Appreciation of bone density and osteoporosis is critical for planning instrumented spinal fusions and can influence decisions such as length of construct, material choice, and surgical adjuncts such as cement augmentation or bracing1).
Dual-energy X-ray absorptiometry (DXA) is considered the gold standard for the quantitative assessment of bone mineral density (BMD)2). There is generally a strong relationship between mechanical bone strength and BMD as assessed by DXA, and BMD scores show a strong inverse correlation with fracture risk3). However, 10%-20% of patients who sustain low-energy osteoporotic fractures have normal BMD measurements4), and normal BMD does not equate to normal bone quality5). However, once a low-energy, osteoporotic fracture has occurred, this is indication enough that a patient has poor bone quality and should be treated as such regardless of BMD. Here, we present an illustrative case in accordance with the CARE guidelines6).
A 47-year-old male presents to the Emergency Department with a one-month history of left-sided chest pain and mid back pain. He had a past medical history of obesity, 20 pack year smoking history, hypertension, type 2 diabetes, and new onset schizophrenia.
The onset of back pain was insidious and without trauma. Chest computed tomography (CT) showed a large left-sided pleural effusion, T4 and T6 compression fractures (Fig. 1). At that time, he was neurologically intact. Thoracentesis did not suggest malignancy or infection. The patient left the hospital against medical advice and before the involvement of the spine team. He returned three weeks later after a minor fall from a standing height. At that point, he presented with complete bilateral motor paralysis of the lower extremities and complete sensory loss at the T6 level. The spine team was consulted, and the patient was transferred to our tertiary care centre.
Figure 1.
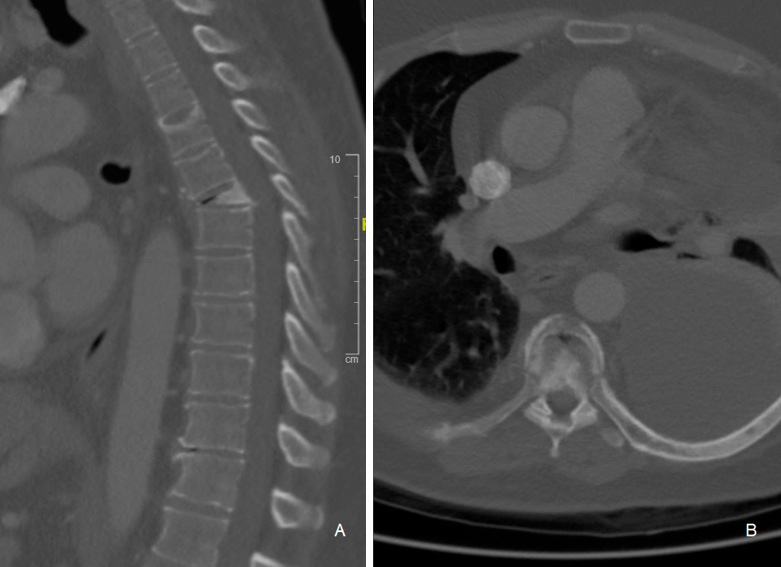
Chest CT scan showing large left-sided pleural effusion, as well as T4 and T6 compression fractures.
Magnetic resonance imaging demonstrated mild ventral cord compression at the level of the fracture with a small anterior hematoma (Fig. 2). Clinically, he had a T6-level ASIA A spinal cord injury (SCI) He underwent a posterior decompression, fusion and a transpedicular (Fig. 3) open biopsy with posterior shortening of the T6 vertebra. Intraoperatively, soft bone was appreciated on screw insertion. Results of the biopsy from the vertebral body were negative for malignancy or infection.
Figure 2.
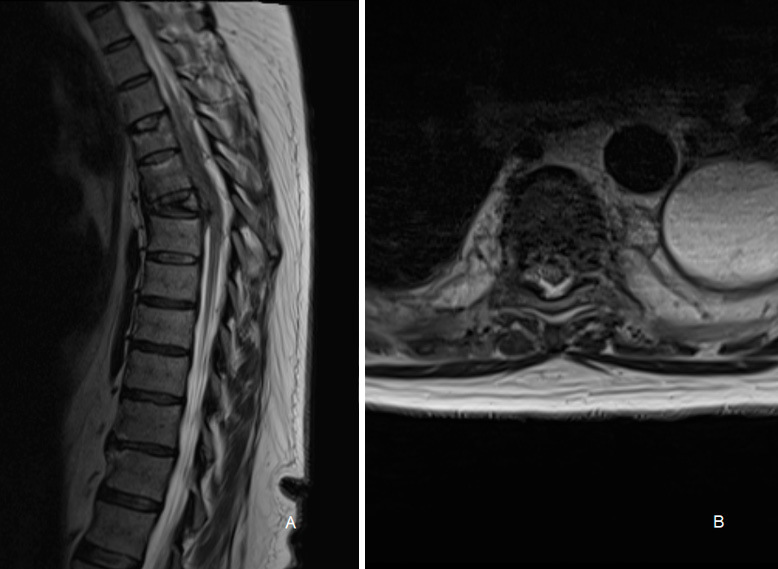
T2 sagittal and axial MRI images showing mild ventral cord compression at the level of the compression fractures with a small anterior hematoma.
Figure 3.
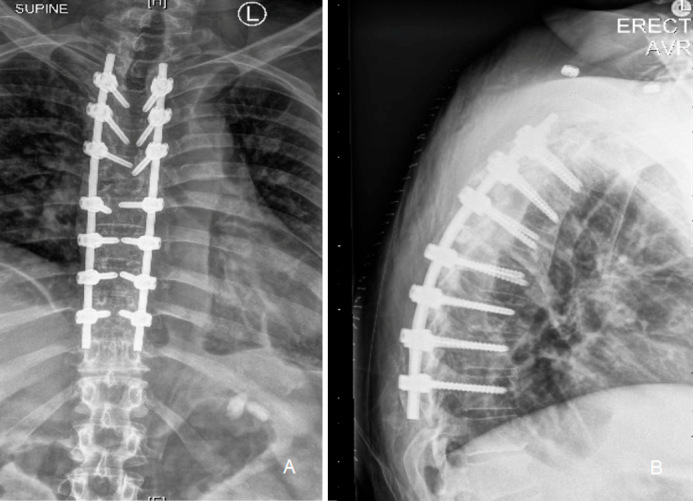
Anteroposterior and lateral postoperative x-rays showing posterior decompression, fusion, and shortening procedure.
Post-operative metastatic workup revealed a right adrenal gland nodule. The patient had a positive dexamethasone suppression test and normal adrenocorticotropic hormone (ACTH) level. The adenoma was confirmed to be a cortisol-secreting tumor. Interestingly, his post-operative BMD (Discovery W DXA, Hologic, Massachusetts, USA) was normal with a T-score of -0.8 in the lumbar spine, 0.0 in the left hip and -0.1 in the right hip, with corresponding Z-scores of -0.6, 0.2, and 0.2, respectively (Fig. 4). Interestingly, pre-operative CT scan shows a Hounsfield Unit measurement of 102+/-32 on axial sequences of the L1 vertebral body, suggesting osteopenia7). At one year post-operatively, he still had complete spinal cord injury (ASIA A).
Figure 4.
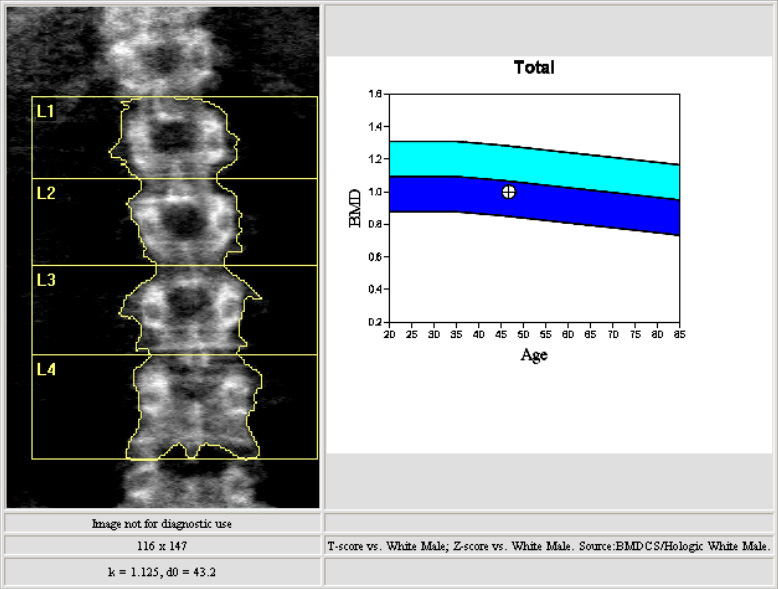
DXA table and image of the lumbar spine.
Cushing's syndrome is characterized by oversecretion of glucocorticoids and is a well-recognized cause of secondary osteoporosis and pathological fractures8). Despite an increased risk of fracture, BMD scores are typically normal or only slightly decreased in patients with Cushing's Syndrome9,10). It is theorized that glucocorticoids interfere with normal trabecular micro-architecture and can impair structural integrity without a concomitant decrease in density as measured by conventional DXA scan10). Trabecular Bone Scan (TBS) is a method applied to DXA that allows estimation of bony trabecular microarchitecture11) and has been shown to be a better predictor of fracture than BMD for patients with Cushing's Syndrome10).
Spinal constructs in osteoporotic spines are often augmented by longer constructs, fenestrated screws with cement injection, or circumferential fixation1). We caution surgeons to not rely on BMD alone in making these surgical planning decisions. As this case demonstrates, even in the absence of technical error, conditions which affect trabecular architecture may yield normal BMD despite poor bone quality.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: None
Author Contributions: All named authors participated substantially in the drafting and review of the manuscript.
Ethics Statement: Informed consent for publication was obtained by the patient who was a subject of the case report. Research Ethics Board approval was not required locally as the patient signed an institutional consent form allowing the use of anonymized information as part of the surgical process.
Publication Statement: This work has not, in whole or in part, been previously published or presented elsewhere.
References
- 1.Pantoja S, Molina M. Surgeon management of osteoporosis in instrumented spine surgery: AOSpine Latin America survey. Glob Spine J. 2019;9(2):169-72. doi: 10.1177/2192568218785369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Briot K. DXA parameters: beyond bone mineral density. Joint Bone Spine. 2013;80(3):265-9. [DOI] [PubMed] [Google Scholar]
- 3.Lotz JC, Cheal EJ, Hayes WC. Fracture prediction for the proximal femur using finite element models: part I―Linear analysis. J Biomech Eng. 1991;113(4):353-60. [DOI] [PubMed] [Google Scholar]
- 4.Schuit SCE, van der Klift M, Weel AEAM, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone. 2004;34(1):195-202. [DOI] [PubMed] [Google Scholar]
- 5.Bandaru S, Hare K, Krueger D, et al. Do patients that fracture with normal DXA-measured BMD have normal bone? Arch Osteoporos. 2020;15(1):70. [DOI] [PubMed] [Google Scholar]
- 6.CARE Checklist. CARE Case Report Guidelines. 2022 Sep. Available from: https://www.care-statement.org/checklist.
- 7.Yaprak G, Gemici C, Seseogullari OO, et al. CT, Derived Hounsfield Unit: an easy way to determine osteoporosis and radiation related fracture risk in irradiated patients. Front Oncol. 2020;10:742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minetto M, Reimondo G, Osella G, et al. Bone loss is more severe in primary adrenal than in pituitary-dependent Cushing's syndrome. Osteoporos Int. 2004;15(11):855-61. [DOI] [PubMed] [Google Scholar]
- 9.Dalle Carbonare LD, Arlot ME, Chavassieux PM, et al. Comparison of trabecular bone microarchitecture and remodeling in glucocorticoid-induced and postmenopausal osteoporosis. J Bone Miner Res. 2001;16(1):97-103. [DOI] [PubMed] [Google Scholar]
- 10.Belaya ZE, Hans D, Rozhinskaya LY, et al. The risk factors for fractures and trabecular bone-score value in patients with endogenous Cushing's syndrome. Arch Osteoporos. 2015;10:44. [DOI] [PubMed] [Google Scholar]
- 11.Pothuaud L, Carceller P, Hans D. Correlations between grey-level variations in 2D projection images (TBS) and 3D microarchitecture: applications in the study of human trabecular bone microarchitecture. Bone. 2008;42(4):775-87. [DOI] [PubMed] [Google Scholar]


