.8) | 134 (35.4) | |||||
| 6 – 2 h | 0 (0.0) | 0 (0.0) | 58 (15.3) | 126 (33.3) | |||||
| Nighttime digital screen use, n (%) | < 2 h | 18 (52.9) | 10 (29.4) | 94 (24.9) | 32 (8.5) | < 0.001 a | < 0.001 a | < 0.001 b | < 0.001 b |
| 2 – 4 h | 12 (35.3) | 8 (23.5) | 96 (25.4) | 66 (17.5) | |||||
| 4 – 6 h | 4 (11.8) | 16 (47.1) | 106 (28.0) | 116 (30.7) | |||||
| 6 – 12 h | 0 (0.0) | 0 (0.0) | 82 (21.7) | 164 (43.4) | |||||
| Daytime reading , n (%) | < 2 h | 20 (58.8) | 24 (70.6) | 176 (46.6) | 242 (64.0) | 0.009 a | < 0.001 a | 0.211 b | 0.050 b |
| 2 – 4 h | 6 (17.6) | 10 (29.4) | 64 (16.9) | 60 (15.9) | |||||
| 4 – 6 h | 0 (0.0) | 0 (0.0) | 30 (7.9) | 52 (13.8) | |||||
| 6 – 12 h | 8 (23.5) | 0 (0.0) | 108 (28.6) | 24 (6.3) | |||||
| Nighttime reading , n (%) | < 2 h | 22 (64.7) | 22 (64.7) | 158 (41.8) | 212 (56.1) | 0.366 a | 0.092 a | 0.008 b | 0.258 b |
| 2 – 4 h | 10 (29.4) | 6 (17.6) | 158 (41.8) | 82 (21.7) | |||||
| 4 – 6 h | 2 (5.9) | 6 (17.6) | 36 (9.5) | 58 (15.3) | |||||
| 6 – 12 h | 0 (0.0) | 0 (0.0) | 26 (6.9) | 26 (6.9) | |||||
| Daytime TV watching, n (%) | < 2 h | 30 (88.2) | 26 (76.5) | 306 (81.0) | 246 (65.1) | 0.383 a | < 0.001 a | 0.290 b | 0.186 b |
| 2 – 4 h | 2 (5.9) | 6 (17.6) | 38 (10.1) | 66 (17.5) | |||||
| 4 – 6 h | 2 (5.9) | 0 (0.0) | 16 (4.2) | 48 (12.7) | |||||
| 6 – 12 h | 0 (0.0) | 2 (5.9) | 18 (4.8) | 18 (4.8) | |||||
| Nighttime TV watching, n (%) | < 2 h | 30 (88.2) | 20 (58.8) | 268 (70.9) | 192 (50.8) | 0.002 a | < 0.001 a | 0.011 b | 0.081 b |
| 2 – 4 h | 4 (11.8) | 10 (29.4) | 52 (13.8) | 80 (21.2) | |||||
| 4 – 6 h | 0 (0.0) | 4 (11.8) | 42 (11.1) | 78 (20.6) | |||||
| 6 – 12 h | 0 (0.0) | 0 (0.0) | 16 (4.2) | 28 (7.4) | |||||
Abbreviations: COVID-19, coronavirus disease 2019; n, number of participants; %, percentage; h, hours; TV, television. P-values < 0.05 are shown in bold. Note: a, Wilcoxon matched pairs signed ranks test was used; b, Cochran – Armitage trend test was used; P1, P-value from test comparing staff data before and after COVID-19 lockdown; P2, P-value from test comparing student data before and after COVID-19 lockdown; P3, P-value from test comparing staff and student data before COVID-19 lockdown; P4, P -value from test comparing staff and student data after COVID-19 lockdown.
Among the staff, there were significant increases in the PHQ-4 severity scale and the presence of anxiety and depression (all P < 0.05). Among the students, there were significant increases in the frequency of eye lubricant use, PHQ-4 severity scale, mean PSS-4 scale, and presence of anxiety and depression after the COVID-19 lockdown (all P < 0.001) (Table 2).
Table 2.
Eye lubricant use, anxiety, depression, and stress among the participants before and after the COVID-19 pandemic (total n = 412)
| Parameters | Staff (n = 34) | Student (n = 378) | P 1 | P 2 | P 3 | P 4 | |||
|---|---|---|---|---|---|---|---|---|---|
| Before COVID-19 | After COVID-19 | Before COVID-19 | After COVID-19 | ||||||
| Lubricant use, n (%) | None | 30 (88.2) | 32 (94.1) | 312 (82.5) | 298 (78.8) | 0.500 a | < 0.001 a | 0.300 d | 0.025 d |
| Once daily | 4 (11.8) | 2 (5.9) | 46 (12.2) | 38 (10.1) | |||||
| 2 – 5 times daily | 0 (0.0) | 0 (0.0) | 20 (5.3) | 36 (9.5) | |||||
| > 5 times daily | 0 (0.0) | 0 (0.0) | 0 (0.0) | 6 (1.6) | |||||
| PHQ-4 severity score, n (%) | Normal (0 – 2) | 24 (70.6) | 12 (35.3) | 184 (48.7) | 64 (16.9) | 0.003 a | < 0.001 a | 0.162 d | 0.056 d |
| Mild (3 – 5) | 4 (11.8) | 12 (35.3) | 124 (32.8) | 142 (37.6) | |||||
| Moderate (6 – 8) | 4 (11.8) | 4 (11.8) | 48 (12.7) | 106 (28.0) | |||||
| Severe (9 – 12) | 2 (5.9) | 6 (17.6) | 22 (5.8) | 66 (17.5) | |||||
| PSS-4 score | Mean ± SD | 9.5 ± 1.6 | 9.7 ± 1.7 | 8.8 ± 2.3 | 10.3 ± 2.2 | 0.545 b | < 0.001 b | 0.024 e | 0.059 e |
| Anxiety, n (%) | No | 30 (88.2) | 20 (58.8) | 308 (81.5) | 212 (56.1) | 0.013 c | < 0.001 c | 0.326 d | 0.758 d |
| Yes | 4 (11.8) | 14 (41.2) | 70 (18.5) | 166 (43.9) | |||||
| Depression, n (%) | No | 28 (82.4) | 20 (58.8) | 284 (75.1) | 186 (49.2) | 0.008 c | < 0.001 c | 0.347 d | 0.283 d |
| Yes | 6 (17.6) | 14 (41.2) | 94 (24.9) | 192 (50.8) | |||||
Abbreviations: COVID-19, coronavirus disease 2019; n, number of participants; %, percentage; PHQ-4, the 4-item Patient Health Questionnaire; PSS-4, the Perceived Stress Scale questionnaire. P-values < 0.05 are shown in bold. Note: a, Wilcoxon matched pairs signed ranks test was used; b, paired t-test w; P1, P-value from test comparing staff data before and after COVID-19 lockdown; P2, P-value from test comparing student data before and after COVID-19 lockdown; P3, P-value from test comparing staff and student data before COVID-19 lockdown; P4, P -value from test comparing staff and student data after COVID-19 lockdown.
A simple binomial logistic regression analysis was conducted to assess the effect of each potential risk factor on the development of DES during the COVID-19 pandemic (Table 3). The variables that were significantly associated with a decreased probability of DES development included older age (OR, 0.90; 95% CI, 0.83 – 0.97) (P < 0.05), astigmatism (OR, 0.24; 95% CI, 0.07 – 0.84) (P < 0.05), near-sightedness (OR, 0.28; 95% CI, 0.09 – 0.82) (P < 0.05), wearing of eyeglasses (OR, 0.20; 95% CI, 0.09 – 0.44) (P < 0.001), and bright room illumination (OR, 0.47; 95% CI, 0.23 – 0.98) (P < 0.05). The factors that were significantly associated with increased probability of DES development included studenthood (OR, 11.29; 95% CI, 2.37 – 54.63) (P < 0.05) and increased daytime (OR, 3.11; 95% CI, 1.48 – 6.56) (P < 0.05) and nighttime (OR, 3.78; 95% CI, 1.72 – 8.30) (P < 0.05) screen use.
Table 3.
Simple binomial logistic regression analysis to assess the effect of the pattern of digital screen use and psychological factors on participants with newly developed DES during the COVID-19 pandemic (total n = 84)
| Parameters | P -value | OR (95% CI) |
|---|---|---|
| Sociodemographic data | ||
| Age (y) | 0.007 | 0.90 (0.83 – 0.97) |
| Sex (Female versus Male) | 0.159 | 0.59 (0.28 – 1.23) |
| Occupation (Student versus Staff) | 0.002 | 11.29 (2.37 – 54.63) |
| Refractive error and visual aids | ||
| Astigmatism | 0.025 | 0.24 (0.07 – 0.84) |
| Near-sightedness | 0.021 | 0.28 (0.09 – 0.82) |
| Eyeglasses | < 0.001 | 0.20 (0.09 – 0.44) |
| Pattern of digital screen use | ||
| Number of digital screens used | 0.404 | 0.78 (0.43 – 1.41) |
| Voluntary blinking when using screens | 0.253 | 1.54 (0.74 – 3.22) |
| Distance between eye and screen during use | 0.875 | 0.95 (0.53 – 1.72) |
| Position of screen (downward versus same eye level) | 0.842 | 0.93 (0.44 – 1.95) |
| Position of screen (upward versus same eye level) | 0.565 | 1.636 (0.31 – 8.74) |
| Change in daytime digital screen duration after COVID-19 (increased versus same / decreased) | 0.003 | 3.11 (1.48 – 6.56) |
| Change in nighttime digital screen duration after COVID-19 (increased versus same / decreased) | 0.001 | 3.78 (1.72 – 8.30) |
| Change in daytime reading duration after COVID-19 (increased versus same / decreased) | 0.358 | 1.75 (0.53 – 5.78) |
| Change in nighttime reading duration after COVID-19 (increased versus same / decreased) | 0.477 | 0.72 (0.29 – 1.78) |
| Change in daytime TV watching duration after COVID-19 (increased versus same / decreased) | 0.773 | 0.89 (0.39 – 2.03) |
| Change in nighttime TV watching duration after COVID-19 (increased versus same / decreased) | 0.168 | 1.80 (0.78 – 4.15) |
| Direction of room illumination during screen use (from above versus side) | 0.066 | 0.40 (0.149 – 1.06) |
| Room illumination intensity during screen use (bright versus dim) | 0.045 | 0.47 (0.23 – 0.98) |
| Anxiety, depression, and stress scales | ||
| Change in PHQ-4 scale score after COVID-19 (increased versus same / decreased) | 0.220 | 1.61 (0.75 – 3.43) |
| Depression | 0.773 | 0.89 (0.39 – 2.03) |
| Anxiety | 0.967 | 0.98 (0.41 – 2.35) |
| Change in PSS-4 scale score after COVID-19 (increased versus same / decreased) | 0.056 | 2.06 (0.98 – 4.33) |
Abbreviations: DES, digital eye strain; COVID-19, coronavirus disease 2019; n, number of participants with newly developed DES; OR, odds ratio; CI, confidence interval; y, years; TV, television; PHQ-4, the 4-item Patient Health Questionnaire; PSS-4 scale, the Perceived Stress Scale questionnaire. P-values < 0.05 are shown in bold (the dependent variable: DES).
Backward, stepwise, multiple, and binomial logistic regression analysis was then conducted to adjust for confounders (Table 4). In step 1, we included all factors with a P-value < 0.2 in simple regression analysis. The Nagelkerke R-square of model 1 was 0.303. The final model showed risk factors that increased the probability of DES during the COVID-19 lockdown: studenthood (OR, 10.60; 95% CI, 2.12 – 53.00) (P < 0.05), increased nighttime screen use (OR, 3.99; 95% CI, 1.71 – 9.34) (P < 0.05), and increased PSS-4 score (OR, 2.08; 95% CI, 0.91 – 4.74) (P = 0.081). Although the P-value for the PSS-4 score in the final model was greater than 0.05, the measurement was retained, as its removal would significantly affect the model. The Nagelkerke R-square of the final model was 0.259.
Table 4.
Multiple binomial logistic regression analysis to assess the effect of various risk factors on participants with newly developed DES during the COVID-19 pandemic (total n = 84)
| Model | Parameters | P -value | OR (95% CI) |
|---|---|---|---|
| Model 1 | Age (y) | 0.366 | 1.13 (0.87 – 1.46) |
| Sex (female versus male) | 0.213 | 0.515 (0.18 – 1.46) | |
| Occupation (student versus staff) | 0.123 | 42.19 (0.36 – 4897.59) | |
| Astigmatism with near-sightedness | 0.723 | 1.45 (0.18 – 11.46) | |
| Duration of daytime digital screen use (increased versus same / decreased) | 0.661 | 1.29 (0.41 – 4.09) | |
| Duration of nighttime digital screen use (increased versus same / decreased) | 0.036 | 3.12 (1.08 – 9.05) | |
| Duration of nighttime TV watching (increased versus same / decreased) | 0.328 | 1.74 (0.57 – 5.30) | |
| Direction of room illumination during screen use (from above versus side) | 0.245 | 0.49 (0.14 – 1.64) | |
| Room illumination intensity during screen use (bright versus dim) | 0.739 | 0.86 (0.34 – 2.14) | |
| PHQ-4 scale score (increased versus same / decreased) | 0.498 | 1.42 (0.515 – 3.91) | |
| PSS-4 scale score (increased versus same / decreased) | 0.115 | 2.03 (0.84 – 4.92) | |
| Model 2 | Occupation (student versus staff) | 0.004 | 10.60 (2.12 – 53.00) |
| Duration of nighttime digital screen use (increased versus same / decreased) | 0.001 | 3.99 (1.71 – 9.34) | |
| PSS-4 (increased versus same / decreased) | 0.081 | 2.08 (0.91 – 4.74) |
Abbreviations: DES, digital eye strain; COVID-19, coronavirus disease 2019; n, number of participants with newly developed DES; OR, odds ratio; CI, confidence interval; y, years; TV, television; PHQ-4, the 4-item Patient Health Questionnaire; PSS-4 scale, the Perceived Stress Scale questionnaire. P-values < 0.05 are shown in bold (the dependent variable: DES).
DISCUSSION
We found that the COVID-19 lockdown in the university, with the shift to online learning, increased the exposure of staff and students to digital screens and increased the number of individuals with DES. Studenthood and prolonged nighttime digital screen use were independent risk factors for DES.
The American Optometric Association defines computer vision syndrome as a “complex of eye and vision problems related to near work, which are experienced during or related to computer use” [12, 13, 18]. The current terminology for this syndrome is DES [7]. The emergence of the COVID-19 pandemic in late 2019 and early 2020 caused many changes in the lifestyles and academic strategies of teachers and students in universities and schools [19-21], including the more frequent and prolonged use of digital screens, with an expected increase in the prevalence of DES [6, 22, 23]. In the current study, 412 participants were analyzed (378 university students and 34 staff members), and 71.4% of them had symptoms of DES before the COVID-19 lockdown, which increased to 88.8% during the last month.
Our results are comparable to those of a study conducted among Nepalese medical students, which reported a 71.6% prevalence of DES [24]. However, other studies have reported higher prevalences of 94.8% and 89.9% among university students in Pakistan and Malaysia, respectively [25, 26]. The incidence of DES among users of digital screens ranges between 64% and 90% [10, 26-29].
DES symptoms can develop with a daily digital screen exposure of more than 3.59 h [13]. After the COVID-19 pandemic, 23.5% of staff and 65.7% of students used digital screens for more than 4 h per day during the daytime, and 47.1% of staff and 74.1% of students used screens for more than 4 h at night. With the shift to online learning, we found a significant increase in the frequency of DES and severity of symptoms with an increased duration of nighttime digital screen use, with an OR of 3.99 (95% CI, 1.71 – 9.34).
The main reported ocular symptoms of DES are dry eye, eye burning, red eye, blurred vision, diplopia, and watery eye. These symptoms increase with an increased duration of exposure to digital screens [10, 29]. The symptoms recorded in our study, in order of decreasing frequency, were eye burning, diplopia at near, red eye, blurred vision, dry eye, diplopia at far, lid heaviness, and watery eye.
Decreased blinking rate, completeness of blinking, and increased evaporation during digital screen use are the main causes of ocular surface changes and dry eye [30]. Excessive eye watering sometimes occurs after prolonged screen exposure to rebuild the chemical balance of the tear film and re-wet the eye [31]. The students accounted for 91.7% of our participants and reported a significant increase in eye lubricant use after the COVID-19 lockdown. Overall, 23.8% of the participants reported a watery eye.
Blurred vision and diplopia are common symptoms of DES [32-36], which could be due to a reduced accommodative response, vergence abnormalities, and ocular muscle fatigue caused by prolonged use and improper positioning of screens [37]. Other causes include uncorrected refractive error, dry eye, and unstable tear film [7]. We documented diplopia at near in 66.6%, blurred vision in 59.6%, dry eye in 35.7%, and diplopia at far in 33.4% of participants. Future studies with detailed slit-lamp examinations and comprehensive binocular vision testing could identify the underlying cause of these DES-related symptoms in this cohort.
Uncorrected refractive errors add more strain to the oculomotor system to adjust the retinal image and decrease blur [38]. Zayed et al. [39] found that wearing corrective glasses was a significant predictor of DES, with an OR of 5.01, among information technology professionals at Tanta University, Egypt. Other significant predictors in order of the OR magnitude were the use of an air conditioner (OR, 23.02), exposure to air pollution (OR, 5.67), wearing corrective glasses (OR, 5.01), distance from the monitor of less than 20 inches (OR, 4.39), exposure to windy environments (OR, 3.59), female sex (OR, 2.85), duration of work more than 10 years (OR, 1.79), daily computer use for more than 6 h (OR, 1.35), age ≥ 35 years (OR, 1.11), not using an antiglare screen (OR, 0.21), no brightness adjustment of the screen (OR, 0.02), and not taking break time during computer work (OR, 0.01) [39]. In our study, near-sightedness and astigmatism were significant risk factors for DES, with ORs of 0.28 and 0.24, respectively.
In our study, DES was higher among participants with refractive errors who did not wear eyeglasses than among those who did. However, a recent study on DES among radiologists did not report any statistically significant differences between the groups [14]. Frequent breaks are essential when using digital screens, and frequent short breaks are more effective than longer occasional breaks [40]. However, in our study, less than 6% of all participants took regular breaks from screen work every 30 min; 5.9% of staff and 5.8% of students took regular breaks.
Most of our participants were students (91.7%) with a higher risk for DES than staff, which could be explained by the longer duration of digital screen use among students than staff, as we found that 65.7% of students versus 23.5% of staff used digital screens more than 4 h per day during the daytime, and 74.1% of students versus 47.1% of staff used screens more than 4 h at nighttime. Reducing nighttime screen use and using glasses that block blue light, which is radiated by a light-emitting diode computer screen [41, 42], were recommended to relieve the undesirable effects of digital screen use.
In addition to eye symptoms, somatic disorders, anxiety, stress, and depression are associated with prolonged use of digital screens [13, 31, 43]. In this study, we included questions on symptoms of stress, depression, and anxiety, adapted from the PHQ-4 [16] and PSS-4 questionnaires [17]. We found a significant increase in the PHQ-4 scale scores for anxiety and depression and the PHQ-4 severity scale scores among staff and students after the COVID-19 lockdown. In addition, there was a significant increase in PSS-4 scores among the students. Fear, total lockdown, isolation, and quarantine could be contributing factors [44].
Concerning DES-related somatic symptoms, 47.6% of our participants complained of neck pain, and 40.5%, 35.7%, 23.8%, and 16.7% had shoulder pain, back pain, wrist pain, and finger pain, respectively. Proper positioning of digital screens with the top line at or just below eye level can effectively relieve most of these symptoms [13]. Munchi et al. [45] found that eye muscles are less strained when viewing computer screens in a downward gaze position with an angle of 14° or more [45]. Fifty percent of our participants used digital screens below eye level, 46.6% at the same eye level, and 3.4% above eye level.
The recommended strategy for reducing DES symptoms is the famous (20/20/20) rule: viewing a distant object at 20 feet or more for at least 20 s after 20 min of digital screen use. However, frequent breaks in general and moving about can also help reduce eye and somatic manifestations [13]. The use of lubricating eye drops, maintaining a regular blink rate [26], placing the screens in an ergonomic posture (a distance of 20 – 40 inches with the top line at or just below eye level), correcting refractive errors, proper illumination, and regular ocular examinations with associated counseling [13, 46] are among the recommended solutions. In our study, the final model showed increased nighttime screen use as an independent risk factor for DES during the COVID-19 lockdown, with an OR of 3.99 (95% CI, 1.71 – 9.34). One possible reason is reduced illumination at night.
Our online survey highlighted the magnitude of DES and its associated risk factors to help prevent complications of DES among university students and staff. Our study is limited by the small sample size, lack of randomization, subjective nature of the online survey, and the possibility of recall bias. However, considering the COVID-19 restrictions and the limitations on elective medical services, this online survey was our means to measure the impact of DES and to raise awareness among university students and staff regarding proper practices during the use of digital screens. Future randomized studies with face-to-face interviews and detailed ocular examinations could provide strong evidence for the associated risk factors of developing DES among university students and staff. Furthermore, studies on the prevalence and risk factors of DES among the same population, comparing similar data collected during and after the pandemic, may reveal other aspects of DES caused by virtual reality-based training.
CONCLUSIONS
The COVID-19 lockdown and closure of the university, with a shift to online learning, increased the exposure of both staff and students to digital screens and was associated with an increased frequency of DES. The frequency of DES increased among the students and staff of the Faculty of Medicine, Tanta University, after the COVID-19 lockdown. Studenthood and prolonged nighttime digital screen use were independent risk factors for DES in our study. Future randomized clinical trials with face-to-face interviews are needed to verify our findings concerning the associated risk factors for developing DES among university students and staff.
ETHICAL DECLARATIONS
Ethical approval:
The study protocol was in accordance with the tenets of the Declaration of Helsinki and reviewed and approved by the Medical Ethics Committee of Tanta University (IRB0010038/Approval code: 34009). All Participants provided informed consent.
Conflict of interest:
None.
FUNDING
None.
ACKNOWLEDGMENTS
None.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan JF, Lau SK, To KK, Cheng VC, Woo PC, Yuen KY. Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS-like disease. Clin Microbiol Rev. 2015;28(2):465–522. doi: 10.1128/CMR.00102-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Girum T, Lentiro K, Geremew M, Migora B, Shewamare S. Global strategies and effectiveness for COVID-19 prevention through contact tracing, screening, quarantine, and isolation: a systematic review. Trop Med Health. 2020;48(1):91 . doi: 10.1186/s41182-020-00285-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harapan H, Itoh N, Yufika A, Winardi W, Keam S, Te H, et al. Coronavirus disease 2019 (COVID-19): A literature review. J Infect Public Health. 2020;13(5):667–673. doi: 10.1016/j.jiph.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital eye strain among kids (DESK study-1) Indian J Ophthalmol. 2021;69(1):140–144. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coles-Brennan C, Sulley A, Young G. Management of digital eye strain. Clin Exp Optom. 2019;102(1):18–29. doi: 10.1111/cxo.12798. [DOI] [PubMed] [Google Scholar]
- 8.Klamm J, Tarnow KG. Computer Vision Syndrome: A Review of Literature. Medsurg Nurs. 2015;24(2):89–93. [PubMed] [Google Scholar]
- 9.Kaur K, Gurnani B, Nayak S, Deori N, Kaur S, Jethani J, et al. Digital Eye Strain- A Comprehensive Review. Ophthalmol Ther. 2022;11(5):1655–1680. doi: 10.1007/s40123-022-00540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Travers PH, Stanton BA. Office workers and video display terminals: physical, psychological and ergonomic factors. AAOHN J. 2002;50(11):489–93. [PubMed] [Google Scholar]
- 11.Mahdy MAA, Sayed RKA. Evaluation of the online learning of veterinary anatomy education during the Covid-19 pandemic lockdown in Egypt: Students’ perceptions. Anat Sci Educ. 2022;15(1):67–82. doi: 10.1002/ase.2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Optometric Association (2010-2011) Computer vision syndrome. [Accessed: October 20, 2022]. [Google Scholar]
- 13.Bali J, Neeraj N, Bali RT. Computer vision syndrome: A review. Journal of clinical ophthalmology and research. 2014;2(1):61. [Google Scholar]
- 14.Al Dandan O, Hassan A, Al Shammari M, Al Jawad M, Alsaif HS, Alarfaj K. Digital Eye Strain Among Radiologists: A Survey-based Cross-sectional Study. Acad Radiol. 2021;28(8):1142–1148. doi: 10.1016/j.acra.2020.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Logaraj M, Madhupriya V, Hegde S. Computer vision syndrome and associated factors among medical and engineering students in chennai. Ann Med Health Sci Res. 2014;4(2):179–85. doi: 10.4103/2141-9248.129028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1-2):86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Cheema S, Maisonneuve P, Abraham A, Chaabna K, Tom A, Ibrahim H, et al. Factors associated with perceived stress in Middle Eastern university students. J Am Coll Health. 2022;70(8):2462–2469. doi: 10.1080/07448481.2020.1865979. [DOI] [PubMed] [Google Scholar]
- 18.Ranasinghe P, Wathurapatha WS, Perera YS, Lamabadusuriya DA, Kulatunga S, Jayawardana N, et al. Computer vision syndrome among computer office workers in a developing country: an evaluation of prevalence and risk factors. BMC Res Notes. 2016;9:150 . doi: 10.1186/s13104-016-1962-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Plakhotnik MS, Volkova NV, Jiang C, Yahiaoui D, Pheiffer G, McKay K, et al. The Perceived Impact of COVID-19 on Student Well-Being and the Mediating Role of the University Support: Evidence From France, Germany, Russia, and the UK. Front Psychol. 2021;12:642689. doi: 10.3389/fpsyg.2021.642689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tan W. School closures were over-weighted against the mitigation of COVID-19 transmission: A literature review on the impact of school closures in the United States. Medicine (Baltimore). 2021;100(30):e26709. doi: 10.1097/MD.0000000000026709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barrot JS, Llenares II, Del Rosario LS. Students’ online learning challenges during the pandemic and how they cope with them: The case of the Philippines. Educ Inf Technol (Dordr). 2021;26(6):7321–7338. doi: 10.1007/s10639-021-10589-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seresirikachorn K, Thiamthat W, Sriyuttagrai W, Soonthornworasiri N, Singhanetr P, Yudtanahiran N, et al. Effects of digital devices and online learning on computer vision syndrome in students during the COVID-19 era: an online questionnaire study. BMJ Paediatr Open. 2022;6(1):e001429 . doi: 10.1136/bmjpo-2022-001429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abuallut I, Qumayi EA, Mohana AJ, Almalki NM, Ghilan ME, Dallak FH, et al. Prevalence of Asthenopia and Its Relationship with Electronic Screen Usage During the COVID-19 Pandemic in Jazan, Saudi Arabia: A Cross-Sectional Study. Clin Ophthalmol. 2022;16:3165–3174. doi: 10.2147/OPTH.S377541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kharel Sitaula R, Khatri A. Knowledge, Attitude and practice of Computer Vision Syndrome among medical students and its impact on ocular morbidity. J Nepal Health Res Counc. 2018;16(3):291–296. [PubMed] [Google Scholar]
- 25.Noreen K, Batool Z, Fatima T, Zamir T. Prevalence of computer vision syndrome and its associated risk factors among under graduate medical students of urban karachi. Pakistan Journal of Ophthalmology. 2016;32(3):140–146. [Google Scholar]
- 26.Reddy SC, Low CK, Lim YP, Low LL, Mardina F, Nursaleha MP. Computer vision syndrome: a study of knowledge and practices in university students. Nepal J Ophthalmol. 2013;5(2):161–8. doi: 10.3126/nepjoph.v5i2.8707. [DOI] [PubMed] [Google Scholar]
- 27.Hayes JR, Sheedy JE, Stelmack JA, Heaney CA. Computer use, symptoms, and quality of life. Optom Vis Sci. 2007;84(8):738–44. doi: 10.1097/OPX.0b013e31812f7546. [DOI] [PubMed] [Google Scholar]
- 28.Munsamy AJ, Naidoo S, Akoo T, Jumna S, Nair P, Zuma S, et al. A case study of digital eye strain in a university student population during the 2020 COVID-19 lockdown in South Africa: evidence of an emerging public health issue. J Public Health Afr. 2022;13(3):2103. doi: 10.4081/jphia.2022.2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basnet A, Pathak SB, Marasini A, Pandit R, Pradhan A. Digital Eye Strain among Adults Presenting to Tertiary Care Hospital in the Era of COVID-19 Pandemic: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2022;60(245):22–25. doi: 10.31729/jnma.7092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palakuru JR, Wang J, Aquavella JV. Effect of blinking on tear dynamics. Invest Ophthalmol Vis Sci. 2007;48(7):3032–7. doi: 10.1167/iovs.06-1507. [DOI] [PubMed] [Google Scholar]
- 31.Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: a review. Surv Ophthalmol. 2005;50(3):253–62. doi: 10.1016/j.survophthal.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 32.Gowrisankaran S, Sheedy JE. Computer vision syndrome: A review. Work. 2015;52(2):303–14. doi: 10.3233/WOR-152162. [DOI] [PubMed] [Google Scholar]
- 33.Bogdănici CM, Săndulache DE, Nechita CA. Eyesight quality and Computer Vision Syndrome. Rom J Ophthalmol. 2017;61(2):112–116. doi: 10.22336/rjo.2017.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thorud HM, Helland M, Aarås A, Kvikstad TM, Lindberg LG, Horgen G. Eye-related pain induced by visually demanding computer work. Optom Vis Sci. 2012;89(4):E452–64. doi: 10.1097/OPX.0b013e31824c1801. [DOI] [PubMed] [Google Scholar]
- 35.Chu C, Rosenfield M, Portello JK, Benzoni JA, Collier JD. A comparison of symptoms after viewing text on a computer screen and hardcopy. Ophthalmic Physiol Opt. 2011;31(1):29–32. doi: 10.1111/j.1475-1313.2010.00802.x. [DOI] [PubMed] [Google Scholar]
- 36.Sa EC, Ferreira Junior M, Rocha LE. Risk factors for computer visual syndrome (CVS) among operators of two call centers in São Paulo, Brazil. Work. 2012;41 Suppl 1:3568–74. doi: 10.3233/WOR-2012-0636-3568. [DOI] [PubMed] [Google Scholar]
- 37.Butzon SP, Sheedy JE, Nilsen E. The efficacy of computer glasses in reduction of computer worker symptoms. Optometry. 2002;73(4):221–30. [PubMed] [Google Scholar]
- 38.Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31(5):502–15. doi: 10.1111/j.1475-1313.2011.00834.x. [DOI] [PubMed] [Google Scholar]
- 39.Zayed HAM, Saied SM, Younis EA, Atlam SA. Digital eye strain: prevalence and associated factors among information technology professionals, Egypt. Environ Sci Pollut Res Int. 2021;28(20):25187–25195. doi: 10.1007/s11356-021-12454-3. [DOI] [PubMed] [Google Scholar]
- 40.Mclean L, Tingley M, Scott RN, Rickards J. Computer terminal work and the benefit of microbreaks. Appl Ergon. 2001;32(3):225–37. doi: 10.1016/s0003-6870(00)00071-5. [DOI] [PubMed] [Google Scholar]
- 41.Mylona I, Deres ES, Dere GS, Tsinopoulos I, Glynatsis M. The Impact of Internet and Videogaming Addiction on Adolescent Vision: A Review of the Literature. Front Public Health. 2020;8:63. doi: 10.3389/fpubh.2020.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Lely S, Frey S, Garbazza C, Wirz-Justice A, Jenni OG, Steiner R, et al. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J Adolesc Health. 2015;56(1):113–9. doi: 10.1016/j.jadohealth.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Thomée S, Härenstam A, Hagberg M. Computer use and stress, sleep disturbances, and symptoms of depression among young adults--a prospective cohort study. BMC Psychiatry. 2012;12:176 . doi: 10.1186/1471-244X-12-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 45.Munshi S, Varghese A, Dhar-Munshi S. Computer vision syndrome-A common cause of unexplained visual symptoms in the modern era. Int J Clin Pract. 2017;71:7. doi: 10.1111/ijcp.12962. [DOI] [PubMed] [Google Scholar]
- 46.Anshel JR. Visual ergonomics in the workplace. AAOHN J. 2007;55(10):414–20; quiz 421-2. doi: 10.1177/216507990705501004. [DOI] [PubMed] [Google Scholar]