Abstract
The basic principle of head and neck surgery is based on the identification and preservation of important structures, rather than avoidance. Thyroid surgeries are the most frequently performed endocrine procedures worldwide. Recurrent laryngeal nerve (RLN) palsy after thyroid surgery is a serious postoperative complication that can diminish the quality of life. While it is generally accepted that direct visualisation of the nerve is the gold standard, intraoperative nerve monitoring (IONM) is being used increasingly as an adjuvant to help identify the nerve. This study was carried out in Mahatma Gandhi medical college and hospital, Jaipur, Rajasthan from June 2018 to March 2020. 100 patients were enrolled in the study. RLN is identified & visualized in Beahr’s triangle or in Lore’s triangle. We have randomly selected the patient and use IONM as an adjunct to standard visual identification of the recurrent laryngeal nerve (RLN) to prevent nerve lesion. 8 out of 108 nerves which were at risk during thyroid surgery were found injured. 2 of 50 (4%) nerves at risk were injured with IONM that caused temporary paresis. Without IONM, 5 of 58 (8.6%) nerves at risk suffered temporary paresis and 1of 58(1.72%) had paralysis. Visual nerve identification alone remains the gold standard of recurrent laryngeal nerve management in thyroid surgery and one can use operating microscope for magnification. Neuromonitoring helps to identify the RLN particularly in difficult cases, but it does not decrease the injury to RLN as compared to visualization alone.
Keywords: Thyroid surgery, Recurrent laryngeal nerve, Intraoperative nerve monitoring (IONM), Thyroidectomy
Introduction
The basic principle of head and neck surgery is based on the identification and preservation of important structures, rather than avoidance [1]. Thyroid surgeries are the most frequently performed endocrine procedures worldwide. Recurrent laryngeal nerve (RLN) palsy after thyroid surgery is a serious postoperative complication that can diminish the quality of life [2]. While it is generally accepted that direct visualisation of the nerve is the gold standard, intraoperative nerve monitoring (IONM) is being used increasingly as an adjuvant to help identify the nerve [3]. In the 1950s, Riddell [4] reported this technique of comparing identification and non-identification of the nerve during thyroidectomies. Since that report, nerve visualization, anatomical knowledge, and surgeons’ experience have been the most important tools for protecting RLN and hence serve as the standard of care. Intra-operative nerve monitoring (IONM) has become the widely used adjunct for identifying and preserving RLN. This technology uses both spontaneous and evoked potentials to monitor the functionality of the vocalis muscle and the RLN. The surgeon uses a probe to send a stimulatory impulse to the nerve stimulating the vocalis muscle; in turn, the surface electrodes on the endotracheal tube pick up if the vocal cord muscles respond to the stimulus. An injured nerve will require a higher stimulus than an intact one, allowing for the detection of early injury [5]. A large prospective evaluation study showed that IONM helps during revision surgery, but research has not proven IONM use to be more effective than nerve identification alone for protecting the nerve during thyroid surgery [6]. Aim of this study is to establish whether the use of IONM to identify and preserve RLN during thyroid surgery is worth or not.
Material & Method
This study was carried out in Mahatma Gandhi medical college and hospital, Jaipur, Rajasthan from June 2018 to March 2020. 100 patients were enrolled in the study who require thyroid surgery according to inclusion and exclusion criteria.
Inclusion Criteria
All the patients of age group > 18 years, having thyroid swelling and who will require surgery.
Exclusion Criteria
Patients age < 18 years.
Patients who are unfit/ unwilling for surgery.
Patients with deranged thyroid function test.
RLN is identified & visualized in Beahr’s triangle (bounded by common carotid artery as base, inferior thyroid artery superiorly and recurrent laryngeal nerve as lower arm of triangle) or in Lore’s triangle (bounded medially by the trachea / oesophagus, laterally by the carotid artery and superiorly inferior pole of thyroid) and followed upward in Tracheo-oesophageal groove and we look for the branches if present till cricothyroid joint. We have randomly selected the patient and use IONM as an adjunct to standard visual identification of the recurrent laryngeal nerve (RLN) to prevent nerve lesion. We have use NIM-Response 3.0 System (Medtronic Xomed, Jacksonville, Florida, USA) for RLN monitoring. It transforms laryngeal muscle activity into audible and visual EMG signals whenever the RLN is stimulated intraoperatively. This system consists of a combination of two electrical circuits a stimulation side and a recording side. The stimulation side consists of a nerve stimulator probe which transmits electric current to the nerve, and a grounding electrode. The nerve stimulation probe can be either monopolar or bipolar. The recording side consists of the endotracheal tube with its surface electrodes, which are placed strategically at the level of the vocal cord, and their ground electrodes. These two main systems combine on the interconnection box, through which they connect to the monitor. Tracheal intubation is done and non-paralysing anaesthesia is administered for the rest of the procedure as muscle relaxants can interfere with the nerve monitoring process. Every time before ligating any vessel in Beahr’s and Lore’s triangle, a hand-held probe was used to identify RLN. In case RLN is identified, sound and graphics will appear on the monitor screen which alerts the surgeon.
Results
Amongst the 100 patients included in our study, 108 recurrent laryngeal nerves were at risk of injury. Out of 100, 50 patients were randomly selected and operated with IONM to check its efficacy. IONM was used to identify and preserve RLN. In case of remaining 58 nerves, RLN was preserved with visualization alone. Of the 100 patients, overall female preponderance was seen with 79 cases & remaining 21 cases were males. Male: Female ratio is 1: 3.76.
In our study 100 cases were operated for various causes of thyroid swelling. Maximum number of patients underwent Hemithyroidectomy i.e. 83 cases. 6 patients underwent Total thyroidectomy with ACND followed by Completion thyroidectomy with ACND and B/L PLND in 5 cases, while 4 patients underwent Completion thyroidectomy and 2 cases had Total thyroidectomy with ACND and B/L PLND (Table 1).
Table 1.
Operative procedures performed in the patients
| Surgery | (n = 100)(n)(%) |
|---|---|
| Hemithyroidectomy | 83(83%) |
| Total thyroidectomy with ACND & B/L PLND | 2(2%) |
| Total thyroidectomy with ACND | 6(6%) |
| Completion thyroidectomy | 4(4%) |
| Completion thyroidectomy with ACND & B/L PLND | 5(5%) |
Post operatively all thyroidectomy specimens were sent for histopathological examination. Most histopathological reports were of colloid goiter with 56 cases followed by 10 cases of Hashimoto’s thyroiditis, 8 cases of Follicular adenoma, 7 cases of Non invasive follicular neoplasm with papillary nuclear pattern (NIFTP) and 5 cases each of follicular carcinoma, papillary carcinoma and medullary carcinoma of thyroid were seen. 4 cases were reported to be of normal thyroid in which previously hemithyroidectomy was done (Table 2).
Table 2.
Histopathology of Thyroidectomy specimen
| Histopathology Report | (n = 100)Number of patients (n)(%) |
|---|---|
| Colloid goiter | 56(56%) |
| Follicular adenoma | 8(8%) |
| Follicular carcinoma | 5(5%) |
| Hashimoto’s thyroiditis | 10(10%) |
| Non invasive follicular neoplasm with papillary nuclear pattern (NIFTP) | 7(7%) |
| Papillary carcinoma | 5(5%) |
| Medullary carcinoma thyroid | 5(5%) |
| Normal thyroid | 4(4%) |
We define “transient” as an injury in which the mobility of the vocal cords fully recover within 3 months of surgery. A total 8 out of 108 nerves which were at risk during thyroid surgery were found injured. 2 of 50 (4%) nerves at risk were injured with IONM that caused temporary paresis. Without IONM, 5 of 58 (8.6%) nerves at risk suffered temporary paresis and 1of 58(1.72%) had paralysis (Table 3).
Table 3.
Number of nerve injured
| Injured Recurrent laryngeal nerve | Paralysis | Temporary paresis |
|---|---|---|
|
Thyroidectomy with IONM (50 Nerves at risk) |
0 | 2(4%) |
|
Thyroidectomy without IONM (58 Nerves at risk) |
1(1.72%) | 5(8.6%) |
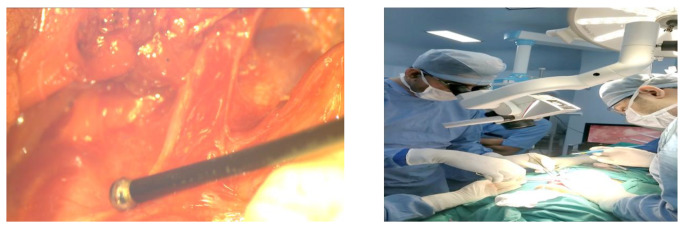
Many studies have proven the valuable role of IONM in certain circumstances, such as revision thyroid surgery and malignancy cases where anatomical landmarks are usually obscured, Fig. 1, 2.
Fig. 1.
a)Intra-operative photo showing nerve monitoring of RLN with neuromonitoring probe b) use of operating microscope for magnification during thyroid suregry
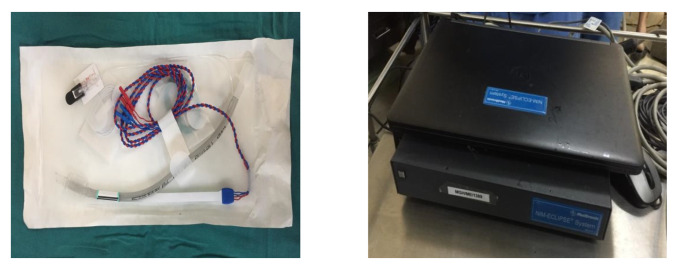
Fig. 2.
Endotracheal tube with surface electrodes & neuromonitoring device used in this study
Disscussion
The incidence of recurrent laryngeal nerve palsy varies from less than 1% to as high as 20% 14. There are several factors that influence the likelihood of nerve injury, which includes the underlying disease, the extent of resection, and the experience of the surgeon [9]; substernal goiters and revision thyroid surgeries have a higher rate of complications because of scarring and loss of normal tissue planes. Even experienced surgeons report inadvertent injury to the nerve and persistent palsy in about 1–2% of patients [7]. Recurrent laryngeal nerve is said to suffer injury in cases of thermal lesions, excessive nerve skeletonization of the nerve, when the nerve’s anatomic integrity is hampered or in case of axon damage which are caused by excessive straining, edema, hematoma formation, difficult tracheal intubation, and neuritis [16]; but the actual causes of recurrent laryngeal nerve injury, especially in those with visual integrity, are still not well understood. Many studies have shown that visual identification of recurrent laryngeal nerve during thyroid surgery has been associated with lower rates of permanent recurrent laryngeal nerve palsy and is considered the gold standard of recurrent laryngeal nerve treatment [13].
Lahey in 1938, started to dissect recurrent laryngeal nerve in every case; careful dissection decreased the number of injuries to the recurrent nerves and this approach is accepted by most endocrine surgeons [14]. Nerve identification is difficult in cases which include revision surgeries, surgery for malignant cases, anatomic variants, a history of radiation or inflammation [9, 14]. Nerve monitoring was developed to aid surgeons for identification of the recurrent laryngeal nerve during thyroid surgery [17].
Nowadays, a wide variety of neuromonitoring techniques are available. The most common method of neuromonitoring is with the help of a special endotracheal tube with electrodes embedded on it which act by registering the effect of stimulation of the vocal cords [18]. Despite the increasing popularity of this technology, its impact in the avoidance of nerve injury and the reduction of the incidence of postoperative nerve palsy remain doubtful [12]. Several non-randomised studies demonstrated that an improved intraoperative recurrent laryngeal nerve identification rate with neuromonitoring resulted in lower palsy rates than in historical patient cohorts with identification alone [10]. A large multicentre study was carried out on 4382 patients and found a statistically significant reduction in rates of transient and permanent recurrent laryngeal nerve paralysis with the use of intraoperative nerve monitoring in surgery for benign goiter; subgroup analysis of the same study found higher rates of injury when intraoperative nerve monitoring was used for total thyroidectomy [10, 12].
A large single-centre study on 1000 consecutive nerve at risk found that continuous nerve monitoring offered no benefit in reducing the risk of nerve injury compared with the adoption of routine nerve identification, with no difference in both the temporary and the permanent nerve injury rates [11, 12]. Dralle in his study concluded that intraoperative nerve monitoring did not lower the risk of nerve injury although failure to visually identify the nerve was associated with a higher rate of injury [8]. In the meta-analysis of Higgins [19], intraoperative neuromonitoring and identification performed alone did not demonstrate a statistically significant difference in rates of total, transient, or persistent RLN palsy.
In a prospective, randomized study of 1000 patients, the prevalence of transient recurrent laryngeal nerve palsy was significantly lower in the group of patients who had surgery with intraoperative neuromonitoring by 2.9% in high-risk patients and 0.9% in low-risk patients [20].
In this study we identified and preserved RLN in either Beahr’s triangle or Lore’s triangle. Before ligating any vessel in Beahr’s and Lore’s triangle, a hand-held probe was used to identify RLN in cases in which IONM were used. In case of confirmation of RLN, sound and graphics appear on the monitor screen which alerts the surgeon. In our study the rates of postoperative recurrent laryngeal nerve paralysis did not differ significantly (p value = 0.809) between the two groups. We used operative microscope in addition to IONM for visualization of RLN. This may one of the additional reasons for low rate of paresis/palsy. The rate of temporary and definitive recurrent laryngeal nerve paralysis was 4.62% and 1.85% respectively. This temporary paresis was recovered completely within 1 month. These were found to be due to either anatomical variations or due to malignancy. Our opinion is that neuromonitoring can help in the nerve identification particularly in difficult situation such as malignancy, revision surgery or anatomic variations. However, difficult situations are not always predictable preoperatively. It was observed that an anatomically intact nerve does not always correlate with normal vocal fold function and that the absence of signal does not necessarily imply nerve dysfunction [15].
In the study of Thomusch a normal intraoperative neuromonitoring signal certainly excluded postoperative vocal cord dysfunction. Indirect stimulation of the RLN via the vagus nerve is a better predictor than direct stimulation of RLN for assessing postoperative dysfunction hence it should be performed to monitor the axonal excitability as well as to see the mechanical intactness of the nerve. Direct nerve stimulation detects the RLN anatomy and hence is used exclusively for this purpose. After assessing the integrity of nerve on one side though direct and indirect stimulation, the surgeon can proceed the operation to the contralateral side, being reassured that the nerve on the resected side has a 99.6% chance of being intact. An absent or abnormal intraoperative neuromonitering signal may be due to technical problems, wrong application or continuous relaxation of vocal cords during surgery due to use of muscle relaxants, resulting in aberrant or absent signal causing failure to predict postoperative palsy. An absent or abnormal signal was a rare phenomenon, with an incidence of 2.7% after indirect recurrent laryngeal nerve stimulation, and in these cases, 45.9% of the patients had postoperative vocal cord dysfunction [10].
The use of such devices during thyroid surgery seems to be more expensive than the use of conventional techniques. This is probably the major disadvantage and particularly for this reason routine nerve monitoring is not cost-effective.
Conclusion
Visual nerve identification alone remains the gold standard of recurrent laryngeal nerve management in thyroid surgery and one can use operating microscope for magnification. The technique of intra-operative neuromonitoring is safe, effective, and reliable in excluding postoperative recurrent laryngeal nerve palsy. Neuromonitoring helps to identify the recurrent laryngeal nerve particularly in difficult cases, but it does not decrease the injury to recurrent laryngeal nerve as compared to visualization alone.
Funding
No funding was there.
Declarations
Compliance with Ethical Standards
All the accepted principles of ethical and professional conduct have been followed and compliance is maintained.
Conflict of Interest
There was no conflict of interest.
Informed consent
Informed consent were obtained from all individual participants included in the study.
Ethical approval
All the procedures performed in this study involving human participants were in accordance with the ethical standards of institutional ethical committee.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mustafa A, Bokare B. Surgical anatomy of external branch of superior laryngeal nerve (EBSLN) in thyroid surgery. Int J Biomedical Adv Res. 2016;7(10):493–496. doi: 10.7439/ijbar.v7i10.3684. [DOI] [Google Scholar]
- 2.Rulli F, Ambrogi V, Dionigi G, Amirhassankhani S, Mineo TC, Ottaviani F, et al. Meta–analysis of recurrent laryngeal nerve injury in thyroid surgery with or without intraoperative nerve monitoring. Acta Otorhinolaryngol Ital. 2014;34:223–229. [PMC free article] [PubMed] [Google Scholar]
- 3.Flukes S, Ling S, Leahy T, Sader C. Intraoperative nerve monitoring in otolaryngology: a survey of clinical practice patterns. Int J Otolaryngol Head Neck Surg. 2013;2:21–26. doi: 10.4236/ijohns.2013.21007. [DOI] [Google Scholar]
- 4.Riddell VH Injury to recurrent laryngeal nerves during thyroidectomy; a comparison between the results of identification and non-identification in 1022 nerves exposed to risk. Lancet. 1956 Sep29;271(6944):638–641 [DOI] [PubMed]
- 5.Dillon FX (2010 Sep) Electromyographic (EMG) neuromonitoring in otolaryngology-head and neck surgery. Anesthesiol Clin 28(3):423–442 [DOI] [PubMed]
- 6.Dralle H, Sekulla C, Haerting J et al (2004 Dec) Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 136(6):1310–1322 [DOI] [PubMed]
- 7.Calò PG, Pisano G, Medas F, Tatti A, Pittau MR, Demontis R, Favoriti P, Nicolosi A. Intraoperative recurrent laryngeal nerve monitoring in thyroid surgery: is it really useful? Clin Ter. 2013;164:e193–e198. doi: 10.7417/CT.2013.1567. [DOI] [PubMed] [Google Scholar]
- 8.Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A, the German IONM Study Group Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008;32:1358–1366. doi: 10.1007/s00268-008-9483-2. [DOI] [PubMed] [Google Scholar]
- 9.Calò PG, Pisano G, Medas F, Tatti A, Tuveri M, Nicolosi A. Risk factors in reoperative thyroid surgery for recurrent goitre. Our experience. G Chir. 2012;33:335–338. [PubMed] [Google Scholar]
- 10.Thomusch O, Sekulla C, Machens A, Neumann HJ, Timmermann W, Dralle H. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg. 2004;389:499–503. doi: 10.1007/s00423-003-0444-9. [DOI] [PubMed] [Google Scholar]
- 11.Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery. 2006;140:866–872. doi: 10.1016/j.surg.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 12.Loch-Wilkinson TJ, Stalberg PL, Sidhu SB, Sywak MS, Wilkinson JF, Delbridge LW. Nerve stimulation in thyroid surgery: is it really useful? ANZ J Surg. 2007;77:377–380. doi: 10.1111/j.1445-2197.2007.04065.x. [DOI] [PubMed] [Google Scholar]
- 13.Chiang FY, Lu IC, Kuo WR, Lee KW, Chang NC, Wu CW. The mechanism of recurrent laryngeal nerve injury during thyroid surgery – the application of intraoperative neuromonitoring. Surgery. 2008;143:743–749. doi: 10.1016/j.surg.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Sari S, Erbil Y, Sümer A, Agcaoglu O, Bayraktar A, Issever H. Ozarmagan S:evaluation of recurrent laryngeal nerve monitoring in thyroid surgery. Int J Surg. 2010;8:474–478. doi: 10.1016/j.ijsu.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 15.Shindo M, Chheda NN. Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2007;133:481–485. doi: 10.1001/archotol.133.5.481. [DOI] [PubMed] [Google Scholar]
- 16.Calò PG, Pisano G, Medas F, Tatti A, Tuveri M, Nicolosi A. The use of harmonic scalpel in thyroid surgery. Our experience. Ann Ital Chir. 2012;83:7–12. [PubMed] [Google Scholar]
- 17.Hermann M, Hellebart C, Freissmuth M. Neuromonitoring in thyroid surgery. Prospective evaluation of intraoperative electrophysiological responses for the prediction of recurrent laryngeal nerve injury. Ann Surg. 2004;240:9–17. doi: 10.1097/01.sla.0000132260.34503.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanabria A, Ramirez A, Kowalski LP, Silver CE, Shaha AR, Owen RP, Suárez C, Khafif A, Rinaldo A, Ferlito A. Neuromonitoring in thyroidectomy: a meta-analysis of effectiveness from randomized controlled trials. Eur Arch Otorhinolaryngol. 2013;270:2175–2189. doi: 10.1007/s00405-013-2557-2. [DOI] [PubMed] [Google Scholar]
- 19.Higgins TS, Gupta R, Ketcham AS, Sataloff RT, Wadsworth JT, Sinacori JT. Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope. 2011;121:1009–1017. doi: 10.1002/lary.21578. [DOI] [PubMed] [Google Scholar]
- 20.Alesina PF, Rolfs T, Hommeltenberg S, Hinrichs J, Meier B, Mohmand W, Hofmeister S, Walz MK. Intraoperative neuromonitoring does not reduce the incidence of recurrent laryngeal nerve palsy in thyroid reoperations: results of a retrospective comparative analysis. World J Surg. 2012;36:1348–1353. doi: 10.1007/s00268-012-1548-6. [DOI] [PubMed] [Google Scholar]