Abstract
Assessment of salvage endoscopic nasopharyngectomy for recurrent nasopharyngeal carcinoma (rNPC). This is a retrospective study of ten rNPC who underwent salvage endoscopic nasopharyngectomy. Recurrent status for each recurrence was determined before surgery and only recurrent T1 (rT1) and recurrent T2 (rT2) were taken up for surgery after review with radiation oncology colleagues. There were seven rT2 and three rT1 patients. Two patients have undergone simultaneous radical neck dissection (RND) together with endoscopic nasopharyngectomy for associated neck nodes. Outcome of the study was done in turn of disease free, disease residual and disease recurrence. Locally disease free and overall survival rates were 40% (4/10) and 50% (5/10) respectively. Locally disease free till the last follow up was achieved in 4 patients while one patient is on palliative chemotherapy post-surgery for locally positive disease for the last three years. Of the four patients that are locally disease free, two patients received chemoradiation (CTRT) post-surgery while two patients only underwent endoscopic nasopharyngectomy for rT1. There were no any major operative complications except nasal crusting. Recurrent T1 and T2 can be manage with endoscopic nasopharyngectomy and post-surgery ctrt should be given in feasible patients. To detect early recurrent and improve the survival, regular endoscopic follow up is needed.
Keywords: Recurrent, Nasopharyngeal carcinoma, Salvage, Endoscopic nasopharyngectomy
Introduction
The incidence of nasopharyngeal carcinoma (NPC) is rare in most of the countries in the world with remarkable racial and geographical distribution. The incidence of NPC is high in certain part of the world like South China Cantonese speaking people, Southeast Asia, some parts of North Africa and the Eskimos in the Arctic [1–4]. The incidence of NPC in Northeast hill states of India, particularly Nagaland, Manipur and Mizoram is high [5, 6]. Even though NPC responds well to chemoradiation (CTRT) [7–9], around 15% to 58% of the patients will have recurrence and undergo re-treatment [10–12]. Recurrent NPC is a clinical dilemma and a challenge, due to the difficult anatomical accessibility and the high risk nature of complications. Generally, the management options for recurrent cases are re-irradiation, open nasopharyngectomy or endoscopic nasopharyngectomy. Re-irradiation of recurrent lesion can be done provided there is sufficient gap since the initial treatment. Open surgical options are maxillary swing, infratemporal fossa, trans-mandibular pterygoid, trans-palatal and trans-cervical approaches. However, open surgeries are associated with a lot of morbidity such as palatal defects, trismus, dysphagia, nasal regurgitation etc. [13–15]. Endoscopic nasopharyngectomy is a challenging procedure and is performed in very few centres around the world. We purpose this study is to know the locally disease free as well as overall survival rates of recurrent nasopharyngeal carcinoma (rNPC) patients who underwent salvage endoscopic nasopharyngectomy.
Methods
We reviewed retrospectively ten patients who had underwent salvage endoscopic nasopharyngectomy for rNPC in our centre from 2014 to 2021. Three patients were rT1 and seven patients were rT2 tumourss. The primary stage of the disease and the treatment received are depicted in Table 1. Surgeries were planned after reviewing with radiation oncology team. All patients who were operated had recurrence with no significant skull base involvement. Patients with significant skull base involvement or associated bilateral neck nodes were excluded for surgery. Our centre is a teaching and tertiary referral centre; and all the patients were compliant with the ethical standards approval and informed consent. Prior to 2014 we opted open nasopharyngectomy but from 2014 onwards endoscopic nasopharyngectomy became our prefer approach whenever feasible rather than open approach. Two patients had undergone endoscopic nasopharyngectomy with radical neck dissection (RND) for associated neck nodes; and two patients had undergone subsequence twice surgery; one patient staged RND for relapse neck node and the other patient underwent second endoscopic surgery for recurrent tumours which was localized to the nasal cavity. All rT2 received post-surgery adjuvant treatment as shown in Table. 1. Patients age ranged from 17 to 52 years with seven male patients and three female patients. All the patients were followed up in the outpatient department with direct nasal endoscope and on any suspicion, imaging was carried out.
Table 1.
Disease recurrent stage, surgery, post-surgery adjuvant treatment and outcome
| Sl. no. | Age/Sex | Recurrent stage (rT) | Surgery | Post-surgery adjuvant treatment | Outcome |
|---|---|---|---|---|---|
| 1 | 41/M | rT2 after 1 year of primary treatment | Endoscopic Nasopharyngectomy | CT | Post-surgery residual local disease |
| 2 | 35/M | rT1 after 1 year of primary treatment | Endoscopic Nasopharyngectomy | CT | Locoregionally disease recurred |
| 3 | 35/M | rT2 after 2 years of primary treatment | Endoscopic Nasopharyngectomy | CTRT | NED |
| 4 | 17/F | rT2 in less than 1 year of primary treatment | Endoscopic Nasopharyngectomy and RND | CT | Metastasis to liver |
| 5 | 43/F | rT2 after 1 year of primary treatment | Endoscopic Nasopharyngectomy | CT | Tumor recurred locally with intracranial extension |
| 6 | 45/M | rT2 after 2 years of primary treatment | Endoscopic Nasopharyngectomy | CTRT | Relapse neck node for which patient underwent RND but disease recurred locally |
| 7 | 45/M | rT2 in less than 1 years of primary treatment | Endoscopic Nasopharyngectomy and RND | CT | Tumor recurred locally but patient surviving till date on palliative ct |
| 8 | 36/M | rT1 after 1 year of primary treatment | Endoscopic Nasopharyngectomy | None | NED |
| 9 | 52/F | rT2 after 4 years of primary treatment | Endoscopic Nasopharyngectomy | CTRT | NED |
| 10* | 52/M | rT1 after 2 years of primary treatment | Endoscopic Nasopharyngectomy | None | NED |
M Male, F Female, CT Chemotherapy, CTRT Concurrent Chemo-Radiotherapy
*Patient underwent second endoscopic surgery for recurrent tumor confined to nasal cavity
NED = No evidence of disease
Complete tumours removal (Ro) was achieved by en-bloc resection of the tumours. En-bloc resection was achieved starting superiorly by sphenoidectomy with drilling of the sphenoid rostrum and floor of the sphenoid sinus. From basisphenoid the resection proceeds downwards along the prevertebral muscles with pharyngobasilar fascia as the posterior margin. Laterally the medial part of the eustachian tube was resected along with the tumours.
Result
Ten patients had undergone salvage endoscopic nasopharyngectomy and in nine patients R0 resection could be achieved by this approach. As shown in Table-1, locally disease free and overall survival in our series were 40% (4/10) and 50% (5/10) respectively till the last follow up. Till the last follow up four patients were disease free while one patient had positive local disease for whom palliative chemotherapy was started. Of the four patients who had achieved disease free locally, one patient had received post-surgery adjuvant chemotherapy (cisplatin-gemcitabine three cycles); while another patient received post-surgery adjunct chemoradiation (five cycles cisplatin and 56 Gy radiation). Adjuvant treatment were given to both of these patients in view of rT2 diseases. The rest two patients had only undergone endoscopic nasopharyngectomy without post-surgery adjunct treatment in view of rT1. All the patients were kept on regular endoscopic follow up every 2 to 3 months. Of the total ten rNPC patients that had undergone salvage endoscopic nasopharyngectomy; five patients succumbed to the disease. Of the five patients that succumbed to the disease; in one patient salvage nasopharyngectomy failed to achieved tumour removal in toto; in another patient disease recurred locally extending intracranially after being disease free for 6 months. This patient had also complaint of diplopia. The third patient presented with recurrent neck node in the follow up period and on further investigations there was associated local recurrence of the disease invading internal carotid artery. The fourth patient had relapse of the neck node for which he underwent RND but disease recurred in three months’ time which was not amendable for surgery in view of significant skull base involvement, while the fifth patient died of liver metastasis. There was no any major operative complication apart from minor complications like nasal crusting. None of the patient had regurgitation problem. Figures 1 and 2 are preoperative axial and coronal views of a patient showing the extend of the growth. Figures 3 and 4 are post resection images of the same patient (axial and coronal respectively). Figure 5 is the endoscopic picture showing post endoscopic nasopharyngectomy and Fig. 6 shows the histological picture.
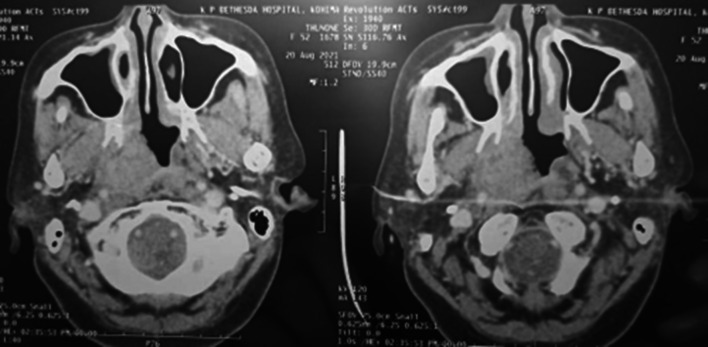
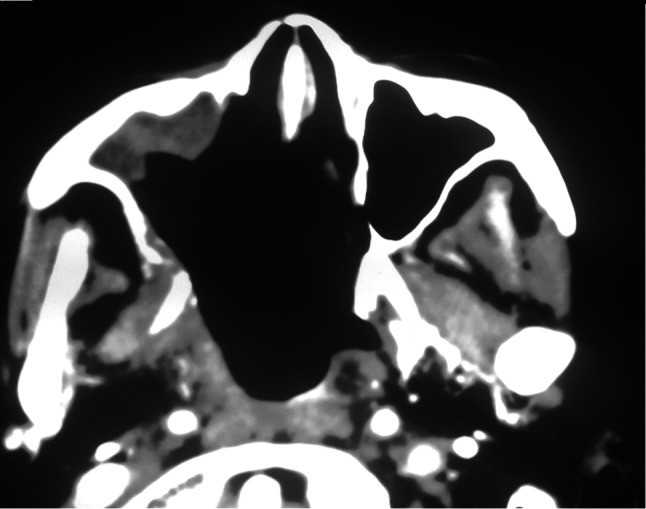
Fig. 1.
Pre-operative axial CECT scan showing the recurrent tumor in the nasopharynx
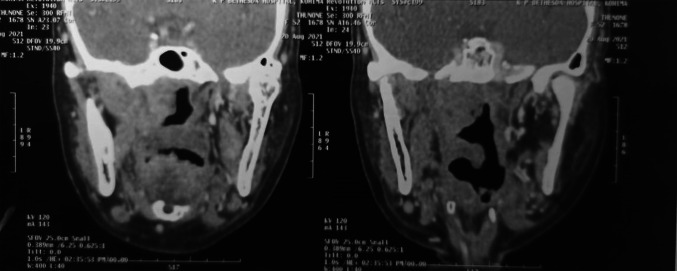
Fig. 2.
Pre-operative coronal CECT scan showing the recurrent tumor in the nasopharynx
Fig. 3.
Post-operative axial CECT scans of the nasopharynx
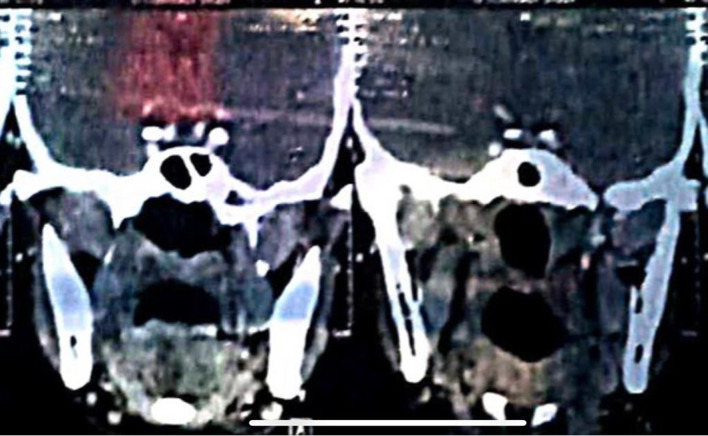
Fig. 4.
Post-operative coronal CECT scans of the nasopharynx
Fig. 5.
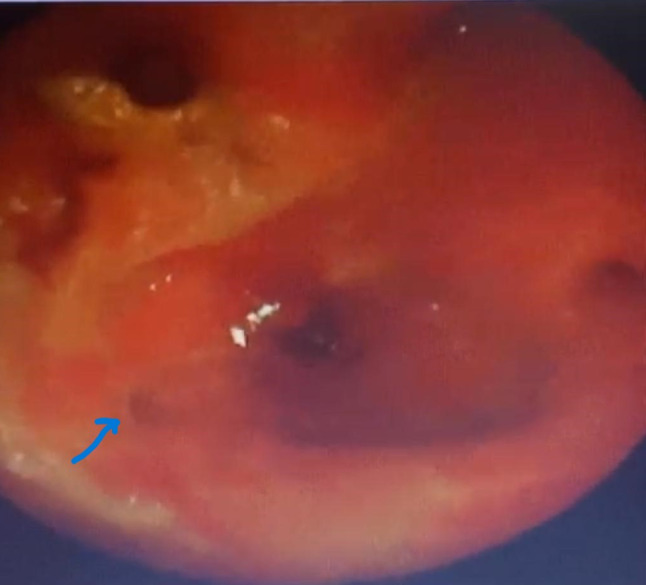
Endoscopic picture of post endoscopic nasopharyngectomy, arrow pointing the resected eustachian tube right side
Fig. 6.
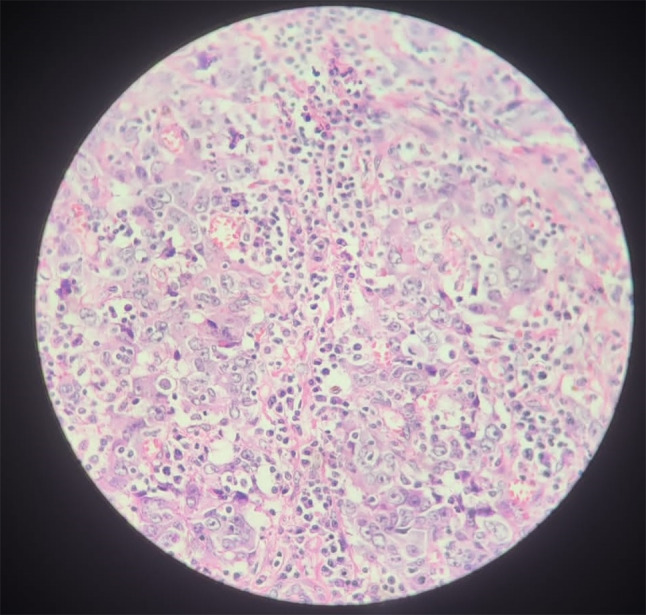
Histological picture-Interconnecting trabeculae with little keratinization, stromal lymphocytic infiltration. Cells with eosinophilic cyptoplasm with round nucleoli with vesicular chromatin
Discussion
Recurrent NPC is not only a clinical dilemma but also a challenge to treat. Salvage treatment available for rNPC are re-irradiation, open nasopharyngectomy or endoscopic nasopharyngectomy. Endoscopic nasopharyngectomy for rNPC has recently been done in few centres including in our centre. Since salvage endoscopic nasopharyngectomy for rNPC is a relatively new approach and there are only few published literatures available on its outcome. In this paper we described endoscopic nasopharyngectomy for rNPC. According to the available published literature, salvage endoscopic nasopharyngectomy for rNPC give a 2-year survival rate ranging from 59.4 to 100% [16–20] and a 5-year survival rate from 50 to 78.1% [21, 22]. Recently Thamboo et al. [23] report 5-year local disease free rate of 53.9% and overall survival rate of 84.6% with salvage endoscopic nasopharyngectomy for rNPC. These reports are encouraging both in turn of overall survival as well as local free disease control and are comparable to rT1–rT2 tumours treated by intensity modulated radiotherapy (IMRT) [24, 25] or by open surgical techniques [13, 26]. Study by You et al. [27] reported that endoscopic nasopharyngectomy have higher survival rate as well as better quality of life with fewer treatment related complications and lesser in costs than IMRT for similar staged rNPC. Our study has almost similar result with salvage endoscopic nasopharyngectomy for rNPC giving a local disease-free control rate of 40% (4/10) and overall survival rate of 50% (5/10). Of the three patients with rT1 lesion; in two patients, disease free could be achieved with endoscopic nasopharyngectomy as a single modality of treatment without post-operative adjuvant treatment. This finding stressed the need for regular endoscopic follow-up to detect early recurrences. With better understanding of the endoscopic sinonasal anatomy, endoscopic nasopharyngectomy for rNPC should produce better result in turn of survival of the patient with fewer complications. Moreover salvage endoscopic nasopharyngectomy is not associated with major perioperative complications. Minor complication like nasal crusting can occur but this can be taken care by regular saline nasal douching.
Limitation of the Study
No surgical margin status was assessed in our study.
Conclusion
Given the survival outcomes demonstrated by earlier studies as well as our present Study; NPC rT1 and rT2 can be treated by salvage endoscopic nasopharyngectomy rather than open nasopharyngectomy with the same or better efficacy in turn of survival of the patient and better quality of life. Close endoscopic follow-up every 2 to 3 months should be a protocol in all treated NPC so that the recurrent can be treated by detecting them early.
Acknowledgements
We are grateful to Professor S.Chakraborty, HOD, ENT department for his intellectual guidance, Ms W. Dkhar, librarian and her teams for plagiarism check.
Declarations
Conflict of interest
The authors have no competing interests to declare relevant to the content of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yu M, Yuan J. Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol. 2002;12:421–429. doi: 10.1016/S1044579X02000858. [DOI] [PubMed] [Google Scholar]
- 2.Wee JT, Ha TC, Loong SL, Qian CN. Is nasopharyngeal carcinoma really a “Cantonese Cancer”? Chin J Cancer. 2010;29(5):517–526. doi: 10.5732/cjc.009.10329. [DOI] [PubMed] [Google Scholar]
- 3.Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2006;15(10):1765–1777. doi: 10.1158/1055-9965.EPI-06-0353. [DOI] [PubMed] [Google Scholar]
- 4.Hirayama T. Descriptive and analytic epidemiology of nasopharyngeal carcinoma. In: De The G, Ito Y, editors. Nasopharyngeal carcinoma: etiology and control. Lyon: IARC Scientific Publications; 1978. pp. 167–189. [Google Scholar]
- 5.Kataki AC, Simons MJ, Das AK, Sharma K, Mehra NK. Nasopharyngeal carcinoma in the Northeastern states of India. Chin J Cancer. 2011;30(2):106–113. doi: 10.5732/cjc.010.10607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma TD, Singh TT, Laishram RS, Sharma LDC, Sunita AK, Imchen LT. Nasopharyngeal carcinoma—a clinico-pathological study in a Regional Cancer Centre of Northeastern India. Asian Pac J Cancer Prev. 2011;12:1583–1587. [PubMed] [Google Scholar]
- 7.Al-Sarraf M, LeBlanc M, Giri PG, Fu KK, Cooper J, Vuong T, Forastiere AA, Adams G, Sakr WA, Schuller DE, Ensley JF. Chemoradiotherapy versus radiotherapy in patients with advanced with advanced nasopharyngeal cancer: phase III randomized Intergroup study 0099. Clin Oncol. 1998;16(4):1310–1317. doi: 10.1200/JCO.1998.16.4.1310. [DOI] [PubMed] [Google Scholar]
- 8.Chan ATC, Leung SF, Ngan RKC, Teo PML, Lau WH, Kwan WH, Hui EP, Yiu HY, Yeo W, Cheung FY, Yu KH, Chiu KW, Chan DT, Mok TSK, Yau S, Yuen KT, Mo FKF, Lai MMP, Ma BBY, Kam MKM, Leung TWT, Johnson PJ, Choi PHK, Zee BCY. Overall survival after concurrent cisplatin-radiotherapy compared with radiotherapy alone in locoregionally advanced nasopharyngeal carcinoma. J Natl Cancer Inst. 2005;97(7):536–539. doi: 10.1093/jnci/dji084. [DOI] [PubMed] [Google Scholar]
- 9.Sarma G, Paul M, Nath J, Medhi PP, Bhattacharyya M, Kalita AK. Clinical outcomes and prognostic factors of locally advanced nasopharyngeal cancer treated with intensity modulated radiotherapy: first experience report from Northeast India. Indian J Otolaryngol Head Neck Surg. 2022;74:5964–5973. doi: 10.1007/s12070-021-02653-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li JX, Lu TX, Huang Y, et al. Clinical features of 337 patients with recurrent nasopharyngeal carcinoma. Chin J Cancer. 2010;29:82–86. doi: 10.5732/cjc.009.10412. [DOI] [PubMed] [Google Scholar]
- 11.Yang TS, Ng KT, Wang HM, Wang CH, Liaw CC, Lai GM. Prognostic factors of locoregionally recurrent nasopharyngeal carcinoma—a retrospective review of 182 cases. Am J Clin Oncol. 1996;19:337–343. doi: 10.1097/00000421-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Chang JT, See LC, Liao CT, et al. Locally recurrent nasopharyngeal carcinoma. Radiother Oncol. 2000;54:135–142. doi: 10.1016/S0167-8140(99)00177-2. [DOI] [PubMed] [Google Scholar]
- 13.King WW, Ku PK, Mok CO, Teo PM. Nasopharyngectomy in the treatment of recurrent nasopharyngeal carcinoma: a twelve-year experience. Head Neck. 2000;22(3):215–222. doi: 10.1002/(SICI)1097-0347(200005)22:3<215::AID-HED2>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 14.Hsu MM, Hong RL, Ting LL, Ko JY, Sheen TS, Lou PJ. Factors affecting the overall survival after salvage surgery in patients with recurrent nasopharyngeal carcinoma at the primary site: experience with 60 cases. Arch Otolaryngol Head Neck Surg. 2001;127(7):798–802. [PubMed] [Google Scholar]
- 15.Vlantis AC, Chan HS, Tong MC, Yu BK, Kam MK, van Hasselt CA. Surgical salvage nasopharyngectomy for recurrent nasopharyngeal carcinoma: a multivariate analysis of prognostic factors. Head Neck. 2011;33(8):1126–1131. doi: 10.1002/hed.21585. [DOI] [PubMed] [Google Scholar]
- 16.Vlantis AC, Lee DL, Wong EW, Chow SM, Ng SK, Chan JY. Endoscopic nasopharyngectomy in recurrent nasopharyngeal carcinoma: a case series, literature review, and pooled analysis. Int Forum Allergy Rhinol. 2017;7(4):425–432. doi: 10.1002/alr.21881. [DOI] [PubMed] [Google Scholar]
- 17.Ko JY, Wang CP, Ting LL, Yang TL, Tan CT. Endoscopic nasopharyngectomy with potassium-titanyl-phosphate (KTP) laser for early locally recurrent nasopharyngeal carcinoma. Head Neck. 2009;31(10):1309–1315. doi: 10.1002/hed.21091. [DOI] [PubMed] [Google Scholar]
- 18.Chen MY, Wen WP, Guo X, et al. Endoscopic nasopharyngectomy for locally recurrent nasopharyngeal carcinoma. Laryngoscope. 2009;119(3):516–522. doi: 10.1002/lary.20133. [DOI] [PubMed] [Google Scholar]
- 19.Emanuelli E, Albu S, Cazzador D, Pedruzzi B, Babighian G, Martini A. Endoscopic surgery for recurrent undifferentiated nasopharyngeal carcinoma. J Craniofac Surg. 2014;25(3):1003–1008. doi: 10.1097/SCS.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 20.Hsu NI, Shen PH, Chao SS, Ong YK, Li CS. En bloc resection concept for endoscopic endonasal nasopharyngectomy: surgical anatomy and outcome. Chin Med J. 2014;127(16):2934–2939. [PubMed] [Google Scholar]
- 21.Wong EHC, Liew YT, Loong SP, Prepageran N. Five-year survival data on the role of endoscopic endonasal nasopharyngectomy in advanced recurrent rT3 and rT4 nasopharyngeal carcinoma. Ann Otol Rhinol Laryngol. 2020;129(3):287–293. doi: 10.1177/0003489419887410. [DOI] [PubMed] [Google Scholar]
- 22.Zou X, Han F, Ma WJ, et al. Salvage endoscopic nasopharyngectomy and intensitymodulated radiotherapy versus conventional radiotherapy in treating locally recurrent nasopharyngeal carcinoma. Head Neck. 2015;37(8):1108–1115. doi: 10.1002/hed.23719. [DOI] [PubMed] [Google Scholar]
- 23.Thamboo A, Petal VS, Hwang PH. 5- year outcomes of salvage endoscopic nasopharyngectomy for recurrent nasopharyngeal cancer. J Otolaryngol Head Neck Surg. 2021;50:12. doi: 10.1186/s40463-020-00482-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hua YJ, Han F, Lu LX, et al. Long-term treatment outcome of recurrent nasopharyngeal carcinoma treated with salvage intensity modulated radiotherapy. Eur J Cancer. 2012;48(18):3422–3428. doi: 10.1016/j.ejca.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 25.Qiu S, Lin S, Tham IW, Pan J, Lu J, Lu JJ. Intensity-modulated radiation therapy in the salvage of locally recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2012;83(2):676–683. doi: 10.1016/j.ijrobp.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Fee WE, Jr, Moir MS, Choi EC, Goffinet D. Nasopharyngectomy for recurrent nasopharyngeal cancer: a 2- to 17-year follow-up. Arch Otolaryngol Head Neck Surg. 2002;128(3):280–284. doi: 10.1001/archotol.128.3.280. [DOI] [PubMed] [Google Scholar]
- 27.You R, Zou X, Hua YJ, et al. Salvage endoscopic nasopharyngectomy is superior to intensity-modulated radiation therapy for local recurrence of selected T1–T3 nasopharyngeal carcinoma - a case-matched comparison. Radiother Oncol. 2015;115(3):399–406. doi: 10.1016/j.radonc.2015.04.024. [DOI] [PubMed] [Google Scholar]