Abstract
Context/objective
To investigate predictors of participation enfranchisement of individuals living with spinal cord injury (SCI) who use a wheelchair full-time.
Design
Secondary data analysis of a cross-sectional study.
Setting
Community, United States.
Participants
Participants were 59 wheelchair users (median age of 52.5 years, IQR = 21) with chronic SCI (>1 year after injury).
Interventions
No intervention.
Main outcome measures
Participation enfranchisement was measured using the enfranchisement scale of the Community Participation Indicators (CPI). Dependent variables included importance of participation (CPI-Importance) and control over participation (CPI-Control) subscales of the CPI. Independent variables included demographics and clinical characteristics (age, sex, time since injury, level of injury), wheelchair skills, mobility level, symptoms of depression, and environmental barriers. Backward multivariable linear regression analyses were carried-out to identify predictors of CPI-Importance and CPI-Control.
Results
Five predictors including mobility level, wheelchair skills, sex, level of injury, and symptoms of depression explained 57% (F = 14; P < 0.01) of the variance in CPI-Importance. Three predictors including mobility level, symptoms of depression, and environmental barriers explained 60% (F = 27; P < 0.01) of the variance in CPI-Control.
Conclusion
This study provides evidence of potential modifiable factors such as mobility, wheelchair skills, environmental barriers, and symptoms of depression that can influence importance of participation and control over participation of wheelchair users with SCI. The models presented in this study can serve as a conceptual framework to design effective interventions to improve participation enfranchisement of wheelchair users with SCI.
Keywords: Participation, Spinal cord injury, Mobility, Depression, Barriers, Wheelchair
Introduction
Spinal cord injury (SCI) is a health condition, that can result in significant physical, psychological, and social impairments. The extent of functional ability after a SCI depends on the level and completeness of injury and sociodemographic parameters.1 Due to the variability in the characteristics of the injury and the number of resources in the environment (i.e. facilitators and access to rehabilitation services), the level of independence and mobility vary greatly from one individual with SCI to another. Also, depending on the type of wheelchair (manual vs. power) that individuals with SCI use, the barriers encountered in the community greatly vary.2 At year 1 post-injury, 59.3% of individuals with SCI use a wheelchair for their daily living activities because of mobility limitations.3 Individuals who use a wheelchair full time have reported significant reductions in their societal roles and restrictions in their community participation.4,5
Community participation has been reported as a key factor influencing quality of life (QoL) of individuals with SCI.6 Therefore, meaningful community participation has been viewed by clinicians and researchers as an important rehabilitation goal in order to improve the QoL of individuals with SCI.7 To successfully develop interventions, allocate resources, and develop services to improve community participation in this population, it is crucial to better understand those factors that influence community participation after SCI.
In the last decade, several studies have investigated potential predictors of community participation in individuals living with SCI.4,5,8,9 The studies highlighted a variety of factors associated with community participation.4 Researchers have identified as predictors, level and severity of injury,8,9 sociodemographic information (i.e. age, sex, marital status, employment, education),8,10 mobility limitations and reduced functional independence,11,12 environmental barriers,13 and psychological measures.14 The studies have developed and presented multivariable regression models that were only able to explain 1.8–29% of the variance in community participation.8–10,13 The need to develop more accurate models with specific predictors that will be able to explain a higher percentage of the variance in community participation in this population is evident. In addition, most measurement approaches of community participation utilized in the studies have focused on the frequency with which individuals engage in community activities and/or difficulty that they experience with those activities.8–10,13 However, from the perspective of individuals with disabilities, community participation is defined as a sense of inclusion and membership within the community.15 These concepts of sense of inclusion and membership in the community labeled “enfranchisement” are not well-represented in most current outcome measures of community participation.15,16 Based on this information, Heinemann et al. developed the enfranchisement scale of the Community Participation Indicator (CPI), a dimension of community participation that includes the context and personal significance factors of community participation.17 Exploring predictors of participation enfranchisement will help clinicians to develop specific interventions to improve the quality of community participation.
Moreover, most studies investigating predictors of community participation of individuals living with SCI have not focused on wheelchair users, rather, individuals who ambulate and those who use a wheelchair were analyzed together in the studies.8,9 Significant differences exist between individuals who ambulate and those who use a wheelchair in terms of functional abilities, skills needed to operate a mobility aid (i.e. wheelchair vs. walker), and environmental barriers. Among wheelchair users in general, a review indicated that wheelchair factors, accessibility, skills with wheelchair use, pain, finances, and education have been reported to be associated with participation.18 To the best of our knowledge, only wheelchair skills,12 shoulder pain,19 and satisfaction with the wheelchair20 have been separately investigated as predictors of community participation among wheelchair users with SCI. To date, no study has specifically investigated predictors of participation enfranchisement among wheelchair users with SCI. Since community participation is multidimensional, investigating a broad range of predictors including for example, environmental barriers4 and psychological measures14 might provide more useful findings that are more clinically relevant. Therefore, the purpose of the current study was to determine predictors of participation enfranchisement among wheelchair users with SCI using a broad range of potential predictors. The authors hypothesized that low functional mobility levels, poor wheelchair skills, the presence of significant environmental barriers, and symptoms of depression will be associated with low participation enfranchisement.
Methods
Participants
This is a secondary data analysis of data collected as part of a research study aiming to investigate factors associated with falls among wheelchair users with SCI.21 Participants were recruited from SCI support groups across the US, Facebook SCI groups, personal communication, and magazine/newsletter advertisements. Readers were invited to take part in the study if they met the following inclusion criteria: (1) 18 years old or over with a chronic SCI after at least 12 months after injury; (2) motor complete injury classified as American Spinal Injury Association Impairment Scale (AIS) A or B and motor incomplete injury AIS C who are wheelchair users; (3) level of injury between C5 and L5; (4) self-report use of a wheelchair for at least 75% of mobility, and (5) able to read and understand English. Participants were excluded if they were classified as AIS D or E.
Procedures
Initially, potential participants who were interested in the study contacted the research team and were screened against the eligibility criteria. Those who met the eligibility criteria signed an online informed consent and were enrolled in the study. Then, a researcher sent a link to the participants to complete the outcome measures noted below through a survey. All the outcome measures were self-reported and collected between January and July 2021 using the Research Electronic Data Capture (REDCap)22 survey platform. The Institutional Office for the Protection of Research Subjects (#20718) reviewed the procedures and approved the study.
Measures
The variables included as potential predictors were selected based on the results from previous studies indicating environmental barriers,4 wheelchair skills,12 psychological measures,14 and mobility11 were the most important factors that influence community participation among individuals with SCI.
Dependent variable
Participation enfranchisement was assessed using the enfranchisement scale of the CPI.17 The enfranchisement scale of the CPI was used because it encompasses the context and personal significance factors of community participation as opposed to many other measures that only evaluate the difficulty or frequency of involvement in selected community activities.16,17 This scale evaluates participation enfranchisement of people with disabilities using two subscales: importance of participation and control over participation. The scale was developed by Heinemann et al. who initially identified four factors of CPI labeled as (1) importance and meaning of participation; (2) social connections, inclusion, and membership; (3) control over participation; and (4) access to transportation and communication services.17 A bifactor model conducted by the authors suggested a single CPI component.17 However, a final Rasch model supported the independence and unidimensionality of two final subscales: 14 importance and 13 control items.17 Importance refers to the feelings of being valued by the community and contributing to the community.16 Control measures the sense of choice and control over community participation.16 The 14 importance and 13 control items are presented in Appendix A, respectively. Items are measured on a 1–5 scale and summed to get a total score for each subscale. CPI-Importance raw score ranges from 14 to 70 and CPI-Control subscale raw score ranges from 13 to 65. Raw scores are converted into a percentage score varying from 0 to 100. Higher percentages indicate higher levels of participation for each domain.17 The Cronbach’s α used to assess the internal consistency reliability of both subscales of the participation enfranchisement scale is 0.91.17 Convergent validity between the participation enfranchisement scale and participation ability measure was also demonstrated among individuals with disabilities including SCI, stroke, and traumatic brain injury (Importance subscale r = 0.52 and Control subscale r = 0.56).16
Independent variables
Demographics and characteristics of SCI: participants reported their age, sex, time since injury, and level of injury. Level of injury was classified into 4 categories including cervical injuries (C3–C8), high thoracic (T1–T7), low thoracic (T8–T12), lumbar (L1–L5).
Mobility: participants reported their level of mobility using the sub-score (SCIM-Mobility) of the Spinal Cord Independence Measure (SCIM) III.23 The intraclass correlation coefficients (ICC) of the SCIM III and its domains is >0.94 and the Cronbach’s α used to evaluate the internal consistency reliability is >0.7.23 SCIM-Mobility scores vary from 0 to 40. Higher scores indicate greater mobility levels.23
Psychological measures: the Hospital Anxiety and Depression Scale (HADS) was used to assess symptoms of depression and anxiety.24 Only the HADS-Depression sub-score that evaluates how the individual felt during the last week was used in the regression model. HADS-Anxiety was not associated with any CPI subscale and was not included in the models. A HADS-Depression subscale score >8 denotes depressive mood. The Cronbach’s α used to evaluate the internal consistency reliability of the HADS-Depression among individuals with SCI is 0.74.25
Wheelchair skills: participants’ performance of power or manual wheelchair skills were assessed using the Wheelchair Skills Test 5.0 questionnaire (WST-Q).26 Only the WST-Q performance component of the WST-Q was used in the regression model to avoid collinearity of independent variables. The WST-Q performance measures the use of wheelchair skills in everyday life. Higher percentages indicate greater performance of wheelchair skills. The ICC reported for the WST-Q is 0.99.27
Environmental barriers: The 12 items of the Craig Hospital Inventory of Environmental Factors-short form (CHIEF-SF) was used to quantify perceived environmental barriers.28 The CHIEF-SF is a subjective measure that comprehensively assesses the frequency and magnitude of barriers that keep people from doing what they need or want to do.28 The CHIEF-SF quantifies environmental barriers experienced within five domains including: policies, physical and structural, work and school, attitudes and support, and services and assistance.28 The Cronbach’s α used to evaluate the internal consistency reliability of the CHIEF-SF for the 5 domains varies from 0.62 to 0.93 among the general population and individuals with disabilities including SCI.28 Each CHIEF-SF item measures two domains pertaining to the frequency of an environmental barrier (from 0 = never to 4 = daily) and the magnitude of the effect of this problem (1 = little problem or 2 = a big problem), with a range in score product of the frequency and magnitude of the problem scores) from 0 to 8.28 Total score across the 12 items was calculated as the average of the frequency-magnitude product score across all the scale items.28 Higher scores indicate greater frequency and/or magnitude of environmental barriers.
Statistical analyses
Sample size calculation was carried out using the G-power software.29 In order to include 5 independent variables in the multivariable regression analyses, a minimum of 58 individuals would be required considering an effect size of 0.25 for all predictors combined, an alpha level of 0.05, and a power of 0.80.29
Tests for normality were conducted for all variables and due to the non-normal distribution of the data, descriptive statistics (medians, IQRs, and proportions) were reported to characterize the sample. Initial and final multivariable linear regression models were created separately for the subscales CPI-Importance and CPI-Control using backward stepwise multivariable linear regression analyses. The backward regression method was preferred compared with other methods because it estimates the joint predictive ability of included variables and removes the least important variables early on in the model.30 All potential predictors with a P value < 0.10 from the initial model were included in the final model. The following were inspected to ensure there were no violations of the assumptions of multiple linear regression: normality of residuals (visual inspection of histograms and data plots), independence of the residuals (Durbin-Watson’s test: values close to 2), linearity and homoscedasticity (plots of the standardized residuals against the standardized predicted values), multicollinearity (variance inflation factor-VIF average not substantially > 1), and influential outliers (Cook’s distance > 1).
Variable entry for the models was set at ≤0.05 and removal was set at ≥0.10. All analyses were performed using SPSS for Macintosh, Version 25.0, SPSS Inc. Chicago, IL, USA.
Results
Participant’s characteristics
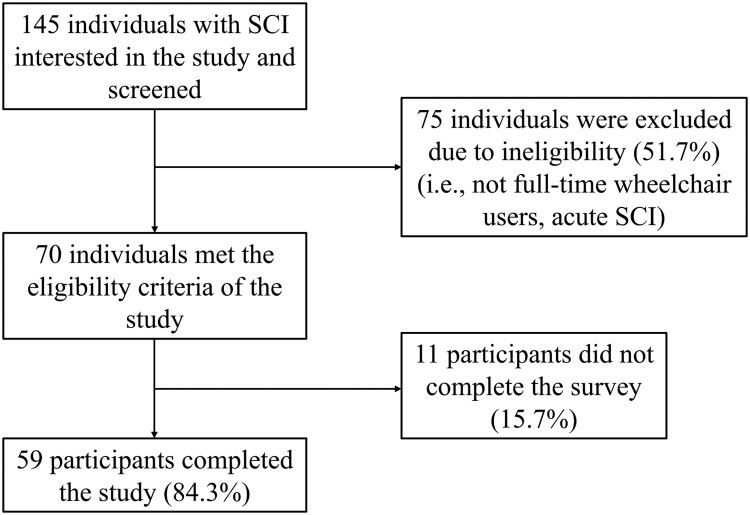
Of a total of 145 individuals, 75 did not meet the inclusion criteria. In total, 70 individuals met the eligibility criteria and agreed to participate, but 11 did not complete the demographic information and outcome measures and were excluded. Therefore, 59 participants, who had a median age of 53 years (IQR 21), 48% male, and a median time since injury of 17 years (IQR 27.25) were included. A flow diagram of the participants is presented in Figure 1. Clinical and demographic characteristics of the participants are presented in Table 1. Briefly, our sample presented with similar participation enfranchisement (CPI-control: 55 vs. 58.4) and (CPI-Importance: 50 vs. 48.3) compared with individuals with disabilities including SCI, stroke, and traumatic brain injury.16 Participants in our sample also reported similar level of mobility and depressive mood compared with previous cohorts of wheelchair users with SCI (SCIM III-Mobility: 16 vs. 16.2)31 and (HADS-Depression 5 vs. 5.5),25 respectively. However, participants in our study reported lower wheelchair skills performance and environmental barriers compared to previously reported samples of wheelchair users with SCI (WST-Q performance: 65 vs. 76)32 and (CHIEF-SF: 1.75 vs. 3), respectively.33
Figure 1.
Flowchart of the study participants.
Table 1.
Clinical and demographics characteristics of the participants.
| Characteristic | n = 59 |
|---|---|
| Age (years), median (IQR) Male Female |
53 (21) 53 (25) 50 (20) |
| Sex (male), (%) | 48 |
| Race/ethnicity, (%) Asian African American Caucasian Hispanic |
5 10 81 4 |
| Height (cm), median (IQR) | 172 (17) |
| Weight (Kg), median (IQR) | 75 (27) |
| Cause of SCI, (%) Traumatic Non-traumatic |
73 27 |
| Time since injury (years), median (IQR) | 17 (27) |
| Level of injury, (%) Cervical High thoracic Low thoracic Lumbar Unknown |
22 25 37 9 7 |
| SCIM-Mobility score, median (IQR) | 16 (6) |
| HADS-Depression, median (IQR) | 5 (5) |
| WST-Q performance, median (IQR) | 65 (31) |
| CHIEF-SF, median (IQR) | 1.75 (1.33) |
| CPI-Importance, median (IQR) | 50 (15) |
| CPI-Control, median (IQR) | 55 (8) |
IQR: interquartile range; CHIEF-SF: Craig Hospital Inventory of Environmental factors- Short Form; CPI: Community Participation Indicators; HADS: Hospital Anxiety and Depression Scale; SCIM III: Spinal Cord Injury Measures III; WST-Q: Wheelchair Skills Test Questionnaire.
Predictors of participation enfranchisement
For the CPI-Importance model, the initial regression analysis indicated that five potential predictors, sex, SCIM-Mobility, HADS-Depression, WST-Q performance, and level of injury presented with a P < 0.10 (Table 2). The final model including these five predictors explained 57% (F = 14; P < 0.01) of the variance in CPI-Importance (Table 3). SCIM-Mobility, sex, and WST-Q performance scores positively correlated, whereas HADS-Depression scores and level of injury correlated negatively with CPI-Importance.
Table 2.
Initial backward regression model of potential predictors of community participation assessed by the importance and control over participation domains of the CPI.
| Community participation | Model | B | 95% CI for B | β | P value |
|---|---|---|---|---|---|
| CPI-importance | Constant Age Sex (male) Level of injury Time since injury SCIM-mobility HADS-depression WST-Q performance CHIEF-SF |
47.8 ± 11.0 –0.1 ± 0.1 5.9 ± 3.2 –3.9 ± 1.3 0.1 ± 0.1 0.1 ± 0.4 –2.1 ± 0.5 0.1 ± 0.1 0.1 ± 0.1 |
25.6 to 69.9 –0.3 to 0.2 –0.5 to 12.3 –6.6 to –1.1 –0.2 to 0.2 0.1 to 1.8 0.1 to 1.8 –0.1 to 0.3 –0.2 to 0.3 |
– –0.1 0.2 –0.3 0.1 0.3 –0.6 0.2 0.1 |
<0.01 0.88 0.07 <0.01 0.66 0.02 <0.01 0.08 0.88 |
| CPI-control | Constant Age Sex (male) Level of injury Time since injury SCIM-mobility HADS-depression WST-Q performance CHIEF-SF |
59.2 ± 10.6 –0.1 ± 0.1 4.8 ± 3.1 –2.7 ± 1.3 0.1 ± 0.1 0.1 ± 0.4 –2.1 ± 0.4 0.1 ± 0.1 0.2 ± 0.1 |
37.8 to 80.6 –0.3 to 0.2 –1.3 to 11.0 –5.3 to –0.1 –0.1 to 0.2 0.1 to 1.7 –3.0 to –1.3 –0.1 to 0.3 –0.5 to 0.1 |
– –0.1 –0.1 –0.2 0.1 0.3 –0.5 0.2 –0.2 |
<0.01 0.81 0.12 0.05 0.61 0.02 <0.01 0.07 0.08 |
CHIEF-SF: Craig Hospital Inventory of Environmental factors-Short Form; CPI: Community Participation Indicators; HADS: Hospital Anxiety and Depression Scale; SCIM III: Spinal Cord Injury Measures III; WST-Q: Wheelchair Skills Test Questionnaire.
Table 3.
Final model of potential predictors of community participation assessed by the importance and control over participation domains of the CPI.
| Community participation | R2 | Model | B | 95% CI for B | β | P value |
|---|---|---|---|---|---|---|
| CPI-importance | 0.57 | Constant SCIM-mobility HADS-depression WST-Q performance Level of injury Sex (Male) |
46.8 ± 7.5 1.0 ± 0.37 –2.1 ± 0.4 0.2 ± 0.1 –3.9 ± 1.3 6.6 ± 2.9 |
31.8 to 61.9 0.2 to 1.7 –2.9 to –1.3 0.1 to 0.3 –6.5 to –1.3 0.8 to 12.4 |
– 0.3 –0.6 0.2 –0.3 0.2 |
<0.01 0.01 <0.01 0.04 <0.01 0.03 |
| CPI-control | 0.60 | Constant SCIM-mobility HADS-depression CHIEF-SF |
70.6 ± 5.6 0.6 ± 0.3 –2.4 ± 0.4 –0.2 ± 0.1 |
59.4 to 81.9 –0.1 to 1.2 –3.2 to –1.5 –0.4 to –0.1 |
– 0.2 –0.6 –0.2 |
<0.01 0.06 <0.01 0.04 |
CHIEF-SF: Craig Hospital Inventory of Environmental factors-Short Form; CPI: Community Participation Indicators; HADS: Hospital Anxiety and Depression Scale; SCIM III: Spinal Cord Injury Measures III; WST-Q: Wheelchair Skills Test Questionnaire.
For the CPI-Control domain’s model, the initial regression analysis indicated that the following five potential predictors: level of injury, WST-Q performance, SCIM-Mobility, CHIEF-SF, and HADS-Depression presented with a P < 0.10 (Table 2). The final model revealed three predictors, SCIM-Mobility, CHIEF-SF, and HADS-Depression, that explained 60% (F = 27; P < 0.01) of the variance in CPI-Control (Table 3). HADS-Depression and CHIEF-SF scores negatively correlated, whereas SCIM-Mobility score correlated positively with CPI-Control.
Discussion
The purpose of the study was to identify factors influencing participation enfranchisement of wheelchair users with SCI living in the United States. This study is novel because it is the first study that investigated predictors of participation enfranchisement specifically among wheelchair users with SCI. The data presented were obtained during the COVID-19 pandemic when engagement in social and community activities were impacted for most people including people with SCI. Our findings indicate that potential modifiable factors such as mobility level, symptoms of depression, wheelchair skills, and environmental barriers should be emphasized when developing interventions to enhance participation enfranchisement among wheelchair users with SCI. Non-modifiable factors such as sex and level of injury of these individuals should also be considered in developing these interventions.
To the best of our knowledge, this is the first study analyzing a combination of a broad range of predictors of participation enfranchisement using specific domains of the CPI among wheelchair users living with SCI. Our findings highlighted that men with higher mobility levels, higher wheelchair skills, reduced symptoms of depression, and lower injury levels give higher importance to community participation. The level of functional ability has played an important role in this model. Individuals with lower injury levels present with better dynamic sitting stability when compared with individuals with higher thoracic SCI34,35 which might lead to a higher level of mobility, wheelchair skills, and functional performance.36 Individuals with higher functional ability may engage in more community-based activities, such as being employed outside of the home,10 that increases their perceived importance of community participation. In fact, Suttiwong et al.37 presented functional performance as one of the significant predictors of community participation in individuals with SCI. Hosseini et al. also indicated that manual wheelchair users with SCI with the ability to perform wheelchair skills presented with better community participation and life satisfaction.12 Beaudoin et al. recently found that better wheelchair skills were associated with improvement of community participation of wheelchair users with various disabilities including individuals with SCI.38 These findings corroborate with our results highlighting the role of functional ability in the importance of community participation among wheelchair users with SCI.
In addition to the functional abilities in a wheelchair, sex, and the level of injury, our study also found that reduced symptoms of depression predicted importance of community participation in this population. The findings align with the results by Geyh et al. who also showed a negative correlation between the presence of depressive symptoms with participation of individuals with SCI.14 The combination of the predictors presented in our model explained 57% of the variance in the importance of participation enfranchisement among the individuals in our sample. Our model explained a high percentage of the variance in the importance of community participation, which is better than the prediction models previously reported that explained 1.8 to 29% in community participation among ambulatory individuals and wheelchair users with SCI.8–10,13 Our finding suggests that clinicians and researchers aiming to enhance the importance of community participation among wheelchair users with SCI should focus on improving their functional independence (i.e. wheelchair skills training, transfer training) and treat any symptoms of depression in this population. Interventional studies are needed to confirm our findings.
Control over participation was another participation enfranchisement domain investigated in our study. The findings highlight an association between control over participation and symptoms of depression and environmental barriers. A trend to significance was also observed for mobility level (P = 0.06). Besides the association between participation enfranchisement, mobility level, and depressive mood discussed above, wheelchair users with SCI expressed an increased control over their ability to participate in their community when there are less environmental barriers. Environmental barriers have also been associated with community participation in individuals with SCI in a previous study.13 Also, challenges related to accessibility of home and public buildings and transportation have been reported as factors limiting community participation in individuals with SCI.4 The measure of environmental barriers (CHIEF-SF) used in our study asks participants to evaluate, in addition to physical and structural barriers, other aspects related to policies, work and school, attitudes and support, and services and assistance.28 Minimizing barriers associated with accessibility, policies, work and school, attitudes and support, and services and assistance may enhance the ability of wheelchair users to have a higher level of control over their community participation. Therefore, it seems evident that improving wheelchair skills, treating symptoms of depression, and minimizing environmental barriers may enhance control over community participation. The combination of the predictors presented in our study explains 60% of the variance in control over participation of wheelchair users with SCI. Our model explained a high percentage of the variance in control over participation, which is better than the prediction models previously reported that explained 1.8 to 29% in community participation among ambulatory individuals and wheelchair users with SCI.8–10,13 Our finding indicates that the model developed to inform about the predictors of control over participation in our study can be used to develop interventions to enhance participation enfranchisement in this population. Accounting for experiences of wheelchair users with SCI to improve their quality of community participation is highly recommended.39,40
Limitations
There are some limitations in this study that need to be highlighted. First, as this study is a secondary data analysis and the data presented were not originally collected to verify the hypothesis established in this report, the number of predictors included in this study was limited to the available data. Other potential predictors such as employment status, pain, finances, education, pressure ulcers, and spasticity were not analyzed in our study. Also, our linear regression analysis was conducted just with the minimum sample required. We believe that a broader sample size would provide more precise estimates (i.e. narrower confidence intervals). Another limitation that may hinder the evaluation of the representativeness of our sample and the generalizability of our findings is related to the low percentage of male full-time wheelchair users included in our study (48%). This percentage is lower than the national US average of all new SCI cases that are males (approximately 78%).3 However, to the best of our knowledge, no data exists on the percentage and demographics of male full-time wheelchair users living with SCI to provide a fair comparison with our data. Also, the study was conducted only in the United States limiting its applicability to other countries where the culture, healthcare policies, environmental barriers, and resources are certainly different. Finally, as there are differences in barriers associated with community participation experienced by manual and power wheelchair users,2 failing to make the distinction between manual and power wheelchair users in this study should be considered a limitation.
Conclusions
In summary, mobility level, wheelchair performance, environmental barriers, and symptoms of depression were found as potential modifiable factors influencing participation enfranchisement defined by importance and control over participation of wheelchair users with SCI. Participation enfranchisement is an important domain of community participation. Because of the unique characteristics of wheelchair users compared to ambulatory individuals, these findings provide useful information for the development of interventions to enhance community participation in this population. Healthcare policymakers should take these predictors into consideration to improve the efficiency of rehabilitation services to enhance community participation among wheelchair users living with SCI. Future longitudinal studies with bigger sample size are warranted to further consolidate the predictors of participation enfranchisement presented in this study.
Disclaimer statements
Funding This work was supported by the Illinois Physical Therapy Association [grant number IPTF 098442].
Conflicts of interest The authors report no conflicts of interest.
Appendix A.
Items of the CPI-Importance and their response options
Please mark the choice that most closely reflects your opinion:
| Items | All the time | Frequently | Sometimes | Seldom | Almost never |
|---|---|---|---|---|---|
| I participate in a variety of activities | |||||
| I spend time things that improve my community | |||||
| I spend time helping others | |||||
| I regularly seek out new challenges | |||||
| I have a say on decisions in my community | |||||
| I contribute to society | |||||
| I assume leadership roles in organizations | |||||
| I do important things with my life | |||||
| I have influence in my community | |||||
| I feel safe participating in community activities | |||||
| People see my potential | |||||
| People count on me | |||||
| I contribute to the well-being of my community | |||||
| I am actively involved in my community |
Items of the CPI-Control and their response options
Please mark the choice that most closely reflects your opinion:
| Items | All the time | Frequently | Sometimes | Seldom | Almost never |
|---|---|---|---|---|---|
| I live my life the way that I want | |||||
| I participate in activities that I choose | |||||
| I have the freedom to make my own decisions | |||||
| I live my life fully | |||||
| I have choices about the activities I do | |||||
| I actively pursue my dreams and desires | |||||
| I do things that are important to me | |||||
| I am able to go out and have fun | |||||
| I have opportunities to make new friends | |||||
| I take responsibility for my own life | |||||
| I am in control of my own life | |||||
| I have control over how I spend my time | |||||
| I participate in activities when I want |
References
- 1.Aidinoff E, Front L, Itzkovich M, et al. Expected spinal cord independence measure, third version, scores for various neurological levels after complete spinal cord lesions. Spinal Cord 2011;49(8):893–896. [DOI] [PubMed] [Google Scholar]
- 2.Hastings J, Robins H, Griffiths Y, Hamilton C.. The differences in self-esteem, function, and participation between adults with low cervical motor tetraplegia who use power or manual wheelchairs. Arch Phys Med Rehabil 2011;92(11):1785–1788. [DOI] [PubMed] [Google Scholar]
- 3.The NSCISC 2020 Annual Statistical Report. University of Alabama at Birmingham; 2020. https://www.nscisc.uab.edu/public/2020%20Annual%20Report%20-%20Complete%20Public%20Version.pdf.
- 4.Kashif M, Jones S, Darain H, Iram H, Raqib A, Butt AA.. Factors influencing the community integration of patients following traumatic spinal cord injury: a systematic review. J Pak Med Assoc 2019;69(9):1337–1343. [PubMed] [Google Scholar]
- 5.Barclay L, McDonald R, Lentin P.. Social and community participation following spinal cord injury: a critical review. Int J Rehabil Res 2015;38(1):1–19. [DOI] [PubMed] [Google Scholar]
- 6.Barker RN, Kendall MD, Amsters DI, Pershouse KJ, Haines TP, Kuipers P.. The relationship between quality of life and disability across the lifespan for people with spinal cord injury. Spinal Cord 2009;47(2):149–155. [DOI] [PubMed] [Google Scholar]
- 7.Gómara-Toldrà N, Sliwinski M, Dijkers MP.. Physical therapy after spinal cord injury: a systematic review of treatments focused on participation. J Spinal Cord Med 2014;37(4):371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whiteneck G, Tate D, Charlifue S.. Predicting community reintegration after spinal cord injury from demographic and injury characteristics. Arch Phys Med Rehabil 1999;80(11):1485–1491. [DOI] [PubMed] [Google Scholar]
- 9.Kader M, Perera NKP, Sohrab Hossain M, Islam R.. Socio-demographic and injury-related factors contributing to activity limitations and participation restrictions in people with spinal cord injury in Bangladesh. Spinal Cord 2018;56(3):239–246. [DOI] [PubMed] [Google Scholar]
- 10.Carr JJ, Kendall MB, Amsters DI, et al. Community participation for individuals with spinal cord injury living in Queensland, Australia. Spinal Cord 2017;55(2):192–197. [DOI] [PubMed] [Google Scholar]
- 11.Oyster ML, Karmarkar AM, Patrick M, Read MS, Nicolini L, Boninger ML.. Investigation of factors associated with manual wheelchair mobility in persons with spinal cord injury. Arch Phys Med Rehabil 2011;92(3):484–490. [DOI] [PubMed] [Google Scholar]
- 12.Hosseini SM, Oyster ML, Kirby RL, Harrington AL, Boninger ML.. Manual wheelchair skills capacity predicts quality of life and community integration in persons with spinal cord injury. Arch Phys Med Rehabil 2012;93(12):2237–2243. [DOI] [PubMed] [Google Scholar]
- 13.Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB.. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil 2004;85(11):1793–1803. [DOI] [PubMed] [Google Scholar]
- 14.Geyh S, Nick E, Stirnimann D, et al. Self-efficacy and self-esteem as predictors of participation in spinal cord injury–an ICF-based study. Spinal Cord 2012;50(9):699–706. [DOI] [PubMed] [Google Scholar]
- 15.Hammel J, Magasi S, Heinemann A, Whiteneck G, Bogner J, Rodriguez E.. What does participation mean? An insider perspective from people with disabilities. Disabil Rehabil 2008;30(19):1445–1460. [DOI] [PubMed] [Google Scholar]
- 16.Kersey J, Terhorst L, Heinemann AW, et al. Construct validity of the enfranchisement scale of the community participation indicators. Clin Rehabil 2022;36(2):263–271. [DOI] [PubMed] [Google Scholar]
- 17.Heinemann AW, Magasi S, Bode RK, et al. Measuring enfranchisement: importance of and control over participation by people with disabilities. Arch Phys Med Rehabil 2013;94(11):2157–2165. [DOI] [PubMed] [Google Scholar]
- 18.Smith EM, Sakakibara BM, Miller WC.. A review of factors influencing participation in social and community activities for wheelchair users. Disabil Rehabil Assist Technol 2016;11(5):361–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gutierrez DD, Thompson L, Kemp B, Mulroy SJ.. The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med 2007;30(3):251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Groot S, Post MW, Bongers-Janssen HM, Bloemen-Vrencken JH, van der Woude LH.. Is manual wheelchair satisfaction related to active lifestyle and participation in people with a spinal cord injury? Spinal Cord 2011;49(4):560–565. [DOI] [PubMed] [Google Scholar]
- 21.Abou L, Rice LA.. Risk factors associated with falls and fall-related injuries among wheelchair users with spinal cord injury. Arch Rehabil Res Clin Transl 2022: 100195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Itzkovich M, Gelernter I, Biering-Sorensen F, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil 2007;29(24):1926–1933. [DOI] [PubMed] [Google Scholar]
- 24.Zigmond AS, Snaith RP.. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
- 25.Woolrich RA, Kennedy P, Tasiemski T.. A preliminary psychometric evaluation of the Hospital Anxiety and Depression Scale (HADS) in 963 people living with a spinal cord injury. Psychol Health Med 2006;11(1):80–90. [DOI] [PubMed] [Google Scholar]
- 26.Kirby R, Rushton P, Smith C, et al. Wheelchair skills program manual version 5.0. 2019. www.wheelchairskillsprogram.ca/eng/manual.php.
- 27.Passuni D, Dalzotto E CFG, et al. Reliability of the Spanish version of the wheelchair skills test 4.2 for manual wheelchair users with spinal cord injury. Disabil Rehabil Assist Technol 2019;14(8):788–791. [DOI] [PubMed] [Google Scholar]
- 28.Whiteneck GG, Harrison-Felix CL, Mellick DC, Brooks CA, Charlifue SB, Gerhart KA.. Quantifying environmental factors: a measure of physical, attitudinal, service, productivity, and policy barriers. Arch Phys Med Rehabil 2004;85(8):1324–1335. [DOI] [PubMed] [Google Scholar]
- 29.Faul F, Erdfelder E, Lang AG, Buchner A.. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- 30.Chowdhury MZI, Turin TC.. Variable selection strategies and its importance in clinical prediction modelling. Fam Med Community Health 2020;8(1):e000262–e000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khamnon N, Amatachaya S, Wattanapan P, et al. Reliability and concurrent validity of the Spinal Cord Independence Measure III among rehabilitation professionals. Spinal Cord 2022: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirby RL, Worobey LA, Cowan R, et al. Wheelchair skills capacity and performance of manual wheelchair users with spinal cord injury. Arch Phys Med Rehabil 2016;97(10):1761–1769. [DOI] [PubMed] [Google Scholar]
- 33.Callahan MK, Cowan RE.. Relationship of fitness and wheelchair mobility with encounters, avoidances, and perception of environmental barriers among manual wheelchair users with spinal cord injury. Arch Phys Med Rehabil 2018;99(10):2007–2014. [DOI] [PubMed] [Google Scholar]
- 34.Chen CL, Yeung KT, Bih LI, Wang CH, Chen MI, Chien JC.. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil 2003;84(9):1276–1281. [DOI] [PubMed] [Google Scholar]
- 35.Abou L, Sung J, Sosnoff JJ, Rice LA.. Reliability and validity of the function in sitting test among non-ambulatory individuals with spinal cord injury. J Spinal Cord Med 2020;43(6):846–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abou L, Rice LA.. The associations of functional independence and quality of life with sitting balance and wheelchair skills among wheelchair users with spinal cord injury. J Spinal Cord Med 2022: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suttiwong J, Vongsirinavarat M, Chaiyawat P, Vachalathiti R.. Predicting community participation after spinal cord injury in Thailand. J Rehabil Med 2015;47(4):325–329. [DOI] [PubMed] [Google Scholar]
- 38.Beaudoin M, Best KL, Raymond É, Routhier F.. Influence of Roulez avec confiance, a peer-led community-based wheelchair skills training program, on manual wheelchair users. Disabil Rehabil Assist Technol 2021: 1–8. [DOI] [PubMed] [Google Scholar]
- 39.Giroux EE, Casemore S, Clarke TY, McBride CB, Wuerstl KR, Gainforth HL.. Enhancing participation while aging with spinal cord injury: applying behaviour change frameworks to develop intervention recommendations. Spinal Cord 2021;59(6):665–674. [DOI] [PubMed] [Google Scholar]
- 40.Martin Ginis KA, Evans MB, Mortenson WB, Noreau L.. Broadening the conceptualization of participation of persons With physical disabilities: a configurative review and recommendations. Arch Phys Med Rehabil 2017;98(2):395–402. [DOI] [PubMed] [Google Scholar]