Abstract
Background:
The coronavirus disease 2019 (COVID-19) pandemic has been the most challenging health problem in the last 2 years. Post-COVID-19 multisystem inflammatory syndrome of children (MIS-C) is a severe post-COVID-19 complication in pediatric patients. Ocular manifestations may be the first presentation of MIS-C, wherein prompt treatment may improve outcomes. In this systematic review, we aimed to summarize the acute and sub-acute ocular manifestations in pediatric patients with laboratory-confirmed COVID-19.
Methods:
We included all online primary studies, with no language restriction and published between January 1, 2019 and November 18, 2020, reporting any acute or sub-acute ocular manifestations in children with laboratory-confirmed COVID-19. PubMed/MEDLINE was searched using the following MeSH and Emtree terms: “eye,” “ophthalmologic,” “ocular,” “vision,” “conjunctivitis,” “severe acute respiratory syndrome coronavirus 2,” “SARS-CoV-2,” “corona,” “2019-nCoV,” “COVID19,” and “COVID.” The eligibility and quality of the selected records were assessed by two independent reviewers as per the Cochrane Handbook for Systematic Review.
Results:
A total of 1,192 records were identified electronically. Seven papers were extracted from the reference lists of the eligible records. Thirty-six papers met the inclusion criteria and were categorized into two subgroups according to acute or sub-acute presentation of ocular manifestations. Among 463 pediatric patients with COVID-19, 72 (15.5%) had acute ocular manifestations. There was one patient with central retinal vein occlusion and another with photophobia and diplopia associated with meningoencephalitis. Among 895 pediatric patients with post-COVID-19 MIS-C, 469 (52.4%) had ocular manifestations, which only included non-purulent conjunctivitis.
Conclusions:
Ocular manifestations have been reported in less than one-fifth of pediatric patients with acute COVID-19. Furthermore, conjunctivitis was the only ocular manifestation reported in half of the patients with MIS-C, and it may be missed easily due to its non-purulent nature. During the COVID-19 pandemic, pediatricians and health workers must remain vigilant for early detection of signs of this potentially fatal post-COVID-19 inflammatory syndrome.
Key Words: COVID-19, pandemic, coronavirus disease 2019, severe acute respiratory syndrome coronavirus 2, SARS-CoV-2, children, conjunctivitis, multisystem inflammatory syndrome, pediatrician
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has been the most challenging health concern in the last two years. Due to different mutations in the causative virus, the presenting symptoms of COVID-19 continue to change and have caused diagnostic problems [1]. The signs and symptoms of COVID-19 in pediatric patients differ from those in adults. Among pediatric patients, ocular involvement has been reported as an acute COVID-19 presentation or as a sub-acute manifestation of post-COVID-19 multisystem inflammatory syndrome in children (MIS-C) [2-5].
MIS-C has a latency phase of 4–5 weeks and may be associated with myocardial dysfunction and shock [4]. Ocular manifestations can be self-resolving in children with COVID-19 [3]. However, they may be the first symptoms, especially in MIS-C, in which accelerated treatment may improve outcomes [3, 6].
Previous systematic reviews have evaluated MIS-C as a complication of post-COVID-19 condition and underlined ocular signs as an important clue for diagnosing MIS-C [7-10]. Although ocular manifestations have been reported as an acute presentation of COVID-19 in children [11-18], to our knowledge, no previous systematic review has addressed this topic. Owing to the significance of detecting early ocular signs or symptoms in children with COVID-19, we aimed to summarize the acute and sub-acute ocular manifestations in pediatric patients with laboratory-confirmed COVID-19.
METHODS
This systematic review was conducted according to the guidelines of the Cochrane Handbook for Systematic Reviews [19] and Methodological Expectations of Cochrane Intervention Reviews (MECIR) [20], and reported as per the Preferred Reporting Items for Systematic Review and Meta-Analysis checklist [21]. The protocol for this systematic review was registered and peer-reviewed at the Endocrinology and Metabolism Research Institute of Tehran University of Medical Science, Tehran, Iran, and received ethical approval (ethical code: IR.TUMS.EMRI.REC.1399.063).
The eligibility criteria included: online primary studies with no language restrictions, reporting any ocular manifestations (patient-reported or clinician-observed) in children (aged < 18 years) with laboratory-confirmed COVID-19 according to the World Health Organization (WHO) diagnostic criteria [22], regardless of their ethnicity. Studies published between January 1, 2019, and November 18, 2020, were included.
Ocular manifestations could be a sign of MIS-C [22], which is reportedly an adverse effect of sub-acute post-COVID-19 condition. Therefore, we included studies reporting a history of laboratory-confirmed COVID-19 (reverse transcription-polymerase chain reaction, antigen test, or serologic test) before ocular manifestations. We excluded studies that did not report the patients’ age, the exact type of ocular manifestation, or pediatric patients with no laboratory evidence of COVID-19 infection. Moreover, we excluded all types of review papers, in vitro, and animal studies.
All online primary studies published between January 1, 2019, and November 18, 2020 were extracted from the PubMed/MEDLINE database, with no language limitation or publication-type restriction. The following MeSH or Emtree keywords were selected: “eye,” “ophthalmologic,” “ocular,” “vision,” “conjunctivitis,” “severe acute respiratory syndrome coronavirus 2,” “SARS-CoV-2,” “corona,” “2019-nCoV,” “COVID19,” and “COVID.” We developed syntax for the PubMed/MEDLINE database, as shown in Table 1. We determined the syntax sufficiency, and the number needed to read the finalized syntax was 50.
Table 1.
Final search syntax developed for searching the PubMed/MEDLINE database
| Summary Search Syntax | Complete Search Syntax |
|---|---|
| #1 Mesh or Emtree descriptor for first component #2 (Eye) #3(Ophthal*) #4(Vision AND Ocular) #5 (Conjunc*) #6 (#1 OR #2 OR #3 OR #4 OR #5) #7 Mesh or Emtree descriptor for second component #8 (COVID*) #9 “COVID19” #10 (corona*) #11 (SARS-CoV-2*) #12 (2019-nCoV*) #13 “Severe acute respiratory syndrome coronavirus 2” #14 (#7 OR #8 OR #9 #10 OR #11 OR #12 OR #13) #15 (#6 AND #14), from 2019 to 2020/11/18 |
“(Eye[tiab] OR Ophthal*[tiab] OR (Vision AND Ocular)[tiab] OR Conjunc*) AND (COVID*[tiab] OR “COVID19”[tiab] OR corona*[tiab] OR SARS-CoV-2*[tiab] OR 2019-nCoV*[tiab] OR “Severe acute respiratory syndrome coronavirus 2”[tiab]) AND 2019:2020/11/18[dp]” |
Abbreviations: tiab, title or abstract; dp, date of publication.
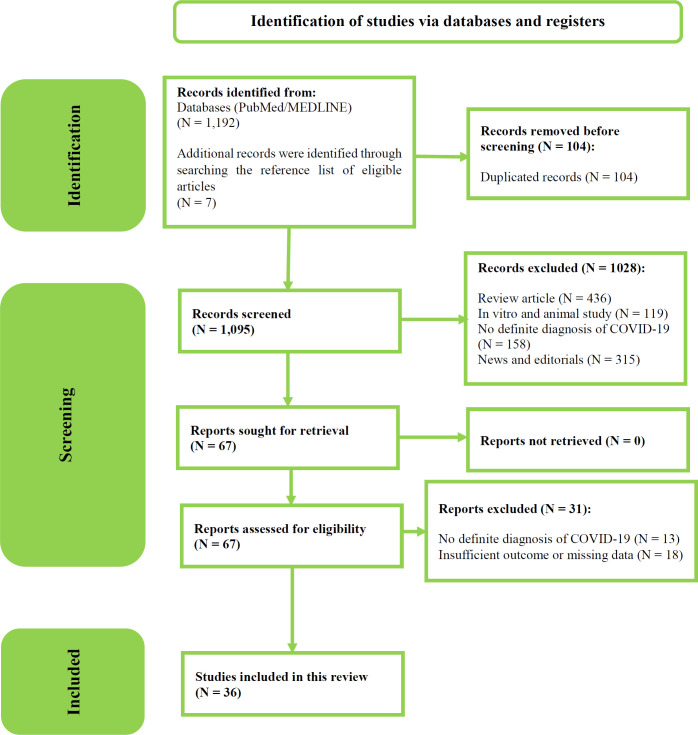
For study selection, we pooled the searched records using EndNote X8 (Clarivate Analytics, Philadelphia, PA), following which, the duplicate records were removed. Two independent reviewers screened the titles and abstracts of the remaining articles to assess their quality and eligibility, which were evaluated by the same two reviewers in accordance with the Cochrane Handbook for Systematic Review [19]. Figure 1 shows the flowchart for the search strategy, screening, and selection of the final eligible studies.
Figure 1.
Flowchart of the search strategy, screening, and selection of the eligible primary studies
For data extraction and management, the complete text of all eligible studies was reviewed by the same two independent reviewers, and the required information was extracted. This included the PubMed identifier, first author’s name, year of publication, title, total number of pediatric patients with laboratory-confirmed COVID-19 infection, number of children with ocular manifestations, mean ± standard deviation (SD) or median (interquartile range [IQR]) age of the included pediatric patients, and type of ocular manifestation. The reported ocular manifestations comprised conjunctivitis; eye pruritis; white mucoid, watery, or purulent conjunctival discharge; conjunctival congestion or hyperemia; pain; eye rubbing; eyelid dermatitis; diplopia; photophobia; and central retinal vein occlusion. In case of a conflict, a decision was taken based on the consensus among the reviewers.
For studies that lacked any of the aforementioned data, two emails with a 1-week interval were sent to the corresponding authors to recover the missing data, and if no reply was received within a 2-weeks’ time, those papers were excluded. All data extraction and analyses were completed independently by two reviewers. For data synthesis, all selected studies, including cross-sectional studies, case series, or case reports, were reported according to the time course of the ocular manifestations (acute or sub-acute subsets of presentation; Table 2).
Table 2.
Characteristics of included articles; categorized into two sub-groups (acute and sub-acute ocular manifestations)
| Course of ocular presentation | Code | Author (publication year) | Type of study | N | Age (y); Mean ± SD or Median (IQR) | N’ (%) | Ocular manifestations |
|---|---|---|---|---|---|---|---|
| Acute | 1 | Burke et al. (2020) [18] | Cross-sectional | 9 | 3.8 ± 3.1 | 2 (22.2) | Conjunctivitis |
| 2 | Ma et al. (2020) [17] | Cross-sectional | 216 | 7.25 (2.6–11.6) | 49 (22.7) | Conjunctival discharge, conjunctival congestion, eye rubbing | |
| 3 | Storch-de-Gracia et al. (2020) [16] | Cross-sectional | 39 | 2.5 (1–10) | 7 (17.9) | Conjunctival hyperaemia | |
| 4 | Valente et al. (2020) [15] | Cross-sectional | 27 | 9.6 ± 4.2 / 8.8 (6–14) | 4 (15) | Conjunctivitis | |
| 5 | Walinjkar et al. (2020) [14] | Case report | 1 | 17 | 1 (NR) | Central retinal vein occlusion | |
| 6 | Wu et al. (2020) [13] | Case report | 1 | 2.8 | 1 (NR) | Conjunctivitis, eyelid dermatitis | |
| 7 | Yousefi et al. (2021) [12] | Case report | 1 | 9 | 1 (NR) | Photophobia, diplopia | |
| 8 | Garazzino et al. (2020) [11] | Cross-sectional | 168 | 5 ± NM, 2.3 (0.3–9.6) | 6 (3.6) | Conjunctivitis | |
| 9 | Ya et al. (2020) [23] | Case report | 1 | 16 | 1 (NR) | Conjunctivitis | |
| Sub-acute | 10 | Whittaker et al. (2020) [24] | Case series | 58 | 9 (5.7–14) | 26 (45) | Conjunctivitis |
| 11 | Verdoni et al. (2020) [25] | Cross-sectional | 8 | 7.5 ± 3.5 | 3 (37.5) | Conjunctivitis | |
| 12 | Toubiana et al. (2020) [26] | Cross-sectional | 19 | 7.9 (3.7–16.6) | 17 (81) | Conjunctivitis | |
| 13 | Tam et al. (2020) [27] | Case report | 1 | 10 | 1 (NR) | Conjunctivitis | |
| 14 | Spencer et al. (2020) [28] | Case series | 2 | 9 ± 2 | 2 (100) | Conjunctivitis | |
| 15 | Schneider et al. (2020) [29] | Case report | 1 | 9 | 1 (NR) | Conjunctivitis | |
| 16 | Riphagen et al. (2020) [30] | Case series | 2 | 6 | 1 (50) | Conjunctivitis | |
| 17 | Raut et al. (2021) [31] | Case report | 1 | 0.4 | 1 (NR) | Conjunctivitis | |
| 18 | Pouletty et al. (2020) [32] | Cross-sectional | 15 | 9 (4.5–12) | 14 (91.6) | Conjunctivitis | |
| 19 | Nelson et al. (2020) [33] | Case report | 1 | 15 | 1 (NR) | Conjunctivitis | |
| 20 | Mamishi et al. (2020) [34] | Cross-sectional | 45 | 7 (4 –9.9) | 23 (51) | Conjunctivitis | |
| 21 | Licciardi et al. (2020) [35] | Case report | 2 | 9.5 ± 3.5 | 2 (100) | Conjunctivitis | |
| 22 | Lee et al. (2020) [36] | Case report | 1 | 7 | 1 (NR) | Conjunctivitis | |
| 23 | Vukomanovic et al. (2021) [37] | Case series | 3 | 15 ± 1.7 | 3 (100) | Conjunctivitis | |
| 24 | Kim et al. (2020) [38] | Case report | 1 | 11 | 1 (NR) | Conjunctivitis | |
| 25 | Khan et al. (2020) [39] | Case report | 1 | 8 | 1 (NR) | Conjunctivitis | |
| 26 | Kest et al. (2020) [40] | Case series | 3 | 8.3 ± 2 | 3 (100) | Conjunctivitis | |
| 27 | Heidemann et al. (2020) [41] | Case series | 3 | 6 ± 1 | 2 (66.6) | Conjunctivitis | |
| 28 | Grimaud et al. (2020) [42] | Cross-sectional | 20 | 10 (2.9–15) | 6 (30) | Conjunctivitis | |
| 29 | Godfredl-Cato et al. (2020) [43] | Cross-sectional | 565 | 8 (4 –12) | 276 (48.4) | Conjunctivitis | |
| 30 | Felsenstein et al. (2020) [44] | Cross-sectional | 15 | 6 (3.8–9.9) | 9 (62) | Conjunctivitis | |
| 31 | Falah et al. (2020) [45] | Cross-sectional | 9 | 6.3 ± 4.1 | 8 (89) | Conjunctivitis | |
| 32 | Dufort et al. (2020) [6] | Cross-sectional | 99 | 8.9 ± 3.1 | 55 (56) | Conjunctivitis | |
| 33 | Chiu et al. (2020) [46] | Case report | 1 | 10 | 1 (NR) | Conjunctivitis | |
| 34 | Blumfield et al. (2021) [47] | Case series | 14 | 10.8 ± 5.8/ 9.3 (8.8) | 8 (57) | Conjunctivitis | |
| 35 | Blondiaux et al. (2020) [48] | Case series | 4 | 10 ± 2.8 | 2 (50) | Conjunctivitis | |
| 36 | Al Ameer et al. (2020) [49] | Case report | 1 | 13 | 1 (NR) | Conjunctivitis |
Abbreviations: Code, article code; N, total number of participants; N’, total number of participants with ocular manifestations; %, percentage; y, years; SD, standard deviation; IQR, interquartile range; NM, Not Mentioned; NR, Not Relevant.
Missing data that were received from the corresponding authors were recorded. Data were analyzed using Excel 2016 (Microsoft Inc., Redmond, WA, USA). The total number and mean ± SD or median (IQR) age of the participants, frequency and percentage of ocular manifestations, and patients with ocular manifestations were calculated.
RESULTS
A total of 1,192 records were electronically identified, and seven papers were extracted from the reference lists of the eligible articles. After removing 104 duplicate records using the EndNote software, the titles and abstracts of 1,095 records were screened. Among these, 1,028 studies were excluded due to the reasons outlined in Figure 1. Finally, the reviewers independently assessed the eligibility of 67 articles. Thirty-six papers met our inclusion criteria, and 31 were excluded due to the reasons outlined in Figure 1. The data extracted from these 36 articles are listed in Table 2 [6, 11-18, 23-49].
Eligible articles were categorized into two subgroups: acute or sub-acute presentation of ocular manifestations. Nine articles [11-18, 23] reported acute ocular manifestations; in these studies, 72 (15.5%) out of 463 pediatric patients with COVID-19 had ocular manifestations. Except for one patient with central retinal vein occlusion [14] and another with photophobia and diplopia associated with meningoencephalitis [12], the acute ocular symptoms observed following a viral infection included conjunctivitis, conjunctival discharge, conjunctival hyperemia, and eyelid dermatitis. Twenty-seven [6, 24-49] articles reported cases of post-COVID-19 MIS-C, in which 469 (52.4%) out of 895 pediatric patients had ocular manifestations, and non-purulent conjunctivitis was the only ocular manifestation documented in these articles (Table 2).
DISCUSSION
According to this systematic review, acute and sub-acute ocular manifestations were reported in 15.5% of pediatric patients with COVID-19 and 52.4% of patients with post-COVID-19 MIS-C, respectively. Most of the patients in both subgroups had conjunctivitis [6, 11, 13, 15-18, 23-49], although two patients experienced severe ocular manifestations such as central retinal vein occlusion and diplopia [12, 14]. In adults, acute ocular signs and symptoms such as conjunctival hyperemia, epiphora, increased secretion, chemosis, follicular conjunctivitis, episcleritis, photophobia, itchiness, burning sensation, gritty feeling, blurred vision, and various posterior segment manifestations such as central retinal vein occlusion, have been reported [5, 50-52].
In a meta-analysis, conjunctivitis was the most common acute ophthalmic manifestation of COVID-19 in adults [53]. In this systematic review, 72 out of 463 pediatric patients with COVID-19 had acute ocular manifestations, mainly conjunctivitis. Therefore, similar to adults, conjunctivitis is the most common ophthalmic manifestation in pediatric patients with COVID-19. Furthermore, conjunctivitis was the only ocular manifestation reported in almost half of the patients with MIS-C in the studies included in this review.
The WHO has detailed the MIS-C diagnostic requirements and specified bilateral non-purulent conjunctivitis as one of its diagnostic criteria [54]. Considering the reported mortality following MIS-C, which may be higher in middle- and low-income countries compared with high-income countries [55], monitoring the accompanying symptoms of this disease for early intervention can be lifesaving. Pediatricians and health workers must remain vigilant for early detection of the signs of this potentially fatal post-COVID-19 inflammatory syndrome [56].
MIS-C is a Kawasaki-like disease; however, its definition and precise diagnostic criteria have not been finalized [56]. In this systematic review, we noted that half of the patients with MISC-C had conjunctivitis, and conjunctivitis has been reported in > 90% of pediatric patients with Kawasaki disease [57]. MIS-C as a post-COVID-19 inflammatory complication in pediatric patients should be investigated separately, and Kawasaki-like disease may not be a good definition for this condition. MIS-C can cause life-threatening cardiac complications [34], and pediatricians should consider conjunctivitis a key presentation of suspected MIS-C in pediatric patients with COVID-19.
In this systematic review, we reported the prevalence of acute or subacute ocular manifestations in pediatric patients with COVID-19. Our report may be a good estimation of the ocular manifestations of COVID-19 in this age group. The most important limitation of our review was the lack of response from the corresponding authors of some original articles, which resulted in the removal of those studies from the final assessment. Another limitation was the lack of well-designed original studies in almost all retrieved records on this topic. We only searched the PubMed/MEDLINE database; future systematic reviews that include more databases might be able to include more studies or find original studies with a strong design to reach more robust conclusions. Future cohort studies on pediatric patients with laboratory-confirmed COVID-19 and a long follow-up period could report on more ocular manifestations or identify a definite association between ocular signs and symptoms and acute COVID-19, or side effects of post-COVID-19 condition such as MIS-C.
CONCLUSIONS
Ocular manifestations have been reported in less than one-fifth of pediatric patients with acute COVID-19. Furthermore, conjunctivitis is an important ocular manifestation that was present in half of the patients with MIS-C and could be missed due to its non-purulent nature. During the COVID-19 pandemic, we propose complete investigations of all children with fever and conjunctivitis to identify MIS-C. Blood investigation for inflammation markers and cardiac assessment may also be needed in such patients.
ETHICAL DECLARATIONS
Ethical approval:
The protocol of this systematic review was peer-reviewed and registered at the Endocrinology and Metabolism Research Institute of Tehran University of Medical Science and received ethical approval (ethical code: IR.TUMS.EMRI.REC.1399.063).
Conflict of interest:
None.
FUNDING
None.
ACKNOWLEDGEMENTS
I would like to thank Dr. Reza Gharebaghi as the second independent reviewer for the screening of retrieved records, assessing the quality and eligibility of selected articles, and assisting in data extraction and management, as well as Dr. Maryam Nadi for her expert opinion.
References
- 1.Allen WE, Altae-Tran H, Briggs J, Jin X, McGee G, Shi A, et al. Population-scale longitudinal mapping of COVID-19 symptoms, behaviour and testing. Nat Hum Behav. 2020;4(9):972–982. doi: 10.1038/s41562-020-00944-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mizrahi B, Shilo S, Rossman H, Kalkstein N, Marcus K, Barer Y, et al. Longitudinal symptom dynamics of COVID-19 infection. Nat Commun. 2020;11(1):6208 . doi: 10.1038/s41467-020-20053-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ling XC, Kang EY, Lin JY, Chen HC, Lai CC, Ma DH, et al. Ocular manifestation, comorbidities, and detection of severe acute respiratory syndrome-coronavirus 2 from conjunctiva in coronavirus disease 2019: A systematic review and meta-analysis. Taiwan J Ophthalmol. 2020;10(3):153–166. doi: 10.4103/tjo.tjo_53_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belot A, Antona D, Renolleau S, Javouhey E, Hentgen V, Angoulvant F, et al. SARS-CoV-2-related paediatric inflammatory multisystem syndrome, an epidemiological study, France, 1 March to 17 May 2020. Euro Surveill. 2020;25(22):2001010 . doi: 10.2807/1560-7917.ES.2020.25.22.2001010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bostanci Ceran B, Ozates S. Ocular manifestations of coronavirus disease 2019. Graefes Arch Clin Exp Ophthalmol. 2020;258(9):1959–1963. doi: 10.1007/s00417-020-04777-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dufort EM, Koumans EH, Chow EJ, Rosenthal EM, Muse A, Rowlands J, et al. Multisystem Inflammatory Syndrome in Children in New York State. N Engl J Med. 2020;383(4):347–58. doi: 10.1056/NEJMoa2021756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed M, Advani S, Moreira A, Zoretic S, Martinez J, Chorath K, et al. Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine. 2020;26:100527. doi: 10.1016/j.eclinm.2020.100527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baradaran A, Malek A, Moazzen N, Abbasi Shaye Z. COVID-19 Associated Multisystem Inflammatory Syndrome: A Systematic Review and Meta-analysis. Iran J Allergy Asthma Immunol. 2020;19(6):570–588. doi: 10.18502/ijaai.v19i6.4927. [DOI] [PubMed] [Google Scholar]
- 9.Kaushik A, Gupta S, Sood M, Sharma S, Verma S. A Systematic Review of Multisystem Inflammatory Syndrome in Children Associated With SARS-CoV-2 Infection. Pediatr Infect Dis J. 2020;39(11):e340–e346. doi: 10.1097/INF.0000000000002888. [DOI] [PubMed] [Google Scholar]
- 10.Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J, et al. Multi-system inflammatory syndrome in children & adolescents (MIS-C): A systematic review of clinical features and presentation. Paediatr Respir Rev. 2021;38:51–57. doi: 10.1016/j.prrv.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garazzino S, Montagnani C, Donà D, Meini A, Felici E, Vergine G, et al. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Euro Surveill. 2020;25(18):2000600 . doi: 10.2807/1560-7917.ES.2020.25.18.2000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yousefi K, Poorbarat S, Abasi Z, Rahimi S, Khakshour A. Viral Meningitis Associated With COVID-19 in a 9-year-old Child: A Case Report. Pediatr Infect Dis J. 2021;40(2):e87–e98. doi: 10.1097/INF.0000000000002979. [DOI] [PubMed] [Google Scholar]
- 13.Wu P, Liang L, Chen C, Nie S. A child confirmed COVID-19 with only symptoms of conjunctivitis and eyelid dermatitis. Graefes Arch Clin Exp Ophthalmol. 2020;258(7):1565–1566. doi: 10.1007/s00417-020-04708-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walinjkar JA, Makhija SC, Sharma HR, Morekar SR, Natarajan S. Central retinal vein occlusion with COVID-19 infection as the presumptive etiology. Indian J Ophthalmol. 2020;68(11):2572–2574. doi: 10.4103/ijo.IJO_2575_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valente P, Iarossi G, Federici M, Petroni S, Palma P, Cotugno N, et al. Ocular manifestations and viral shedding in tears of pediatric patients with coronavirus disease 2019: a preliminary report. J AAPOS. 2020;24(4):212–215. doi: 10.1016/j.jaapos.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Storch-de-Gracia P, Leoz-Gordillo I, Andina D, Flores P, Villalobos E, Escalada-Pellitero S, et al. Espectro clínico y factores de riesgo de enfermedad complicada en niños ingresados con infección por SARS-CoV-2 [Clinical spectrum and risk factors for complicated disease course in children admitted with SARS-CoV-2 infection] An Pediatr (Engl Ed). 2020;93(5):323–333. doi: 10.1016/j.anpedi.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma N, Li P, Wang X, Yu Y, Tan X, Chen P, et al. Ocular Manifestations and Clinical Characteristics of Children With Laboratory-Confirmed COVID-19 in Wuhan, China. JAMA Ophthalmol. 2020;138(10):1079–1086. doi: 10.1001/jamaophthalmol.2020.3690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke RM, Killerby ME, Newton S, Ashworth CE, Berns AL, Brennan S, et al. Symptom Profiles of a Convenience Sample of Patients with COVID-19 - United States, January-April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):904–908. doi: 10.15585/mmwr.mm6928a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Wiley Online Library; 2008. [Google Scholar]
- 20.Higgins J, Churchill R, Lasserson T, Chandler J, Tovey D. Update from the methodological Expectations of Cochrane Intervention reviews (MECIR) project. Cochrane methods. 2012;2(3) [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. ‘Living guidance for clinical management of COVID-19’. 2021. [Accessed: November 17, 2021]. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2.
- 23.Ya Y, Yanping S, Ming Y, Cheng H, Xiao C, Juan Y, et al. Novel coronavirus pmneumonia combined with conjunctivitis: three cases report. Chin J Exp Ophthalmol. 2020;38:242–4. [Google Scholar]
- 24.Whittaker E, Bamford A, Kenny J, Kaforou M, Jones CE, Shah P, et al. PIMS-TS Study Group and EUCLIDS and PERFORM Consortia Clinical Characteristics of 58 Children With a Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2. JAMA. 2020;324(3):259–269. doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395(10239):1771–1778. doi: 10.1016/S0140-6736(20)31103-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. 2020;369:m2094. doi: 10.1136/bmj.m2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tam H, El Tal T, Go E, Yeung RSM. Pediatric inflammatory multisystem syndrome temporally associated with COVID-19: a spectrum of diseases with many names. CMAJ. 2020;192(38):E1093–E1096. doi: 10.1503/cmaj.201600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spencer R, Closson RC, Gorelik M, Boneparth AD, Hough RF, Acker KP, et al. COVID-19 Inflammatory Syndrome With Clinical Features Resembling Kawasaki Disease. Pediatrics. 2020 Sep;146(3):e20201845 . doi: 10.1542/peds.2020-1845. [DOI] [PubMed] [Google Scholar]
- 29.Schneider DT, Pütz-Dolderer J, Berrang J. Pediatric Multisystemic Inflammatory Syndrome Associated With SARS-CoV-2 Infection. Dtsch Arztebl Int. 2020;117(25):431. doi: 10.3238/arztebl.2020.0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395(10237):1607–1608. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raut S, Roychowdhoury S, Bhakta S, Sarkar M, Nandi M. Incomplete Kawasaki Disease as Presentation of COVID-19 Infection in an Infant: A Case Report. J Trop Pediatr. 2021;67(3):fmaa047. doi: 10.1093/tropej/fmaa047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pouletty M, Borocco C, Ouldali N, Caseris M, Basmaci R, Lachaume N, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann Rheum Dis. 2020;79(8):999–1006. doi: 10.1136/annrheumdis-2020-217960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nelson C, Ishimine P, Hayden SR, Correia M, Wardi G. Multisystem Inflammatory Syndrome in Children (MIS-C) in an Adolescent that Developed Coronary Aneurysms: A Case Report and Review of the Literature. J Emerg Med. 2020;59(5):699–704. doi: 10.1016/j.jemermed.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mamishi S, Movahedi Z, Mohammadi M, Ziaee V, Khodabandeh M, Abdolsalehi MR, et al. Multisystem inflammatory syndrome associated with SARS-CoV-2 infection in 45 children: a first report from Iran. Epidemiol Infect. 2020;148:e196. doi: 10.1017/S095026882000196X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Licciardi F, Pruccoli G, Denina M, Parodi E, Taglietto M, Rosati S, et al. SARS-CoV-2-Induced Kawasaki-Like Hyperinflammatory Syndrome: A Novel COVID Phenotype in Children. Pediatrics. 2020;146(2):e20201711 . doi: 10.1542/peds.2020-1711. [DOI] [PubMed] [Google Scholar]
- 36.Lee WS, Margolskee E. Leukoerythroblastosis and plasmacytoid lymphocytes in a child with SARS-CoV-2-associated multisystem inflammatory syndrome. Blood. 2020;136(7):914. doi: 10.1182/blood.2020007132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vukomanovic V, Krasic S, Minic P, Petrovic G, Nesic D, Paripovic A, et al. Kawasaki-like disease and acute myocarditis in the SARS-CoV-2 pandemic - reports of three adolescents. Bosn J Basic Med Sci. 2021;21(2):252. doi: 10.17305/bjbms.2020.5037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim H, Shim JY, Ko JH, Yang A, Shim JW, Kim DS, et al. Multisystem Inflammatory Syndrome in Children Related to COVID-19: the First Case in Korea. J Korean Med Sci. 2020;35(43) doi: 10.3346/jkms.2020.35.e391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khan I, Sarwar A, Ahmed Z. Atypical Case of COVID-19 Associated Kawasaki Disease in an Eight-Year-Old Pakistani Boy. Cureus. 2020;12(9):e10670. doi: 10.7759/cureus.10670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kest H, Kaushik A, DeBruin W, Colletti M, Goldberg D. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with 2019 Novel Coronavirus (SARS-CoV-2) Infection. Case Rep Pediatr. 2020;2020:8875987. doi: 10.1155/2020/8875987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heidemann SM, Tilford B, Bauerfeld C, Martin A, Garcia RU, Yagiela L, et al. Three Cases of Pediatric Multisystem Inflammatory Syndrome Associated with COVID-19 Due to SARS-CoV-2. Am J Case Rep. 2020;21:e925779. doi: 10.12659/AJCR.925779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grimaud M, Starck J, Levy M, Marais C, Chareyre J, Khraiche D, et al. Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann Intensive Care. 2020;10(1):69 . doi: 10.1186/s13613-020-00690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, et al. COVID-19-Associated Multisystem Inflammatory Syndrome in Children - United States, March-July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1074–1080. doi: 10.15585/mmwr.mm6932e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Felsenstein S, Willis E, Lythgoe H, McCann L, Cleary A, Mahmood K, et al. Presentation, Treatment Response and Short-Term Outcomes in Paediatric Multisystem Inflammatory Syndrome Temporally Associated with SARS-CoV-2 (PIMS-TS) J Clin Med. 2020;9(10):3293. doi: 10.3390/jcm9103293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Falah NU, Hashmi S, Ahmed Z, Jaan A, Akhtar A, Khalid F, et al. Kawasaki Disease-Like Features in 10 Pediatric COVID-19 Cases: A Retrospective Study. Cureus. 2020;12(10):e11035. doi: 10.7759/cureus.11035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chiu JS, Lahoud-Rahme M, Schaffer D, Cohen A, Samuels-Kalow M. Kawasaki Disease Features and Myocarditis in a Patient with COVID-19. Pediatr Cardiol. 2020;41(7):1526–1528. doi: 10.1007/s00246-020-02393-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blumfield E, Levin TL, Kurian J, Lee EY, Liszewski MC. Imaging Findings in Multisystem Inflammatory Syndrome in Children (MIS-C) Associated With Coronavirus Disease (COVID-19) AJR Am J Roentgenol. 2021;216(2):507–517. doi: 10.2214/AJR.20.24032. [DOI] [PubMed] [Google Scholar]
- 48.Blondiaux E, Parisot P, Redheuil A, Tzaroukian L, Levy Y, Sileo C, et al. Cardiac MRI in Children with Multisystem Inflammatory Syndrome Associated with COVID-19. Radiology. 2020;297(3):E283–E288. doi: 10.1148/radiol.2020202288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al Ameer HH, AlKadhem SM, Busaleh F, AlKhwaitm S, Llaguno MBB. Multisystem Inflammatory Syndrome in Children Temporally Related to COVID-19: A Case Report From Saudi Arabia. Cureus. 2020;12(9):e10589. doi: 10.7759/cureus.10589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen L, Deng C, Chen X, Zhang X, Chen B, Yu H, et al. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: a cross-sectional study. Acta Ophthalmol. 2020;98(8):e951–e959. doi: 10.1111/aos.14472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lawrenson JG, Buckley RJ. COVID-19 and the eye. Ophthalmic Physiol Opt. 2020;40(4):383–388. doi: 10.1111/opo.12708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sanjay S, Agrawal S, Jayadev C, Kawali A, Gowda PB, Shetty R, et al. Posterior segment manifestations and imaging features post-COVID-19. Medical hypothesis discovery and innovation in ophthalmology. 2021;10(3):95–106. doi: 10.51329/mehdiophthal1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Al-Namaeh M. COVID-19 and conjunctivitis: a meta-analysis. Ther Adv Ophthalmol. 2021;13:25158414211003368. doi: 10.1177/25158414211003368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Health Organization. Multisystem inflammatory syndrome in children and adolescents with COVID-19. 2020. [Accessed: November 17, 2021]. Available at: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19.
- 55.Acevedo L, Piñeres-Olave BE, Niño-Serna LF, Vega LM, Gomez IJA, Chacón S, et al. Mortality and clinical characteristics of multisystem inflammatory syndrome in children (MIS-C) associated with covid-19 in critically ill patients: an observational multicenter study (MISCO study) BMC Pediatr. 2021;21(1):516 . doi: 10.1186/s12887-021-02974-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berardicurti O, Conforti A, Ruscitti P, Cipriani P, Giacomelli R. The wide spectrum of Kawasaki-like disease associated with SARS-CoV-2 infection. Expert Rev Clin Immunol. 2020;16(12):1205–1215. doi: 10.1080/1744666X.2021.1847643. [DOI] [PubMed] [Google Scholar]
- 57.Son MBF, Newburger JW. Kawasaki Disease. Pediatr Rev. 2018;39(2):78–90. doi: 10.1542/pir.2016-0182. [DOI] [PubMed] [Google Scholar]