Abstract
Objective
Patients with advanced laryngeal cancer are typically presented with divergent treatment options, namely chemoradiation versus total laryngectomy. This study aims to understand general perspectives of the factors involved in this decision‐making process.
Methods
Surveys were constructed using specialized conjoint analysis software. Seven attributes integral to the decision‐making process for advanced laryngeal cancer treatment were included.
Results
Three hundred one healthy adult volunteers completed the decision‐making program. The relative impact of each treatment attribute on decision making across all participants was scored with an average importance score (standard deviation) as follows: Lifespan 22.2% (±8.5), Voicing 21.4% (±5.9), Swallowing 19.1% (±7.3), Cancer Cure 14.9% (±6.2), Mode of Breathing 11.0% (±3.7), Self‐Image 6.7% (±2.9), and Treatment Type 4.8% (±3.0).
Conclusions
General public opinion ranked lifespan, voicing, and swallowing aspects as similarly important, and all were ranked more important than probability of cure. These data demonstrate a variety of priorities among participants and the need for tailored discussions when determining treatment choice for advanced laryngeal cancer.
Level of Evidence
Level 4.
Keywords: conjoint analysis, decision‐making, laryngeal cancer, priorities, treatment
This study provides new insights into the priorities of the general public when considering treatment choice for advanced laryngeal cancer. General public opinion ranked lifespan, voicing, and swallowing aspects as similarly important, and all were ranked more important than probability of cure. These data demonstrate a variety of priorities amongst participants and emphasizes the need for tailored discussions when determining treatment choice for advanced laryngeal cancer.

1. INTRODUCTION
Laryngeal cancer has an estimated incidence of 12,400 new cases annually in the United States. 1 , 2 Of these cases, approximately 40% are diagnosed at an advanced stage (III or IV), necessitating more aggressive treatment with significantly increased morbidity. 3 Historically, total laryngectomy with adjuvant radiation therapy had been the standard of care for advanced laryngeal cancer. However, after the publication of the 1991 VA Laryngeal Cancer Study Group trial, laryngeal preservation with chemotherapy and radiation became an acceptable alternative to surgical management. 4 Subsequently, laryngeal preservation therapy and locoregional control was demonstrated to be best achieved with concurrent chemotherapy and radiotherapy (CCRT) per RTOG 91‐11. 5 , 6
In more recent years, compelling data have emerged showing that, for T4 laryngeal cancers, total laryngectomy has significantly improved survival compared to CCRT. 7 , 8 However, for stage III disease, both surgical management and laryngeal preservation therapy remain acceptable options, and the decision of which modality to choose is often left up to the provider and patient. 7
Given the morbidities inherent to each modality, patients are forced to accept difficult tradeoffs when making this decision. 8 , 9 , 10 , 11 Laryngectomy not only allows for a functional swallow without risk of aspiration, but also leads to a loss of natural voice, need for a permanent stoma with subsequent stoma care, and alterations to physical appearance. Alternatively, while CCRT allows for an anatomically intact organ, the residual function is suboptimal. Patients often experience dysphonia, poor swallow function with increased aspiration risk, and difficulty breathing leading to transient or permanent need for a tracheostomy. 8 , 9 Given the significant implications on daily life, patients play a large role in choosing the treatment option that they feel is most in line with their values and goals. The process is often further complicated by counseling from physicians with divergent priorities, that is, achieving cancer‐cure.
In 1981, McNeal and colleagues published the landmark Tradeoffs Between Quality and Quantity of Life study (later known as the Firefighter's study) exploring patient preferences on tradeoffs. Based on the attitudes of 37 healthy volunteers, they found that 20% of participants would choose radiation over surgery to preserve their native voice—suggesting that the quality of additional years of life may be as or more important than the quantity of years remaining. 12 Since this study, our understanding of these attitudes, which comprise a significant component of the decision‐making process, has not advanced significantly. Although prior groups have conducted time‐trade off analyses of laryngeal cancer decision‐making, these studies used health states in which participants are presented with clinical vignettes describing bundled treatment options and associated outcomes. 13 , 14 , 15 This approach forces participants to choose an overall treatment option (surgical intervention vs. CCRT) and limits analysis of the individual factors and attributes that comprise such an “overall package,” that is, impact on Lifespan, Cancer Cure, Breathing, Swallowing, and Voicing. Alternatively, choice‐based conjoint analysis allows for a nuanced analysis of the aforementioned factors contained within a treatment option that can affect participants' choice of treatment. Thus, conjoint analysis allows us to explore the factors within treatment options that lend desirability or undesirability, a level of detail previously not available.
Thus, this study aims to investigate acceptable trade‐offs in decision making for the treatment of advanced laryngeal cancer. We aim to better understand patient preferences for not only treatment itself but also for the factors that affect choice of treatment—specifically treatment type, lifespan, likelihood of cancer cure, and impact on breathing, swallowing, voicing, and self‐image. These data would allow for a stronger understanding of patient considerations when choosing treatment for advanced laryngeal cancer and could inform clinical counseling and the development of future therapeutic interventions.
2. METHODS
2.1. Conjoint analysis
This was a cross‐sectional study investigating decision making regarding treatment choice for advanced laryngeal cancer. The study utilizes conjoint analysis, a tool used in business market research for measuring: (1) the value placed on particular features of a product and (2) the impact of those features on consumers choosing that product. In conjoint analysis, respondents are presented with real‐world situations in which they must trade one product for another with different features. The attributes of the products are determined by the researcher, and there are predefined options within each attribute. For example, if a study was performed looking at desirable features of a car, an attribute could be “Color,” and the options may include “Red,” “Black,” and “Blue.” A second attribute could be “Type of Car,” and the options may include “Sedan,” “Convertible,” and “SUV.” Participants would be presented with a series of choices between hypothetical combinations of these attributes. In one such scenario, they may be asked to choose between Option 1 (“Red,” “Sedan”) and Options 2 (“Blue,” “SUV”) (see example in Figure 1). The aggregate of participant choice tasks is then analyzed to yield utility scores, a quantitative measure of a preference for a specific product feature or attribute level (higher utility scores indicate greater preference). The utility scores for each attribute level can be summed together to yield the total utility of that attribute. Importance scores are then calculated from attribute utility scores to characterize the relative importance of each attribute during decision making; the summation of all attribute importance scores in a single study adds up to 100 percent. Further description of calculations of utility and importance scores can be found in the Sawtooth Software technical papers. 16
FIGURE 1.

Example conjoint analysis construction, choice task, and utility calculation.
Conjoint analysis has previously been used in a number of studies investigating medical decision‐making, with results demonstrating that these choice‐based tasks reduce decision conflict and help provide clarity in making important medical decisions. 17 , 18 , 19 , 20 , 21
2.2. Survey construction and administration
Utilizing Sawtooth Software (Lighthouse Studio version 9.2.0, Orem, UT), a conjoint analysis platform was created covering seven attributes integral to the choice of treatment for advanced laryngeal cancer. A list of salient attributes was first determined via review of head and neck oncology qualify‐of‐life literature, 8 , 10 , 22 , 23 and then finalized by head and neck oncologic surgeons at our institution based on their own prior clinical experiences with the laryngeal cancer patient population. This led to the inclusion of the following seven attributes: Lifespan, Treatment Type, Cancer Cure, Self‐Image, Mode of Breathing, Voicing, and Swallowing (see Table 1). When determining the levels for each attribute, we elected to use terms that would be understandable to the general public with minimal to no prior medical knowledge. We additionally elected to determine levels for each attribute based on what would have clinical meaning to participants. For example, to define the various outcomes for the attribute Breathing, we described the levels based on how they would impact participant activity levels as this is a functional outcome that participants can readily understand. Flesch Kincaid grade level was used to assess readability of a sample survey, with a grade level of 6.93.
TABLE 1.
Attributes and levels used in the decision‐making tasks.
| Attribute | Levels |
|---|---|
| Lifespan | Live my expected lifespan. |
| Live 5 years less than my expected lifespan. | |
| Live 10 years less than my expected lifespan. | |
| Live 15 years less than my expected lifespan. | |
| Live 20 years less than my expected lifespan. | |
| Treatment Type | Major surgery, with 2 weeks in the hospital. |
| Major surgery, with 2 weeks in the hospital followed by radiation therapy for 5 weeks. | |
| Chemotherapy as well as radiation therapy for 7 weeks. | |
| Radiation therapy for 7 weeks. | |
| Cancer Cure | 90% chance of cure. |
| 80% chance of cure. | |
| 70% chance of cure. | |
| 60% chance of cure. | |
| 50% chance of cure. | |
| Self‐Image | No change from before treatment. |
| Makes me feel a little worse about my body. | |
| Makes me feel somewhat worse about my body. | |
| Makes me feel much worse about my body. | |
| Mode of Breathing | No limitations on physical exercise. |
| No limitations on physical exercise, but will need a permanent breathing tube (tracheostomy). | |
| Some limitations on physical exercise. | |
| Significant limitations on physical exercise. | |
| Voicing | Normal. |
| 25% decrease in voice quality and/or volume. | |
| 50% decrease in voice quality and/or volume. | |
| 75% decrease in voice quality and/or volume. | |
| Removed completely. Speech and communication would be through non‐verbal means. | |
| Swallowing | Can swallow normally and eat anything I want. |
| Can swallow soft foods with extra effort. | |
| Will need a stomach feeding tube, but still can swallow a little food with effort. | |
| Cannot swallow anything, all nutrition goes through a stomach feeding tube. |
When taking the survey, participants were first presented with a hypothetical scenario in which they were given a diagnosis of advanced cancer of the voice box. They were then presented with a series of 15 choice tasks in which they were asked to indicate which treatment outcome scenario they found the most preferable. Each choice task involved two possible outcome scenarios comparing various options for five attributes; a partial‐profile design was used, with only five of the seven above‐listed attributes included within a single task, to prevent over‐burdening of the participant (Figure 2). Each attribute and attribute level was presented and compared to one another in a randomized manner determined by the software such that each attribute level was equally likely to occur with each level of every other attribute. In addition, attribute levels were included in each task independently of other attribute levels, so that each attribute level's effect (utility) could be measured independently of all other effects. In summary, for survey creation we specified the following within the software: attributes and attribute levels, number of tasks per survey (15), number of outcome scenarios presented within each task (2), and the subset of attributes displayed within any one single‐choice task (5). A sample survey is available for review in the supplemental materials. Once this information was entered into the software, we ran a series of test design simulations in which the software simulates respondent answers and reports the standard errors for main effect size of each attribute and level. We varied the sample size across simulations, starting with n = 300 and sequentially decreasing to the lowest n possible while still achieving standard errors <0.05 for main effect interactions across all attributes and levels. Based on this, a minimum sample size of 260 was established.
FIGURE 2.

Example choice tasks from survey in which participants are asked to choose which treatment option and outcomes they would find more preferable.
This platform was converted to an online survey of choice‐based conjoint tasks administered via portable iPads. Participants were recruited in person from the UCLA Medical Center and the UCLA undergraduate campus. Verbal consent was obtained for each participant who elected to take the survey. Sociodemographic information was collected at the beginning of the survey, including age, sex, smoking history, current profession or retirement status, personal history of head and neck or other type of cancer, and family history of cancer. There was no educational information given to participants prior to starting the survey; however, study personnel were available to answer questions regarding the survey as they came up. Exclusion criteria included subjects under the age of 18, non‐English speakers, and anyone with a personal or immediate family history of head and neck cancer, including laryngeal cancer. This study was exempt from Institutional Review Board approval under Category 2—surveys, interviews, educational tests, public observations.
2.3. Analysis
Average utility scores and individual utility scores were calculated for each attribute using Sawtooth Software. Specifically, using the results of the survey choice tasks, the relative impact of each attribute level on treatment choice was determined using a hierarchical Bayesian estimation. This impact was expressed as the importance, or utility, scores. As detailed in the above section, the standard error for the main effect size of each attribute level was predetermined to be <0.05 based on the survey parameters we previously specified. Statistical analysis was conducted using STATA software (version 17.0; STATA Corp). Univariate analysis was conducted using Fisher's exact tests and one‐way analysis of variance (ANOVA). A Bonferroni correction was used for multiple‐comparisons post‐hoc analysis for statistically significant ANOVA results. For all analyses, p values <.05 were considered significant.
3. RESULTS
Three hundred one healthy adult volunteers (133 male, 167 female, 1 non‐binary) completed the decision‐making program. The mean age of participants was 34.1 (range 18–85) years. Within the group there were 40 (13.2%) active or former tobacco users. Laryngeal cancer treatment attributes were scored with an overall average importance (standard deviation) across the entire cohort as follows: Lifespan 22.2% (±8.5%), Voicing 21.4% (±5.9%), Swallowing 19.1% (±7.3%), Cancer Cure 14.9% (±6.2%), Mode of Breathing 11.0% (±3.7%), Self‐Image 6.7% (±2.9%), and Treatment Type 4.8% (±3.0%) (Figure 3).
FIGURE 3.

Average importance of each attribute across all participants.
The utility of each attribute was also determined on an individual basis for each study participant. Table 2 demonstrates the distribution of participants who found each attribute to have the highest and lowest utility. There was no significant association between gender or history of tobacco use and the distribution of participates assigning each attribute the highest utility and the lowest utility score. There was additionally no association between age and choice of attribute with the highest utility. There was an effect of age on choice of attribute with the lowest utility (p = .039); however, this effect fell away with post‐hoc correction for multiple comparisons. These results are shown in Figures 4 and 5.
TABLE 2.
Number and percentage of participants who assigned each attribute as having the highest and lowest utility.
| Attribute | Highest utility | Lowest utility | ||||
|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |
| Lifespan | 62 (46.6%) | 66 (39.3%) | 128 (42.5%) | 3 (2.3%) | 1 (0.6%) | 4 (1.3%) |
| Breathing | 2 (1.5%) | 0 | 2 (0.07%) | 5 (3.8%) | 7 (4.2%) | 12 (4.0%) |
| Voice | 40 (30.1%) | 54 (32.1%) | 94 (31.2%) | 2 (1.5%) | 1 (0.6%) | 3 (1.0%) |
| Swallow | 23 (17.3%) | 33 (19.6%) | 56 (18.6%) | 1 (0.8%) | 2 (1.2%) | 3 (1.0%) |
| Treatment | 0 | 0 | 0 | 94 (70.7%) | 117 (70.0%) | 211 (70.1%) |
| Cure | 6 (4.5%) | 15 (8.9%) | 21 (7.0%) | 5 (3.8%) | 7 (4.2%) | 12 (4.0%) |
| Self‐Image | 0 | 0 | 0 | 23 (17.3%) | 33 (196%) | 56 (18.6%) |
| Total | 133 | 168 | 301 | 133 | 168 | 301 |
FIGURE 4.
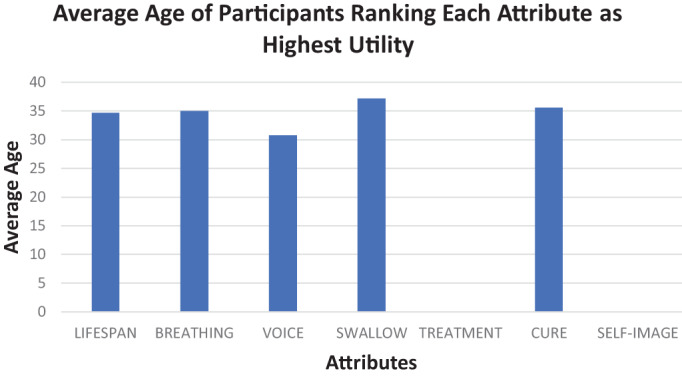
Average age of participants who ranked each attribute as having the highest utility (for Treatment and Self‐Image, there were no participants who ranked them as most important).
FIGURE 5.

Average age of participants who ranked each attribute as having the lowest utility.
4. DISCUSSION
This study sought to investigate the priorities of the general population when deciding treatment for advanced laryngeal cancer. Using choice‐based conjoint analysis, we are able to assess the specific components and attributes of treatment options that most affect this decision.
The results of our investigation demonstrated that while the highest overall importance across the group was assigned to lifespan (22.2%), this is comparable to the second and third highest overall importance values (21.4% for voicing and 19.1% for swallowing). Furthermore, half of the participants (50.5%) considered attributes other than lifespan and cancer cure as most important. These data suggest that the function of the posttreatment anatomy remains important for a majority of the population. These findings are reflective of prior studies, including the original Firefighter's study by McNeil and colleagues and a more recent investigation by Laccourreye et al., who showed that 63% of their study population would consider accepting a reduced chance of cure for preservation of the larynx. 12 , 24 The idea that certain patients would trade off survival years for improved quality of life is particularly salient considering that clinicians may have different values and preferences than patients 22 and emphasizes the importance of careful discussion to establish patient‐specific priorities.
The vast majority (70%) of participants felt that the actual type of treatment (surgical intervention vs. CCRT) was the least important factor in decision making, and none of the participants considered treatment type to be most influential. Thus, the process of undergoing a surgery or having chemoradiation is likely less important than the outcomes and morbidities of these treatment options. Self‐image was additionally found to have low utility across the cohort, and no participants considered a reduction in body image to be the most important factor in the decision‐making process. When taken in the context of the study as a whole, while the low utility does not necessarily indicate that participants do not care about self‐image, it does suggest a lower importance relative to the other attributes. This finding is incongruent with a large body of literature linking body image concerns due to head and neck cancer treatment with depressive symptoms, increased psychological distress, and overall decreased quality of life. 25 , 26 , 27
Of note, participants were not provided any educational material on laryngeal cancer and treatment options prior to taking the survey. The authors elected against this to reflect the knowledge base of patients with newly diagnosed laryngeal cancer who are presenting for their initial consultation, prior to receiving any counseling. Our findings, and particularly the low importance score for Self‐Image, emphasizes the need for in‐depth counseling sessions with patients regarding treatment options and their potential physical and emotional impact in the long term.
When participants are stratified by gender, there are no significant differences between males and females in consideration of attribute utility. There is also no relationship between age and highest utility scores, and while there was a significant association between age and lowest utility scores, this effect did not persist after correcting for multiple comparisons. When looking at overall trends, however, it is interesting to note that average age of those who considered voice most important was younger than that of the other attributes. It is possible that with a larger sample size, trends such as this may become more apparent and more significant differences may be teased out.
There were a number of limitations to this study. The demographics of our population do not align with those of the general public. Our study sample is younger and more female than the laryngeal cancer patient population, and were recruited from a single geographically urban area; the applicability of these findings to this specific population is likely limited by this. However, these findings are consistent with those of the Firefighter's study, which surveyed a smaller, older, and entirely male group. Future studies should aim for a more comprehensive assessment across demographic groups. We additionally did not assess participant education or assumptions regarding treatment types (what laryngectomy and chemoradiation entail) or any of the associated morbidities. Van der Donk et al. has previously shown in a similar investigation of decision making for the treatment of advanced laryngeal cancer that treatment preferences are at least in part influenced by knowledge of treatment modalities. 15 Future studies would benefit from providing a brief overview of these treatment modalities and determining participant understanding prior to beginning the survey, ideally in a manner that mirrors prelaryngectomy and prechemoradiation counseling. We did not include options in the survey for alaryngeal speech, such as tracheoesophageal speech or phonation with an electrolarynx, as these would require presurvey counseling and may not be suitable for every patient. However, these are important components of postlaryngectomy recovery, and adequate counseling about these techniques is crucial prior to choosing a treatment. Finally, regarding survey development, we selected our attributes and levels for inclusion based on the existing literature and clinician review. Although this has served as a good foundation for attribute selection in prior studies, we did not validate our selected attributes using pilot testing with patients. 14 , 20 Although our target population for this study included the general public, future studies would benefit from pilot testing with laryngeal cancer patient to ensure appropriate attribute selection.
Overall, the findings of this study implicate a population with diverse priorities and goals of care. Although this study sought to establish the priorities of the general population as a baseline, we are currently conducting a separate multi‐institutional study examining these decision‐making factors in a patient population that has undergone treatment of laryngeal cancer, with aims to see how their priorities may differ from the general population, as well as based on treatment received. Ultimately, future aims include developing a decision‐making tool that can be used on an individual basis to better clarify patient goals and values prior to making this difficult decision. In addition, we hope to identify specific areas in which patients could be amenable to further counseling and education from providers.
5. CONCLUSION
This study provides new insights into patient decision‐making when choosing treatment for advanced laryngeal cancer. Our data demonstrate that the general public considers voicing considerations and swallowing to be almost equally important as impact on lifespan. Notably, half of all participants found a quality‐of‐life factor (i.e., voicing, swallowing, breathing) as most important, above lifespan or cancer cure. The vast majority of participants found treatment type (laryngectomy vs. chemoradiation) to be the least important variable in their decision, suggesting a need for explicit clinician counseling on what to expect for surgical versus chemoradiation intervention. Similarly, patients placed relatively low utility on body image considerations. This illustrates the diversity in participant values and goals of care and demonstrates the need for individually tailored discussions without assuming patient priorities. These findings aim to shed light on acceptable present‐day trade‐offs in decision making for the treatment of advanced laryngeal cancer, with the goal of facilitating these difficult conversations between physicians and future patients.
FUNDING INFORMATION
Academic grant supporting software access and licensing fees was provided by Sawtooth Software (Sawtooth Software, Inc., Provo, UT). No salary support was provided.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Supporting information
Data S1. Sample survey.
Upton M, Reddy N, Aker M, James K, Wang M, Mendelsohn AH. Laryngeal cancer treatment decision making: A conjoint analysis of general public attitudes and priorities. Laryngoscope Investigative Otolaryngology. 2023;8(4):886‐894. doi: 10.1002/lio2.1103
This study was presented in the podium presentation at AHNS 2021 10th International Conference (virtual).
REFERENCES
- 1. Hoffman HT, Porter K, Karnell LH, et al. Laryngeal cancer in the United States: changes in demographics, patterns of care, and survival. Laryngoscope. 2006;116(S111):1‐3. [DOI] [PubMed] [Google Scholar]
- 2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7‐34. [DOI] [PubMed] [Google Scholar]
- 3. Tamaki A, Miles BA, Lango M, Kowalski L, Zender CA. AHNS series: do you know your guidelines? Review of current knowledge on laryngeal cancer. Head Neck. 2018;40(1):170‐181. [DOI] [PubMed] [Google Scholar]
- 4. Department of Veterans Affairs Laryngeal Cancer Study Group . Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. New Engl J Med. 1991;324(24):1685‐1690. [DOI] [PubMed] [Google Scholar]
- 5. Forastiere AA, Goepfert H, Maor M, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. New Engl J Med. 2003;349(22):2091‐2098. [DOI] [PubMed] [Google Scholar]
- 6. Forastiere AA, Zhang Q, Weber RS, et al. Long‐term results of RTOG 91‐11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer. J Clin Oncol. 2013;31(7):845‐852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lorenzo JG, Martínez VM, Quera AR, et al. Modifications in the treatment of advanced laryngeal cancer throughout the last 30 years. Eur Arch Otorhinolaryngol. 2017;274(9):3449‐3455. [DOI] [PubMed] [Google Scholar]
- 8. Rosenthal DI, Mohamed AS, Weber RS, et al. Long‐term outcomes after surgical or nonsurgical initial therapy for patients with T4 squamous cell carcinoma of the larynx: a 3‐decade survey. Cancer. 2015;121(10):1608‐1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sadoughi B. Quality of life after conservation surgery for laryngeal cancer. Otolaryngol Clin North Am. 2015;48(4):655‐665. [DOI] [PubMed] [Google Scholar]
- 10. Shuman AG, Larkin K, Thomas D, et al. Patient reflections on decision making for laryngeal cancer treatment. Otolaryngol Head Neck Surg. 2017;156(2):299‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lotempio MM, Wang KH, Sadeghi A, Delacure MD, Juillard GF, Wang MB. Comparison of quality of life outcomes in laryngeal cancer patients following chemoradiation vs. total laryngectomy. Otolaryngol Head Neck Surg. 2005;132(6):948‐953. [DOI] [PubMed] [Google Scholar]
- 12. McNeil BJ, Weichselbaum R, Pauker SG. Speech and survival: tradeoffs between quality and quantity of life in laryngeal cancer. New Engl J Med. 1981;305(17):982‐987. [DOI] [PubMed] [Google Scholar]
- 13. Hamilton DW, Bins JE, McMeekin P, et al. Quality compared to quantity of life in laryngeal cancer: a time trade‐off study. Head Neck. 2016;38(S1):E631‐E637. [DOI] [PubMed] [Google Scholar]
- 14. Hamilton DW, Pedersen A, Blanchford H, et al. A comparison of attitudes to laryngeal cancer treatment outcomes: a time trade‐off study. Clin Otolaryngol. 2018;43(1):117‐123. [DOI] [PubMed] [Google Scholar]
- 15. Van der Donk J, Levendag PC, Kuijpers AJ, et al. Patient participation in clinical decision‐making for treatment of T3 laryngeal cancer: a comparison of state and process utilities. J Clin Oncol. 1995;13(9):2369‐2378. [DOI] [PubMed] [Google Scholar]
- 16. Orme BK. Getting Started with Conjoint Analysis: Strategies for Product Design and Pricing Research. Research Publishers LLC; 2006. Accessed January 5, 2023. https://sawtoothsoftware.com/resources/technical-papers/interpreting-conjoint-analysis-data [Google Scholar]
- 17. Hampson LA, Allen IE, Gaither TW, et al. Patient‐centered treatment decisions for urethral stricture: conjoint analysis improves surgical decision‐making. Urology. 2017;99:246‐253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. van Deen WK, Nguyen D, Duran NE, Kane E, van Oijen MG, Hommes DW. Value redefined for inflammatory bowel disease patients: a choice‐based conjoint analysis of patients' preferences. Qual Life Res. 2017;26(2):455‐465. [DOI] [PubMed] [Google Scholar]
- 19. Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403‐413. [DOI] [PubMed] [Google Scholar]
- 20. Naunheim MR, Naunheim ML, Rathi VK, Franco RA, Shrime MG, Song PC. Patient preferences in subglottic stenosis treatment: a discrete choice experiment. Otolaryngol Head Neck Surg. 2018. Mar;158(3):520‐526. [DOI] [PubMed] [Google Scholar]
- 21. Naunheim MR, Randolph GW, Shin JJ. Evidence‐based medicine in otolaryngology part XII: assessing patient preferences. Otolaryngol Head Neck Surg. 2021. Mar;164(3):473‐481. [DOI] [PubMed] [Google Scholar]
- 22. List MA, Stracks J. Evaluation of quality of life in patients definitively treated for squamous carcinoma of the head and neck. Curr Opin Oncol. 2000;12(3):215‐220. [DOI] [PubMed] [Google Scholar]
- 23. Stewart MG, Chen AY, Stach CB. Outcomes analysis of voice and quality of life in patients with laryngeal cancer. Arch Otolaryngol Head Neck Surg. 1998;124(2):143‐148. [DOI] [PubMed] [Google Scholar]
- 24. Laccourreye O, Malinvaud D, Holsinger FC, Consoli S, Ménard M, Bonfils P. Trade‐off between survival and laryngeal preservation in advanced laryngeal cancer: the otorhinolaryngology patient's perspective. Ann Otol Rhinol Laryngol. 2012;121(9):570‐575. [DOI] [PubMed] [Google Scholar]
- 25. Rhoten BA, Deng J, Dietrich MS, Murphy B, Ridner SH. Body image and depressive symptoms in patients with head and neck cancer: an important relationship. Support Care Cancer. 2014;22(11):3053‐3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fingeret MC, Yuan Y, Urbauer D, Weston J, Nipomnick S, Weber R. The nature and extent of body image concerns among surgically treated patients with head and neck cancer. Psychooncology. 2012;21(8):836‐844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fingeret MC, Vidrine DJ, Reece GP, Gillenwater AM, Gritz ER. Multidimensional analysis of body image concerns among newly diagnosed patients with oral cavity cancer. Head Neck. 2010. Mar;32(3):301‐309. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Sample survey.


