Abstract
Risk stratification based mainly on the impairment of left ventricular ejection fraction has limited performance in patients with nonischemic dilated cardiomyopathy (NIDCM). Evidence is rapidly growing for the impact of myocardial scar identified by late gadolinium enhancement (LGE) cardiac magnetic resonance imaging (CMR) on cardiovascular events. We aim to assess the prognostic value of LGE on long-term arrhythmic and mortality outcomes in patients with NIDCM. PubMed, Scopus, and Cochrane databases were searched from inception to January 21, 2022. Studies that included disease-specific subpopulations of NIDCM were excluded. Data were independently extracted and combined via random-effects meta-analysis using a generic inverse-variance strategy. Data from 60 studies comprising 15,217 patients were analyzed with a 3-year median follow-up. The presence of LGE was associated with major ventricular arrhythmic events (pooled OR: 3.99; 95% CI 3.08, 5.16), all-cause mortality (pooled OR: 2.14; 95% CI 1.81, 2.52), cardiovascular mortality (pooled OR 2.83; 95% CI 2.23, 3.60), and heart failure hospitalization (pooled OR: 2.53; 95% CI 1.78, 3.59). Real-world evidence suggests that the presence of LGE on CMR was a strong predictor of adverse long-term outcomes in patients with NIDCM. Scar assessment should be incorporated as a primary determinant in the patient selection criteria for primary prophylactic implantable cardioverter-defibrillator placement.
Subject terms: Outcomes research, Arrhythmias, Cardiomyopathies
Introduction
Cardiovascular complications particularly major ventricular arrhythmia and heart failure remain the leading causes of morbidity and mortality in patients with nonischemic dilated cardiomyopathy (NIDCM) despite advances in therapeutic strategies1–3. One of many efforts to reduce the risk of ventricular arrhythmia and death is the implantable cardioverter-defibrillator (ICD) insertion. For primary prevention, left ventricular ejection fraction (LVEF) ≤ 35% is the main selection criterion for ICD implantation in NIDCM patients1. However, there is growing evidence, that LVEF has significant limitations: (i) LVEF showed no or weak association with arrhythmic endpoints4; (ii) a recent clinical trial showed that a selection based on LVEF criteria failed to demonstrate mortality benefit3; (iii) less than one-third of ICD implanted patients with LVEF ≤ 35% had appropriate device therapy (ADT)2. Accordingly, LVEF ≤ 35% as an indication for primary ICD implantation has been downgraded from the class of recommendation I to IIa in the recent ESC Guidelines for the treatment of heart failure5 and the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death6.
The pathophysiology of ventricular arrhythmia in NIDCM is frequently a reentry mechanism in the context of myocardial scar1. Late gadolinium enhancement (LGE) cardiovascular magnetic resonance imaging (CMR) is a noninvasive technique for the detection of scar in ischemic and non-ischemic cardiomyopathies. Over the past few years, a number of observational studies, as well as large, multicenter registries, have investigated the importance of LGE on CMR to predict adverse cardiovascular outcomes including cardiovascular mortality and ventricular arrhythmia7–10. These studies have shown that the presence of even a small area of LGE in patient with NIDCM has been associated with worse outcomes8–10. So far, no randomized clinical trial has demonstrated, however, that an intervention based on the information of CMR can reduce the risk of cardiovascular mortality. Guideline statements and Food and Drug Administration (FDA) approvals for medical devices have traditionally been based only on randomized clinical trials (RCT), however more recently the FDA is accepting real-world evidence (RWE) from registry data to aid in regulatory decision-making for medical device use11.
The aim of the present study was to perform a systematic review and meta-analysis to assess the predictive value of LGE on long-term outcomes in patients with NIDCM by utilizing the rapidly growing database and thus provide real-world evidence for consideration in regulatory decision-making.
Methods
Search strategy
This analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statements and Meta-analysis of Observational Studies in Epidemiology (MOOSE)12. We (N.T., R.C.) conducted a systematic search of PubMed, Scopus, and Cochrane library databases from inception until 21 January 2022 for studies on the prognostic value of LGE in NIDCM. The references of included studies were reviewed for the completeness of the result. The search keywords were shown in Supplementary Data.
Study eligibility
The inclusion criteria were: (i) prospective or retrospective cohort studies from patients diagnosed with NIDCM which were published in the peer-review, English-language journals; (ii) NIDCM definition fulfills the ESC guidelines for the diagnosis and treatment of acute and chronic heart failure diagnostic criteria based on LV dilatation and systolic dysfunction in the absence of known abnormal loading conditions or significant coronary artery disease5; (iii) studies with the available data on LGE presentation; (iv) mean follow-up time was longer than 6 months. Studies that included disease-specific subpopulations of NIDCM (e.g. hypertrophic or arrhythmogenic right ventricular cardiomyopathy, left ventricular non-compaction, infiltrative heart disease namely cardiac amyloidosis and sarcoidosis, acute myocarditis, drug- and toxin-induced cardiomyopathy, severe primary valvulopathy) were excluded. Editorials, reviews, conference abstracts, case reports, case series, systematic reviews, and meta-analyses were also excluded. Any disagreements concerning study choices were settled through collaborative conversation.
Two independent reviewers (N.T., R.C.) reviewed abstracts and full texts. The third reviewer (P.C.) will make the final decision when the consensus could not be determined. A study with the largest number of patients was selected for the analysis when two or more studies had an overlapping population.
Data extraction and outcomes
Data extraction was performed by A.M. and M.T. The extracted data were first author, publication year, study site and country, study design, major inclusion, and exclusion criteria, LGE quantification and analysis methods, age, gender, comorbidities, New York Heart Association functional class, medications, and CMR parameters. Endpoints included in the meta-analysis were cardiovascular mortality (cardiovascular death, sudden cardiac death (SCD), and heart transplantation), major ventricular arrhythmic events (SCD, sustained ventricular tachycardia (VT), ventricular fibrillation (VF), and ADT), heart failure hospitalization, all-cause mortality (including heart transplantation), and major adverse cardiovascular events (MACE) by definition of the individual studies (when the definition was not provided, MACE was composite of all-cause mortality, heart transplantation, major ventricular arrhythmic events and heart failure hospitalization).
Quality assessment
The modified Newcastle–Ottawa scale (NOS) for cohort studies was used to assess the quality of included studies based on eight domains categorized in three aspects: patient selection, comparability, and outcome. Two reviewers (A.M., M.T.) evaluated the study quality independently. Any disagreement was resolved by the consensus of the third reviewer (P.C.). Studies with a score of 6 or more were considered high-quality studies.
Statistical analysis
All statistical analyses were performed using STATA version 16.1 (College Station, TX: StataCorp LLC.). The main analyses of each pre-specified outcome were performed using random-effect meta-analysis for binary outcomes using logarithmic odds-ratios (logOR) as effect size. The continuity correction of 0.5 was applied to studies with zero cells. DerSimonian and Laird’s generic inverse variance technique was used to calculate adjusted point estimates from each study, which assigned a weight to each study based on its variance13. In each analysis we reported the odds ratio and their 95% confidence intervals (95% CI) by exponentiating the logOR. The heterogeneity of the population was assessed by Cochran’s Q statistics and I2. The random-effect meta-regression was performed to examine the heterogeneity within the data. Funnel plots and the Egger test were utilized to assess the presence of publication bias14.
Results
A total of 1477 citations were acquired from a systematic search. Of these, 1342 citations were excluded by title and abstract screening, leaving 135 citations for full-text review. Seventy-five citations were excluded due to an ineligible population, redundant cohort, inappropriate outcome, non-English language, and improper study design. Finally, 60 studies were included in a systematic review (Fig. 1).
Figure 1.
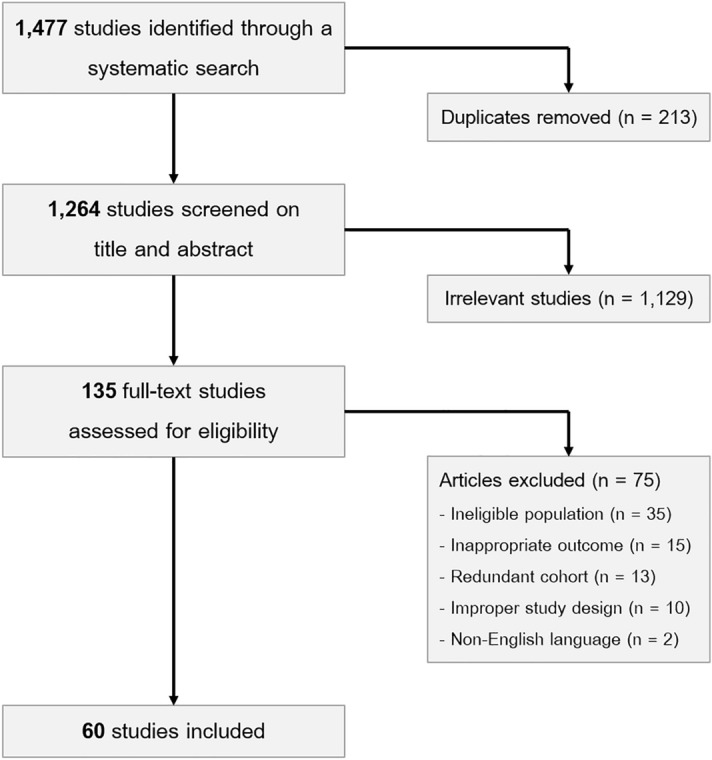
Flow diagram of studies searched in this meta-analysis.
Characteristics of included studies
Of 60 included studies, a total of 15,217 patients were enrolled with the number of participants in each study ranging from 31 to 1165 patients4,9,10,15–71. The median age was 54 years old (IQR: 50.0, 56.4). The proportion of males was 68.7%. The median follow-up time was 3.0 years (IQR: 1.8, 4.2). The median LVEF was 29.5% (IQR: 25.3, 35.8) and LGE was present in 7061 patients (46%, ranging from 25 to 82%) (Table 1).
Table 1.
Baseline characteristics of included studies.
| First author | Year | Study design | N | Inclusion criteria | Age (years) | LVEF (%) | LGE assessment | LGE present n (%) | Endpoint | Follow-up (year) |
|---|---|---|---|---|---|---|---|---|---|---|
| Wu66 | 2008 | Prospective cohort | 65 | NIDCM, LVEF ≤ 35%, primary ICD prevention | 55 ± 12 | 23.5 ± 10 | Visualization* | 27 (41.5%) | CV mortality, major VA event, HHF | 1.4 + 17 |
| Looi42 | 2010 | Prospective cohort | 103 | NIDCM, LVEF < 50%, clinical HF | 58 ± 13 | 32 ± 12 | Visualization† | 31 (30%) | All-cause mortality, major VA event, HHF | 1.8 ± 0.9 |
| Kono37 | 2010 | Prospective cohort | 32 | NIDCM, LVEF < 40% | 61.1 ± 11.5 | 21.3 ± 12 | Intensity > 2 SD† | 18 (56.3%) | All-cause mortality, CV mortality, major VA event, HHF | 2.6 + 1.1 |
| Cho21 | 2010 | Prospective cohort | 79 | NIDCM, LVEF < 35% | 56.4 ± 13.5 | 26.7 ± 8.4 | Visualization† | 42 (53.2%) | CV mortality, HHF | 1.6 ± 0.8 |
| Iles32 | 2011 | Prospective cohort | 61 | NIDCM, advanced HF, primary ICD prevention | 54 ± 13 | 26 ± 9 | Intensity > 2 SD† | 31 (61%) | Major VA event | 1.6 |
| Lehrke38 | 2011 | Prospective cohort | 184 | NIDCM, LVEF < 50% | 51.6 ± 1.1 | 31 | Intensity > 2 SD* | 72 (39.1%) | CV mortality, major VA event, HHF | 1.8 ± 0.1 |
| Gao25 | 2012 | Prospective cohort | 65 | NIDCM, LVEF ≤ 35% | 61 ± 11 | 25.5 | Visualization, intensity, FWHM* | 46 (70.8%) | Major VA event | 1.7 ± 0.7 |
| Gulati28 | 2013 | Prospective cohort | 472 | NIDCM for at least 6 months, LVEF < 50% | 51.1 ± 14.7 | 37.2 ± 13.1 | FWHM* | 142 (30.1%) | All-cause mortality, major VA event, HHF | 5.3 |
| Neilan48 | 2013 | Prospective cohort | 162 | NIDCM, LVEF < 50%, primary ICD prevention | 55 ± 14 | 28 ± 9 | Visualization, intensity > 2 SD, FWHM* | 81 (50%) | CV mortality, major VA event | 2.2 |
| Li41 | 2013 | Retrospective cohort | 293 | NIDCM, LVEF < 50% | 48.9 ± 15 | 33.5 ± 8.7 | Visualization† | 145 (49.5%) | All-cause mortality | 3.2 |
| Müller46 | 2013 | Prospective cohort | 185 | Newly diagnosed NIDCM, clinical HF | 51.2 ± 15.9 | 43.3 ± 16 | Visualization† | 94 (50.8%) | All-cause mortality, major VA event, HHF | 1.75 |
| Masci44 | 2014 | Prospective cohort | 228 | NIDCM, no history of HF | 50 ± 15 | 43 ± 10 | Visualization† | 61 (27%) | CV mortality, major VA event, HHF | 1.9 |
| Pöyhönen54 | 2014 | Retrospective cohort | 86 | NIDCM, clinical HF | 53 | 50 | Visualization* | 62 (70.9%) | MACE including CV mortality, major VA event | 2.3 |
| Rodríguez-Capitán57 | 2014 | Retrospective cohort | 64 | NIDCM, LVEF < 50% | 56.2 ± 13.4 | 29.1 ± 7.6 | Visualization† | 23 (35.9%) | CV mortality, major VA event, HHF | 2.6 |
| Machii43 | 2014 | Retrospective cohort | 72 | NIDCM, LVEF < 45%, clinical HF | 64 ± 14 | 24.8 ± 10.6 | Intensity > 3 SD† | 48 (67%) | CV mortality, major VA event, HHF | 3 ± 1.7 |
| Nabeta47 | 2014 | Prospective cohort | 76 | Newly diagnosed NIDCM, LVEF < 45% | 56 ± 13 | 30.2 ± 7.3 | Intensity > 5 SD* | 36 (47.4%) | MACE including major VA event, HHF | 0.9 ± 0.3 |
| Yamada68 | 2014 | Prospective cohort | 57 | NIDCM, LVEF < 50% | 55 ± 13 | 30 ± 11 | Visualization, intensity > 2 SD* | 25 (43.9%) | CV mortality, major VA event, HHF | 5.9 ± 2.6 |
| Perazzolo Marra51 | 2014 | Prospective cohort | 137 | NIDCM, LVEF < 50% | 49 | 36 | Visualization, intensity > 2 SD* | 76 (55.5%) | CV mortality, major VA event, HHF | 3 |
| Sadahiro58 | 2015 | Retrospective cohort | 76 | NIDCM, LVEF < 45%, clinical HF | 54 ± 14.9 | 21.9 ± 9.7 | Visualization† | 39 (51.3%) | All-cause mortality, CV mortality, HHF | 2.22 ± 0.15 |
| Tateishi63 | 2015 | Prospective cohort | 207 | NIDCM, LVEF < 50% | 50 ± 16 | 27 ± 11 | Visualization† | 105 (50.7%) | CV mortality, major VA event, HHF | 3.6 |
| Piers53 | 2015 | Prospective cohort | 87 | NIDCM, LVEF < 50%, primary ICD prevention | 56 ± 13 | 29 ± 12 | Intensity > 35%* | 55 (63%) | Major VA event | 3.75 |
| Venero64 | 2015 | Retrospective cohort | 31 | Newly diagnosed NIDCM, LVEF ≤ 45% | 46 ± 14 | 18 ± 8.8 | Visualization† | 18 (58%) | All-cause mortality, MACE including mortality, HHF | 1 |
| Chimura19 | 2015 | Retrospective cohort | 175 | NIDCM, LVEF < 35%, clinical HF | 60 + 15 | 29 + 5.4 | Visualization† | 122 (70%) | Major VA event | 5.1 + 3.3 |
| Gaztanaga26 | 2016 | Retrospective cohort | 105 | NIDCM, LVEF ≤ 40% | 51 ± 14 | 25.5 ± 9 | Visualization, intensity > 2 SD* | 71 (67.6%) | All-cause mortality, major VA event, HHF | 2.2 ± 1.6 |
| Shin60 | 2016 | Retrospective cohort | 365 | NIDCM, LVEF < 50%, clinical HF | 54.1 ± 14.5 | 26.5 ± 10.9 | Visualization, FWHM* | 261 (71.5%) | Major VA event | 1.25 |
| Puntmann55 | 2016 | Prospective cohort | 637 | NIDCM | 50 | 47 | Visualization, FWHM* | 171 (27%) | All-cause mortality | 1.8 |
| Hu31 | 2016 | Prospective cohort | 85 | NIDCM, LVEF < 45%, clinical HF | 56.5 ± 15.2 | 42 ± 13.6 | Visualization, intensity* | 35 (41.2%) | CV mortality, major VA event, HHF | 7 |
| Youn70 | 2017 | Prospective cohort | 117 | NIDCM, LVEF ≤ 40% | 51.9 ± 16.7 | 24.9 ± 8.1 | Visualization, intensity > 5 SD* | 82 (70.1%) | MACE including CV mortality, HHF | 0.93 |
| Halliday10 | 2017 | Prospective cohort | 399 | NIDCM, LVEF ≥ 40% | 49.9 ± 15.3 | 49.6 ± 4.9 | Visualization, FWHM* | 101 (25.3) | All-cause mortality, major VA event, MACE including CV mortality, HHF | 4.6 |
| Chimura20 | 2017 | Retrospective cohort | 179 | NIDCM, LVEF < 50% | 61 ± 15 | 33 | Visualization† | 100 (56%) | MACE including CV mortality, HHF | 2.5 |
| Arenja15 | 2017 | Retrospective cohort | 441 | NIDCM, LVEF < 55%, clinical HF | 53.5 ± 15.1 | 36.2 ± 12.9 | Visualization† | 185 (42%) | MACE including CV mortality, major VA event, HHF | 4.2 |
| Leyva39 | 2017 | Retrospective cohort | 252 | NIDCM, clinical HF | 66.6 ± 10 | 24.8 ± 12.4 | Visualization† | 68 (27.0%) | All-cause mortality, CV mortality, major VA event, HHF | 3.8 |
| Zhang71 | 2018 | Prospective cohort | 220 | NIDCM, LVEF < 50% | 49.5 ± 13.4 | 25.4 ± 10.4 | Intensity > 2 SD† | 101 (45.9%) | All-cause mortality, CV mortality, major VA event, HHF | 5.1 |
| Pi52 | 2018 | Prospective cohort | 172 | NIDCM, LVEF < 40% | 56.4 ± 14.3 | 23.7 ± 7.9 | Visualization, intensity > 6 SD* | 66 (38.4%) | All-cause mortality | 3.9 |
| Gutman29 | 2019 | Prospective cohort | 452 | NIDCM, LVEF ≤ 35%, clinical HF | 53.4 | 25.2 | Visualization† | 277 (61.3%) | All-cause mortality, CV mortality | 3.2 |
| Vita65 | 2019 | Retrospective cohort | 240 | NIDCM, LVEF < 60%, clinical HF | 49 ± 16 | 43 ± 15 | Visualization, intensity > 4 SD* | 81 (35%) | MACE including all-cause mortality, HHF | 3.8 ± 1.6 |
| Sree Raman62 | 2019 | Prospective cohort | 49 | NIDCM, LVEF ≤ 45%, clinical HF | 61 | 20 | Visualization† | 17 (34.7%) | CV mortality, major VA event, HHF | 8.2 |
| Halliday30 | 2019 | Prospective cohort | 874 | NIDCM, LVEF < 50% | 53.4 ± 14.7 | 36.4 ± 12.7 | Visualization, FWHM* | 300 (34.3%) | All-cause mortality, major VA event | 4.9 |
| Yi69 | 2020 | Retrospective cohort | 378 | NIDCM, LVEF < 50%, clinical HF | 55 ± 15 | 24.1 ± 8.9 | Visualization, FWHM* | 258 (68.3%) | MACE including all-cause mortality, major VA event, HHF | 3.4 ± 3 |
| Cojan-Minzat23 | 2020 | Prospective cohort | 178 | Newly diagnosed NIDCM, LVEF ≤ 45% | 48 ± 14.4 | 35 ± 9.3 | Intensity > 5 SD* | 64 (36.0%) | MACE including major VA event, HHF | 1.4 |
| Behera17 | 2020 | Retrospective cohort | 112 | NIDCM, LVEF < 50% | 40 | 21 | Intensity > 2 SD* | 44 (39%) | All-cause mortality, CV mortality, major VA event, HHF | 2 ± 0.9 |
| Barison16 | 2020 | Retrospective cohort | 183 | NIDCM, primary ICD prevention | 66 | 27 | Visualization, intensity > 6 SD* | 116 (63%) | Major VA event | 2.5 |
| Elming9 | 2020 | Prospective cohort | 236 | NIDCM, LVEF ≤ 35%, NT-proBNP > 200 pg/mL | 61 | 33 | Visualization, FWHM* | 113 (47.9%) | All-cause mortality, CV mortality, major VA event | 5.3 |
| Cittar22 | 2021 | Retrospective cohort | 273 | NIDCM, LVEF < 50% | 51 | 34 | Visualization† | 140 (52%) | MACE including CV mortality, major VA event | 3.25 |
| Ota50 | 2021 | Retrospective cohort | 101 | NIDCM, LVEF < 50%, clinical HF | 61.2 ± 12.3 | 32.3 ± 9.3 | Visualization, intensity > 5 SD* | 53 (52.5%) | MACE including CV mortality, major VA event, HHF | 5.4 |
| Infante33 | 2021 | Retrospective cohort | 86 | NIDCM, LVEF ≤ 50% | 44.9 ± 16.1 | 36.9 ± 12.2 | Visualization† | 55 (64%) | CV mortality, major VA event, HHF | 4.9 ± 3.2 |
| Kolluru36 | 2021 | Prospective cohort | 61 | NIDCM, LVEF ≤ 40%, clinical HF | 54 ± 13 | 33 | Visualization, intensity > 2.5 SD* | 21 (34.4%) | MACE including CV mortality, major VA event | 2 ± 0.3 |
| Kim34 | 2021 | Retrospective cohort | 78 | NIDCM, LVEF < 35%, clinical HF | 54.9 ± 13.6 | 25.4 | Intensity > 5 SD* | 63 (80.8%) | MACE including CV mortality, major VA event, HHF | 3 |
| Chen18 | 2021 | Retrospective cohort | 157 | NIDCM, LVEF ≤ 50% | 52.3 ± 16.1 | 27 ± 10.7 | Visualization, intensity > 5 SD* | 121 (77.1%) | All-cause mortality, major VA event | 1.1 |
| Klem35 | 2021 | Prospective cohort | 1020 | NIDCM, LVEF < 50% | 54 | 33 | Visualization, intensity > 2 SD* | 461 (45.2%) | All-cause mortality, CV mortality, major VA event | 5.2 |
| Xu67 | 2021 | Prospective cohort | 412 | NIDCM | 48 ± 14.4 | 23.7 ± 9.8 | Visualization, FWHM* | 201 (48.8%) | All-cause mortality | 2.3 |
| Ochs49 | 2021 | Retrospective cohort | 350 | NIDCM, LVEF ≤ 45% | 52.2 ± 15.2 | 36.4 ± 13.7 | Visualization† | 134 (38.3%) | MACE including CV mortality, major VA event | 4.2 |
| Raafs56 | 2021 | Prospective cohort | 209 | NIDCM, LVEF < 50% | 54 ± 13 | 34 ± 12 | Visualization, FWHM* | 65 (31%) | MACE including all-cause mortality, major VA event, HHF | 6.3 |
| Fu24 | 2021 | Retrospective cohort | 126 | NIDCM, LVEF < 40% | 49.9 ± 15.8 | 22.3 ± 8.1 | Intensity > 5 SD* | 66 (52.4%) | MACE including CV mortality, HHF | 2.5 |
| Mikami45 | 2021 | Prospective cohort | 645 | NIDCM, LVEF ≤ 50% | 56 ± 14 | 37 ± 11 | Visualization† | 306 (47%) | MACE including all-cause mortality, HHF | 2.9 |
| Shams59 | 2021 | Retrospective cohort | 75 | NIDCM, LVEF < 45% | 38.7 ± 13 | 29.3 ± 12 | Visualization† | 28 (37.3%) | MACE including all-cause mortality, major VA event, HHF | 3.3 ± 2.3 |
| Shu61 | 2021 | Retrospective cohort | 129 | NIDCM, LVEF < 35% | 47 | 15.33 | Intensity > 6 SD* | 97 (82.2%) | MACE including all-cause mortality, major VA event | 1.4 |
| Guaricci27 | 2021 | Prospective cohort | 1000 | NIDCM, LVEF < 50% | 56.7 ± 14.2 | 33.4 ± 10.9 | Visualization† | 457 (46%) | All-cause mortality, major VA event | 2.6 |
| Di Marco4 | 2021 | Retrospective cohort | 1165 | NIDCM, LVEF < 50%, nonischemic non-dilated cardiomyopathy | 58 | 39 | Visualization† | 486 (41.7%) | Major VA event | 3 |
| Li40 | 2022 | Retrospective cohort | 659 | NIDCM, LVEF < 45% | 45 ± 15 | 29.6 ± 9.3 | FWHM* | 355 (55.9%) | CV mortality | 5.4 ± 1.8 |
*Studies reported the extent of myocardial scar (late gadolinium enhancement quantification).
†Studies reported the presence or absence of late gadolinium enhancement.
LGE late gadolinium enhancement, LVEF left ventricular ejection fraction, NIDCM nonischemic dilated cardiomyopathy, ICD implantable cardioverter-defibrillator, CV cardiovascular, HHF hospitalized heart failure, MACE major adverse cardiovascular events, VA ventricular arrhythmia, FWHM full width at half maximum.
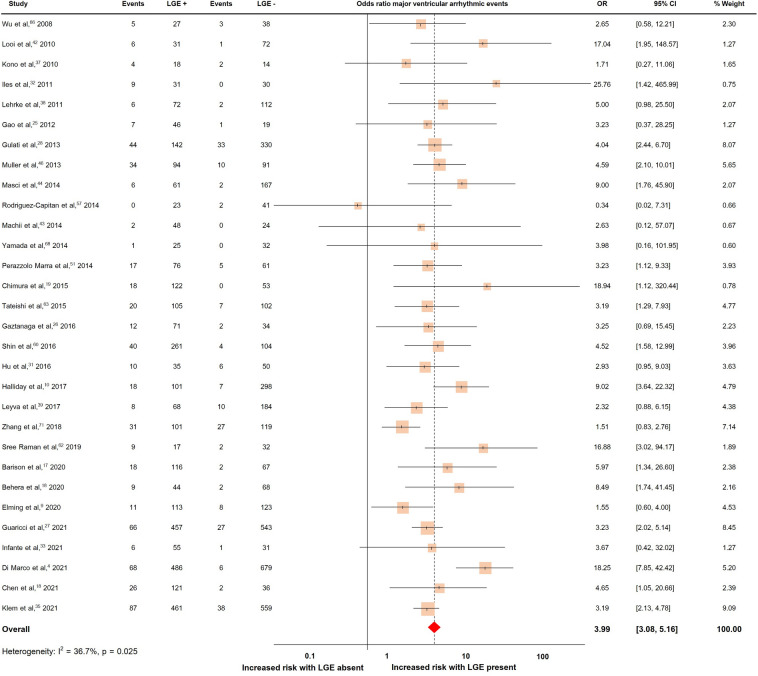
LGE and major ventricular arrhythmic events
Thirty studies with a total of 7541 patients reported major ventricular arrhythmic events, which occurred in 810 patients (10.7%)4,9,16–19,25–28,31–33,35,37–39,42–44,46,51,57,60,62,63,66,68,71. The pooled OR and rates of major ventricular arrhythmic events were shown in Fig. 2. The presence of LGE predicted major ventricular arrhythmic events with a pooled OR of 3.99 (95% CI 3.08, 5.16). The heterogeneity (I2) was 36.7% (p = 0.025).
Figure 2.
Forrest plot illustrating the risk of major ventricular arrhythmic events in individual studies.
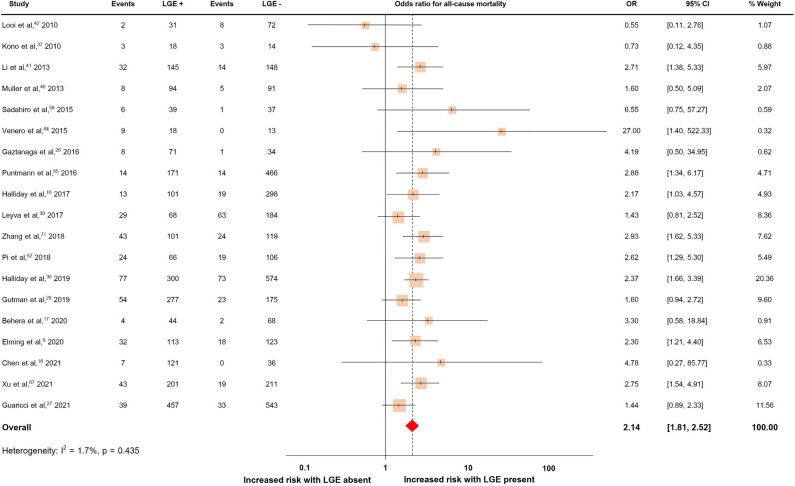
LGE and all-cause mortality
Nineteen studies with a total of 5748 patients reported all-cause mortality, which occurred in 786 patients (13.7%)9,10,17,18,26,27,29,30,37,39,41,42,46,52,55,58,64,67,71. The pooled OR and rates of all-cause mortality were shown in Fig. 3. The presence of LGE predicted all-cause mortality with a pooled OR of 2.14 (95% CI 1.81, 2.52). The heterogeneity (I2) was 1.7% (p = 0.435).
Figure 3.
Forrest plot illustrating the risk of all-cause mortality in individual studies.
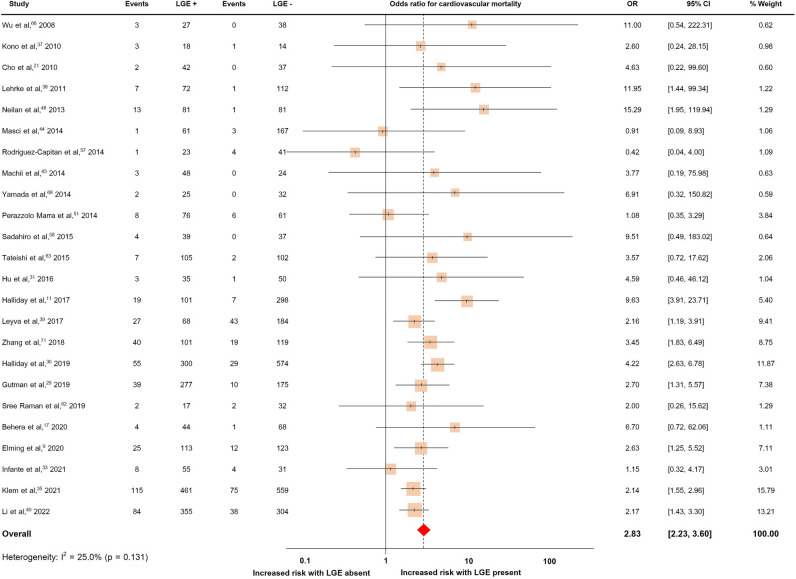
LGE and cardiovascular mortality
Twenty-four studies with a total of 5807 patients reported cardiovascular mortality, which occurred in 734 patients (12.6%)9,10,17,21,29–31,33,35,37–40,43,44,48,51,57,58,62,63,66,68,71. The pooled OR and rates of cardiovascular mortality were shown in Fig. 4. The presence of LGE predicted cardiovascular mortality with a pooled OR of 2.83 (95%CI 2.23, 3.60). The heterogeneity (I2) was 25.0% (p = 0.131).
Figure 4.
Forrest plot illustrating the risk of cardiovascular mortality in individual studies.
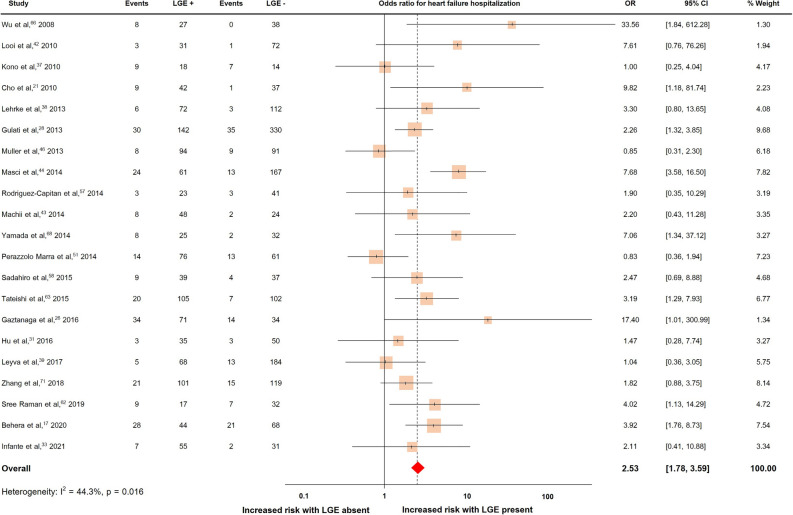
LGE and heart failure hospitalization
Twenty-one studies with a total of 2870 patients reported heart failure hospitalization, which occurred in 407 patients (14.2%)17,21,26,28,31,33,37–39,42–44,46,57,58,62,63,66,68,71. The pooled OR and rates of heart failure hospitalization were shown in Fig. 5. The presence of LGE predicted heart failure hospitalization with a pooled OR of 2.53 (95% CI 1.78, 3.59). The heterogeneity (I2) was 44.3% (p = 0.016).
Figure 5.
Forrest plot illustrating the risk of heart failure hospitalization in individual studies.
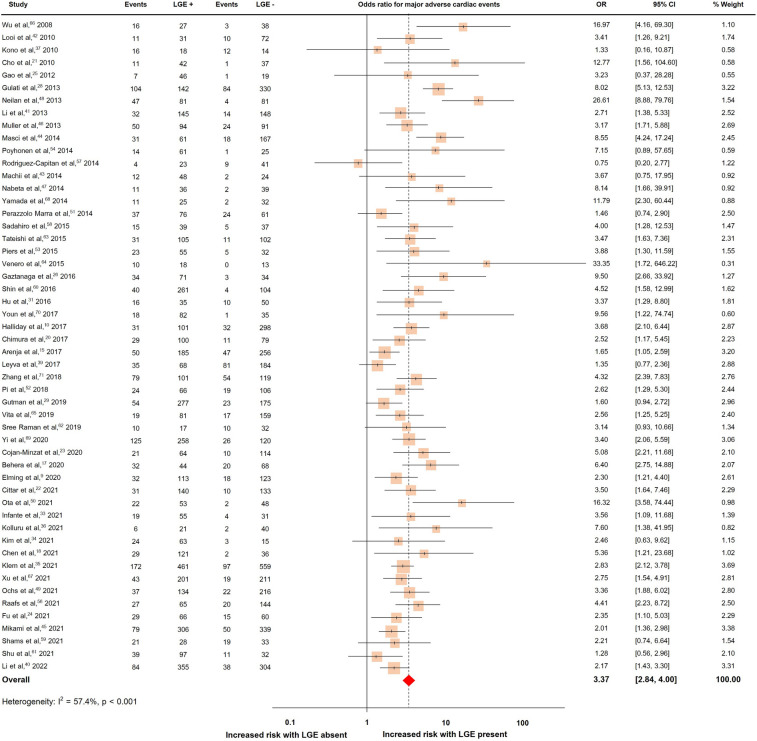
LGE and major adverse cardiac events
Fifty-two studies with a total of 10,923 patients reported MACE, which occurred in 2736 patients (25.1%)9,10,15,17,18,20–26,28,29,31,33–37,39–54,56–71. The pooled OR and rates of MACE were shown in Fig. 6. The presence of LGE predicted MACE with a pooled OR of 3.37 (95% CI 2.84, 4.00). The heterogeneity (I2) was 57.4% (p < 0.001).
Figure 6.
Forrest plot illustrating the risk of major adverse cardiac events in individual studies.
Meta-regression
The meta-regression results revealed no significant association between ORs in the main studies and LVEF or LGE extent for all adverse outcomes. However, a statistically significant negative correlation was observed between the effect sizes of all-cause mortality and age (log odds − 0.04, 95% CI − 0.07, − 0.01; p = 0.01) (Supplementary Table 1).
Quality assessment
All included studies had a NOS score of 6 or more and were considered high-quality studies. Forty-five studies (75%) had a follow-up time of more than 2 years (Supplementary Table 2).
Evaluation of publication bias
The funnel plots of all outcomes appeared asymmetrical (Figs. A–E in the Supplement). The Egger test showed a presence of publication bias (p 0.039).
Discussion
From the current meta-analysis, we found that the presence of LGE on CMR predicts all major clinical outcomes in patients with NIDCM. During the median follow-up time of 3 years, the pooled ORs were 3.99 (95% CI 3.08, 5.16) for major ventricular arrhythmic events, 2.14 (95% CI 1.81, 2.52) for all-cause mortality, 2.83 (95% CI 2.23, 3.60) for cardiovascular mortality, 2.53 (95% CI 1.78, 3.59) for heart failure hospitalization, and 3.37 (95% CI 2.84, 4.00) for MACE. The present meta-analysis reflects the rapidly growing evidence of LGE for risk stratification in NIDCM including 60 studies with over 15,000 patients, some were very recent large, multi-center registries with over 1000 subjects35. The average LGE prevalence was 46%, ranging from 25 to 82%. The LGE quantification techniques used were quite heterogenous between studies, some using the standard deviation of a signal of normal myocardium (e.g. > 2, 2.5, 3, 5 and 6SD) intensity thresholding method, others using the full width at half maximum method and some used visual scoring of LGE extent. Also, the metric system of LGE extent was various; for example, 26 studies used the percentage of LGE compared to the total LV mass (reported range from 2.1 to 17.2%) and 8 studies used absolute extent as a gram of LGE (reported range from 2.9 to 34.5 g). Furthermore, 26 studies did not quantify the extent of LGE (Table 1). Despite the existence of a quantitative relationship between the LGE extent and the increase in arrhythmic risk35, the cutoff threshold for LGE extent (expressed as a percentage of LV mass) and its associated risk has not been determined yet. This is partly due to the use of different quantification methods in the literature. Additionally, a direct comparison to demonstrate the prognostic value between evaluations based on LGE extent and those based on the presence or absence of LGE has not been conducted. Nonetheless, we consider evaluating the presence or absence of LGE to be a practically reasonable and validated risk marker at present. The mere presence of LGE has been associated with a 2.8-fold higher cardiovascular mortality risk and nearly fourfold higher risk for arrhythmic events. Further studies are warranted to refine the optimal LGE quantification technique and determine the LGE extent for improved risk stratification.
To date, the guideline recommendation for primary ICD insertion in patients with NIDCM is depending mainly on LVEF of 35% or less1,5. The role of LGE on CMR has been acknowledged primarily as an additional risk factor that should be considered in conjunction with impaired LVEF when contemplating ICD implantation in the latest guideline (class IIa)6. However, many publications showed that LVEF might not be an appropriate prognosticator3,4,72. Halliday et al.10 conducted a prospective cohort study specifically focusing on patients with NIDCM and mild to moderate LV systolic dysfunction, including only patients with LVEF ≥ 40%. The incidence of the primary composite endpoint, which comprised SCD and aborted SCD (defined as major ventricular arrhythmic events in our study), was 6%. Notably, the incidence was significantly higher at 17.8% in patients with LGE, compared to 2.3% in patients without LGE. On the contrary, LGE on CMR, as a representative of myocardial fibrosis, has emerged as an important risk marker whether based on arrhythmic pathophysiology or evidence from recent studies7,8,73. Furthermore, LGE is a highly consistent risk marker because once it is present on CMR, it does not regress in size or resolve over time74.
The previous systemic review and meta-analysis by Di Marco et al. in 201775 and by Becker et al. in 20187 nicely reported the valuable prognostic tool of LGE in NIDCM patients. Given the exponential growth of studies with a large sample size published in the past few years, the present meta-analysis, which utilized the rapidly growing database available in 2022, strengthened the role of LGE in identifying NIDCM patients at risk of future adverse events. It is important to highlight the fact that we included 15,217 patients from 60 studies compared with 4554 patients from 34 studies as reported by Becker et al. A substantial number of patients provided an adequate number of individuals per each analytic outcome. Hence, we could assess all major clinical endpoints including all-cause mortality that was not reported in the recent meta-analysis7. By comparing the results, we found a very similar OR for heart failure hospitalizations compared with the study by Becker et al. (2.53 vs 2.66). In addition, despite including more than the double of patients than the study by Di Marco et al.75, the pooled OR for major ventricular arrhythmic events was very similar (3.99 vs 4.3). The new larger analysis has largely confirmed the findings of smaller prior ones with consistent results. These emphasize the strength of the association between LGE and specific cardiovascular events.
The meta-regression results revealed no significant association between ORs in the main studies and LVEF or LGE extent for all adverse outcomes. However, a statistically significant negative correlation was observed between the effect sizes of all-cause mortality and age. This indicates that the presence of LGE is more strongly linked to all-cause mortality in a younger population. Our hypothesis is that in an older population, the likelihood of death from non-cardiovascular causes is higher, which diminishes the impact of LGE. This hypothesis is supported by the insignificant meta-regression results of age in other cardiovascular outcomes.
For many years, it has been widely accepted that well-designed RCTs are warranted to provide the best evidence for refining the indication for prophylactic ICD in patients with NIDCM. However, the FDA has already accepted the RWE from registry data to aid in regulatory decision-making for medical device implantation11. While we are still waiting for the results of using the presence of LGE as guidance for ICD implantation from an ongoing multicenter RCT that has just started enrolling subjects76, based on the robust findings derived from the present meta-analysis, which encompasses a substantial number of patients, we believe that these results can enhance the importance of LGE assessment as a primary determinant, transcending its current contributory role.
Limitation
This meta-analysis has some limitations. First, although we performed an extensive systematic search via several large databases, the results are still subjected to publication bias as demonstrated by asymmetrical funnel plots and the Egger test result. Second, there was population heterogeneity in the analysis for major ventricular arrhythmic events, heart failure hospitalization, and MACE. Even though we included only studies focused on NIDCM, the inclusion and exclusion criteria, magnetic field strength, contrast type and dosage, and also pulse sequence used for LGE analysis in the individual studies are varied. Thus, we used the random-effect model in our meta-analysis for this reason. Third, most of the included studies were retrospective and had a small number of participants e.g. 38 studies (61%) had participants of less than 200. Nevertheless, all studies had NOS scores of 6 or more, which are considered high-quality studies and could strengthen the results. Fourth, in some patients with NIDCM, the LGE extent may increase over time, and progressive disease is associated with a particularly high risk74. Therefore, a quantitative assessment of LGE on CMR may be necessary to evaluate the progressive condition. Lastly, LGE on CMR only detected focal and dense but not diffuse and interstitial fibrosis. Newer techniques e.g. T1 mapping, which showed promising result in detecting diffuse fibrosis may provide additional prognostic information in patients with NIDCM.
Conclusion
Real-world evidence suggests that the presence of LGE on CMR was a strong predictor of adverse outcomes including mortalities, major ventricular arrhythmic events, heart failure hospitalization, and MACE in patients with NIDCM. Scar assessment should be incorporated as a primary determinant in the patient selection criteria for primary prophylactic ICD placement.
Supplementary Information
Acknowledgements
We thank Wasinee Promratpan, MD and Noppachai Siranart, MD for assistance with the data entry. The authors acknowledge the support for article processing from Cardiac Center, King Chulalongkorn Memorial Hospital.
Author contributions
N.T. and P.C. wrote the manuscript. N.T., R.C. and P.C. were involved in the study design. N.T., R.C. and J.P. were involved in the literature search and analysis of studies. A.M. and M.T. were involved in data collection. I.K. and P.C. were responsible for the supervision and take responsibility for its content. All authors revised the final version of the manuscript.
Data availability
All data generated or analyzed during this study are included in this published article and in its supplementary information file. The processed data are available from the corresponding author upon request.
Competing interests
Dr. Klem received grant support from Medtronic. All other authors declare no competing of interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-41087-4.
References
- 1.Al-Khatib SM, et al. 2017 AHA/ACC/HRS guideline for management of matients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2018;72:e91–e220. doi: 10.1016/j.jacc.2017.10.054. [DOI] [PubMed] [Google Scholar]
- 2.Bardy GH, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N. Engl. J. Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 3.Køber L, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N. Engl. J. Med. 2016;375:1221–1230. doi: 10.1056/NEJMoa1608029. [DOI] [PubMed] [Google Scholar]
- 4.Di Marco A, et al. Improved risk stratification for ventricular arrhythmias and sudden death in patients with nonischemic dilated cardiomyopathy. J. Am. Coll. Cardiol. 2021;77:2890–2905. doi: 10.1016/j.jacc.2021.04.030. [DOI] [PubMed] [Google Scholar]
- 5.McDonagh TA, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021;42:3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 6.Zeppenfeld K, et al. 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022;43:3997–4126. doi: 10.1093/eurheartj/ehac262. [DOI] [PubMed] [Google Scholar]
- 7.Becker MAJ, et al. The prognostic value of late gadolinium-enhanced cardiac magnetic resonance imaging in nonischemic dilated cardiomyopathy: A review and meta-analysis. JACC Cardiovasc. Imaging. 2018;11:1274–1284. doi: 10.1016/j.jcmg.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Klem I, et al. Assessment of myocardial scarring improves risk stratification in patients evaluated for cardiac defibrillator implantation. J. Am. Coll. Cardiol. 2012;60:408–420. doi: 10.1016/j.jacc.2012.02.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elming MB, et al. Myocardial fibrosis and the effect of primary prophylactic defibrillator implantation in patients with non-ischemic systolic heart failure-DANISH-MRI. Am. Heart J. 2020;221:165–176. doi: 10.1016/j.ahj.2019.10.020. [DOI] [PubMed] [Google Scholar]
- 10.Halliday BP, et al. Association between midwall late gadolinium enhancement and sudden cardiac death in patients with dilated cardiomyopathy and mild and moderate left ventricular systolic dysfunction. Circulation. 2017;135:2106–2115. doi: 10.1161/circulationaha.116.026910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Food and Drug Administration. Use of real-world evidence to support regulatory decision-making for medical devices, guidance for Industry and Food and Drug Administration Staff. https://www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm513027.pdf (Accessed 1 August 2020) (2017).
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Open Med. 2009;3:e123–130. [PMC free article] [PubMed] [Google Scholar]
- 13.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 14.Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337:867–872. doi: 10.1016/0140-6736(91)90201-y. [DOI] [PubMed] [Google Scholar]
- 15.Arenja N, et al. The prognostic value of right ventricular long axis strain in non-ischaemic dilated cardiomyopathies using standard cardiac magnetic resonance imaging. Eur. Radiol. 2017;27:3913–3923. doi: 10.1007/s00330-016-4729-0. [DOI] [PubMed] [Google Scholar]
- 16.Barison A, et al. The extent and location of late gadolinium enhancement predict defibrillator shock and cardiac mortality in patients with non-ischaemic dilated cardiomyopathy. Int. J. Cardiol. 2020;307:180–186. doi: 10.1016/j.ijcard.2020.02.028. [DOI] [PubMed] [Google Scholar]
- 17.Behera DR, et al. Prognostic value of late gadolinium enhancement in cardiac MRI of non-ischemic dilated cardiomyopathy patients. Indian Heart J. 2020;72:362–368. doi: 10.1016/j.ihj.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen W, et al. Ring-like late gadolinium enhancement for predicting ventricular tachyarrhythmias in non-ischaemic dilated cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging. 2021;22:1130–1138. doi: 10.1093/ehjci/jeab117. [DOI] [PubMed] [Google Scholar]
- 19.Chimura M, et al. Distribution of ventricular fibrosis associated with life-threatening ventricular tachyarrhythmias in patients With nonischemic dilated cardiomyopathy. J. Cardiovasc. Electrophysiol. 2015;26:1239–1246. doi: 10.1111/jce.12767. [DOI] [PubMed] [Google Scholar]
- 20.Chimura M, et al. Longitudinal strain combined with delayed-enhancement magnetic resonance improves risk stratification in patients with dilated cardiomyopathy. Heart. 2017;103:679–686. doi: 10.1136/heartjnl-2016-309746. [DOI] [PubMed] [Google Scholar]
- 21.Cho JR, et al. Delayed enhancement magnetic resonance imaging is a significant prognostic factor in patients with non-ischemic cardiomyopathy. Circ. J. 2010;74:476–483. doi: 10.1253/circj.cj-09-0446. [DOI] [PubMed] [Google Scholar]
- 22.Cittar M, et al. Prognostic significance of feature-tracking right ventricular global longitudinal strain in non-ischemic dilated cardiomyopathy. Front. Cardiovasc. Med. 2021;8:765274. doi: 10.3389/fcvm.2021.765274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cojan-Minzat BO, et al. Left ventricular geometry and replacement fibrosis detected by cMRI are associated with major adverse cardiovascular events in nonischemic dilated cardiomyopathy. J. Clin. Med. 2020 doi: 10.3390/jcm9061997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fu H, et al. Prognostic value of multiple cardiac magnetic resonance imaging parameters in patients with idiopathic dilated cardiomyopathy. Int. J. Cardiol. 2021;325:89–95. doi: 10.1016/j.ijcard.2020.09.079. [DOI] [PubMed] [Google Scholar]
- 25.Gao P, et al. Prediction of arrhythmic events in ischemic and dilated cardiomyopathy patients referred for implantable cardiac defibrillator: Evaluation of multiple scar quantification measures for late gadolinium enhancement magnetic resonance imaging. Circ. Cardiovasc. Imaging. 2012;5:448–456. doi: 10.1161/circimaging.111.971549. [DOI] [PubMed] [Google Scholar]
- 26.Gaztanaga J, et al. Prognostic value of late gadolinium enhancement in nonischemic cardiomyopathy. Am. J. Cardiol. 2016;118:1063–1068. doi: 10.1016/j.amjcard.2016.06.059. [DOI] [PubMed] [Google Scholar]
- 27.Guaricci AI, et al. cardiac magnetic resonance for prophylactic implantable-cardioverter defibrillator therapy in non-ischaemic dilated cardiomyopathy: An international registry. Europace. 2021;23:1072–1083. doi: 10.1093/europace/euaa401. [DOI] [PubMed] [Google Scholar]
- 28.Gulati A, et al. Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA. 2013;309:896–908. doi: 10.1001/jama.2013.1363. [DOI] [PubMed] [Google Scholar]
- 29.Gutman SJ, et al. Reduction in mortality from implantable cardioverter-defibrillators in non-ischaemic cardiomyopathy patients is dependent on the presence of left ventricular scar. Eur. Heart J. 2019;40:542–550. doi: 10.1093/eurheartj/ehy437. [DOI] [PubMed] [Google Scholar]
- 30.Halliday BP, et al. Outcome in dilated cardiomyopathy related to the extent, location, and pattern of late gadolinium enhancement. JACC Cardiovasc. Imaging. 2019;12:1645–1655. doi: 10.1016/j.jcmg.2018.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu DJ, et al. Cardiac magnetic resonance and galectin-3 level as predictors of prognostic outcomes for non-ischemic cardiomyopathy patients. Int. J. Cardiovasc. Imaging. 2016;32:1725–1733. doi: 10.1007/s10554-016-0958-1. [DOI] [PubMed] [Google Scholar]
- 32.Iles L, et al. Myocardial fibrosis predicts appropriate device therapy in patients with implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. J. Am. Coll. Cardiol. 2011;57:821–828. doi: 10.1016/j.jacc.2010.06.062. [DOI] [PubMed] [Google Scholar]
- 33.Infante AN, et al. Magnetic resonance imaging of dilated cardiomyopathy: Prognostic benefit of identifying late gadolinium enhancement in Asian patients. Singap. Med. J. 2021;62:347–352. doi: 10.11622/smedj.2019166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim EK, et al. The extent of late gadolinium enhancement can predict adverse cardiac outcomes in patients with non-ischemic cardiomyopathy with reduced left ventricular ejection fraction: A prospective observational study. Korean J. Radiol. 2021;22:324–333. doi: 10.3348/kjr.2020.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klem I, et al. Relationship of LVEF and myocardial scar to long-term mortality risk and mode of death in patients with nonischemic cardiomyopathy. Circulation. 2021;143:1343–1358. doi: 10.1161/circulationaha.120.048477. [DOI] [PubMed] [Google Scholar]
- 36.Kolluru L, Srikala J, Rao HN, Maheen S, Rao BH. Incremental value of late gadolinium enhancement by cardiac MRI in risk stratification of heart failure patients with moderate and severe LV dysfunction. Indian Heart J. 2021;73:49–55. doi: 10.1016/j.ihj.2020.11.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kono AK, et al. Late gadolinium enhancement on cardiac magnetic resonance imaging: Is it associated with a higher incidence of nonsustained ventricular tachycardia in patients with idiopathic dilated cardiomyopathy? Jpn. J. Radiol. 2010;28:355–361. doi: 10.1007/s11604-010-0433-1. [DOI] [PubMed] [Google Scholar]
- 38.Lehrke S, et al. Use of cardiovascular magnetic resonance for risk stratification in chronic heart failure: Prognostic value of late gadolinium enhancement in patients with non-ischaemic dilated cardiomyopathy. Heart. 2011;97:727–732. doi: 10.1136/hrt.2010.205542. [DOI] [PubMed] [Google Scholar]
- 39.Leyva F, et al. Outcomes of cardiac resynchronization therapy with or without defibrillation in patients with nonischemic cardiomyopathy. J. Am. Coll. Cardiol. 2017;70:1216–1227. doi: 10.1016/j.jacc.2017.07.712. [DOI] [PubMed] [Google Scholar]
- 40.Li S, et al. T1 mapping and extracellular volume fraction in dilated cardiomyopathy: A prognosis study. JACC Cardiovasc. Imaging. 2022;15:578–590. doi: 10.1016/j.jcmg.2021.07.023. [DOI] [PubMed] [Google Scholar]
- 41.Li X, et al. Prognostic impact of late gadolinium enhancement by cardiac magnetic resonance imaging in patients with non-ischaemic dilated cardiomyopathy. Int. J. Cardiol. 2013;168:4979–4980. doi: 10.1016/j.ijcard.2013.07.134. [DOI] [PubMed] [Google Scholar]
- 42.Looi JL, et al. Characteristics and prognostic importance of myocardial fibrosis in patients with dilated cardiomyopathy assessed by contrast-enhanced cardiac magnetic resonance imaging. Clin. Med. Insights Cardiol. 2010;4:129–134. doi: 10.4137/cmc.S5900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Machii M, et al. Distribution of late gadolinium enhancement in end-stage hypertrophic cardiomyopathy and dilated cardiomyopathy: Differential diagnosis and prediction of cardiac outcome. Magn. Reson. Imaging. 2014;32:118–124. doi: 10.1016/j.mri.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 44.Masci PG, et al. Incremental prognostic value of myocardial fibrosis in patients with non-ischemic cardiomyopathy without congestive heart failure. Circ. Heart Fail. 2014;7:448–456. doi: 10.1161/circheartfailure.113.000996. [DOI] [PubMed] [Google Scholar]
- 45.Mikami Y, et al. Right ventricular insertion site fibrosis in a dilated cardiomyopathy referral population: Phenotypic associations and value for the prediction of heart failure admission or death. J. Cardiovasc. Magn. Reson. 2021;23:79. doi: 10.1186/s12968-021-00761-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Müller KA, et al. Prognostic value of contrast-enhanced cardiac magnetic resonance imaging in patients with newly diagnosed non-ischemic cardiomyopathy: Cohort study. PLoS One. 2013;8:e57077. doi: 10.1371/journal.pone.0057077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nabeta T, et al. Baseline cardiac magnetic resonance imaging versus baseline endomyocardial biopsy for the prediction of left ventricular reverse remodeling and prognosis in response to therapy in patients with idiopathic dilated cardiomyopathy. Heart Vessels. 2014;29:784–792. doi: 10.1007/s00380-013-0415-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neilan TG, et al. CMR quantification of myocardial scar provides additive prognostic information in nonischemic cardiomyopathy. JACC Cardiovasc. Imaging. 2013;6:944–954. doi: 10.1016/j.jcmg.2013.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ochs A, et al. Myocardial mechanics in dilated cardiomyopathy: Prognostic value of left ventricular torsion and strain. J. Cardiovasc. Magn. Reson. 2021;23:136. doi: 10.1186/s12968-021-00829-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ota S, et al. Implications of multiple late gadolinium enhancement lesions on the frequency of left ventricular reverse remodeling and prognosis in patients with non-ischemic cardiomyopathy. J. Cardiovasc. Magn. Reson. 2021;23:32. doi: 10.1186/s12968-021-00734-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Perazzolo Marra M, et al. Impact of the presence and amount of myocardial fibrosis by cardiac magnetic resonance on arrhythmic outcome and sudden cardiac death in nonischemic dilated cardiomyopathy. Heart Rhythm. 2014;11:856–863. doi: 10.1016/j.hrthm.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 52.Pi SH, et al. Prognostic value of myocardial strain and late gadolinium enhancement on cardiovascular magnetic resonance imaging in patients with idiopathic dilated cardiomyopathy with moderate to severely reduced ejection fraction. J. Cardiovasc Magn. Reson. 2018;20:36. doi: 10.1186/s12968-018-0466-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Piers SR, et al. Myocardial scar predicts monomorphic ventricular tachycardia but not polymorphic ventricular tachycardia or ventricular fibrillation in nonischemic dilated cardiomyopathy. Heart Rhythm. 2015;12:2106–2114. doi: 10.1016/j.hrthm.2015.05.026. [DOI] [PubMed] [Google Scholar]
- 54.Pöyhönen P, Kivistö S, Holmström M, Hänninen H. Quantifying late gadolinium enhancement on CMR provides additional prognostic information in early risk-stratification of nonischemic cardiomyopathy: A cohort study. BMC Cardiovasc. Disord. 2014;14:110. doi: 10.1186/1471-2261-14-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Puntmann VO, et al. T1-mapping and outcome in nonischemic cardiomyopathy: All-cause mortality and heart failure. JACC Cardiovasc. Imaging. 2016;9:40–50. doi: 10.1016/j.jcmg.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 56.Raafs AG, et al. The combination of carboxy-terminal propeptide of procollagen type I blood levels and late gadolinium enhancement at cardiac magnetic resonance provides additional prognostic information in idiopathic dilated cardiomyopathy—A multilevel assessment of myocardial fibrosis in dilated cardiomyopathy. Eur. J. Heart Fail. 2021;23:933–944. doi: 10.1002/ejhf.2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodríguez-Capitán J, et al. Long-term prognostic value of late gadolinium enhancement in a cohort of patients with nonischemic dilated cardiomyopathy. Int. J. Cardiol. 2014;177:17–19. doi: 10.1016/j.ijcard.2014.09.110. [DOI] [PubMed] [Google Scholar]
- 58.Sadahiro T, et al. MRI and serum high-sensitivity C reactive protein predict long-term mortality in non-ischaemic cardiomyopathy. Open Heart. 2015;2:e000298. doi: 10.1136/openhrt-2015-000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shams P, Sultan FAT. Clinical characteristics, cardiac magnetic resonance features, and outcomes of patients with dilated cardiomyopathy—An experience from a South Asian Country. J. Clin. Imaging Sci. 2021;11:40. doi: 10.25259/jcis_126_2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shin DG, et al. Pattern of late gadolinium enhancement predicts arrhythmic events in patients with non-ischemic cardiomyopathy. Int. J. Cardiol. 2016;222:9–15. doi: 10.1016/j.ijcard.2016.07.122. [DOI] [PubMed] [Google Scholar]
- 61.Shu SL, et al. Prognostic value of feature-tracking circumferential strain in dilated cardiomyopathy patients with severely reduced ejection fraction incremental to late gadolinium enhancement. Curr. Med. Sci. 2021;41:158–166. doi: 10.1007/s11596-021-2331-4. [DOI] [PubMed] [Google Scholar]
- 62.Sree Raman K, et al. Long term prognostic importance of late gadolinium enhancement in first-presentation non-ischaemic dilated cardiomyopathy. Int. J. Cardiol. 2019;280:124–129. doi: 10.1016/j.ijcard.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 63.Tateishi E, et al. Prognostic impact of blood pressure response plus gadolinium enhancement in dilated cardiomyopathy. Heart. 2015;101:774–780. doi: 10.1136/heartjnl-2014-307007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Venero JV, et al. Mid wall fibrosis on CMR with late gadolinium enhancement may predict prognosis for LVAD and transplantation risk in patients with newly diagnosed dilated cardiomyopathy-preliminary observations from a high-volume transplant centre. ESC Heart Fail. 2015;2:150–159. doi: 10.1002/ehf2.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vita T, et al. Comparing CMR mapping methods and myocardial patterns toward heart failure outcomes in nonischemic dilated cardiomyopathy. JACC Cardiovasc. Imaging. 2019;12:1659–1669. doi: 10.1016/j.jcmg.2018.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu KC, et al. Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J. Am. Coll. Cardiol. 2008;51:2414–2421. doi: 10.1016/j.jacc.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xu Y, et al. Prognostic value of left ventricular remodelling index in idiopathic dilated cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging. 2021;22:1197–1207. doi: 10.1093/ehjci/jeaa144. [DOI] [PubMed] [Google Scholar]
- 68.Yamada T, et al. Prognostic impact of combined late gadolinium enhancement on cardiovascular magnetic resonance and peak oxygen consumption in ambulatory patients with nonischemic dilated cardiomyopathy. J. Card. Fail. 2014;20:825–832. doi: 10.1016/j.cardfail.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 69.Yi JE, et al. Additive prognostic value of red cell distribution width over late gadolinium enhancement on CMR in patients with non-ischemic dilated cardiomyopathy. Sci. Rep. 2020;10:9212. doi: 10.1038/s41598-020-66198-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Youn JC, et al. Contrast-enhanced T1 mapping-based extracellular volume fraction independently predicts clinical outcome in patients with non-ischemic dilated cardiomyopathy: A prospective cohort study. Eur. Radiol. 2017;27:3924–3933. doi: 10.1007/s00330-017-4817-9. [DOI] [PubMed] [Google Scholar]
- 71.Zhang K, et al. Long-term prognostic value of combined free triiodothyronine and late gadolinium enhancement in nonischemic dilated cardiomyopathy. Clin. Cardiol. 2018;41:96–103. doi: 10.1002/clc.22858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van der Bijl P, Podlesnikar T, Bax JJ, Delgado V. Sudden cardiac death risk prediction: The role of cardiac magnetic resonance imaging. Rev. Esp. Cardiol. (Engl. Ed) 2018;71:961–970. doi: 10.1016/j.rec.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 73.Ganesan AN, Gunton J, Nucifora G, McGavigan AD, Selvanayagam JB. Impact of late gadolinium enhancement on mortality, sudden death and major adverse cardiovascular events in ischemic and nonischemic cardiomyopathy: A systematic review and meta-analysis. Int. J. Cardiol. 2018;254:230–237. doi: 10.1016/j.ijcard.2017.10.094. [DOI] [PubMed] [Google Scholar]
- 74.Mandawat A, et al. Progression of myocardial fibrosis in nonischemic DCM and association with mortality and heart failure outcomes. JACC Cardiovasc. Imaging. 2021;14:1338–1350. doi: 10.1016/j.jcmg.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Di Marco A, et al. Late gadolinium enhancement and the risk for ventricular arrhythmias or sudden death in dilated cardiomyopathy: Systematic review and meta-analysis. JACC Heart Fail. 2017;5:28–38. doi: 10.1016/j.jchf.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 76.Eitel I. Cardiac Magnetic Resonance Guidance of Implantable Cardioverter Defibrillator Implantation in Non-ischemic Dilated Cardiomyopathy (CMR-ICD). ClinicalTrials.gov identifier: NCT04558723. https://clinicaltrials.gov/ct2/show/NCT04558723 (Accessed 18 July 2022) (2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and in its supplementary information file. The processed data are available from the corresponding author upon request.