Abstract
Background
Malnutrition is a frequent problem in oncology and is associated with reduced response to cancer treatments, increased drug-related toxicity, higher rates of clinical complications, reduced quality of life (QoL) and worse prognosis. Guidelines on clinical nutrition in oncology emphasise the usefulness of early assessment of nutritional status for a prompt identification of malnutrition and the implementation of effective interventions, but no real-world clinical data are available on the adequate management of nutritional support in patients with cancer in Italy.
Methods and analysis
This is an observational, longitudinal, multicentre registry of patients with a new diagnosis of cancer or metastatic disease, candidates for active treatment. They will be identified in at least 15 Italian oncological centres, members of the Alliance Against Cancer Working Group ‘Survivorship Care and Nutritional Support’. At least 1500 patients with cancer are expected to be enrolled each year. Detailed clinical and nutritional data will be collected by oncologists and clinical nutritionists during the visits foreseen in the clinical practice, through an ad hoc developed digital platform (e-Nutracare). The effects of malnutrition and nutritional support—at diagnosis and during follow-up—on overall survival and progression-free survival, as well as on patients’ symptoms and QoL, will be investigated.
Ethics and dissemination
The study protocol was approved by the Ethics Committee of the Fondazione IRCCS Policlinico San Matteo, Pavia, Italy and from the Ethics Committees of all other participating centres. An informed consent will be obtained from each patient enrolled in the study. Study findings will be disseminated through peer-reviewed journals, conferences and patients with cancer or professional associations. The registry will allow a better monitoring of the nutritional status of patients with cancer, promoting adequate and sustainable nutritional support, with the ultimate goal of improving the care and prognosis of these patients.
Keywords: quality of life, nutritional support, registries
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The study will allow the implementation of the first Italian, real-world register for detecting and monitoring malnutrition in patients with cancer.
The study will make use of an ad hoc developed digital platform for data collection, which could be proposed and extended in the near future to other oncological centres within the national territory.
The study will allow a more appropriate evaluation and monitoring of cancer patients’ nutritional status of, promoting adequate and sustainable nutritional support, with the ultimate goal of improving the quality of care and prognosis.
Study limitations consist in the observational design, which will not allow to compare the efficacy of personalised nutritional support interventions in specific oncological diseases.
Introduction
Malnutrition is a frequent problem in oncology and is associated with a reduced response to cancer treatment, an increase in treatment-related toxicity, higher occurrence of clinical symptoms and complications, impaired quality of life (QoL), and worse overall prognosis.1–6 Different causes are linked to this condition, including factors such as cancer site and metastatic localisations, and the deregulation of systemic inflammation pathways.5 Medical treatments and surgery could also be responsible for nutritional derangements, through the increase of basal caloric requirements and the occurrence of symptoms that negatively impact on food intake and nutrient absorption (eg, anorexia, mucositis, dysphagia, smell alterations, taste alterations, xerostomia, vomiting, nausea, diarrhoea). Taken together, these factors impair the maintenance of functional body composition.3–5 7
Sarcopenia (ie, the loss of skeletal muscle (SM) and strength) is the main issue which contributes to functional deterioration in patients with cancer.8 In particular, it has been observed that handgrip strength assessment is a reliable survival predictor associated with body composition variations, being also a good indicator of functional capacities in chronic diseases.9 In oncology, low handgrip strength levels are associated with fatigue, impaired QoL, treatment-related toxicity and higher mortality.10 11
National and international guidelines on clinical nutrition in oncology—including those issued by the Italian Ministry of Health in 201712—underline the utility of early evaluation of nutritional status in patients with cancer and of a prompt and appropriate nutritional support, whenever indicated, in order to prevent or treat malnutrition, improve patients’ clinical outcomes and QoL, and increase the efficacy and tolerability of cancer treatments.3–5 12 Only an early and adequate nutritional support can effectively prevent or treat malnutrition and support patients with cancer during their entire illness trajectory.
Despite these indications, there are several critical issues related to the quality of nutritional care in oncology, and no reliable data are available on the current implementation of adequate nutritional support in patients with cancer in Italy. Nowadays, only real-world data collected by administrative databases are available in the context of nutrition in oncology, but these have various inherent weaknesses, which somehow limit the possibility to interpret their evidence from a clinical point of view.13 14 Therefore, it is of foremost importance to start collecting real-world clinical data on malnutrition in oncology, in order to strengthen the evidence and concretely improve nutritional care practices.
Based on these premises, the study ‘Italian Registry of Malnutrition in Oncology’ has been elaborated in collaboration with the oncological centres that joined the Working Group (WG) ‘Survivorship Care and Nutritional Support’ of Alliance Against Cancer (Alleanza Contro il Cancro, ACC). This study aims to set up a digital register of newly diagnosed patients with cancer, in order to monitor their nutritional status and explore the implications of their nutritional support. This will represent the first national, real-world register for detecting and monitoring malnutrition in patients with cancer and will allow the creation of a multicentric, longitudinal cohort of oncological patients to be used for specific analyses.
Methods and analysis
Study design
This is a multicentric, longitudinal, observational registry of newly diagnosed patients with cancer, candidates for active treatment. Detailed clinical and nutritional data will be collected by oncologists and clinical nutritionists during the visits foreseen in the clinical practice, through the ad hoc developed digital platform, e-Nutracare. The initial duration of the study is of 3 years (between October 2022 and September 2025). Patients’ enrolment and follow-up will last for all the duration of the study. However, for the primary and secondary endpoints of the study only patients enrolled during the first year and followed up for another year will be analysed.
Study subjects
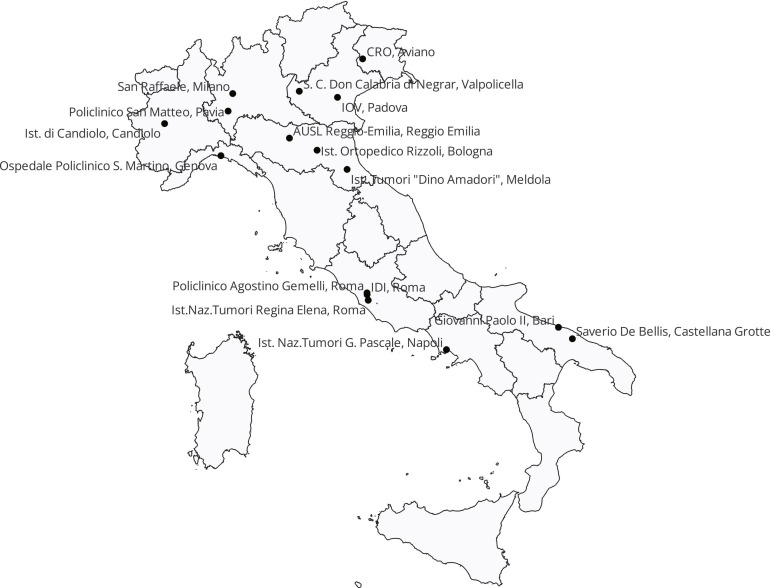
Individuals enrolled in the study will be all consecutive newly diagnosed or treated patients with cancer, candidate for active treatment identified in a least 15 Italian IRCCS members of the ACC WG ‘Survivorship Care and Nutritional Support’ (figure 1). They should be aged 18 years or more, had a new diagnosis of selected cancer sites (ie, head and neck, oesophagus/stomach, colorectal, hepatobiliary, pancreatic, lung, prostate, other urogenital, breast, gynaecological, soft tissue sarcomas and melanoma), or a new diagnosis of metastatic disease, be eligible for active treatment, and provide informed consent to participate in the registry. Individuals with impossibility to undertake the expected measurements or to guarantee the attendance of the follow-up visits will be excluded.
Figure 1.
Participating centres.
The digital platform e-Nutracare
The registry data will be collected through e-Nutracare (OPT S.r.l., Milan, Italy), a digital, web-based platform specifically designed to provide the participating centres with the necessary resources for data collection. The platform is accessible via an internet browser, without the installation of application modules. It will enable both real-time data collection during routine clinical practice visits and transmission of information to various health professionals who participate in the study, thus facilitating their work, involvement and collaboration.
Data will be entered in single data entry. In the electronic database, patients will be identified through a unique identification code to preserve their anonymity. Separately, a list of codes and corresponding identification of patients’ data will be kept. Data completeness and plausibility will be remotely assessed. Once the corrections have been completed (‘cleaned’ database), the database will be frozen (‘closed’ database). Access to the application by users will take place only in HTTPS, therefore the information will be always transmitted through an encrypted channel. Data correction after the database closure will have to be jointly agreed by the research manager, the statistician and the data manager and appropriately documented. The number of screened patients, of eligible patients and the reason for non-enrolment will also be documented.
Assessments
Medical oncologists will collect baseline data at the first patient’s visit and will carry out subsequent assessments during the oncological scheduled visits, according to treatment and follow-up protocols envisaged for these patients in the clinical practice. All collected variables, resumed in box 1, will include:
Box 1. Collected variables.
Age, sex, cancer diagnosis, tumour stage, comorbidities.
Actual body weight, height, BMI, weight loss in the previous 6 months months, NRS 2002 score.
Body composition parameters using BIVA (PhA, SPhA, FFM) and CT (SM).
Oncological treatment, severe adverse effects (grade ≥3 CTCAE).
Performance status (ECOG Scale).
Symptoms (ESAS Scale), QoL (Short Form 12).
Disease outcome (progression or death).
BIVA, bioelectrical impedance vector analysis; BMI, body mass index; CTCAE, Common Terminology Criteria for Adverse Events; ECOG, Eastern Cooperative Oncology Group; ESAS, Edmonton Symptom Assessment Scale; FFM, fat free mass; NRS 2002, Nutritional Risk Screening 2002; PhA, phase angle; QoL, quality of life; SM, skeletal muscle; SPhA, standardised phase angle.
Demographic, anamnestic and clinical data (such as age, sex, cancer type, tumour stage and comorbidities).
Oncological treatments and related severe (grade≥3) adverse effects or complications, according to Common Terminology Criteria for Adverse Events (CTCAE V.5.0).15
Anthropometric measurements (actual body weight, height, body mass index, weight and weight trend in the previous 6 months).
Performance status according to the Eastern Cooperative Oncology Group Performance Status Scale.16
Patients’ symptoms by the Edmonton Symptom Assessment Scale.17
QoL assessed using the Short Form 12 questionnaire18
Disease outcomes (as progression or death).
Using anthropometric and nutritional data collected, the Nutritional Risk Screening 2002 (NRS 2002) will be calculated.5 19 The NRS 2002 is a tool developed by the European Society of Clinical Nutrition and Metabolism, which is currently used to identify patients at risk of surgical complications and mortality and has been recently proposed as a useful tool for indicating the need of an early nutritional intervention in patients with cancer.20–22
Patients at risk of malnutrition (NRS 2002 score≥3) will be referred for a nutritional examination. Clinical nutritionists will collect the following information:
Detailed patient’ nutritional requirements, nutritional support provided and adherence to the Mediterranean Diet using a validated food frequency questionnaire.23
Body composition parameters obtained throughout scans of CT at third level of lumbar (L3) or cervical (C3) vertebra as SM and bioelectrical impedance vector analysis, as phase angle (PhA), standardised phase angle (SPhA) and fat-free mass. The measurements will be based on the availability of instrumentation at the different participating centres.
Every effort will be made to ensure the accuracy of patients monitoring and to avoid patients’ loss at follow-up.
Study endpoints
Study endpoints are described in box 2. The primary endpoint will be 1-year overall survival (OS) and progression-free survival (PFS) according to patients’ risk of malnutrition (defined as NRS 2002 score≥3) on diagnosis.
Box 2. Study endpoints.
Primary endpoint
To assess 1-year OS and PFS according to the NRS 2002 cut-off score ≥3 on diagnosis.
Secondary endpoints
To assess 1-year OS and PFS according to the NRS 2002 cut-off score ≥3 on diagnosis of metastatic disease.
To assess 1-year OS and PFS according to the NRS 2002 cut-off score ≥3 on diagnosis in the different selected cancer types.
To assess 1-year OS and PFS according to the changes of NRS 2002 score and body weight during the follow-up.
Explorative endpoints
To assess 1-year OS and PFS according to the type and timing of nutritional support provided.
To assess 1-year OS and PFS according to the body composition measured with CT scan and BIVA methods at diagnosis and during follow-up.
To assess the percentage of patients with severe toxicities oncological and discontinuations or delays of treatment according to the NRS 2002 cut-off scores and body composition evaluated at diagnosis and during follow-up.
To explore the correlations between NRS 2002 scores, body composition parameters, type and timing of nutritional support, QoL, symptoms during follow-up.
BIVA, bioelectrical impedance vector analysis; NRS 2002, Nutritional Risk Screening 2002; OS, overall survival; PFS, progression-free survival; QOL, quality of life.
Secondary endpoints will be 1-year OS and PFS according to malnutrition risk on diagnosis in relation to cancer type, disease stage, nutritional risk changes and body weight changes during follow-up (at 3, 6, 9, 12 months).
As explorative endpoints, we will investigate 1-year OS and PFS according to the type and timing of nutritional support provided and body composition as well as the rate of severe toxicities (grade III/IV) and discontinuation or delay of treatment according to NRS 2002 score and body composition. Furthermore, we will explore the correlations between NRS 2002 score, body composition parameters, type and timing of nutritional support, QoL, symptoms and toxicities during follow-up.
Statistical methods and sample size
The main characteristics of the enrolled patients at baseline will be summarised with appropriate descriptive statistics, such as absolute and relative frequencies for categorical variables, and mean or medians with corresponding precision indices (SD or IQR) for continuous variables.
For the associations of NRS 2022 score and other nutritional factors with OS or PFS, we will use survival analysis methods, such as rate calculation, Kaplan-Meier curves and logrank test. In addition, Cox models will be used to calculate the HR, and corresponding 95% CI, for patients at high risk of malnutrition vs low-risk patients and other nutritional factors. HRs will be computed adjusting for potential confounding factors, including age, sex, tumour characteristics, stage, comorbidities and cancer treatment. For explorative endpoints, we will use logistic regression models to calculate the (crude and adjusted) OR and corresponding 95% CI of severe toxicity and interruption/delay in cancer treatments, and multiple regression methods for the calculation of crude and adjusted associations.
All analyses will be conducted using the SAS software V.9.4 (SAS Institute).
Considering that each centre will be able to enrol between 30 and 300 patients/year (depending on their patients’ load), we expect to enrol at least 1500 patients with cancer/year.
Since the average 1-year survival rate for the two sexes combined is 75%24 and about 30% of patients are at risk of malnutrition (NRS 2002 score≥3),20 we estimate an HR of 12-month mortality of at least 1.36 for malnourished patients, with a power of 80% and an alpha error of 5%.
Patient and public involvement
The registry has been developed in collaboration with Italian Federation of Volunteer-based Cancer Organisations in order to delineate the better way to improve cancer patients’ involvement in the registry.
Ethics and dissemination
The study will be conducted in accordance with the good clinical practice rules, the Declaration of Helsinki, and current national and European laws and regulations. The study protocol was approved by the Ethics Committee of the Fondazione IRCCS Policlinico San Matteo, Pavia, Italy (5 July 2022; prot. N. 0035571/22) and from the ethics committees of all other participating centres. An informed consent will be obtained from each patient enrolled in the study. At any time, patients will have the right to withdraw their consent without modifying their current or future care. The progress of the study will be shared with the patients’ general practitioners.
The results of the study will be presented at local, national and international medical conferences. The findings will be published in peer-reviewed medical/scientific journals and made open-access on acceptance. Information may also be disseminated to patients with cancer and professional associations and the general population via public engagement and community outreach programmes.
Discussion
Malnutrition in oncology still represents an overlooked problem, which negatively affects clinical outcomes.4 6 13 25 An altered nutritional status brings more frequently to drug-related toxicities and requires suspending or delay anticancer therapies, resulting in reduced response rates and worse prognosis.2 Therefore, an early nutritional support since treatment beginning is crucial. The target is not only to maintain or improve the nutritional status by providing energy and proteins and fully satisfy nutritional requirements, but also effectively impact on clinical outcomes by enhancing the adherence to anticancer treatment.
The global trend of research in the field of nutrition in cancer is gradually increasing.26 To date, there is evidence that an individualised nutritional support reduces the risk of mortality and improves QoL in patients with cancer at malnutritional risk.27 Moreover, nutritional support for oncology patients is a low-cost intervention compared with other cares28 and it does not require additional costs for the healthcare system.29 However, the impact on survival still requires confirmation as reliable real-world data are lacking.
This study will allow us to collect real-world clinical data on malnutrition in Italy. So, it will be possible to improve the strength of evidence on the impact of malnutrition and nutritional support, and to develop quality improvement programmes, which help both healthcare professionals to ameliorate nutritional care practices and institutions to allocate adequate resources to this issue.30 Moreover, the creation of a data registry allows us to study the cost-effectiveness of nutritional support on a broader scale.31
The innovative aspect of this study is the implementation of the first Italian real-world register for detecting malnutrition and monitoring nutritional status in patients with cancer. This will allow the creation of a multicentric, longitudinal cohort of oncological patients for further research in the field of nutrition in oncology. Furthermore, it will permit a better monitoring of the nutritional status of patients with cancer, fostering an appropriate and sustainable nutritional support, with the goal to improve their care, in agreement with the most recent evidence-based guidelines and recommendations.3–5 12 The idea is to build a model for a standardised digital platform to monitor the nutritional status of patients with cancer. In the near future, the registry could be extended to all the other oncological centres within the national territory.
Supplementary Material
Footnotes
Correction notice: This article has been corrected since it was published. The given names and surnames of the collaborators have been corrected.
Collaborators: IRMO collaborators are the following: Riccardo Caccialanza, Fondazione IRCCS Policlinico San Matteo Pavia, Pavia, Italy. Renato Cannizzaro, Centro di Riferimento Oncologico, Aviano (PN), Italy. Valentina Casalone, Istituto di Candiolo - Fondazione del Piemonte per l'Oncologia - IRCCS, Candiolo (TO), Italy. Rosalisa Cici, IRCCS Saverio De Bellis, Castellana Grotte (BA), Italy. Francesco De Lorenzo, Italian Federation of Volunteer-based Cancer Organizations, Rome, Italy. Giovanni De Pergola, IRCCS Saverio De Bellis, Castellana Grotte (BA), Italy. Teresa Di Lauro, Istituto Nazionale Tumori IRCCS Fondazione G. Pascale, Napoli, Italy. Cristina Fortes, IDI IRCCS - Istituto Dermopatico dell'Immacolata, Roma, Italy. Stefania Gori, IRCCS Sacro Cuore Don Calabria di Negrar, Valpolicella (VR), Italy. Iannelli Elisabetta, Italian Federation of Volunteer-based Cancer Organizations, Rome, Italy. Toni Ibrahim, Istituto Ortopedico Rizzoli, Bologna, Italy. Alessandra Longhi, Istituto Ortopedico Rizzoli, Bologna, Italy. Cristina Mele Maria, Policlinico Universitario Agostino Gemelli, Roma, Italy. Roberto Mele, IRCCS Ospedale San Raffaele, Milano, Italy. Filippo Montemurro, Istituto di Candiolo - Fondazione del Piemonte per l'Oncologia - IRCCS, Candiolo (TO), Italy. Teresa Nardi Maria, IOV Istituto Oncologico Veneto, Padova, Italy. Paolo Pedrazzoli, Fondazione IRCCS Policlinico San Matteo Pavia, Pavia, Italy. Debora Pezzuolo, AUSL IRCCS Reggio-Emilia, Italy. Carmine Pinto, AUSL IRCCS Reggio-Emilia, Italy. Sandro Pignata, Istituto Nazionale Tumori IRCCS Fondazione G. Pascale, Napoli, Italy. Carmelo Pozzo, Policlinico Universitario Agostino Gemelli, Roma, Italy. Lupe Sanchez Mete, Istituto Nazionale Tumori Regina Elena, Roma, Italy. Patrizia Serra, Istituto Romagnolo per lo Studio dei Tumori "Dino Amadori" IRCCS, Meldola (FC), Italy. Guseppe Sukkar Samir, IRCCS Ospedale Policlinico San Martino, Genova, Italy. Marco Tonello, IOV Istituto Oncologico Veneto, Padova, Italy. Vittorina Zagonel, IOV Istituto Oncologico Veneto, Padova, Italy.
Contributors: Conceptualisation: CB and RC. Methodology: CB and RC. Software: CB. Data curation: all authors. Writing—original draft: CB, AC, EC and RC. Writing—review and editing: all authors. Supervision: CB, PP and RC. Project administration: CB, PP and RC.
Funding: The study was supported by ACC (Bando Ricerca Corrente Reti IRCCS 2021, grant number RCR-2021-23671213 and Bando Ricerca Corrente Reti IRCCS 2022, grant number RCR-2022-23682293).
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
Collaborators: on behalf of the IRMO collaborators, Riccardo Caccialanza, Renato Cannizzaro, Valentina Casalone, Rosalisa Cici, Francesco De Lorenzo, Giovanni De Pergola, Teresa Di Lauro, Cristina Fortes, Stefania Gori, Iannelli Elisabetta, Toni Ibrahim, Alessandra Longhi, Cristina Mele Maria, Roberto Mele, Filippo Montemurro, Teresa Nardi Maria, Paolo Pedrazzoli, Debora Pezzuolo, Carmine Pinto, Sandro Pignata, Carmelo Pozzo, Lupe Sanchez Mete, Patrizia Serra, Guseppe Sukkar Samir, Marco Tonello, and Vittorina Zagonel
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. McRackan TR, Watkins JM, Herrin AE, et al. Effect of body mass index on Chemoradiation outcomes in head and neck cancer. Laryngoscope 2008;118:1180–5. 10.1097/MLG.0b013e31816fca5c [DOI] [PubMed] [Google Scholar]
- 2. Norman K, Pichard C, Lochs H, et al. Prognostic impact of disease-related malnutrition. Clin Nutr 2008;27:5–15. 10.1016/j.clnu.2007.10.007 [DOI] [PubMed] [Google Scholar]
- 3. August DA, Huhmann MB, American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors . A.S.P.E.N. clinical guidelines: nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. JPEN J Parenter Enteral Nutr 2009;33:472–500. 10.1177/0148607109341804 [DOI] [PubMed] [Google Scholar]
- 4. Caccialanza R, De Lorenzo F, Gianotti L, et al. Nutritional support for cancer patients: still a neglected right Support Care Cancer 2017;25:3001–4. 10.1007/s00520-017-3826-1 [DOI] [PubMed] [Google Scholar]
- 5. Arends J, Bachmann P, Baracos V, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr 2017;36:11–48. 10.1016/j.clnu.2016.07.015 [DOI] [PubMed] [Google Scholar]
- 6. Hamaker ME, Oosterlaan F, van Huis LH, et al. Nutritional status and interventions for patients with cancer - A systematic review. J Geriatr Oncol 2021;12:6–21. 10.1016/j.jgo.2020.06.020 [DOI] [PubMed] [Google Scholar]
- 7. Brook I. Early side effects of radiation treatment for head and neck cancer. Cancer Radiother 2021;25:507–13. 10.1016/j.canrad.2021.02.001 [DOI] [PubMed] [Google Scholar]
- 8. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis [published correction appears in age ageing. 2019 Jul 1;48(4):601]. Age Ageing 2019:16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cereda E, Tancredi R, Klersy C, et al. Muscle weakness as an additional criterion for grading Sarcopenia-related prognosis in patients with cancer. Cancer Med 2022;11:308–16. 10.1002/cam4.4362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kilgour RD, Vigano A, Trutschnigg B, et al. Handgrip strength predicts survival and is associated with markers of clinical and functional outcomes in advanced cancer patients. Support Care Cancer 2013;21:3261–70. 10.1007/s00520-013-1894-4 [DOI] [PubMed] [Google Scholar]
- 11. Moreau J, Ordan M-A, Barbe C, et al. Correlation between muscle mass and Handgrip strength in digestive cancer patients undergoing chemotherapy. Cancer Med 2019;8:3677–84. 10.1002/cam4.2238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ministero della Salute . “Accordo Stato-Regioni su “Linee Di Indirizzo Sui Percorsi Nutrizionali Nei Pazienti Oncologici”- Rep. Atti N. 224/CSR”. n.d. Available: http://wwwsalutegovit/portale/documentazione/p6_2_2_1jsp?lingua=italiano&id=2682
- 13. Caccialanza R, Goldwasser F, Marschal O, et al. Unmet needs in clinical nutrition in oncology: a multinational analysis of real-world evidence. Ther Adv Med Oncol 2020;12:1758835919899852. 10.1177/1758835919899852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pedrazzoli P, Caccialanza R, Cotogni P, et al. n.d. The advantages of clinical nutrition use in oncologic patients in Italy: real world insights. Healthcare;8:125. 10.3390/healthcare8020125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. U.S. Department of Health and Human Services . Common terminology criteria for adverse events (CTCAE). Versione 5.0. 2017. Available: https://ctepcancergov/protocoldevelopment/electronicapplications/docs/CTCAE_v5_Quick_Reference_5x7pdf
- 16. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern cooperative oncology group. Am J Clin Oncol 1982;5:649–55. [PubMed] [Google Scholar]
- 17. Moro C, Brunelli C, Miccinesi G, et al. Edmonton symptom assessment scale: Italian validation in two palliative care settings. Support Care Cancer 2006;14:30–7. 10.1007/s00520-005-0834-3 [DOI] [PubMed] [Google Scholar]
- 18. Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of Reliability and validity. Med Care 1996;34:220–33. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 19. Kondrup J, Rasmussen HH, Hamberg O, et al. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003;22:321–36. 10.1016/s0261-5614(02)00214-5 [DOI] [PubMed] [Google Scholar]
- 20. Bozzetti F, Mariani L, Lo Vullo S, et al. The nutritional risk in oncology: a study of 1,453 cancer outpatients. Support Care Cancer 2012;20:1919–28. 10.1007/s00520-012-1387-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Orell-Kotikangas H, Österlund P, Saarilahti K, et al. NRS-2002 for pre-treatment nutritional risk screening and nutritional status assessment in head and neck cancer patients. Support Care Cancer 2015;23:1495–502. 10.1007/s00520-014-2500-0 [DOI] [PubMed] [Google Scholar]
- 22. Hersberger L, Bargetzi L, Bargetzi A, et al. Nutritional risk screening (NRS 2002) is a strong and Modifiable Predictor risk score for short-term and long-term clinical outcomes: secondary analysis of a prospective randomised trial. Clin Nutr 2020;39:2720–9. 10.1016/j.clnu.2019.11.041 [DOI] [PubMed] [Google Scholar]
- 23. Gnagnarella P, Dragà D, Misotti AM, et al. Validation of a short questionnaire to record adherence to the Mediterranean diet: an Italian experience. Nutr Metab Cardiovasc Dis 2018;28:1140–7. 10.1016/j.numecd.2018.06.006 [DOI] [PubMed] [Google Scholar]
- 24. ECIS . European cancer information system. n.d. Available: https://ecisjrceceuropaeu/
- 25. Baldwin C, Spiro A, Ahern R, et al. Oral nutritional interventions in malnourished patients with cancer: a systematic review and meta-analysis. J Natl Cancer Inst 2012;104:371–85. 10.1093/jnci/djr556 [DOI] [PubMed] [Google Scholar]
- 26. Youn BY, Lee SY, Cho W, et al. Global trends of nutrition in cancer research: A Bibliometric and visualized analysis study over the past 10 years. Int J Environ Res Public Health 2022;19:4165. 10.3390/ijerph19074165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bargetzi L, Brack C, Herrmann J, et al. Nutritional support during the hospital stay reduces mortality in patients with different types of cancers: secondary analysis of a prospective randomized trial. Ann Oncol 2021;32:1025–33. 10.1016/j.annonc.2021.05.793 [DOI] [PubMed] [Google Scholar]
- 28. Schuetz P, Sulo S, Walzer S, et al. Nutritional support during the hospital stay is cost-effective for preventing adverse outcomes in patients with cancer. Front Oncol 2022;12:916073. 10.3389/fonc.2022.916073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Martin B, Cereda E, Caccialanza R, et al. Cost-effectiveness analysis of oral nutritional supplements with nutritional counselling in head and neck cancer patients undergoing radiotherapy. Cost Eff Resour Alloc 2021;19:35. 10.1186/s12962-021-00291-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Arensberg MB, Richards J, Benjamin J, et al. Opportunities for quality improvement programs (Qips) in the nutrition support of patients with cancer. Healthcare (Basel) 2020;8:227. 10.3390/healthcare8030227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vitaloni M, Caccialanza R, Ravasco P, et al. The impact of nutrition on the lives of patients with digestive cancers: a position paper. Support Care Cancer 2022;30:7991–6. 10.1007/s00520-022-07241-w [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.