Abstract
Background
Understanding discrepancies in mental health and substance use treatment utilization can help identify inequities in access to health services. We investigate mental health and substance use treatment utilization as function of demographic and social determinants, as well as pre-existing mental health and substance use disorders.
Methods
In this repeated cross-sectional study, we used the 2017–2019 National Survey on Drug Use and Health data on US adults above age 18. Two logistic regression models were conducted, using predictors of age, gender, race/Hispanicity, sexual identity, education, insurance, family income, and past year mental health and substance use disorders, with outcomes of mental health or substance use treatment utilization. Weighted estimates of substance use disorders and insurance types and Pearson's correlation tests of vulnerability among age, gender, and treatment type were reported.
Findings
Racial minorities, uninsured populations, sexual minorities, and females had lower odds of receiving mental health treatment, while older populations, lower income groups, and dual eligible enrollees had higher odds. Individuals with substance use disorders but no mental illness had higher odds of receiving mental health treatment. Those utilizing mental health treatment were mostly of high income, privately insured, and using cannabis, cocaine, and opioids. Older populations, men, and Medicaid only enrollees had higher odds of receiving substance use disorder treatment, whereas racial minorities had lower odds. Distribution of income, insurance type, and substance use were more widespread than mental health treatment.
Interpretation
Mental health treatment can be used as an avenue for substance use treatment, particularly opioid use disorders. It is important to target vulnerable populations, like racial minorities and uninsured populations to improve access to mental health and substance use treatment.
Introduction
Mental health and substance use disorders have become an increasing burden among adults in the US, affecting one in five adults [1]. Among adults aged 18 or older, the percentage who had any mental illness rose from 17.7% in 2008 to 20.6% in 2019 [2]. Furthermore, compared to 37 other Organization for Economic Cooperation and Development (OECD) countries in 2019, America had the seventh highest suicide rate, at 16.1 suicides per 100,000 persons [3]. Mental health and substance use disorders are costly from a health systems perspective, rising from 131 billion USD in 2006 to 280 billion USD in 2020 [4,5]. Similarly, substance use has outside impact on public health in the U.S., which has the third largest prevalence of substance use disorders and highest death rate from opioids in 2019 (13.69 deaths per 100,000) worldwide [6]. Furthermore, more than 91,799 drug overdose deaths occurred in 2020, quadrupling since 1999 [7,8]. Both substance use and mental health disorders pose a burden on the United States, emphasizing the need to better understand barriers and inequities in access to receiving treatment.
In the United States, the Affordable Care Act (ACA) aimed to improve accessibility to health insurance among underserved populations, encouraging states to expand Medicaid to individuals of 138% of the federal poverty level (FPL; previously 64% FPL) [9,10]. ACA marketplace exchanges were also created, where individuals can purchase coverage on the marketplace website including subsidies for individuals between 138% and 400% of FPL [9]. The ACA included mental health care in its basic benefit package for Medicaid expansion options in attempts to improve access [11]. In 2016, 2.8 million adults received behavioral health services through Medicaid expansion [12]. Though Medicaid and Marketplace Qualified Health Plans are required to offer mental health and other preventative services, they exclude important services like support services and opioid treatment [11]. Furthermore, provider networks (created to reduce costs by contracting providers and insurance companies) limit services and specialists, bottlenecking access to health services [13]. The ACA was designed as a steppingstone to improving mental health treatment access, yet barriers persist, especially among Black Americans [14].
In previous research, alcohol use disorders have been assessed as a predictor of mental health treatment [15], but not solely illicit drug disorders or illicit drug use disorders in conjunction with alcohol use disorders as predictors. Understanding substance use disorders as a predictor of mental health treatment utilization can help us recognize if mental health resources are improperly delivered to individuals with substance use disorders without other mental health disorders. Though concurrent treatment is important, few studies have independently assessed mental health disorders and substance use disorders in relationship to treatment utilization.
The aim of this research was to understand the extent to which demographic, social determinants, as well as existing mental health and substance use disorders are associated with mental health and substance use treatment utilization in United States. These predictors were further explored by analyzing how substance use disorders and insurance status are distributed among those who receive treatment. Furthermore, trends in those receiving mental health treatment (inpatient, outpatient, prescription) and substance use treatment among vulnerable populations were assessed to understand unmet need.
Methods
Data overview and analysis
We used data from the 2017–2019 National Survey on Drug Use and Health (NSDUH) among adults above 18 years of age in the United States. The NSDUH is an annual cross-sectional, national survey on the non-institutionalized, civilian United States population aged 12 and older conducted by the Substance Abuse and Mental Health Services Administration (SAHMSA). It aims to estimate the prevalence of substance use and mental illness and elucidates their determinants [16,17]. Survey participants include household residents and individuals residing in non-institutional group quarters. Members of the active-duty military, homeless individuals not in shelters, and individuals in institutional group quarters (i.e., hospitals, prisons, nursing homes, treatment centers) were excluded. NSDUH data is available to the public and anonymized (see supplementary materials).
Variable selection
Adults over 18 years were pooled for analysis. Due to inconsistent and limited data collection from the COVID-19 pandemic, SAMHSA discouraged NSDUH 2020 and 2021 data comparisons to previous years [18]. As outcome variables, mental health treatment utilization in the past year (yes/no) was used in the first analysis and substance use treatment utilization (yes/no) in the second analysis.
The analysis incorporated a number of demographic variables and their association with mental health and substance use treatment utilization, as unmet need of treatment resources is largest for the elderly, racial minorities, lower income, and uninsured [19]. Demographic variables included age (18–25, 26–34, 35–49, 50 or older), gender (Male, Female), race/Hispanicity (Non-Hispanic White, Non-Hispanic Black/African American, Non-Hispanic Native American/Alaskan Native, Non-Hispanic Native Hawaiian/Other Pacific Islander, Non-Hispanic Asian, Non-Hispanic More than One Race), and sexual identity (Heterosexual, Lesbian/Gay, Bisexual). The term sexual identity will be used to refer to sexual orientation, following the terminology used in coding of variables in the NSDUH Codebook [18].
Several proxies for social determinants of health were also included. Individuals were grouped based on their highest level of education (Less than High School, High School, Some College/Associate's Degree, College Graduate), insurance status (Insured or Uninsured), and total family income (Less than $10,000 (Including Loss); $10,000–$19,999; $20,000–$29,999; $30,000–$39,999; $40,000–$49,000; $50,000–$74,999; $75,000 or more). Regarding health status, both mental health and substance use disorders were considered. An additional composite variable that we labelled vulnerability score was created to assess trends in vulnerability in three dimensions across age group, gender, and mental health treatment utilization [17,20,21]. This composite score was created by assigning one point for each of the following: not insured, income less than $20,000, and less than a high school education. Our rationale was to include a measure of insurance status due to its importance in accessing health services, a measure of low income because of the links between low income and mental health status and a measure of educational outcome to assess how low educational achievement might be involved in vulnerability and also of course associate with insurance status and low incomes. Mental health status was categorized as having or not having a mental illness in the past year. Substance use disorders were classified based on past year illicit drug disorder, alcohol use disorder, both, or neither. Variables are summarized in Table S1.
Data analysis
Two separate survey-weighted generalized logistic regression models were used to assess the different independent variable measures and their association with mental health or substance use treatment utilization, respectively. Respondents with missing data for any category were excluded from the analysis. Furthermore, individuals that reported both any mental illness and alcohol or illicit drug dependence or abuse in the past year were excluded to minimize collinearity and assess each as a predictor independently. To test for independence between variables, a chi-square test was conducted between mental health or substance use treatment status and every other variable measure across each year.
To assess the potential effect of missing data, an imputed odds ratio was calculated as a sensitivity analysis using Multivariate Imputation Using Chained Equations (MICE; see Fig. S1a and S1b) [22]. Another sensitivity analysis compared odds ratios from pooled data of 2015–2016 (N = 80,439) and 2017–2019 (N = 118,798) to assess whether time period and sample size affected odds ratio outcomes (see Table S5a and Table S5b). We predicted missing data variables on mental health treatment utilization and sexual identity based on age group, gender, race/Hispanicity, education, insurance coverage, family income, type of substance use disorder, and mental illness. The analysis was performed in RStudio version 1.4.1717.
Results
Baseline characteristics
A total of 118,798 adults were included for this analysis (39,565 from 2017, 39,832 from 2018, and 39,401 from 2019; see Table 1 and S2). Among those who did not receive mental health treatment, 50.1% were female, whereas 69.8% were female among those who did receive mental health treatment. Similarly, among those who did not receive substance use treatment, 53.3% were female, while 38.0% were female among those who did receive substance use treatment. Non-Hispanic white, heterosexual, and insured individuals, respectively, made up the largest proportion of adults in the sample. Most individuals did not report a mental health or substance use disorder in the past year.
Table 1.
Baseline Characteristics of Individuals Across Mental Health Treatment Utilization.
| Characteristics | No Mental Health Treatment (N = 100,823) | Mental Health Treatment (N = 17,975) |
|---|---|---|
| Age (years) | ||
| 18–25 | 32,362 (32.1%) | 5286 (29.4%) |
| 26–34 | 20,225 (20.1%) | 3676 (20.5%) |
| 35–49 | 26,401 (26.2%) | 5433 (30.2%) |
| 50 or older | 21,835 (21.7%) | 3580 (19.9%) |
| Gender | ||
| Male | 50,306 (49.9%) | 5427 (30.2%) |
| Female | 50,517 (50.1%) | 12,548 (69.8%) |
| Race and Hispanicity | ||
| Non-Hispanic White | 58,051 (57.6%) | 13,615 (75.7%) |
| Non-Hispanic Black/African American | 13,700 (13.6%) | 1286 (7.2%) |
| Non-Hispanic Native American/Alaskan Native | 1374 (1.4%) | 188 (1.0%) |
| Non-Hispanic Native Hawaiian/Other Pacific Islander | 541 (0.5%) | 28 (0.2%) |
| Non-Hispanic Asian | 5393 (5.3%) | 363 (2.0%) |
| Non-Hispanic More than One Race | 3137 (3.1%) | 660 (3.7%) |
| Hispanic | 18,627 (18.5%) | 1835 (10.2%) |
| Sexual Identity | ||
| Heterosexual | 94,952 (94.2%) | 15,523 (86.4%) |
| Lesbian/Gay | 1914 (1.9%) | 594 (3.3%) |
| Bisexual | 3957 (3.9%) | 1858 (10.3%) |
| Highest Level of Education | ||
| Less than High School | 12,868 (12.8%) | 1616 (9.0%) |
| High School | 27,508 (27.3%) | 3781 (21.0%) |
| Some College/Associate's Degree | 33,080 (32.8%) | 6689 (37.2%) |
| College Graduate | 27,367 (27.1%) | 5889 (32.8%) |
| Insurance Status | ||
| Not Insured | 12,351 (12.3%) | 1089 (6.1%) |
| Insured | 88,472 (87.7%) | 16,886 (93.9%) |
| Family Income | ||
| Less than $10,000 (Including Loss) | 7948 (7.9%) | 1661 (9.2%) |
| $10,000 - $19,999 | 10,158 (10.1%) | 1895 (10.5%) |
| $20,000 - $29,999 | 10,436 (10.4%) | 1731 (9.6%) |
| $30,000 - $39,999 | 10,228 (10.1%) | 1624 (9.0%) |
| $40,000 - $49,999 | 10,546 (10.5%) | 1673 (9.3%) |
| $50,000 - $74,999 | 16,051 (15.9%) | 2823 (15.7%) |
| $75,000 or more | 35,456 (35.2%) | 6568 (36.5%) |
| Past Year Substance Disorder | ||
| No Substance Use Disorder | 95,146 (94.4%) | 17,159 (95.5%) |
| Illicit Drug Disorder Only | 1362 (1.4%) | 200 (1.1%) |
| Alcohol Use Disorder Only | 3789 (3.8%) | 509 (2.8%) |
| Both Alcohol and Illicit Drug Disorder | 526 (0.5%) | 107 (0.6%) |
| Past Year Mental Illness | ||
| No Mental Illness | 87,546 (86.8%) | 8132 (45.2%) |
| Mental Illness | 13,277 (13.2%) | 9843 (54.8%) |
Mental health treatment utilization logistic regression results
The results of our logistic regression model for mental health treatment utilization (Fig. 1a and Table S3a) show individuals aged 35–49 years old and 50 or older both had higher odds of receiving mental health treatment compared to individuals 18–25 years old (OR 1.35[1.26, 1.44] and OR 1.23[1.14, 1.32], respectively). Females had nearly double the odds of receiving mental health treatment than males (OR 1.85 [1.76, 1.94]). Furthermore, every racial and Hispanicity category had lower odds of mental health treatment utilization than non-Hispanic whites. Compared to heterosexual individuals, both individuals who were lesbian/gay and bisexual had higher odds of receiving mental health treatment (OR 1.72 [1.44, 2.05] and OR 1.73 [1.55, 1.94], respectively). People with some college/Associate's Degree or a college degree reported higher odds of utilizing mental health treatment than individuals with less than a high school education (OR 1.40 [1.26, 1.55] and OR 1.55 [1.38, 1.74], respectively). Compared to uninsured individuals, insured individuals had nearly double the odds of receiving mental health treatment (OR 1.98 [1.77, 2.20]). Those with a family income of less than 10,000 USD had greater odds of utilizing mental health treatment (OR 1.40 [1.26, 1.55], while those with family incomes between $30,000 - $39,999 and $40,000 - $49,999 had lower odds of utilizing mental health treatment compared to family incomes above $75,000 (OR 0.86 [0.77, 0.96] and OR 0.88 [0.78, 0.98], respectively). Individuals with illicit drug disorders (OR 2.27 [1.79, 2.87]), alcohol disorders (OR 1.89 [1.64, 2.17]), and both disorders (OR 3.10 [2.28, 4.21]) had a higher odds of utilizing mental health treatment than those without a substance use disorder. Individuals that reported a mental illness in the past year had nearly eight times greater odds of receiving mental health treatment than those without a mental health disorder (OR 7.94 [7.53, 8.37]).
Fig. 1.
a. Odds Ratios of Logistic Regression for Mental Health Treatment. * indicates reference category.b. Odds Ratios of Logistic Regression for Substance Use Treatment. * indicates reference category.
Substance use disorder treatment logistic regression results
The results of the logistic regression for substance use treatment utilization (Fig. 1b and Table S3b) show that all age groups (26–34, 34–49, 50 or older) had a higher odds of receiving substance use treatment compared to those aged 18–25 years. Compared to males, females had 0.48 [0.40, 0.57] times lower odds of utilizing substance use treatment. Non-Hispanic Black/African Americans (OR 0.75 [0.58, 0.96]), non-Hispanic Asians (OR 0.22 [0.11, 0.42]), and Hispanic individuals (OR 0.50 [0.39, 0.65]) were at lower odds of receiving substance use treatment as compared to non-Hispanic Whites. Bisexual individuals had lower odds of receiving treatment compared to heterosexuals (OR 0.22[0.11, 0.42]). Those with some college/Associate's degree (OR 0.73 [0.58, 0.92]) and college degree (OR 0.46 [0.33, 0.64]) each had lowers odds of receiving treatment than those with less than a high school degree. Odds of utilizing treatment did not differ based on insurance status. All family income brackets had higher odds of receiving substance use treatment compared to families with an income greater than 75,000 USD. Individuals with any type of substance use disorder in the past year had a higher odds of receiving substance use treatment than those without a substance abuse disorder. Compared to individuals without a mental illness in the past year, those with a mental illness had nearly triple the odds of utilizing substance use treatment (OR 2.98[2.41, 3.67]).
Reported illicit drug use disorders among adults who receive treatment
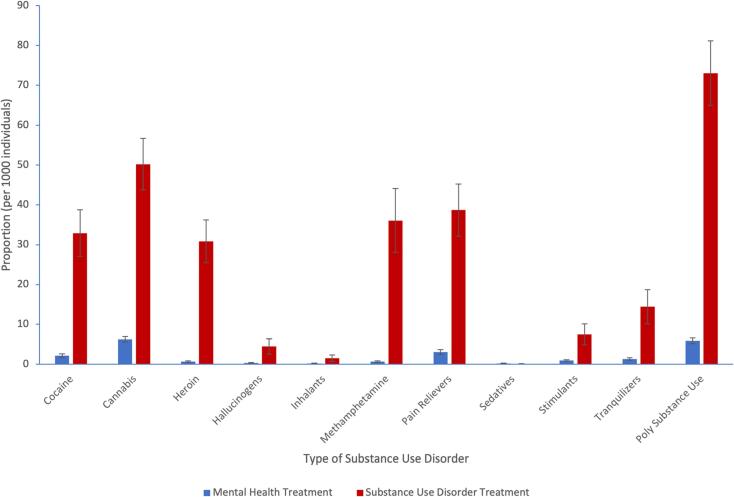
Illicit drug disorders encompass many different types of drugs. Fig. 2 depicts the reported illicit drug disorders among adults who receive mental health treatment (i.e., mental health treatment not for substance use disorders). Dependence and abuse of cannabis and poly-substance use had a higher reported prevalence than all other drug use disorders. This was followed by dependence and abuse of pain relievers and cocaine. Fig. 2 also shows the weighted distribution of substance use disorders among those who receive substance use treatment. Reported poly-substance use was higher than any substance use disorder individually. The most reported substance use disorders include cannabis, pain relievers, methamphetamine, cocaine, and heroin. Compared to the report of substance use disorders among utilizers of mental health treatment, the report of substance use disorders among utilizers of substance use treatment was higher across all disorders except for sedatives.
Fig. 2.
Reported Illicit Drug Disorders Among Adults Who Receive Mental Health and Substance Use Disorder Treatment. Note that individuals included in poly substance use are also included in individual substance use disorders.
Types of insurance among adults who receive treatment
Weighted estimates were calculated to explore types of insurance among individuals who receive treatment. Among individuals who receive mental health treatment, a higher proportion had private insurance than all other forms of insurance. This was followed by Medicare and Medicaid/CHIP (Fig. 3). A different distribution of types of insurance was seen among adults who utilized substance use treatment. Reported private insurance and Medicaid/CHIP were higher than other forms of insurance and not different from one another. These types of insurance were followed by Medicare. Among those with more than one insurance, 48.1% were dual eligible, approximately double the proportion within mental health treatment.
Fig. 3.
Reported Insurance Types Among Adults Who Receive Mental Health and Substance Use Disorder Treatment. Note that individuals included in more than one insurance are also included in individual types of insurance.
Vulnerability and mental health treatment
To further explore vulnerability in relationship to types of treatments, we show a heat map based on age group, vulnerability score, gender, and mental health treatment type, with darker shades representing higher weighted prevalence (Fig. 4a). In each row of gender and treatment type, we show the prevalence of receiving mental health treatment of any type generally increases with decreasing vulnerability. Pearson's correlation tests between vulnerability score within age group and prevalence within gender and treatment type (Table S10a) show that groups with higher vulnerability scores received less treatment and higher vulnerability scores are more frequently reported among those aged 18–25 years within most gender-treatment type combinations. Likewise, Fig. 4b shows a heat map based on age group, vulnerability score, gender, and substance use treatment, with darker shades representing higher reporting. Within each row of gender and treatment type, a similar trend can be seen of increased prevalence of receiving substance uses treatment with lower vulnerability scores. Table S10b shows the results of Pearson's correlation tests vulnerability score within age group and prevalence within gender and treatment type. Across each age group and gender, increasing vulnerability scores are associated with lower report of substance use treatment.
Fig. 4.
a. Reported Age Group and Vulnerability Score Within Gender and Mental Health Treatment Type. Percentages based on each row of each pane of the figure. b. Reported Age Group and Vulnerability Score Within Gender and Substance Use Treatment. Percentages based on each row of each pane of the figure.
Discussion
Many findings of this analysis replicate previous evidence on mental health and substance use treatment utilization. This analysis found that racial minorities and those without insurance had lower odds of utilizing mental health treatment. This aligns with previous research findings stating that unmet need for mental health care is higher among these same groups in the United States [19,23,24]. Females also had higher odds of receiving mental health treatment compared to males. Individuals with alcohol use disorders had a greater odds of receiving mental health treatment than those without a substance use disorder, aligning with evidence that individuals with alcohol use disorders are more likely to receive mental health treatment [15].
So far, there is mixed evidence on the relationship between age and mental healthcare needs [19,25]. This analysis showed that age groups 35–49 and 50 or older had higher odds of receiving mental health treatment. However, higher odds of receiving treatment does not necessarily indicate a lack of unmet need. Thus, there may still be large unmet need in older populations, despite higher odds of receiving treatment. Additionally, increased vulnerability scores were associated with a lower prevalence of any type of mental health treatment for females and most types of treatment for males, especially among people aged 18–25 years.
Lower family income was previously associated with increased risk of mental health disorders [26], which may contribute to higher odds of receiving mental health treatment. Findings for family income brackets from $30,000 to $39,999 and $40,000 to $49,999 having lower odds of receiving treatment aligned with previous evidence on greater unmet need for lower income populations [19,23]. A plausible explanation for this is the role of Medicaid and Medicare with the former being the single largest payer for mental health services in the United States [27]. That said, most individuals who received mental health treatment in this study were privately insured, pointing to the need to increase mental health coverage among private insurers.
Another interesting finding for mental health treatment utilization is in relationship to substance use disorders. In our analysis, mental health treatment and substance use disorder treatment were mutually exclusive and individuals with co-occurring mental health and substance use disorders were removed, meaning that adults with substance use disorders did not report any other mental health conditions. Despite this exclusion, those with only illicit drug use disorders, only alcohol use disorder, and both disorders still reported greater odds of receiving mental health treatment than those without substance use disorders. This may signal inefficiencies in the diagnosis of substance use or mental health disorders, as well as seeking and receiving treatment for these disorders. Additionally, adults with substance use disorders may believe that their disorder is a product of the need to self-medicate to reduce mental health symptoms [28]. Even though both mental health and substance use disorders have historically been stigmatized, the acceptability and attitudes toward seeking mental health treatment have improved among Americans [29]. However, substance use has remained stigmatized particularly due to its criminalized status. The greater normalization of mental health treatment may therefore encourage substance users to seek treatment at mental health sites, rather than specific substance use facilities.
Among adults who received mental health treatment, the most reported illicit drug use disorders included cannabis, cocaine, and pain relievers. All three drugs are accessed and used by individuals of different socioeconomic status. Some evidence suggests that higher income settings are associated with greater cannabis use [30,31], though other evidence suggests lower income individuals are more likely to use cannabis [32,33]. Between 2001 and 2002 and 2012 and 2013, the risk of cocaine use was reported across multiple socioeconomic groups [34]. Lastly, opioids are prescribed at greater rates to individuals of higher socioeconomic status in emergency and noncancer settings [35,36]. This aligns with the high reporting of private insurance among those who receive mental health treatment, as higher income individuals can afford private insurance. The high reporting of cannabis, cocaine, and pain relievers may also suggest that these subgroups are wrongfully receiving mental health treatment, as individuals with comorbid conditions were excluded from analysis.
With respect to substance use disorder treatment, there is less available research on predictors. However, among existing evidence, the study findings are corroborated regarding race and ethnicity. In this analysis, African American and Hispanic adults had lower odds of receiving substance use disorder treatment than white adults, supported by evidence that these racial minorities were less likely to receive alcohol or drug abuse treatment and more likely to perceive unmet need for treatment [37,38]. The increasing substance use disorders among the aging baby boomer population may account for the increased odds of receiving mental health treatment for older age groups, as compared to 18–25 year age group [39]. Findings from another demographic factor, gender, also aligns with existing evidence. Females had lower odds of receiving substance use treatment, and generally have lower rates of use and dependence on illicit drugs and alcohol than men [40]. Generally, across all substance use disorders, there was a higher odds of receiving substance use treatment as compared to individuals without a substance use disorder. This is hopeful, as individuals with substance use disorders should be receiving substance use treatment.
All lower family income levels had higher odds of receiving substance use treatment as compared to the highest income level, $75,000 or over. This may be due to the fact that lower income individuals are more likely to report problems with substance use [20,41]. Additionally, among high income countries like the United States, drug use disorders follow a gradient in which risk of suffering from a substance use disorder increases with decreasing socioeconomic status [42]. Across all age groups and both genders, increasing vulnerability was associated with a lower prevalence of receiving substance use treatment. This does not mean that population groups with high socioeconomic status do not experience risks of substance use disorders, but rather that they may experience a lower magnitude of risk. Substance use disorders affecting multiple income levels also aligns with the distribution of insurance status among individuals who received substance use treatment. Medicaid and private insurance were the two most common forms of individual insurance, with higher reporting than any other insurance type.
Considering that private insurance is mainly acquired through employer-based insurance or directly purchase by income earners and Medicaid is for low-income populations, this suggests that there is a distribution of income levels receiving substance use treatment. The insurance distribution of substance use treatment contrasts with mental health treatment utilization, where reporting of only private insurance was higher than any other form of insurance. Additionally, among those with more than one insurance, the proportion of dual eligible adults among those with more than one insurance was more than double within substance use treatment than mental health treatment, further demonstrating the widespread income distribution in substance use treatment utilization.
The distribution of substance use disorders among those who receive substance use treatment was also more widespread than mental health treatment utilization. The most common individual drug use disorders included cannabis, pain relievers, cocaine, heroin, and methamphetamine. The addition of heroin and methamphetamine, as compared to mental health treatment utilization, may account for lower-income populations utilizing substance use disorder treatment. Comparing the opioids of heroin and prescription pain relievers, heroin users have greater odds of being socioeconomically disadvantaged, while prescription painkiller users have greater odds of being economically stable among adults in the United States [43]. Furthermore, rates of heroin use between 2002 and 2004 and 2011–2013 remained highest among individuals with family incomes less than $20,000 and with no insurance or Medicaid [44]. Similarly, risk factors for methamphetamine include lower annual household income [45], further supporting a greater spread of income levels and insurance among those who receive substance use treatment.
There are some limitations to this analysis, including the design of the NSDUH itself. This data is based on self-reported measures, which depend on truthfulness and memory of respondents [46]. Thus, this analysis is susceptible to response bias, as individuals may feel stigmatized and hesitant to report certain symptoms or illnesses. Furthermore, 3 % of the population is excluded from the survey, including active-duty military, persons in institutional group quarters, and homeless individuals. This exclusion of these groups may result in slightly inaccurate survey measurements [46]. Specifically for substance use treatment, both individuals who did not report receiving treatment and with unknown treatment status were recorded as “No” for receiving treatment. This may partially account for the presence of individuals without substance use disorders who received substance use treatment. Lastly, among heroin users there is likely to be under-reporting and selective non-response, leading to underestimates of heroin prevalence [47].
Conclusion
In short, people with substance use disorders continue to commonly seek out mental health treatment. Mental health services should seek to develop the specialized capacity to treat this population group, while public policy should look to improve widespread access to services through initiatives like broader health insurance coverage. Additionally, mental health professionals should be trained to diagnose and address substance use disorders to create a more streamlined process for substance use treatment, by improving knowledge and decreasing stigma surrounding substance use disorders [48,49]. Finally, the high reporting of opioids and poly-substance use among those receiving substance use treatment reflects the continued existence of the global opioid epidemic in the United States.
Funding
No funding was acquired for this research.
CRediT authorship contribution statement
Jaskiran Dhinsa: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Writing – original draft, Writing – review & editing, Visualization. Andres Roman-Urrestarazu: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Writing – original draft, Writing – review & editing, Visualization, Project administration, Supervision. Robin van Kessel: Validation, Writing – original draft, Writing – review & editing. Keith Humphreys: Validation, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
No conflicts of interest are reported.
Acknowledgements
We would like to thank Ms. Alicja Mastylak for her thorough language edits in the finalization of this article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.gloepi.2023.100109.
Appendix A. Supplementary data
Supplementary material
Data availability
All data for this study is openly available at https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health.
References
- 1.2022 State of Mental Health in America.pdf [Internet] https://mhanational.org/sites/default/files/2022%20State%20of%20Mental%20Health%20in%20America.pdf [cited 2022 Oct 5]. Available from:
- 2.Lipari R.N. 2019. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health; p. 114. [Google Scholar]
- 3.Suicide mortality rate (per 100,000 population) - OECD members | Data [Internet] https://data.worldbank.org/indicator/SH.STA.SUIC.P5?locations=OE&most_recent_value_desc=false [cited 2022 Oct 5]. Available from:
- 4.bhsua-2006-2015-508.pdf [Internet] https://store.samhsa.gov/sites/default/files/d7/priv/bhsua-2006-2015-508.pdf [cited 2022 Jun 13]. Available from:
- 5.Reducing the Economic Burden of Unmet Mental Health Needs [Internet] The White House. https://www.whitehouse.gov/cea/written-materials/2022/05/31/reducing-the-economic-burden-of-unmet-mental-health-needs/ [cited 2022 Oct 5]. Available from:
- 6.Share of the population with alcohol or drug use disorders [Internet] Our World in Data. https://ourworldindata.org/grapher/share-with-alcohol-or-drug-use-disorders [cited 2022 Jul 12]. Available from:
- 7.Death Rate Maps & Graphs | Drug Overdose | CDC Injury Center [Internet] 2022. https://www.cdc.gov/drugoverdose/deaths/index.html [cited 2022 Jun 12]. Available from:
- 8.Understanding the Epidemic | Drug Overdose | CDC Injury Center [Internet] 2022. https://www.cdc.gov/drugoverdose/epidemic/index.html [cited 2022 Jun 12]. Available from:
- 9.Apr 25 P, 2013 Summary of the Affordable Care Act [Internet]. KFF. 2013. https://www.kff.org/health-reform/fact-sheet/summary-of-the-affordable-care-act/ [cited 2022 Jun 13]. Available from:
- 10.Eliminating the ACA: What Could It Mean for Medicaid Expansion? [Internet] KFF. 2020. https://www.kff.org/policy-watch/eliminating-the-aca-what-could-it-mean-for-medicaid-expansion/ [cited 2022 Jul 19]. Available from:
- 11.Robertson-Preidler J., Trachsel M., Johnson T., Biller-Andorno N. The affordable care act and recent reforms: policy implications for equitable mental health care delivery. Health Care Anal. 2020 Sep 1;28(3):228–248. doi: 10.1007/s10728-020-00391-0. [DOI] [PubMed] [Google Scholar]
- 12.Ali M.M., Teich J., Woodward A., Han B. The implications of the affordable care act for behavioral health services utilization. Adm Policy Ment Health Ment Health Serv Res. 2016 Jan 1;43(1):11–22. doi: 10.1007/s10488-014-0615-8. [DOI] [PubMed] [Google Scholar]
- 13.Montz E., Layton T., Busch A.B., Ellis R.P., Rose S., McGuire T.G. Risk-adjustment simulation: plans may have incentives to distort mental health and substance use coverage. Health Aff (Millwood) 2016 Jun;35(6):1022–1028. doi: 10.1377/hlthaff.2015.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han B., Lai J., Yu H. Impact of the ACA Medicaid expansion on utilization of mental health care. Med Care. 2020 Sep;58(9):757–762. doi: 10.1097/MLR.0000000000001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edlund M.J., Booth B.M., Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J Stud Alcohol Drugs. 2012 Jul;73(4):635–646. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Medley G., Lipari R.N., Bose J., Cribb D.S., Kroutil L.A., Mc Henry G. 2015. Sexual Orientation and Estimates of Adult Substance Use and Mental Health: Results from the 2015 National Survey on Drug Use and Health; p. 54. [Google Scholar]
- 17.Rosner B., Neicun J., Yang J.C., Roman-Urrestarazu A. Substance use among sexual minorities in the US – linked to inequalities and unmet need for mental health treatment? Results from the National Survey on drug use and health (NSDUH) J Psychiatr Res. 2021 Mar 1;135:107–118. doi: 10.1016/j.jpsychires.2020.12.023. [DOI] [PubMed] [Google Scholar]
- 18.National Survey on Drug Use and Health 2020 (NSDUH-2020-DS0001) | SAMHDA [Internet] https://www.datafiles.samhsa.gov/dataset/national-survey-drug-use-and-health-2020-nsduh-2020-ds0001 [cited 2022 May 11]. Available from:
- 19.Wang P.S., Lane M., Olfson M., Pincus H.A., Wells K.B., Kessler R.C. Twelve-month use of mental health services in the United States: results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005 Jun 1;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 20.Neicun J., Yang J.C., Shih H., Nadella P., van Kessel R., Negri A., et al. Lifetime prevalence of novel psychoactive substances use among adults in the USA: sociodemographic, mental health and illicit drug use correlates. Evidence from a population-based survey 2007–2014. Angkurawaranon C, editor. PloS One. 2020 Oct;15(10) doi: 10.1371/journal.pone.0241056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang J.C., Roman-Urrestarazu A., Brayne C. Binge alcohol and substance use across birth cohorts and the global financial crisis in the United States. PloS One. 2018 Jun 25;13(6) doi: 10.1371/journal.pone.0199741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Buuren S., Groothuis-Oudshoorn K. mice : Multivariate imputation by chained equations in R. J Stat Softw [Internet] 2011;45(3) http://www.jstatsoft.org/v45/i03/ [cited 2022 Jul 12]. Available from: [cited 2022 Jul 12]. Available from: [Google Scholar]
- 23.Roll J.M., Kennedy J., Tran M., Howell D. Disparities in unmet need for mental health Services in the United States, 1997–2010. Psychiatr Serv. 2013 Jan;64(1):80–82. doi: 10.1176/appi.ps.201200071. [DOI] [PubMed] [Google Scholar]
- 24.Walker E.R., Cummings J.R., Hockenberry J.M., Druss B.G. Insurance status, use of mental health services, and unmet need for mental health care in the United States. Psychiatr Serv. 2015 Jun;66(6):578–584. doi: 10.1176/appi.ps.201400248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kessler R.C., Berglund P.A., Bruce M.L., Koch J.R., Laska E.M., Leaf P.J., et al. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001 Dec;36(6 Pt 1):987–1007. [PMC free article] [PubMed] [Google Scholar]
- 26.Sareen J., Afifi TO, McMillan K.A., Asmundson G.J.G. Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch Gen Psychiatry. 2011 Apr 4;68(4):419–427. doi: 10.1001/archgenpsychiatry.2011.15. [DOI] [PubMed] [Google Scholar]
- 27.Behavioral Health Services | Medicaid [Internet] https://www.medicaid.gov/medicaid/benefits/behavioral-health-services/index.html [cited 2022 Jul 4]. Available from:
- 28.Khantzian E.J. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997 Feb;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- 29.Americans'’ Attitudes Toward Mental Health Treatment Seeking: 1990–2003 | Psychiatric Services [Internet] https://ps.psychiatryonline.org/doi/10.1176/ps.2007.58.5.642?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed [cited 2022 Jul 4]. Available from: [DOI] [PubMed]
- 30.Galea S., Ahern J., Tracy M., Vlahov D. Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am J Prev Med. 2007 Jun 1;32(6, Supplement) doi: 10.1016/j.amepre.2007.04.003. S195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patrick M.E., Wightman P., Schoeni R.F., Schulenberg J.E. Socioeconomic status and substance use among young adults: a comparison across constructs and drugs. J Stud Alcohol Drugs. 2012 Sep;73(5):772–782. doi: 10.15288/jsad.2012.73.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeffers A.M., Glantz S., Byers A., Keyhani S. Sociodemographic characteristics associated with and prevalence and frequency of cannabis use among adults in the US. JAMA Netw Open. 2021 Nov 30;4(11) doi: 10.1001/jamanetworkopen.2021.36571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma M. Determinants of marijuana use, abuse and dependence. J Alcohol Drug Educ. 2009;53(1):3–6. [Google Scholar]
- 34.Kerridge B.T., Chou S.P., Pickering R.P., Ruan W.J., Huang B., Jung J., et al. Changes in the prevalence and correlates of cocaine use and cocaine use disorder in the United States, 2001–2002 and 2012–2013. Addict Behav. 2019 Mar 1;(90):250–257. doi: 10.1016/j.addbeh.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 35.Joynt M., Train M.K., Robbins B.W., Halterman J.S., Caiola E., Fortuna R.J. The impact of neighborhood socioeconomic status and race on the prescribing of opioids in emergency departments throughout the United States. J Gen Intern Med. 2013 Dec 1;28(12):1604–1610. doi: 10.1007/s11606-013-2516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vitzthum L.K., Nalawade V., Riviere P., Sumner W., Nelson T., Mell L.K., et al. Racial, ethnic, and socioeconomic discrepancies in opioid prescriptions among older patients with cancer. JCO Oncol Pract. 2021 Jun;17(6):e703–e713. doi: 10.1200/OP.20.00773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wells K., Klap R., Koike A., Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am J Psychiatry. 2001 Dec;158(12):2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- 38.Mulvaney-Day N., DeAngelo D., Chen C. nan, Cook B.L., Alegría M. Unmet need for treatment for substance use disorders across race and ethnicity. Drug Alcohol Depend. 2012 Sep 1;125:S44–S50. doi: 10.1016/j.drugalcdep.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuerbis A. Substance use among older adults: an update on prevalence, etiology, assessment, and intervention. Gerontology. 2020;66(3):249–258. doi: 10.1159/000504363. [DOI] [PubMed] [Google Scholar]
- 40.Abuse NI on D. Sex and Gender Differences in Substance Use [Internet]. National Institute on Drug Abuse https://nida.nih.gov/publications/research-reports/substance-use-in-women/sex-gender-differences-in-substance-use [cited 2022 Jul 5]. Available from:
- 41.Baptiste-Roberts K., Hossain M. Socioeconomic disparities and self-reported substance abuse-related problems. Addict Health. 2018 Apr;10(2):112–122. doi: 10.22122/ahj.v10i2.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.WDR20_Booklet_5.pdf [Internet] https://wdr.unodc.org/wdr2020/field/WDR20_Booklet_5.pdf [cited 2022 Jul 5]. Available from:
- 43.Rigg K.K., Monnat S.M. Comparing characteristics of prescription painkiller misusers and heroin users in the United States. Addict Behav. 2015 Dec 1;51:106–112. doi: 10.1016/j.addbeh.2015.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jones C.M., Logan J., Gladden R.M., Bohm M.K. Vital signs: demographic and substance use trends among heroin users — United States, 2002–2013. Morb Mortal Wkly Rep. 2015 Jul 10;64(26):719–725. [PMC free article] [PubMed] [Google Scholar]
- 45.Han B., Compton W.M., Jones C.M., Einstein E.B., Volkow N.D. Methamphetamine use, methamphetamine use disorder, and associated overdose deaths among US adults. JAMA Psychiatry. 2021 Dec 1;78(12):1329–1342. doi: 10.1001/jamapsychiatry.2021.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Survey on Drug Use and Health 2019 (NSDUH-2019-DS0001) | SAMHDA [Internet] https://www.datafiles.samhsa.gov/dataset/national-survey-drug-use-and-health-2019-nsduh-2019-ds0001 [cited 2022 May 11]. Available from:
- 47.Reuter P., Caulkins J.P., Midgette G. Heroin use cannot be measured adequately with a general population survey. Addiction. 2021;116(10):2600–2609. doi: 10.1111/add.15458. [DOI] [PubMed] [Google Scholar]
- 48.Howard V., Holmshaw J. Inpatient staff perceptions in providing care to individuals with co-occurring mental health problems and illicit substance use. J Psychiatr Ment Health Nurs. 2010;17(10):862–872. doi: 10.1111/j.1365-2850.2010.01620.x. [DOI] [PubMed] [Google Scholar]
- 49.Harwood H.J., Kowalski J., Ameen A. The need for substance abuse training among mental health professionals. Adm Policy Ment Health Ment Health Serv Res. 2004 Nov 1;32(2):189–205. doi: 10.1023/b:apih.0000042746.79349.64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
All data for this study is openly available at https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health.