Abstract
The primary purpose of this study was to evaluate acute dose response of different intensities with total volume equalized during the abdominal crunch exercise on muscle thickness, echo-intensity, peak force, time under tension, total load lifted, and perception of effort in recreationally-trained participants. Fifteen resistance-trained participants (23 ± 3 years) performed the abdominal crunch exercise in one of two different resistance training (RT) protocols in a randomized order: RT4×10RM (4 sets of 10RM / 1-min rest) or RT1×40RM (1 set of 40RM). Muscle thickness (MT), echo-intensity (EI), peak force (PF), time under tension (TUT), total load lifted (TLL), and session rating of perceived exertion (sRPE) were measured pre-test and post-test (0-min and 15-min). Two-way repeated-measures ANOVAs (2 × 3) were used to test differences between RT protocols (RT4×10RM and RT1×40RM) and time (pre-test, post-0, and post-15) for MT, EI, and PF. Paired t-test was used to compare RT protocols for sRPE, TLL, and TUT. For MT, there were significant differences for RT4×10RM between pre-x post-0 (p = 0.011), pre-x post-15 (p < 0.001), and post-0 × post-15 (p = 0.02); and for RT1×40RM between pre-x post-0 (p < 0.001) and pre-x post-15 (p = 0.003). For EI, there was a significant difference for RT4×10RM between pre-x post-0 (p = 0.002). For sRPE, there was no significant difference between RT protocols. For TLL and TUT, there were significant differences between RT protocols (p < 0.05). In conclusion, both RT protocols (RT4×10RM and RT1×40RM) induced similar increases in MT but not for EI. TLL and TUT were higher for RT4×10RM. PF and sRPE were similar between RT protocols.
Keywords: Strength, muscular performance, muscle pump
INTRODUCTION
It is well established that training of the abdominal muscles can contribute to the movement and stabilization of the trunk, alleviate the symptoms of chronic low back pain, prevent injuries, and possibly maximize sports performance (2, 28). Thus, abdominal exercises are often incorporated into resistance training (RT) programs aimed at different objectives such as performance, quality of life and health, and rehabilitation (2, 22, 24, 25). Superficial muscles like the rectus abdominis (RA) are the main contributors to abdominal exercises (12) and their main functions are to flex the trunk on a fixed pelvis, to flex the pelvis on a fixed trunk (9), or to contribute to trunk stability (28, 29, 39). Despite the rich scientific literature on muscle recruitment in abdominal exercises (8, 11–13), studies that evaluated the acute responses and chronic adaptations of the abdominal muscles with different RT strategies of manipulation of volume and intensity are scarce.
Therefore, in addition to the choice of exercise, the correct manipulation of the acute variables of intensity and volume is essential to induce adequate levels of metabolic stress and mechanical tension in an RT session (20, 21, 26, 31, 32). Metabolic stress can be indirectly characterized by the level of cell swelling after an RT exercise or workout. Furthermore, after an RT session, metabolic stress products such as growth hormone and reactive oxygen species are simultaneously produced and are important in the activation of the mammalian target of rapamycin and muscle protein synthesis (16). Therefore, cell swelling, immediately after an RT session, may be involved in the hypertrophic metabolic stress response, resulting from increased phosphocreatine, increased lactate production, accumulation of hydrogen ions, and increase in the production of growth hormone and cortisol (16). Acute cell swelling can be evaluated by ultrasound images in which two different and complementary techniques are used. The first technique is called muscle thickness (MT) and it is based on defining the distance from the subcutaneous adipose tissue-muscle to muscle-bone interface for a specific muscle (1). The second technique is called echo-intensity (EI) and it is related to the pixel density from an ultrasound image and quantified by a visual scoring (42). Changes in EI have also been used to provide insights into the balance between the extracellular and intracellular fluid in studies investigating acute cell swelling (42). It is known that EI is related to edema and changes in EI were recently used as a non-invasive way to determine whether the acute change in MT was due to an intracellular shift or rather due to the fluid accumulation around the muscle fibers (42, 43). In combination with imaging techniques, the peak force (PF) produced after an RT session and TUT during each set complement the metabolic analysis as it indicates an increase in the production of lactate and hydrogen ions (neuromuscular fatigue) and may influence water uptake into muscle cells according to cell permeability (3, 5, 16, 32, 37, 40). Additionally, TUT may have an even greater impact than cell swelling as a marker of hypertrophy as mechanical signals appear to be a primary hypertrophy stimulus (41). Finally, the total load lifted (TLL) is an indirect way to define the mechanical tension during an RT session. Mechanical tension induced by an RT session causes mechanochemically transduced molecular and cellular responses in myofibers and satellite cells (20, 30) being also fundamental to inducing acute responses and chronic adaptations such as muscle growth (20). In this way, a clear dose-response relationship has been reported between TLL and both muscle strength and hypertrophy (17, 18, 33, 34, 36).
To the best of the authors’ knowledge, no study has been conducted to assess the metabolic stress and mechanical tension induced by different intensities during the abdominal crunch exercise with the total volume equalized in recreationally-trained participants. Therefore, the primary purpose of this study was to evaluate the acute dose response of different intensities with total volume equalized (40 repetitions) during the abdominal crunch exercise on muscle thickness, echo-intensity, peak force, time under tension, total load lifted, and perception of effort in recreationally-trained participants. Based on the same total volume in both RT protocols, it is hypothesized that both RT protocols (RT4×10RM and RT1×40RM) will induce an increase in muscle thickness and induce a similar change in the color of the echo-intensity. Additionally, RT4×10RM will induce a greater reduction in peak force and increase time under tension and total load lifted. And, both RT protocols will induce a similar perception of effort.
METHODS
Participants
The number of participants was determined by a pilot study conducted previously, based on an effect size difference of 0.65, a significance level of 5%, and a power of 80% derived from the muscle thickness (pre-test: 41.3 ± 7.8mm and post-test: 47.1 ± 9.6mm) of individuals with the same characteristics used in the present study (10). Fifteen resistance-trained participants were recruited to this study [13 males and 2 females; age 23 ± 3 years, total body mass 76.4 ± 6.5 kg, height 173.3 ± 6.5 cm, abdominal skinfold 17.6 ± 6.6 mm]. All participants were regularly engaged in an RT program and familiar with the abdominal crunch exercise. They had 3 ± 1 years of RT experience (1 – 2 sessions/week), with no previous surgery or history of injury with residual symptoms (pain) in the spine or abdominal muscles within the last year. The maximal external load performed in each RT protocol (RT4×10RM and RT1×40RM) were 92.3 ± 12.8 kg and 69.3 ± 11.1 kg, respectively (p < 0.001). The participants were informed of the risks and benefits of the study prior to any data collection. All participants provided written informed consent prior to participation and the Institutional Review Board at California State University, Northridge approved the protocol and the study (#FY20-410). This research was carried out fully in accordance to the ethical standards of the International Journal of Exercise Science (27).
Protocol
This study used a randomized and counterbalanced design. Participants attended three laboratory sessions and refrained from performing core exercises other than activities of daily living for at least 48 hours prior to testing. A within-participant approach was used in which each participant performed a different RT protocol per session (RT4×10RM and RT1×40RM).
During the first session, anthropometric data were evaluated (height, weight, and abdominal skinfold). Next, all participants performed a familiarization and a specific warm-up (abdominal crunch exercise) consisting of 1 set of 10 repetitions with 5 kg, and 5-min rest interval. To perform the abdominal crunch exercise, all participants lay down in a supine position on an incline bench (at 15 degrees), lower limbs flexed, feet on the floor, and arms over the chest holding a rope attached to a cable-pulley machine (Star Trac., Lake Forest, CA, USA). They lifted the weight stack from a neutral spine position to a maximal spine flexion (~30 degrees) during the concentric phase and then returned to the initial position (eccentric phase). Afterward, all participants performed two different tests to define the maximal external load for each RT protocol: a). 10RM testing for abdominal crunch exercise, and b). 40RM testing for abdominal crunch exercise. Both tests were randomized among participants and 30-min were given between tests. Both tests are based on the Guidelines of the National Strength and Conditioning Association (NSCA) to determine individual initial training external load. Attempts were performed to progressively increase the external loads until reached their maximal capacity to perform a certain number of repetitions with the correct technique. The cadency (velocity) in each contraction was self-selected. All tests were directly supervised by a research assistant to ensure proper performance and the correct technique.
The second and third sessions were one week apart. During the second and third sessions, a specific warm-up (abdominal crunch exercise) was conducted with 10 repetitions at 50% of their 10RM testing load. Then, as a pre-test, ultrasonography of the rectus abdominis at rest was performed with the subject in apnea, then a test of maximum voluntary isometric contraction in maximum flexion of the spine was performed. Then, participants performed one of two RT protocols with similar total volume (40 repetitions) in random order: RT4×10RM: 4 sets of 10RM / 1-min rest interval between sets; or RT1×40RM: 1 set of 40RM. Stops between repetitions were not allowed during each set. After each RT protocol, another ultrasonography of the rectus abdominis at rest (in apnea) and the maximum voluntary isometric contraction in maximum flexion of the spine were retested immediately after (post-0) and 15-min after (post-15) the end of each RT protocol. All participants reported a session rating of perceived exertion (sRPE) 15-min after each RT protocol and session. The cadency (velocity) for both RT protocols was self-selected. All tests were directly supervised by a research assistant to ensure proper performance and correct technique. All participants received similar verbal encouragement during both RT protocols and all measures were performed at the same hour of the day (between 1 PM and 4 PM) by the same researcher.
Measurements
Muscle Thickness (MT): Ultrasound imaging was used to obtain measurements of MT. A trained technician performed all testing using an ultrasound imaging portable unit (Hitachi Noblus; Hitachi Medical Corporation, Tokyo, Japan). Following a generous application of a water-soluble transmission gel (Cskin, Medics Medical Products LLC., NY, USA) to the measured site, a 7.5-MHz linear array probe (L55 Probe) was placed perpendicular to the tissue interface without depressing the skin. Equipment settings were optimized for image quality according to the manufacturer's user manual and held constant in all conditions. When the quality of the image was deemed to be satisfactory, the image was saved to the hard drive. The MT dimensions were obtained by measuring the distance from the subcutaneous adipose tissue–muscle interface to the muscle-bone interface per methods used by Abe et al. (1). Measurements were taken on the right side of the body at the second portion of the rectus abdominis. Measurements were taken while the participants were lying on a bench. To avoid variations in probe compression, participants were instructed to perform the Valsalva maneuver during measurements. For rectus abdominis, measurements were taken at 25%, 50%, and 75% of the cross-section area. To maintain consistency between pre- and post-tests (0-min and 15-min), each site was marked with ink. To further ensure the accuracy of measurements, 3 images were obtained at each point (25%, 50%, and 75% of the cross-section area). If measurements were more than 1 mm from one another, a fourth image was obtained and averaged. The sum of all 3 measurements (25%, 50%, and 75%) was used to further analysis, and the test-retest ICC (MT) was 0.96 – 0.98 and the intra-rater reliability was 0.96 – 0.97.
Echo-Intensity (EI): The same images used to define muscle thickness were used to quantify EI. EI was assessed using an automated grayscale analysis that ranged from 0 (black) to 255 (white) (arbitrary unit, A. U.). A rectangular region of interest box was drawn as large as possible to encompass the entire cross-section area. Care was taken to ensure that fascia along the borders of the rectus abdominis, subcutaneous adipose tissue, and the bone region was not included in the analyses. The EI measurement was defined twice and the average was used for further analysis. The test-retest ICC (EI) was 0.97.
Peak Force (PF): The PF was measured by a digital load cell acquisition system (FM-204-1000K, Shenzhen Aermanda Technology Co. Ltd., Shenzhen, Guangdong, China / Capacity: 1000 Kgf/Resolution: 0.01 kgf). The digital load cell was placed between the cable and the handles via carabiners. To perform the maximal isometric force testing, all participants lay down in a supine position on an incline bench (at 15 degrees), lower limbs flexed, feet on the floor, and arms over the chest holding a rope attached to a cable-pulley machine. All participants performed 3 maximal voluntary isometric contractions (MVIC) at 30 degrees of spine flexion before (pre-test) and after (post-0 and post-15) each RT protocol (RT4×10RM and RT1×40RM). Each MVIC was performed for 5-sec and 10-sec rest interval. The peak force (PF) of each MVIC was defined and the average of the 3 MVICs was used for further analysis. The test-retest ICC (PF) was 0.95.
Time under tension (TUT): The TUT was measured by a chronometer during each set for both RT protocols (RT4×10RM and RT1×40RM). Then, to define the TUT, the set duration in seconds was divided by the total number of repetitions. For RT4×10RM, the TUT of all sets was summed and divided by 40 repetitions; and for RT1×40RM, the TUT of the set was divided by 40 repetitions.
Total Load Lifted (TLL): The TLL was calculated for both RT protocols (RT4×10RM and RT1×40RM) using the following formula: TLL = Number of Sets * Number of Repetitions * External Load (kg).
Session Rating of Perceived Exertion (sRPE): The sRPE was assessed with a CR-10 scale using the recommendations of Sweet et al., (38). Participants were asked to use an arbitrary unit (A.U.) on the scale to rate their overall effort after both RT protocols. A rating of 0 was associated with no effort and a rating of 10 was associated with maximal effort and the most stressful exercise ever performed. All participants answered the following question based on CR-10 scale: “How was your workout?” The sRPE was asked 15-min after the end of each RT protocol (RT4×10RM and RT1×40RM).
Statistical Analysis
The normality and homogeneity of variances were confirmed by the Shapiro-Wilk and Levene’s tests, respectively. The mean, standard deviation (SD), and delta percentage (Δ%) were calculated. Two-way repeated-measures ANOVAs (2 × 3) were used to test differences between RT protocols (RT4×10RM and RT1×40RM) and time (pre-test, post-0, and post-15) for MT, EI, and PF. Post-hoc comparisons were performed with the Bonferroni test when necessary. Paired t-test was used to compare differences between RT protocols (RT4×10RM and RT1×40RM) for TLL, TUT, and sRPE. Furthermore, the magnitudes of the difference were examined using the standardized difference based on Cohen’s d units using effect sizes (d) (14). The d results were qualitatively interpreted using the following thresholds: < 0.35 - trivial; 0.35 - 0.8 - small; 0.8 – 1.5 - moderate; > 1.5 - large for recreationally trained (7). An alpha of 5% was used to determine statistical significance.
RESULTS
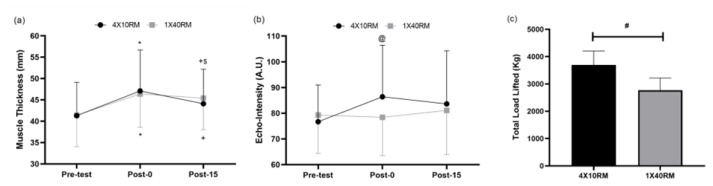
For muscle thickness (MT), there was a significant main effect only for time (p < 0.001). There was no significant interaction between RT protocol and time (p = 0.203). There were significant differences for RT4×10RM between pre-x post-0 (p < 0.001, d = 0.65 [small], Δ% = 12.1), pre-x post-15 (p = 0.011, d = 0.34 [trivial], Δ% = 6.3), and post-0 × post-15 (p = 0.02, d = 0.34 [trivial], Δ% = 6.3) (Figure 1b). There were significant differences for RT1×40RM between pre-x post-0 (p < 0.001, d = 0.67 [small], Δ% = 11) and pre-x post-15 (p = 0.003, d = 0.55 [small], Δ% = 8.9) (Figure 1a).
Figure 1.
Mean ± standard deviation of (a) muscle thickness and (b) echo-intensity between pre- and pos-tests (0-min and 15-min) for both RT protocols (RT4×10RM and RT1×40RM); and (c) total load lifted for both RT protocols (RT4×10RM and RT1×40RM). Legend: * Significant difference between pre- and post-0; +Significant difference between pre- and post-15; $ Significant difference between post-0 and post-15; & Significant difference between RT protocols; @ Significant difference between pre- and post-0 only for RT4×10RM; # Significant difference between RT protocols.
For echo-intensity (EI), there was a significant main effect for time (p = 0.043). There was a significant interaction between RT protocol and time (p = 0.002). There was a significant difference only for RT4×10RM between pre-x post-0 (p = 0.002, d = 0.55 [small], Δ% = 11.6) (Figure 1b).
For peak force (PF), there was no significant main effect for RT protocol (p = 0.855) and time (p = 0.504), and there is no interaction between RT protocol and time (p = 0.051).
For time under tension (TUT), there was a significant difference between RT4×10RM and RT1×40RM (1.4 ± 0.4 s and 1.1 ± 0.4 s, respectively; p = 0.04, d = 0.73 [small], Δ% = 21.4).
For total load lifted (TLL), there was a significant difference between RT4×10RM and RT1×40RM (3,693.3 ± 511.9 kg and 2,773.3 ± 446.4 kg, respectively; p < 0.001, d = 1.91 [large], Δ% = 24.9) (Figure 1c).
For session rating of perceived exertion (sRPE), there was no significant difference between RT4×10RM and RT1×40RM (8.8 ± 1.6 A.U. and 8.2 ± 0.9 A.U., respectively; d = 0.50 [small], Δ% = 6.8).
DISCUSSION
This study aimed to evaluate acute dose response of different intensities with total volume equalized (40 repetitions) during the abdominal crunch exercise on muscle thickness, echo-intensity, peak force, time under tension, total load lifted, and perception of effort in recreationally-trained participants. The main findings include 1. Both RT protocols induced similar increases in MT; 2. There was observed an effect in EI only between pre- and post-0 for RT4×10RM; 3. PF presented a nonsignificant reduction after both RT protocols; 4. The TLL and TUT were higher for RT4×10RM; 5. sRPE was similar between RT protocols. In this way, the present study presents evidence that the modification of the intensity, as well as the modification in the RT session design, might affect the acute mechanical and metabolic responses. To the best of the authors’ knowledge, no study was conducted to measure the acute dose response of different intensities with similar total volume (40 repetitions) during the abdominal crunch exercise in recreationally-trained participants.
Different RT protocols have been shown to induce different acute cell swelling, the extent of which relies on the type of exercise, level of fatigue, volume, and intensity (31). RT exercises with momentary muscle failure reduce the intramuscular ATP and CP levels (and Pi, ADP, and AMP accumulation) and increase the glycolytic flux (production of H+ leads to metabolite accumulation), hypoxia (via muscle contraction), and venous pooling leading to cell swelling (5, 32, 37, 40). In the present study, MT and EI were obtained to measure the acute cell swelling at three-time points (pre-, post-0, and post-15) in both RT protocols (RT4×10RM and RT1×40RM). It was hypothesized that both RT protocols (RT4×10RM and RT1×40RM) would induce an increase in MT and induce a similar effect in EI. The results of this study corroborated the main hypothesis for MT, after all, it was observed an increase in MT after both RT protocols (11 – 12.1%), however, the results did not corroborate the main hypothesis for EI. It was observed changes in the color of the EI only after the RT4×10RM (11.6%) provided insights into the balance between the extracellular and intracellular fluid (42). It is known that EI is related to edema and changes in EI were recently used as a non-invasive way to determine whether the acute change in MT was due to an intracellular shift or rather due to the fluid accumulation around the muscle fibers (42, 43).
The equalization of the total volume of repetitions might be the main cause for these results, however, one cannot ignore the characteristics of the different acute RT variables such as intensity, number of repetitions, and rest interval between sets. These variables, independently, might influence specific responses modulating the level of metabolic stress and mechanical tension in each RT protocol. Possibly, RT protocols with more strenuous stress (intensity) and total volume equalized could induce different effects in EI (14, 31, 32, 42).
Regarding the acute variables analyzed (TUT and TLL), the results of this study showed that the RT4×10RM was a more stressful RT protocol than RT1×40RM. It was hypothesized that RT4×10RM would induce higher values of TUT and TLL when compared to RT1×40RM and the results of this study corroborated the main hypothesis. TUT has been shown to alter neurophysiological, hormonal, and metabolic responses (4, 19) and can be manipulated by movement velocity and/or range of motion (6, 23). Even with a similar total volume (40 repetitions), higher intensities and the inclusion of rest intervals between sets might influence the acute responses. As observed in this study, the total load lifted (TLL), which represents the total work performed per RT protocol was 24.9% higher for RT4×10RM when compared to RT1×40RM. For RT protocols with similar total volume, the intensity and rest intervals between sets have an important influence on the TLL. The level of intensity limits the total number of repetitions performed until muscle failure and the rest interval between sets partially removes the neuromuscular fatigue allowing more sets with a similar external load. In this study, the external load for 10RM was 24.9% higher than for 40RM. In addition, the TUT was 21.4% higher for RT4×10RM than for RT1×40RM representing approximately 0.3 sec more per repetition for the RT4×10RM and possibly affecting EI. However, this difference in time was not sufficient to affect other variables analyzed in this study. Extrapolating these results to chronic adaptations, TUT ranging from 0.5- to 8-sec seems to maximize muscle hypertrophy (35).
The peak force (PF) was measured before and after (0-min and 15-min) aiming to verify the level of neuromuscular fatigue induced by each RT protocol. Neuromuscular fatigue is defined as a reduction in maximal force or power production in response to contractile activity (3). Considering the different levels of intensity of both RT protocols, it was hypothesized that the RT4×10RM would induce a greater reduction in PF. However, the results of this study did not corroborate the main hypothesis, after all, both RT protocols presented a small and non-significant change in PF. The lack of reduction in force production might be influenced by different combinations of acute variables and the external load applied to each RT protocol. For RT1×40RM, the external load (40RM) and the TUT were not as high as for RT4×10RM, however, the higher intensity (10RM) may have been influenced by the constant rest interval between sets.
Finally, the session rating of perceived exertion (sRPE) is frequently used to indirectly quantify the level of effort after sets, exercises, and RT sessions (15, 21). sRPE represents a relationship between the physiological and performance measures and assists in quantifying the overall load (15). In this study, it was hypothesized that both RT protocols (RT4×10RM and RT1×40RM) would induce similar sRPE, corroborating the main hypothesis. Both RT protocols presented high sRPEs (8.2 – 8.8 A.U.). It is well known that sRPE is affected by the level of neuromuscular fatigue after RT protocols for recreationally-trained participants. Probably, the lack of difference in sRPE values was due to a similar level of neuromuscular fatigue induced in both RT protocols.
In conclusion, both RT protocols (RT4×10RM and RT1×40RM) induced similar increases in MT but not for EI. TLL and TUT were higher for RT4×10RM. And, PF and sRPE were similar after both RT protocols. Therefore, when it comes to abdominal exercises, a more intense RT protocol (RT4×10RM) increased the levels of metabolic stress with higher levels of mechanical tension when the total volume was equalized (40 repetitions).
This study has some limitations that should be considered when interpreting the current results. First, we measured only the second portion of the rectus abdominis. A different portion of the rectus abdominis (polygastric muscle) could present a different acute response for MT and EI and it is possible that the set/rep scheme was not enough significantly fatiguing to impact peak force and may have limited changes in cell swelling. Second, the small sample size and the number of comparisons may have affected statistical power. Despite this limitation, analysis of effect sizes provides a good basis for drawing inferential conclusions from the results. Third, we did not measure lactate or by-products from the metabolism. Fourth, the findings of this study cannot, necessarily, be generalized to other exercises, RT protocols, or different populations including adolescents, athletes, and the elderly.
ACKNOWLEDGMENTS
The authors thank the participants for their participation.
REFERENCES
- 1.Abe T, Loenneke JP, Thiebaud RS, Loftin M. Morphological and functional relationships with ultrasound measured muscle thickness of the upper extremity and trunk. Ultrasound. 2014;22(4):229–235. doi: 10.1177/1742271X14554678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson EA, Nilson J, Thorsthensson A. Abdominal and hip flexor muscle activation during various training exercises. Eur J Appl Physiol. 1997;75:115–123. doi: 10.1007/s004210050135. [DOI] [PubMed] [Google Scholar]
- 3.Behrens M, Gube M, Chaabene H, Prieske O, Zenon A, Broscheid KC, Schega L, Husmann F, Weippert M. Fatigue and human performance: An updated framework. Sports Med (Auckland, NZ) 2023;53(1):7–31. doi: 10.1007/s40279-022-01748-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burd NA, Andrews RJ, West DW, Little JP, Cochran AJ, Hector AJ, Cashaback JG, Gibala MJ, Potvin JR, Baker SK, Phillips SM. Muscle time under tension during resistance exercise stimulates differential muscle protein sub-fractional synthetic responses in men. J Physiol. 2012;590(2):351–362. doi: 10.1113/jphysiol.2011.221200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen YL, Wolin MS, Messina EJ. Evidence for cgmp mediation of skeletal muscle arteriolar dilation to lactate. J Appl Physiol. 1996;81(1):349–354. doi: 10.1152/jappl.1996.81.1.349. [DOI] [PubMed] [Google Scholar]
- 6.Cintineo HP, Freidenreich DJ, Blaine CM, Cardaci TD, Pellegrino JK, Arent SM. Acute physiological responses to an intensity and time under tension equated single vs. multiple set resistance training bout in trained men. J Strength Cond Res. 2018;32(12):3310–3318. doi: 10.1519/JSC.0000000000002872. [DOI] [PubMed] [Google Scholar]
- 7.Cohen J. Statistical power analysis for the behavioral sciences. New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 8.Crommert ME, Bjerkefors A, Tarassova O, Ekblom MM. Abdominal muscle activation during common modifications of the trunk curl-up exercise. J Strength Cond Res. 2021;35(2):428–435. doi: 10.1519/JSC.0000000000002439. [DOI] [PubMed] [Google Scholar]
- 9.Delp SL, Suryanarayanan S, Murray WM, Uhlir J, Triolo RJ. Architecture of the rectus abdominis, quadratus lumborum, and erector spinae. J Biomech. 2001;34(3):371–375. doi: 10.1016/s0021-9290(00)00202-5. [DOI] [PubMed] [Google Scholar]
- 10.Eng J. Sample size estimation: How many individuals should be studied? Radiol. 2003;227(2):309–313. doi: 10.1148/radiol.2272012051. [DOI] [PubMed] [Google Scholar]
- 11.Escamilla RF, Babb E, DeWitt R, Jew P, Kelleher P, Burnham T, Busch J, D'Anna K, Mowbray R, Imamura RT. Electromyographic analysis of traditional and nontraditional abdominal exercises: Implications for rehabilitation and training. Phys Ther. 2006;86(5):656–671. [PubMed] [Google Scholar]
- 12.Escamilla RF, Lewis C, Bell D, Bramblet G, Daffron J, Lambert S, Pecson A, Imamura R, Paulos L, Andrews JR. Core muscle activation during swiss ball and traditional abdominal exercises. J Orthop Sports Phys Ther. 2010;40(5):265–227. doi: 10.2519/jospt.2010.3073. [DOI] [PubMed] [Google Scholar]
- 13.Escamilla RF, McTaggart MS, Fricklas EJ, DeWitt R, Kelleher P, Taylor MK, Hreljac A, Moorman CT. An electromyographic analysis of commercial and common abdominal exercises: Implications for rehabilitation and training. J Orthop Sports Phys Ther. 2006;36(2):45–57. doi: 10.2519/jospt.2006.36.2.45. [DOI] [PubMed] [Google Scholar]
- 14.Fleckenstein JL, Canby RC, Parkey RW, Peshock RM. Acute effects of exercise on mr imaging of skeletal muscle in normal volunteers. AJR Am J Roentgenol. 1988;151(2):231–237. doi: 10.2214/ajr.151.2.231. [DOI] [PubMed] [Google Scholar]
- 15.Halperin I, Emanuel A. Rating of perceived effort: Methodological concerns and future directions. Sports Med. 2019:1–9. doi: 10.1007/s40279-019-01229-z. [DOI] [PubMed] [Google Scholar]
- 16.Hirono T, Ikezoe T, Taniguchi M, Tanaka H, Saeki J, Yagi M, Umehara J, Ichihashi N. Relationship between muscle swelling and hypertrophy induced by resistance training. J Strength Cond Res. 2020;1(3):1–6. doi: 10.1519/JSC.0000000000003478. [DOI] [PubMed] [Google Scholar]
- 17.Krieger JW. Single vs. multiple sets of resistance exercise for muscle hypertrophy: A meta-analysis. J Strength Cond Res. 2010;24(4):1150–1159. doi: 10.1519/JSC.0b013e3181d4d436. [DOI] [PubMed] [Google Scholar]
- 18.Krzysztofik M, Wilk M, Wojdała G, Gołaś A. Maximizing muscle hypertrophy: A systematic review of advanced resistance training techniques and methods. Int J Environ Res Public Health. 2019;16(24):4897. doi: 10.3390/ijerph16244897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lacerda LT, Martins-Costa HC, Diniz RCR, Lima FV, Andrade AGP, Tourino FD, Bemben MG, Chagas MH. Variations in repetition duration and repetition numbers influence muscular activation and blood lactate response in protocols equalized by time under tension. J Strength Cond Res. 2016;30(1):251–258. doi: 10.1519/JSC.0000000000001044. [DOI] [PubMed] [Google Scholar]
- 20.Lim C, Nunes EA, Currier BS, McLeod JC, Thomas ACQ, Phillips SM. An evidence-based narrative review of mechanisms of resistance exercise-induced human skeletal muscle hypertrophy. Med Sci Sports Exerc. 2022;54(9):1546–1559. doi: 10.1249/MSS.0000000000002929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marchetti PH. Strength training manual: Applied science. 2nd ed. Dubuque: Kendall Hunt Publishing Company; 2022. [Google Scholar]
- 22.Marchetti PH, Kohn AF, Duarte M. Selective activation of the rectus abdominis muscle during low-intensity and fatiguing tasks. J Sports Sci Med. 2011;10(2):322–327. [PMC free article] [PubMed] [Google Scholar]
- 23.Marchetti PH, Lopes CR. Planejamento e prescrição do treinamento personalizado do iniciante ao avançado. São Paulo: Editora Mundo; 2018. [Google Scholar]
- 24.Marchetti PH, Schoenfeld BJ, Da Silva JJ, Guiselini MA, Freitas FS, Pecoraro SL, Gomes WA, Lopes CR. Muscle activation pattern during isometric ab wheel rollout exercise in different shoulder angle-positions. Medical Express. 2015;02(4):01–05. [Google Scholar]
- 25.Martuscello JM, Nuzzo JL, Ashley CD, Campbell BI, Orriola JJ, Mayer JM. Systematic review of core muscle activity during physical fitness exercises. J Strength Cond Res. 2013;27:1684–1698. doi: 10.1519/JSC.0b013e318291b8da. [DOI] [PubMed] [Google Scholar]
- 26.Medicine ACoS. ACSM's guidelines for exercise testing and prescription. 11 ed. Philadelphia: Wolters Klumer; 2021. [Google Scholar]
- 27.Navalta JW, Stone WJ, Lyons TS. Ethical issues relating to scientific discovery in exercise science. Int J Exerc Sci. 2019;12(1):1–8. doi: 10.70252/EYCD6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Norris CM. Abdominal muscle training in sport. Br J Sports Med. 1993;27(1):19–27. doi: 10.1136/bjsm.27.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saeterbakken AH, Stien N, Pedersen H, Andersen V. Core muscle activation in three lower extremity exercises with different stability requirements. J Strength Cond Res. 2022;36(2):304–309. doi: 10.1519/JSC.0000000000003465. [DOI] [PubMed] [Google Scholar]
- 30.Schoenfeld BJ. The mechanisms of muscle hypertrophy and their application to resistance training. J Strength Cond Res. 2010;24(10):2857–2872. doi: 10.1519/JSC.0b013e3181e840f3. [DOI] [PubMed] [Google Scholar]
- 31.Schoenfeld BJ. Potential mechanisms for a role of metabolic stress in hypertrophic adaptations to resistance training. Sports Med. 2013;43(3):179–194. doi: 10.1007/s40279-013-0017-1. [DOI] [PubMed] [Google Scholar]
- 32.Schoenfeld BJ, Contreras B. The muscle pump: Potential mechanisms and applications for enhancing hypertrophic adaptations. Strength Cond J. 2014;36(3):21–25. [Google Scholar]
- 33.Schoenfeld BJ, Ogborn D, Krieger JW. Dose-response relationship between weekly resistance training volume and increases in muscle mass: A systematic review and meta-analysis. J Sports Sci. 2016;35(11):1073–1082. doi: 10.1080/02640414.2016.1210197. [DOI] [PubMed] [Google Scholar]
- 34.Schoenfeld BJ, Ogborn D, Krieger JW. Effects of resistance training frequency on measures of muscle hypertrophy: A systematic review and meta-analysis. Sports Med. 2016;46(11):1689–1697. doi: 10.1007/s40279-016-0543-8. [DOI] [PubMed] [Google Scholar]
- 35.Schoenfeld BJ, Ogborn DI, Krieger JW. Effect of repetition duration during resistance training on muscle hypertrophy: A systematic review and meta-analysis. Sports Med. 2015;45(4):577–585. doi: 10.1007/s40279-015-0304-0. [DOI] [PubMed] [Google Scholar]
- 36.Schoenfeld BJ, Ratamess NA, Peterson MD, Contreras B, Sonmez GT, Alvar BA. Effects of different volume-equated resistance training loading strategies on muscular adaptations in well-trained men. J Strength Cond Res. 2014;28(10):2909–2918. doi: 10.1519/JSC.0000000000000480. [DOI] [PubMed] [Google Scholar]
- 37.Sjøgaard G, Adams RP, Saltin B. Water and ion shifts in skeletal muscle of humans with intense dynamic knee extension. Am J Physiol. 1985;248(2):R190–196. doi: 10.1152/ajpregu.1985.248.2.R190. [DOI] [PubMed] [Google Scholar]
- 38.Sweet TW, Foster C, McGuigan MR, Brice G. Quantitation of resistance training using the session rating of perceived exertion method. J Strength Cond Res. 2004;18(4):796–802. doi: 10.1519/14153.1. [DOI] [PubMed] [Google Scholar]
- 39.Taylor DC, Meyers WC, Moylan JA, Lohnes J, Bassett FH, Garrett WE., Jr Abdominal musculature abnormalities as a cause of groin pain in athletes. Inguinal hernias and pubalgia. Am J Sports Med. 1991;19(3):239–242. doi: 10.1177/036354659101900306. [DOI] [PubMed] [Google Scholar]
- 40.Usher-Smith JA, Huang CL, Fraser JA. Control of cell volume in skeletal muscle. Biol Rev Camb Philos Soc. 2009;84(1):143–159. doi: 10.1111/j.1469-185X.2008.00066.x. [DOI] [PubMed] [Google Scholar]
- 41.Wackerhage H, Schoenfeld BJ, Hamilton DL, Lehti M, Hulmi JJ. Stimuli and sensors that initiate skeletal muscle hypertrophy following resistance exercise. J Appl Physiol. 2019;126(1):30–43. doi: 10.1152/japplphysiol.00685.2018. [DOI] [PubMed] [Google Scholar]
- 42.Wong V, Spitz RW, Bell ZW, Viana RB, Chatakondi RN, Abe T, Loenneke JP. Exercise induced changes in echo intensity within the muscle: A brief review. J Ultrasound. 2020;23(4):457–472. doi: 10.1007/s40477-019-00424-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yitzchaki N, Kuehne TE, Mouser JG, Buckner SL. Can changes in echo intensity be used to detect the presence of acute muscle swelling? Physiol Meas. 2019;40(4):045002. doi: 10.1088/1361-6579/ab122a. [DOI] [PubMed] [Google Scholar]