Abstract
Background
Most asthma-related deaths occur in low- and middle-income countries, and South Africa (SA) is ranked fifth in global asthma mortality. Little is known about the characteristics and outcome of asthma patients requiring intensive care unit (ICU) admission in SA.
Objectives
To identify and characterise patients with acute severe asthma admitted to the respiratory ICU at Groote Schuur Hospital, Cape Town, SA, in order to evaluate outcomes and identify predictors of poor outcomes in those admitted.
Methods
We performed a retrospective descriptive study of patients with severe asthma admitted to the respiratory ICU at Groote Schuur Hospital between 1 January 2014 and 31 December 2019.
Results
One hundred and three patients (110 admission episodes) were identified with an acute asthma exacerbation requiring ICU admission; all were mechanically ventilated. There was a female preponderance (53.6%; n=59/110), with a median (range) age overall of 33 (13 - 84) years. Of all admissions, 40 (36.4%) were current tobacco smokers and 16 (14.5%) patients with a history of substance abuse. Two thirds (60.0%; n=66/110) of the patients were using an inhaled corticosteroid (ICS). No predictors of mortality were evident in multivariate modelling, although those who died were older, and had higher Acute Physiology and Chronic Health Evaluation (APACHE II) scores and longer duration of admission. Only 59 of the surviving 96 individual patients (61.5%) attended a specialist pulmonology clinic after discharge.
Conclusion
Among patients admitted to the respiratory ICU at Groote Schuur Hospital for asthma exacerbations, there was a high prevalence of smokers and poor coverage with inhaled ICSs. Although mortality was low compared with general ICU mortality, more needs to be done to prevent acute severe asthma exacerbations.
Study synopsis
What the study adds. Intensive care unit (ICU) admission represents the most severe form of exacerbation of asthma. South Africa (SA) has a very high rate of asthma deaths, and this study demonstrates that admission to an ICU with a very severe asthma exacerbation frequently results in a good outcome. However, many of the patients admitted to the ICU were not adequately treated with background asthma medications prior to their admission.
Implications of the findings. Death from asthma should be avoidable, and admission to an ICU is not associated with high mortality. Patients are therefore likely to be dying at home or out of hospital. Better education and access to medication and early access to health services rather than improved in-hospital care would potentially alter SA’s high asthma mortality
Keywords: Asthma, intensive care, outcomes
Background
Asthma is one of the most prevalent chronic diseases globally, with an estimated 339 million people diagnosed with asthma. A disproportionately high number of asthma-related deaths occur in low- and middle-income countries (LMICs); according to the World Health Organization, >80% of asthma-related deaths occur in these countries.[1]
Factors that have been attributed to the high asthma-related mortality in LMICs include lack of access to essential medicines, suboptimal long-term medical care, delays in obtaining medical care, low income, and low levels of education.[2,3] Hospital admissions can be seen as an indirect measure of the burden of uncontrolled and more severe asthma and lack of effective primary asthma care. Treatment in the intensive care unit (ICU), especially mechanical ventilation, represents the most severely affected patients and those who have not been adequately controlled in the outpatient setting.[4,5]
There is no direct correlation between asthma-related mortality and asthma prevalence. South Africa (SA) is currently ranked 25th worldwide for asthma prevalence, but 5th in global asthma mortality.[5] However, not all people with severe asthma will make it to an ICU; the majority (>70%) of asthma deaths in SA occur before arrival at a hospital.[6]
We therefore set out to conduct a retrospective descriptive study to identify and characterise all patients with acute severe asthma admitted to the respiratory ICU at Groote Schuur Hospital, Cape Town, SA, in order to evaluate outcomes and identify predictors of poor outcomes in those admitted.
Methods
We performed a retrospective descriptive study of patients with acute severe asthma admitted to the respiratory ICU at Groote Schuur Hospital. The medical/respiratory ICU is an 8-bed unit admitting primarily medical patients requiring intensive care and/or mechanical ventilation. The records of patients admitted to the ICU between 1 January 2014 and 31 December 2019 (prior to the COVID -19 pandemic) were reviewed, and patients admitted with a primary diagnosis of acute severe asthma were included in the study.
Demographic data, blood results on admission, arterial blood gas measurements, Acute Physiology and Chronic Health Evaluation (APACHE II) score, comorbidities, current medications, length of ICU stay, complications in the ICU, days mechanically ventilated, duration of hospital stay, and outcomes were collected. All data were entered into a REDCap (Research Electronic Data Capture) database.
Statistical analysis
The data were analysed using GraphPad Prism 9 for macOS (GraphPad Software LLC, USA). Descriptive statistics and Fisher’s exact tests were performed on dichotomous categorical variables and t-tests on continuous data. Parametric and non-parametric tests were used in univariate analyses. Predictors of outcome were explored using stepwise multivariate logistic regression analysis. A significance level of p<0.05 was chosen, and all statistical tests were two-sided.
Ethical considerations
The University of Cape Town Faculty of Health Sciences Human Research Ethics Committee (ref. no. HREC REF:110/2020) and the Groote Schuur Hospital Research Committee provided approval to conduct the audit.
Results
During the 6 years 2014 - 2019, there were 2 684 admissions to the respiratory ICU. Of these, a total of 110 individual admissions (103 patients) had a diagnosis of an acute severe asthma exacerbation. These constituted 4.1% of the total ICU admissions. All patients required mechanical ventilation. There was a slight female preponderance (53.6%; n=59/110). The patients were generally young, with a median (range) age of 33.5 (13 - 84) years (Fig. 1). The demographic characteristics (individual admissions) are detailed in Table 1.
Table 1. Demographics and baseline clinical information on patients admitted to the ICU with asthma (N=110 individual admissions).
| Variable | n (%)* |
| Age (years), median (range) | 33.5 (13 - 84) |
| Male | 51 (46.4) |
| Female | 59 (53.6) |
| Previous ICU admission | 7 (6.4) |
| Current tobacco smoker | 40 (36.4) |
| Hypertension | 16 (14.5) |
| Substance abuse | 16 (14.5) |
| Diabetic | 10 (9.1) |
| HIV | 6 (5.4) |
| Pregnant | 5 (4.5) |
ICU = intensive care unit.
* Except where otherwise indicated
Fig. 1.
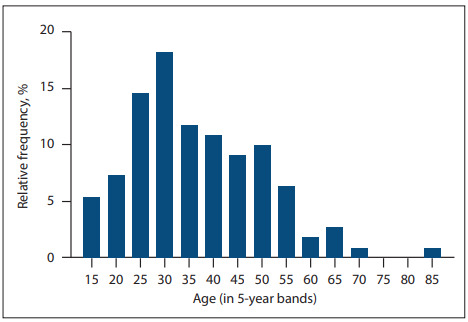
Age distribution of patients admitted with severe asthma for ventilation.
N=110 individual admissions
Over a third (36.4%; n=40/110 individual admissions) of the patients were current tobacco smokers, and 14.5% (n=16/110) had a history of substance abuse; 93.8% of substance abusers smoked tobacco, compared with 26.7% of patients with no history of substance abuse (p<0.001). Patients with a history of substance abuse were significantly younger than the non-substance users (29 years v. 37.9 years; p=0.002).
Almost all (91.8%; n=101/110 individual admissions) of the patients were using a short-acting beta-agonist, but only 60.0% (n=66/110) reported being treated with an inhaled corticosteroid (ICS) before the ICU admission. Half of those on an ICS were additionally receiving a long-acting beta-agonist, either as a separate inhaler ‘free’ or in fixed-dose combination with an inhaled steroid. The prevalence of ICS treatment was significantly lower (25.0%) in patients with a history of substance abuse compared with patients without such a history (69.9%) (p=0.004). A small proportion of patients (10.9%; n=12/110) were on long-term oral corticosteroids. The frequency of prescribed asthma medications taken by the patients admitted to the ICU is shown in Table 2.
Table 2. Asthma-related medication documented on admission to the ICU (N=110 individual admissions).
| Medication | n (%) |
| SABA | 101 (91.8) |
| ICS | 66 (60.0) |
| LABA* | 32 (29.1) |
| SAMA | 13 (11.8) |
| OCS | 12 (10.9) |
| Oral theophylline | 24 (21.8) |
| LAMA | 2 (1.8) |
ICU = intensive care unit
SABA = short-acting beta-agonist
ICS = inhaled corticosteroid
LABA = long-acting beta-agonist
OCS = oral corticosteroid
LAMA = long-acting muscarinic antagonist
* All patients receiving a LABA were also co-prescribed an ICS
All patients were intubated prior to transfer to the ICU. On admission to the ICU, 82.7% (n=91/110 individual admissions) had acute respiratory acidosis, median (interquartile range (IQR)) pH 7.22 (7.13 - 7.31), and 10.9% had a pH <7.0. The median partial pressure of carbon dioxide (PaCO2 ) was 9.09 (6.68 - 11.25) kPa, and 85.5% (n=94/110) of the patients had significant hypercapnia. The median white cell count was 15.30 (12.30 - 22.20) × 109 /L, with low lactate levels (1.30 (0.90 - 1.93) mmol/L) (Table 3).
Table 3. Blood results on admission to the ICU (N=110 individual admissions).
| Variable | Median (IQR) |
| pH | 7.22 (7.13 - 7.31) |
| PaO2 (kPa) | 13.40 (10.73 - 18.15) |
| PaCO2 (kPa) | 9.09 (6.68 - 11.25) |
| HCO3 (mmol/L) | 24.15 (21.0 - 28.43) |
| WCC (× 109/L) | 15.30 (12.30 - 22.20) |
| Hb (g/dL) | 12.40 (11.30 - 13.80) |
| Lactate (mmol/L) | 1.30 (0.90 - 1.93) |
| Creatinine (µmol/L) | 64.50 (52.0 - 84.75) |
| APACHE II score | 9 (8 - 12) |
ICU = intensive care unit
IQR = interquartile range
PaO2 = partial pressure of oxygen
PaCO2 = partial pressure of carbon dioxide
HCO3 = bicarbonate
WCC = white cell count; Hb = haemoglobin
APACHE II = Acute Physiology and Chronic Health Evaluation
The median (IQR) length of mechanical ventilation was 2 (1 - 4) days. ICU stay after extubation was short, with a median overall ICU stay of 3 (2 - 5) days. A minority of the patients (10.0%; n=11/110 individual admissions) had a prolonged ICU stay (>7 days). The median length of total stay in hospital was 5 (4 - 8) days (Fig. 2).
Fig. 2.
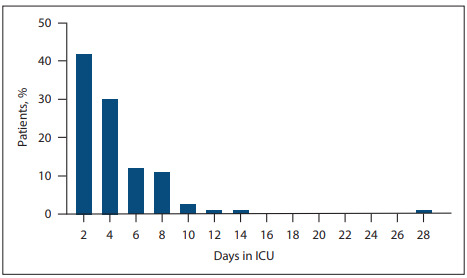
Length of stay of asthma patients admitted to the ICU.
ICU = intensive care unit
Less than a quarter of the patients (22.7%; n=25/110 individual admissions) had a recorded complication during their ICU stay. The most common complications were renal failure (13.6%; n=15/110), sepsis (10.9%; n=12/110), pneumothorax (2.7%; n=3/110) and cardiac arrhythmias (2.7%; n=3/110). Very few patients had more than one complication.
The overall mortality in the ICU (individual admissions) was 4.5% (n=5 deaths); 103 patients (93.6%) survived to hospital discharge, with 2 deaths occurring after ICU discharge. Patients who died were on average older and had a longer length of stay and higher APACHE II scores compared with those who survived to ICU discharge (n=105) (Table 4). No predictors of mortality were evident in the multivariate analysis.
Table 4. Univariate analysis of factors associated with mortality.
| Variable | ICU survivors (n=105) | ICU non-survivors (n=5) | p-value | OR (univariate analysis) |
| pH, mean (SD) | 7.21 (0.14) | 7.13 (0.26) | 0.165 | - |
| PaCO2 (kPa), mean (SD) | 9.36 (3.81) | 11.10 (6.34) | 0.268 | - |
| Age (years), mean (SD) | 35.6 (12.4) | 51.3 (23.8) | 0.003 | 0.94 (0.88 - 0.99) |
| APACHE II score, mean (SD) | 9.8 (3.7) | 14.4 (3.5) | 0.002 | 0.84 (0.70 - 1.02) |
| Days in ICU, mean (SD) | 3.7 (2.5) | 7.1 (9.3) | 0.008 | 0.87 (0.73 - 1.05) |
| Smokers, n (%)* | 40 (38.1) | 0 | 0.15 | - |
| Reported illicit drug use, n (%)* | 16 (15.2) | 0 | 0.9 | - |
ICU = intensive care unit
OR = odds ratio
SD = standard deviation
PaCO2 = partial pressure of carbon dioxide
APACHE II = Acute Physiology and Chronic Health Evaluation
* Of 105 ICU admissions (including readmissions) surviving patients with documentation of substance use/non-use
Among the 96 individual patients who were discharged from hospital after their ICU admission (7 of the 103 had died), 59 (61.5%) had a record of a subsequent follow-up at the specialist respiratory clinic at Groote Schuur Hospital. A smaller percentage (25.0%; n=4/16) of patients with a history of substance abuse returned for follow-up compared with non-substance users (68.8%; n=55/80) (p=0.01). The odds of returning for review after discharge among patients who had a history of substance abuse was 0.21 (95% confidence interval 0.07 - 0.69).
Discussion
We present the outcomes and clinical characteristics of the 2014 - 2019 admissions to the Groote Schuur Hospital respiratory ICU of patients with acute severe asthma requiring invasive mechanical ventilation. Ventilation for asthma represents <5% of ICU admissions, with >95% survival. However, ICU mortality for asthma at our institution has effectively doubled from the previously documented figure of 2.2% for 1980 - 1997.[6] It is unclear why mortality has increased, given the advances in ICU care; however, it remains comparable to high-income countries, which have an ICU mortality for mechanically ventilated asthmatics of ~5%.[4,7]
ICU admission is synonymous with failure of preventive treatment in the healthcare system to prevent severe exacerbations of asthma. The younger age and female preponderance were seen in a previous asthma ICU study in SA, with similar (4.3 days) ICU stay.[6] Long delays in seeking medical attention and underuse of corticosteroids were risk factors for invasive mechanical ventilation.[8]
Only two-thirds of the patients admitted with acute severe asthma in the present study reported being treated with an ICS. Information with regard to adherence and inhaler technique was not obtainable. This low use of ICSs among asthmatics is of concern, given the association with an increased risk of hospitalisation and mortality[9–11] as well as availability of the Global Initiative for Asthma (GINA) strategy document and SA asthma guidelines, which both reinforce the need for all asthma patients to receive an ICS.[5]
Globally it has been reported that the major risk factors for ICU admission for acute severe asthma include a history of smoking (>10 pack-years), atopy, previous mechanical ventilation, and high use of an inhaled beta-agonist.[12–14] Of the patients in the present study (individual admissions), 36.4% were smokers. This figure is higher than the background estimated population smoking rates of 32.9% in Western Cape Province and 17.6% in SA.[15] Asthma control, response to steroids and outcomes are worse in smokers and those abusing other drugs,[16–18] but in our cohort, all the asthmatics who smoked and/or used illicit drugs survived. However, return for follow-up was worse in those who smoked and reported drug use.
There were several limitations to this study. Owing to its retrospective nature and our reliance on medical records, it was not possible to obtain accurate data on medication history and smoking rates, and other information. Specifically, details on the amount of rescue medicine used prior to admission, and adherence to using ICSs, are not available.
The potential exists that some patients with chronic obstructive pulmonary disease (COPD) may have been included in the acute severe asthma cohort, and that some patients with acute severe asthma were erroneously labelled as having COPD. Without complete follow-up of both groups, it is not possible to be 100% certain.
Conclusion
Approximately 18 patients with acute severe asthma are admitted per year to the Groote Schuur Hospital ICU for mechanical ventilation, a third of whom are not being treated with an ICS. These patients frequently smoke and use drugs. More work is required to identify patients in primary care who are at risk of exacerbations and ensure that optimal therapy is provided to prevent ICU admission for mechanical ventilation.
Acknowledgments
We are grateful to the staff in the Division of Critical Care at Groote Schuur Hospital who cared for these patients and allowed us to evaluate the outcomes.
References
- 1.Brakema EA, Tabyshova A, van der Kleij R, et al. The socioeconomic burden of chronic lung disease in low-resource settings across the globe – an observational FRESH AIR study. Respir Res. 2019;20:291. doi: 10.1186/s12931-019-1255-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sinharoy A, Mitra S, Mondal P. Socioeconomic and environmental predictors of asthma-related mortality. J Environ Public Health. 2018;2018:9389570. doi: 10.1155/2018/9389570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant EN, Lyttle CS, Weiss KB. The relation of socioeconomic factors and racial/ethnic differences in US asthma mortality. Am J Public Health. 2000;90(12):1923–1925. doi: 10.2105/ajph.90.12.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gibbison B, Griggs K, Mukherjee M, Sheikh A. Ten years of asthma admissions to adult critical care units in England and Wales. BMJ Open. 2013;3(9):e003420. doi: 10.1136/bmjopen-2013-003420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Global Initiative for Asthma. Fontana, USA: Global Initiative for Asthma – GINA; 2021. [August 2021]. Global Strategy for Asthma Management and Prevention, 2021.https://ginasthma.org/wp-content/uploads/2023/04/GINA-MainReport-2021-V2-WMSA.pdf [Google Scholar]
- 6.Zar HJ, Stickells D, Toerien A, et al. Changes in fatal and near-fatal asthma in an urban area of South Africa from 1980 - 1997. Eur Respir J. 2001;18(1):33–37. doi: 10.1183/09031936.01.00081801. [DOI] [PubMed] [Google Scholar]
- 7.Demoule A, Brochard L, Dres M, et al. How to ventilate obstructive and asthmatic patients. Intensive Care Med. 2020;46(12):2436–2449. doi: 10.1007/s00134-020-06291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westerman DE, Benatar SR, Potgieter PD, et al. Identification of the highrisk asthmatic patient: Experience with 39 patients undergoing ventilation for status asthmaticus. Am J Med. 1979;66(4):565–572. doi: 10.1016/0002-9343(79)91165-3. [DOI] [PubMed] [Google Scholar]
- 9.Gonem S, Cumella A, Richardson M. Asthma admission rates and patterns of salbutamol and inhaled corticosteroid prescribing in England from 2013 to 2017. Thorax. 2019;74(7):705–706. doi: 10.1136/thoraxjnl-2018-212723. [DOI] [PubMed] [Google Scholar]
- 10.Weatherall M, Wijesinghe M, Perrin K, et al. Meta-analysis of the risk of mortality with salmeterol and the effect of concomitant inhaled corticosteroid therapy. Thorax. 2010;65(1):39–43. doi: 10.1136/thx.2009.116608. [DOI] [PubMed] [Google Scholar]
- 11.O’Byrne P, Fabbri LM, Pavord ID, et al. Asthma progression and mortality: The role of inhaled corticosteroids. Eur Respir J. 2019;54(1):1900491. doi: 10.1183/13993003.00491-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Juárez León JE, Gonzalez Islas D, Sandoval Gutierrez JL, et al. Risk factors for hospitalisation and ICU admission for near-fatal asthma. Eur Respir J. 2017;50(suppl 61):PA3575. doi: 10.1183/1393003.congress-2017.PA3575. [DOI] [Google Scholar]
- 13.Eisner MD, Lieu TA, Chi F, et al. Beta agonists, inhaled steroids, and the risk of intensive care unit admission for asthma. Eur Respir J. 2001;17(2):233–240. doi: 10.1183/09031936.01.17202330. [DOI] [PubMed] [Google Scholar]
- 14.Nakwan N, Prateepchaiboon T. Predicting the requiring intubation and invasive mechanical ventilation among asthmatic exacerbation-related hospitalisations. J Asthma. 2022;59(3):507–513. doi: 10.1080/02770903.2020.1853768. [DOI] [PubMed] [Google Scholar]
- 15.Reddy P, Zuma K, Shisana O, et al. Prevalence of tobacco use among adults in South Africa: Results from the first South African National Health and Nutrition Examination Survey. S Afr Med J. 2015;105(8):648–655. doi: 10.7196/SAMJnew.7932. [DOI] [PubMed] [Google Scholar]
- 16.Levine M, Iliescu ME, Margellos-Anast H, et al. The effects of cocaine and heroin use on intubation rates and hospital utilisation in patients with acute asthma exacerbations. Chest. 2005;128(4):1951–1957. doi: 10.1378/chest.128.4.1951. [DOI] [PubMed] [Google Scholar]
- 17.Polosa R, Thomson NC. Smoking and asthma: Dangerous liaisons. Eur Respir J. 2013;41(3):716–726. doi: 10.1183/09031936.00073312. [DOI] [PubMed] [Google Scholar]
- 18.Caponnetto P, Auditore R, Russo C, et al. ‘Dangerous relationships’: Asthma and substance abuse. J Addict Dis. 2013;32(2):158–167. doi: 10.1080/10550887.2013.795469. [DOI] [PubMed] [Google Scholar]