Abstract
The number of outstanding clinical claims that are yet to be resolved as well as their associated estimated costs are at a record high in Ireland. By the end of 2022, the Irish government face 3875 active clinical claims which are expected to cost €3.85 billion in total. This does not account for future claims yet to be brought. The financial burden will be borne by the Irish healthcare system which is already facing unprecedented pressures on its services and staff. If current trends continue, the opportunity costs of the current medicolegal landscape will impact the future provision of healthcare. Aside from the financial consequences, clinical claims have numerous negative impacts on all parties involved. Gaining an understanding as to why claims and costs continue to increase relies on access to, and analysis of high-quality patient safety data, including learning from previous litigation. Addressing the causal and perpetuating factors requires efficient implementation of evidence-based recommendations through engagement with stakeholders, including the public. It is necessary to continuously assess the implementation of recommendations as well as measure their impact. This is to ensure that novel efforts from this point onwards do not suffer the same fate as many previous recommendations that, because of a lack of follow-on research, appear to go no further than the page of the report they are written. Action is required now to change the course of the currently unsustainable trajectory of the Irish medicolegal landscape.
Keywords: Health policy; Incident reporting; Risk management; Significant event analysis, critical incident review
Introduction
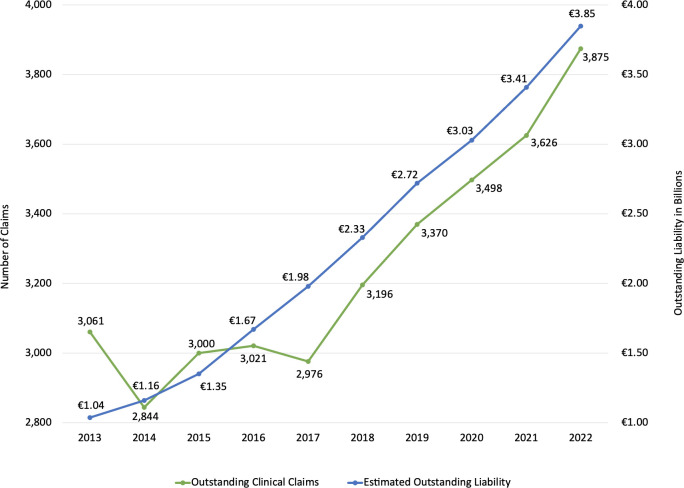
The cost and quantity of outstanding clinical claims in Ireland are rising year on year.1 Now standing at €3.85 billion, the estimated amount required to manage and settle clinical claims involving the State Claims Agency (SCA) is at a record high.2 3 This figure represents a 65.2% increase over 5 years since 2018 and a 270.2% increase over 10 years since 20132 4 5 (figure 1).
Figure 1.
Number of outstanding clinical claims and associated estimated outstanding liability at the end of each year 2013–2022.
As the estimated cost of claims has increased, so too has the annual number of outstanding clinical claims. At the end of 2022, there were 3875 active claims that have yet to be resolved.2 The 21.2% increase over the past 5 years contrasts with a decline in the previous 5 years2 4–6 (figure 1). The increase in cases after 2017 was partially attributed to an increase in mass action claims involving cervical cancer screening and transvaginal implants. However, when mass action claims are excluded there is still an underlying trend showing an increase in cases since 2017.7 The trajectory of liability is unsustainable and its opportunity cost is significant.
The Health Service Executive (HSE) is Ireland’s publicly funded healthcare system, equivalent to the UK’s National Health Service (NHS). The SCA manages clinical claims on behalf of the HSE which results in the SCA being the indemnifier in 90% of all clinical claims in Ireland.8 The remaining 10% are covered by private indemnity providers. In Ireland, litigation costs are resourced from the healthcare budget as the HSE reimburses the SCA for settlements and associated costs.2 While estimated clinical claims’ costs have increased by 270.2% since 2013, the health budget has increased just 54.5%.2 5 9 10 If these trends continue, the long-term financial sustainability of the Irish public healthcare system may be jeopardised.
Contributory factors to rising claims
Despite the increasing number of clinical cases and their costs, there is a lack of specific, detailed data related to the types of claims and the breakdown of costs which limits the understanding about the complexity and severity of the issue. Reasons for pursing legal action vary from case to case. However, research has demonstrated that a commonly cited reason is compensation for losses, both tangible and intangible.11 Some events, for example, catastrophic birth injuries, result in an overwhelming financial burden and services provided by the state are often inadequate.11 In 2010, a report published by an expert working group recommended that the SCA pay plaintiffs periodic payment orders, as opposed to a lump sum, in the cases of catastrophic injury where long-term permanent care is required.1 The periodic payments were implemented in 2017, but by 2019 the Irish High Court found that the index used for estimating future inflation was inadequate and ‘would not meet the cost of future care needs of catastrophically injured people’.1 This reason for litigation is yet to be addressed adequately.
Litigation can be pursued to seek accountability.11 However, this is not always achieved. Localio et al examined the relationship between malpractice claims and adverse events caused by negligence. They found that medical-malpractice litigation ‘infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care’.12 Alternative routes for accountability may be more appropriate than litigation.
A feeling of not being given an explanation or an apology is often a factor, if the not the driver, of many claims.8 11 13 However, legal action seldom addresses these aims. An Irish study explored the emotional burden and impact on both the plaintiff and medical practitioner. One barrister commented that they had never seen “a plaintiff [celebrate] when they win”.13 This can be due to the failure of the system to address extralegal aims such as a desire for communication, openness, an explanation or an apology.13
Open disclosure may address these reasons for litigation. Its significance grew after a controversy involving Ireland’s cervical cancer screening programme, CervicalCheck, which resulted in over 360 legal claims.14 In 2015, internal audits were conducted to retrospectively reanalyse previous cytology of women who had developed interval cervical cancer. In the case of 206 women, cytology previously classified as normal was reclassified. The intention of the audits was quality improvement and the women involved were not informed of the process nor the reclassification.15
In 2018, a scoping inquiry into this controversy was conducted and it found that CervicalCheck was operating at international standards and there was no evidence of laboratory underperformance.14 However, the inquiry did find that Ireland’s ‘policy and practice in relation to open disclosure is deeply contradictory and unsatisfactory’.14 Thereafter, the Patient Safety Bill 2019 was published providing the legislative underpinning for mandatory open disclosure.16 Further work is required to implement mandatory open disclosure in practice as doing so has different challenges in various healthcare contexts.17 Nevertheless, establishing alternative ways of addressing peoples’ reasons for pursuing litigation is vital to reduce the escalating trend.
Impacts of rising claims
The second victim of medical error is the medical professional involved and they too need recognition and support.18 For the doctor, the emotional and psychological impact can progress from initial shock and worry to profound numbness, guilt and isolation.13 The protracted legal process can prevent those involved from moving on and is compounded by the need to continue practising during resolution of the claim.8 13 19 20
Experiencing litigation or a serious adverse event impacts medical practice.21 22 Physicians have reported commonly altering their practice due to risk of litigation.22 Such changes include avoidance of complication-prone procedures and of complex patients. In a survey of surgical practice in Ireland, over half of respondents had a medical negligence claim made against them. All reported practising at least one defensive medicine behaviour occasionally, over one-third were considering early retirement as a result of the current medicolegal climate and one in five would consider emigrating due to a fear of being sued.23 Similarly, a survey of Irish obstetrics and gynaecology trainees noted a negative impact on patient interactions and perception as well as recruitment with one trainee commenting that ‘the current litigation-heavy, fear-inducing, undermining system makes me reconsider my life choice almost every day’.24 In a survey of Irish obstetrics and gynaecology consultants, one described how litigation ‘leaves you a bit on edge… potentially practicing defensive medicines… you are continuously apologising’.25
Contributing factors to rising costs
In 2021, the SCA paid damages in 58% of all cases which totalled €357.4m and was an increase of €35.8m compared with 2020.1 7 Part of the cost of managing and resolving a clinical claim is legal fees. In 2022, the total agency and legal costs were reported to be close to €31m and the total plaintiffs’ legal and other costs were €53.93m.2 Legal costs account for 24% on average of the total cost of a claim.2 An expert group published a ‘Review of the Administration of Civil Justice’ in 2020 and found that ‘Ireland ranks among the highest-cost jurisdictions internationally for civil litigation’.26
In the same year, a separate expert group published a report which reviewed the law of torts and the current systems for the management of clinical negligence claims in Ireland. Despite the group being ‘firmly of the view that our current legal system urgently requires reform’, it did not recommend the introduction of a no-fault system similar to New Zealand, the establishment of a Medical Injuries Assessment Board or a change in fees.8 With no major reforms to the current legal system on the horizon, tackling the unsustainable trajectory of clinical claims and costs in the short-term will be within the constraints of the current system.
The SCA has outlined that a small number of high value claims which relate to maternity services and catastrophic injuries account for a substantial proportion of their outgoings. At the end of 2022, there were 914 active maternity care claims which is 23.6% of the total 3875 active claims. However, their estimated cost reportedly accounts for 63% of the total outstanding liability.2 The SCA also described 365 active catastrophic injury claims which is 9.4% of the 3875 active clinical claims but accounts for €2.8bn or 72.7% of the outstanding liability.2 A catastrophic birth injury may include cerebral palsy/neonatal encephalopathy or death. It is unclear what constitutes a maternity care claim and a catastrophic injury claim. Therefore, calculating overlap is not possible. Nevertheless, they are responsible for a large proportion of cases and costs. The 2023 Irish healthcare budget for women’s health is €32.3m, in contrast an outstanding liability of €2800m is associated with catastrophic injury claims.2 27 This means that significant financial resources will be spent on managing and resolving clinical claims rather than managing and improving clinic services.
Patient safety improvement strategies, which could reduce clinical claims and costs, such as a national health record have stalled. Ireland is one of four countries in the European Union which does not have a fully functioning electronic health record (EHR) and one of five countries which does not have an ePrescription system.28 An integrated EHR would reduce the risk of errors, enhance efficiency and cut costs in the long run.29–31 The SCA has said that a lack of an EHR is a matter of concern as the adequacy of records can be a major issue in clinical claims.2 Unfortunately, a business case for an EHR was rejected in 2018 and has not been resubmitted on the basis that it was necessary to see how the system will work in the new national children’s hospital first which is currently under construction and due to be completed in March 2024.2
Adequate staffing is essential for medical error reduction.32 A recent report by the Economic and Social Research Institute in Ireland forecasts that an additional 15 000 healthcare staff are required by 2035 in a system where there are already significant shortages.33 34 These staffing issues will compound patient safety concerns.32 35–37 On 3 January 2023, the highest ever number of admitted patients without hospital beds in Ireland was recorded, with 931 patients on trolleys.38 An increasing number of doctors are emigrating based on experiences of training and working in an ‘an overstretched, understaffed health system’.39 40 Humphries et al demonstrated that despite improving economic conditions in Ireland, the emigration of doctors to Australia has not decreased as was expected.41 In 2005, 22 doctors in Ireland were issued with working visas. In 2018, this increased to 221 and in the first 9 months of 2022, this has doubled to 442.40 41 The emigration of doctors from Ireland is now at a record high at a time when burdens on the healthcare system are immense.
Data relating to clinical claims
The SCA has a unique position in that it manages 90% of all clinical claims in Ireland, and therefore, has large amounts of data related to patient safety though a claims perspective.8 The SCA has an obligation to advise and assist the HSE on ‘the management of litigation risks and the enhancement of the safety of service users or patients to minimise the incidence of claims and the liabilities of the state’.2 Despite having the legislative remit, the SCA does not routinely evaluate the implementation of the their recommendations in the healthcare system. These evaluations could reduce clinical claims and improve patient safety.2
The HSE has a statutory obligation to record patient safety incidents on the National Incident Management System (NIMS), which is owned by the SCA.42 Capturing no-harm events, near-miss events and events that resulted in a claim is of vital importance to improve patient safety. However, only 25% of incidents that resulted in clinical claims received between 2017 and 2021 were reported by the HSE using NIMS.3 In general, the number of patient safety incidents recorded in NIMS is approximately 50% of incidents that are estimated to occur.43 Lessons cannot be learnt from incidents that are not captured. In a governance review, the Health Information Quality Authority (HIQA) recommended that the HSE and the SCA ‘formalise the governance structures for collaborative work on projects…to ensure the NIMS data are used to their maximum potential’ and that there is scope for an improved approach to the use of incident data to improve patient safety.42 Policy-makers in both the HSE and SCA could focus on creating greater cohesion between the agencies to maximise incident data collection, analysis and distribution.
In other countries, including the UK, there is a greater emphasis on the dissemination and use of national incident data. As well as the the Getting It Right First Time (GIRFT) litigation workstream, the NHS has data from their National Reporting and Learning System available online in accessible formats with an emphasis on consistency across all data users.44 In addition, Organisation Patient Safety Incident Reports are published every 6 months.42 Data sharing is key to facilitating system-wide improvements and the HIQA governance review has advised ‘the HSE, with support from the SCA, to develop an overarching data quality framework’.42 Only then can harm be reduced, safer care provided and spending on clinical negligence minimised.45 46
When risk management strategies have been proposed, follow-through and actions haven’t always occurred. In 2017, the SCA published a comprehensive review titled ‘National Clinical Incidents, Claims and Costs Report-Lessons learnt, a 5-year review: 2010–2014’. The aim of the report was to ‘help improve patient safety by analysing and interrogating national data’ and contained many suggestions for different specialities based on reviewing previous clinical claims or incidents.31 In 2019, the SCA issued a report on claims and incidents related to ‘slips, trips and falls’ between 2014 and 2018 and included risk mitigating strategies.47 To our knowledge, there has been no follow-on research to investigate whether either reports’ suggestions were implemented or the reports’ impacts on claims since their publications.
In Ireland, many inquiries related to healthcare have been carried out, particularly in maternity services. An external inquiry aims to establish the facts around issues or events of public concern and importance. An Irish study examining the content of maternity enquiries found that 9 reports contained 258 recommendations and, on average, a recommendation only contained 3 of the 5 necessary characteristics of a ‘SMART’ aim: specific, measurable, achievable, realistic and time-bound. It was unclear who had responsibility for implementation of the recommendations in 90% of the inquires.48 Furthermore, there are no formal systems in Ireland to assess if any of the recommendations were implemented. The authors highlight that it is unclear who is responsible to follow-up on implementation and who is accountable if there is no implementation.48 Recommendations from reports and inquiries should be SMART, accountability should be clear and implementation should be assessed because as described by Macrae ‘the search for safety starts, rather than ends, with incident reports’.49
Improving the Irish medicolegal landscape
Improving patient safety, reducing risk and clinical claims requires a comprehensive approach which examines no-harm events, near-miss events and adverse events which did not result in a legal claim. However, lessons learnt from litigation have been used in the past to formulate clinical guidelines.50–54 A review of patient safety research carried out since 2000 in Ireland found that just one paper out of 31 included data from clinical claims.55 Internationally, research examining litigation claims have been successful at influencing change. The best example is the findings of the American Society of Anaesthetists Closed Claims Project which contributed significantly to the formulation of standards regarding endotracheal intubation, ulnar nerve injury, spinal cord injury and airway trauma.53 Improving medical guidelines is a central component to addressing patient safety concerns and guidelines can be informed by clinical trials and research, however, learning from previous clinical claims is an underused evidence-based method of enhancing medical practice guidelines which should be further explored.
The NHS Resolution, which is the UK’s equivalent of the SCA, launched ‘Learning from Litigation Claims: GIRFT and NHS Resolution best practice guide for clinicians and managers’.44 Since then, access to claims’ data and standardised analyses have improved. The GIRFT programme advocates and facilitates practical, clinical changes based on learnings and recommendations from NHS claims.44 56–58 Implementing a similar programme here could have similar benefits and allow learnings from previous claims to inform patient safety improvement strategies. However, a central aspect of such a programme should be assessments and audits of the implementation and effectiveness of any recommendations.
An example of tackling the Irish medicolegal landscape is the establishment of the National Neonatal Encephalopathy Action Group, which involves the SCA, the Irish Government’s Department of Health and the HSE’s National Women and Infants Health Programme (NWIHP). The aim of this risk management group is to ‘to identify and address issues relating to avoidable incidents of neonatal encephalopathy…and improve the quality of care within maternity services’.59 The group’s four work streams include a National Obstetric Clinical Advisory Group, the creation of a maternity-specific adverse event review tool, mandatory training in fetal monitoring and obstetric emergencies and progressing practice and supportive technology.60 With regard to implementation and accountability, NWIHP publish an annual report available publicly online which contains a brief update on the progress of the four work streams.59–61 To date, there is no publicly available document outlining the specific goals and aims of the programme nor is there clarity on the responsibilities of the different agencies involved, those being NWIHP, SCA and the Department of Health.
The HSE’s NWIHP has also founded an ‘Obstetric Event Support Team’, however, ‘the responsibility of carrying out the review’ of the event and ‘accountability remain with the hospital’.61 There is an oversight group for this team and engagement with the team is a fixed agenda item on the NWIHP and maternity network meetings.61 While these strategies and groups may represent movement in the right direction, there is guarded optimism that they will result in tangible risk reduction.62–65
Additional measures being taken to improve the Irish medicolegal landscape include the recent announcement by the Irish Department of Health in February 2023 that an interdepartmental working group is to be established and will focus on high value claims.66 Its terms of reference are extensive. They range from examining increasing costs and addressing patient concerns to accelerating legal system changes and considering mass claims’ policy.66 Furthermore, the implementation of a preaction protocol is being amended by the Irish Department of Justice.2 A preaction protocol sets out requirements that must be complied with before a claim is brought.67 Its benefits include an ‘earlier engagement between the parties…well in advance of a court hearing’ which can help avoid the trauma of revisiting the event, reducing the time frame to closure and minimising legal costs.8 13 Mediation is also included in the pre-action protocol. Currently, mediation is underused in Ireland compared internationally for a multitude of reasons, including a lack requesting by plaintiff solicitors, time constraints and availability.68 However, mediation can address many of the extralegal aims of patients, such as receiving an explanation, and can reduce the costs associated with clinical claims.2 68 69
Although not currently planned, an additional method to address the unsustainable medicolegal landscape in Ireland could be to involve the citizens’ assembly. This is a Government of Ireland supported group of people from randomly selected households who meet to discuss important legal and policy issues. The group develop draft recommendations and vote on each. Thereafter, they report their recommendations to the legislature who debate and respond to each recommendation. Over the past decade, citizens’ assemblies have been instrumental in bringing change to the Irish constitution around issues such as same-sex marriage, abortion, gender equality, biodiversity loss and local government structures. As mentioned, the increasing costs and claims are unsustainable for financial and non-financial reasons. A citizens’ assembly may be an appropriate forum to begin understanding the general populations’ opinions, perceptions and feelings about how to address clinical claims and their associated costs.
Conclusion
While progress is being made, the escalating trends of clinical claims and their costs are unsustainable. At the centre of each of these claims is a patient and their family. Any harm or suffering which was potentially preventable is deeply traumatic. Improving patient safety in healthcare systems overall has been shown to reduce avoidable harm.45 The solution to the current growing crisis is multifaceted and will require a whole of Government approach and societal recognition of the growing impact to patient care posed by the opportunity costs of the current landscape. In the short term, a greater culture of learning from litigation and medical error would reduce future burdens. In the long term, legislative change may be required before the spiral of increasing costs compromises needed developments in already overburdened systems and accelerates litigation further.
Footnotes
Correction notice: This article has been corrected since it was first published. The first word in abstract should be “the” and not “a”.
Contributors: Conception and design: CF and SO’R. Manuscript writing: all authors. Final approval of manuscript: all authors. Accountable for all aspects of the work: all authors.
Funding: This study was funded by Academic Track Internship, Intern Network Executive, Ireland. (UCC 4195).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.National Treasury Management Agency . Annual report & financial statements 2021. Dublin, Ireland, 2022. [Google Scholar]
- 2.Committee of Public Accounts . Debate on 2021 financial statements of the state claims agency & chapter 20: management of the clinical indemnity scheme of the report on the accounts of public services 2021. Dublin, Ireland, 2023. [Google Scholar]
- 3.Comptroller and Auditor General . Report on the accounts of the public services 2021. Dublin, Ireland, 2022. [Google Scholar]
- 4.National Treasury Management Agency . Annual report & financial statements 2018. Dublin, Ireland, 2019. [Google Scholar]
- 5.National Treasury management agency . Annual report & financial statements 2013. Dublin, Ireland, 2014. [Google Scholar]
- 6.National Treasury Management Agency . Annual report & financial statements 2017. Dublin, Ireland, 2018. [Google Scholar]
- 7.National Treasury Management Agency . Annual report & financial statements 2020. Dublin, Ireland, 2021. [Google Scholar]
- 8.Expert group report to review the law of torts and the current systems for the management of clinical negligence claims. Dublin, Ireland: Department of Health; 2021. [Google Scholar]
- 9.Government of Ireland . Department of public expenditure and reform. Budget 2022 expenditure report. Dublin, Ireland, 2021. [Google Scholar]
- 10.Government of Ireland . Department of public expenditure and reform. Budget 2013 expenditure report. Dublin, Ireland, 2012. [Google Scholar]
- 11.Vincent C, Young M, Phillips A. Why do people sue doctors? A study of patients and relatives taking legal action. Lancet 1994;343:1609–13. 10.1016/s0140-6736(94)93062-7 [DOI] [PubMed] [Google Scholar]
- 12.Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. N Engl J Med 1991;325:245–51. 10.1056/NEJM199107253250405 [DOI] [PubMed] [Google Scholar]
- 13.Tumelty M-E. Exploring the emotional burdens and impact of medical negligence litigation on the plaintiff and medical practitioner: insights from Ireland. Legal Stud 2021;41:633–56. 10.1017/lst.2021.20 [DOI] [Google Scholar]
- 14.Scally G. Scoping inquiry into the cervicalcheck screening programme. 2018. Available: https://assets.gov.ie/9785/9134120f5b2c441c81eeed06808351c7.pdf [Accessed 09 Nov 2022].
- 15.Cheung M, Fitzpatrick M. The impact of the cervicalcheck controversy on provision of colposcopy services in Ireland: a cohort study. Eur J Obstet Gynecol Reprod Biol 2021;262:228–31. 10.1016/j.ejogrb.2021.05.036 [DOI] [PubMed] [Google Scholar]
- 16.Madden D, Tumelty ME. Open disclosure of patient safety incidents: legislative developments in Ireland. Medico-Legal Journal of Ireland 2019;25 (2):76–89. [Google Scholar]
- 17.Adams M, Hartley J, Sanford N, et al. Strengthening open disclosure after incidents in maternity care: a realist synthesis of international research evidence. BMC Health Serv Res 2023;23:285. 10.1186/s12913-023-09033-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320:726–7. 10.1136/bmj.320.7237.726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nuzum D, Meaney S, O’Donoghue K. The impact of Stillbirth on consultant obstetrician gynaecologists: a qualitative study. BJOG 2014;121:1020–8. 10.1111/1471-0528.12695 [DOI] [PubMed] [Google Scholar]
- 20.Sheen K, Goodfellow L, Balling K, et al. Which events are experienced as traumatic by obstetricians and gynaecologists, and why? A qualitative analysis from a cross-sectional survey and in-depth interviews. BMJ Open 2022;12:e061505. 10.1136/bmjopen-2022-061505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McNamara K, O’Donoghue K. The perceived effect of serious adverse perinatal events on clinical practice. can it be objectively measured? Eur J Obstet Gynecol Reprod Biol 2019;240:267–72. 10.1016/j.ejogrb.2019.05.026 [DOI] [PubMed] [Google Scholar]
- 22.Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 2005;293:2609–17. 10.1001/jama.293.21.2609 [DOI] [PubMed] [Google Scholar]
- 23.Tumelty ME, Cinnamond K, Hannigan A, et al. An exploratory study of the impact of the medico-legal environment on surgical practice in Ireland. Eur J Health Law 2021;2021:1–18. 10.1163/15718093-bja10056 [DOI] [PubMed] [Google Scholar]
- 24.McCarthy CM, O’Sullivan S, Corcoran P, et al. Medicine, media and the law: the effect on training in obstetrics and gynaecology. Eur J Obstet Gynecol Reprod Biol 2021;257:35–41. 10.1016/j.ejogrb.2020.12.004 [DOI] [PubMed] [Google Scholar]
- 25.McCarthy CM, Meaney S, O’Sullivan S, et al. A qualitative review of challenges in recruitment and retention in obstetrics and gynecology in Ireland: the consultants' solution based perspective. PLoS One 2022;17:e0279635. 10.1371/journal.pone.0279635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly P. Review of the administration of civil justice report. Dublin, Ireland, 2020. [Google Scholar]
- 27.Government of Ireland . Department of public expenditure and reform. Budget 2023 expenditure report. Dublin, Ireland, 2023. [Google Scholar]
- 28.Thiel R, Lupiáñez-Villanueva F, Deimel L, et al. eHealth, interoperability of health data and artificial intelligence for health and care in the EU: interoperability of electronic health records in the EU. The European Commission; 2021. [Google Scholar]
- 29.Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood) 2005;24:1103–17. 10.1377/hlthaff.24.5.1103 [DOI] [PubMed] [Google Scholar]
- 30.Sujansky WV. The benefits and challenges of an electronic medical record: much more than a "word-processed" patient chart. West J Med 1998;169:176–83. [PMC free article] [PubMed] [Google Scholar]
- 31.National Treasury Management Agency . National clinical incidents, claims and costs report - lessons learned, a five year review: 2010-2014. Dublin Ireland, 2017. [Google Scholar]
- 32.Griffiths P, Ball J, Murrells T, et al. Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: a cross-sectional study. BMJ Open 2016;6:e008751. 10.1136/bmjopen-2015-008751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keegan C, Brick A, García-Rodríguez A, et al. Projections of workforce requirements for public acute hospitals in Ireland, 2019–2035. Economic and Social Research Institute; 2022. [Google Scholar]
- 34.Irish Hospital Consultants Association . Record waiting lists could spiral further before end of year as over 900 consultant posts remain unfilled. Dublin, Ireland, 2022. Available: https://www.ihca.ie/news-and-publications/record-waiting-lists-could-spiral-further-before-end-of-year-as-over-900-consultant-posts-remain-unfilled [accessed 21 Dec 2022]. [Google Scholar]
- 35.Needleman J, Buerhaus P, Pankratz VS, et al. Nurse staffing and inpatient hospital mortality. N Engl J Med 2011;364:1037–45. 10.1056/NEJMsa1001025 [DOI] [PubMed] [Google Scholar]
- 36.Limb M. Safe staffing: this is how many doctors we really need. BMJ 2018;362:k3136. 10.1136/bmj.k3136 [DOI] [Google Scholar]
- 37.Harvey PR, Trudgill NJ. The association between physician staff numbers and mortality in English hospitals. EClinicalMedicine 2021;32:100709. 10.1016/j.eclinm.2020.100709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Irish Association for Emergency Medicine . National trolley watch. 2023. Available: https://iaem.ie/public/trolley-watch/ [Accessed 04 Jan 2023].
- 39.Humphries N, Crowe S, Brugha R. Failing to retain a new generation of doctors: qualitative insights from a high-income country. BMC Health Serv Res 2018;18:144. 10.1186/s12913-018-2927-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Houston M. Ireland SEES massive emigration of doctors to Australia. BMJ 2023;380:349. 10.1136/bmj.p349 [DOI] [PubMed] [Google Scholar]
- 41.Humphries N, Connell J, Negin J, et al. Tracking the leavers: towards a better understanding of doctor migration from Ireland to Australia 2008-2018. Hum Resour Health 2019;17. 10.1186/s12960-019-0365-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Health Information and Quality Authority . Review of information management practices for the National Incident Management System (NIMS) within the HSE. Dublin, Ireland, 2021. [Google Scholar]
- 43.Connolly W, Rafter N, Conroy RM, et al. The Irish national adverse event Study-2 (INAES-2): longitudinal trends in adverse event rates in the Irish healthcare system. BMJ Qual Saf 2021;30:547–58. 10.1136/bmjqs-2020-011122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Health Service . Learning from litigation claims: the getting it right first time (GIRFT) and NHS resolution best practice guide for clinicians and manager; 2021.
- 45.Yau CWH, Leigh B, Liberati E, et al. Clinical negligence costs: taking action to safeguard NHS sustainability. BMJ 2020;368:m552. 10.1136/bmj.m552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clwyd A, Hart T. A review of the NHS hospitals complaints system: putting patients back in the picture – final report. Williams Lea; 2013. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/255615/NHS_complaints_accessible.pdf [Accessed 18 Jul 2022]. [Google Scholar]
- 47.National Treasury Management Agency . Risk research series. Report 01: slips, trips and falls. Dublin, Ireland, 2019. Available: https://stateclaims.ie/uploads/inner/Risk-Research-Report-01-Slips-Trips-and-Falls-29.11.19.pdf [accessed 24 Apr 2023]. [Google Scholar]
- 48.Helps Ä, Leitao S, O’Byrne L, et al. Irish inquiry reports relating to perinatal deaths and pregnancy loss services. Ir Med J 2020;113:21. [PubMed] [Google Scholar]
- 49.Macrae C. The problem with incident reporting. BMJ Qual Saf 2016;25:71–5. 10.1136/bmjqs-2015-004732 [DOI] [PubMed] [Google Scholar]
- 50.Phillips RL, Bartholomew LA, Dovey SM, et al. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care 2004;13:121–6. 10.1136/qshc.2003.008029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cheney FW. The American society of anesthesiologists closed claims project: what have we learned, how has it affected practice, and how will it affect practice in the future Anesthesiology 1999;91:552–6. 10.1097/00000542-199908000-00030 [DOI] [PubMed] [Google Scholar]
- 52.Forrest C, Madden D, O’Sullivan MJ, et al. Learning from medical litigation. JCO Oncol Pract 2023;19:160–3. 10.1200/OP.22.00763 [DOI] [PubMed] [Google Scholar]
- 53.Vincent C, Davy C, Esmail A, et al. Learning from litigation: an analysis of claims for clinical negligence. Manchester Centre for Healthcare Management, University of Manchester, 2004. [Google Scholar]
- 54.Vincent C, Davy C, Esmail A, et al. Learning from litigation: the role of claims analysis in patient safety. J Eval Clin Pract 2006;12:665–74. 10.1111/j.1365-2753.2006.00634.x [DOI] [PubMed] [Google Scholar]
- 55.O’Connor P, O’Malley R, Kaud Y, et al. A scoping review of patient safety research carried out in the Republic of Ireland. Ir J Med Sci 2023;192:1–9. 10.1007/s11845-022-02930-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.O’Connell RL, Patani N, Machin JT, et al. Litigation in breast surgery: unique insights from the English national health service experience. BJS Open 2021;5:zraa068. 10.1093/bjsopen/zraa068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lane J, Bhome R, Somani B. Urological litigation trends in the UK national health service: an analysis of claims over 20 years. BJU Int 2021;128:361–5. 10.1111/bju.15411 [DOI] [PubMed] [Google Scholar]
- 58.Oglesby FC, Ray AG, Shurlock T, et al. Litigation related to anaesthesia: analysis of claims against the NHS in England 2008-2018 and comparison against previous claim patterns. Anaesthesia 2022;77:527–37. 10.1111/anae.15685 [DOI] [PubMed] [Google Scholar]
- 59.Health Service Executive . National women and Infants health programme. Annual report 2020. Dublin, Ireland, 2021. [Google Scholar]
- 60.Health Service Executive . National women and Infants health programme. Annual report 2021. Dublin Ireland, 2022. [Google Scholar]
- 61.Health Service Executive . National women and Infants health programme. Annual report 2022. Dublin, Ireland, 2023. [Google Scholar]
- 62.Reilly C. Remit of new HSE obstetric incidents team questioned. The Medical Independent; 2023. Available: https://www.medicalindependent.ie/in-the-news/latest-news/remit-of-new-hse-obstetric-incidents-team-questioned/ [Accessed 20 Mar 2023]. [Google Scholar]
- 63.Reilly C. Difficult start for HSE’s obstetric incident team. The Medical Independent; 2023. Available: https://www.medicalindependent.ie/in-the-news/news-features/difficult-start-for-hses-obstetric-incident-team/ [Accessed 10 May 2023]. [Google Scholar]
- 64.Draycott T, Sibanda T, Owen L, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG 2006;113:177–82. 10.1111/j.1471-0528.2006.00800.x [DOI] [PubMed] [Google Scholar]
- 65.Phipps MG, Lindquist DG, McConaughey E, et al. Outcomes from a labor and delivery team training program with simulation component. Am J Obstet Gynecol 2012;206:3–9. 10.1016/j.ajog.2011.06.046 [DOI] [PubMed] [Google Scholar]
- 66.Government of Ireland: Department of Health . Government to establish an interdepartmental working group to examine the rising cost of health-related claims and consider mechanisms to reduce costs. 2023. Available: https://www.gov.ie/en/press-release/e7141-government-to-establish-an-interdepartmental-working-group-to-examine-the-rising-cost-of-health-related-claims-and-consider-mechanisms-to-reduce-costs/ [Accessed 15 Mar 2023].
- 67.Legal services regulation act 2015. Part 15. Part 2A 32 A-D. Available: https://www.irishstatutebook.ie/eli/2015/act/65/section/219/enacted/en/html [Accessed 20 Mar 2023].
- 68.Mitchell B. Look who’s (not) talking: the use of mediation in medical negligence claims in Ireland. J Mediation Appl Confl Anal 2021;7:1–13. 10.33232/jmaca.7.1.15191 [DOI] [Google Scholar]
- 69.Forehand S. Helping the medicine go down: how a spoonful of mediation can alleviate the problems of medical malpractice litigation. OSJDR 1999;14:907–26. [Google Scholar]