Abstract
Immune responses can have opposing effects in colorectal cancer (CRC), the balance of which may determine whether a cancer regresses, progresses, or potentially metastasizes. These effects are evident in CRC consensus molecular subtypes (CMS) where both CMS1 and CMS4 contain immune infiltrates yet have opposing prognoses. The microbiome has previously been associated with CRC and immune response in CRC but has largely been ignored in the CRC subtype discussion. We used CMS subtyping on surgical resections from patients and aimed to determine the contributions of the microbiome to the pleiotropic effects evident in immune-infiltrated subtypes. We integrated host gene-expression and meta-transcriptomic data to determine the link between immune characteristics and microbiome contributions in these subtypes and identified lipopolysaccharide (LPS) binding as a potential functional mechanism. We identified candidate bacteria with LPS properties that could affect immune response, and tested the effects of their LPS on cytokine production of peripheral blood mononuclear cells (PBMCs). We focused on Fusobacterium periodonticum and Bacteroides fragilis in CMS1, and Porphyromonas asaccharolytica in CMS4. Treatment of PBMCs with LPS isolated from these bacteria showed that F. periodonticum stimulates cytokine production in PBMCs while both B. fragilis and P. asaccharolytica had an inhibitory effect. Furthermore, LPS from the latter two species can inhibit the immunogenic properties of F. periodonticum LPS when co-incubated with PBMCs. We propose that different microbes in the CRC tumor microenvironment can alter the local immune activity, with important implications for prognosis and treatment response.
Subject terms: Clinical microbiology, Next-generation sequencing
Introduction
Colorectal cancer (CRC) tumors consist of a complex microenvironment whose characteristics affect the tumor’s progression, prognostics, and therapy response1,2. The immune-cell infiltrate within the microenvironment plays a key role in CRC as it can either enhance or inhibit tumor development. The induction of a tumor-directed immune response can result in the influx of effector cells and subsequent tumor cell death. However, in other contexts, the tumor itself may subvert the immune response and rather than eliminating the tumor, immune infiltrates may contribute to chronic inflammation and provide signals for cell growth and vascular changes2,3. Different cytokines and T-cell subsets have been shown to be capable of both promoting or inhibiting cancer progression, and this likely reflects differences in the immunoregulatory signals provided by different tumor microenvironments.
Due to CRC heterogeneity, several different subtyping classifications have been proposed4–9. Two subgroups are commonly identified among these different schemes, one characterized by microsatellite instability (MSI) and immune activation, and the other defined by angiogenic and mesenchymal characteristics7. The Colorectal Cancer Subtyping Consortium combined data from several large subtyping studies to generate a classification system of four consensus molecular subtypes (CMS), based on gene expression sequencing data5. Subsequent studies of the immune phenotypes associated with each of these molecular subtypes revealed substantive differences in the composition of the immune infiltrates, with the good prognosis CMS1 (MSI-Immune) being immunogenic and the poor prognosis CMS4 (mesenchymal) being inflamed and characterized by immunosuppression10–12.
Understanding immune responses in CRC is not complete without consideration of the microbiome, as evidenced by lower tumor susceptibility in germ-free rats compared to conventional rats upon carcinogen introduction13,14; differences in tumor susceptibility between mice with different microbiome communities15; and differences in microbiomes of cancers with deficient or proficient mismatch repair functions16. Bacteria such as Fusobacterium nucleatum, Porphyromonas asaccharolytica, and Parvimonas micra have been identified as potential biomarkers in studies of CRC17,18. Taxa associated with the oral cavity have also been found to be enriched in CRC18–21, possibly driving the increase seen in species richness18. Of the microbial functional pathways that have been associated with CRC, many involve immune responses. F. nucleatum subspecies animalis can induce CCL20, a chemokine that plays a role in recruitment of Th17, regulatory T-cells, and dendritic cells22, while Enterotoxigenic B. fragilis (ETBF) toxin is associated with murine colon tumor formation, through activation of signal transducer and activator of transcription-3 (STAT3) with Th17 responses, also involving IL-17 and IL-2323.
The CMS1 and CMS4 subtypes differ with respect to both their immune composition and prognoses. Although the microbiome is known to be a strong modulator of immune responses, its potential role in driving the differing immune compositions of CMS1 and CMS4 subtypes is yet unexplored. In this study we analyzed the microbiome composition in each subtype and detected differences in microbiome signatures associated with different patterns of immune activation in CMS1 and CMS4. We therefore aimed to determine how microbes from different subtypes of CRC tumors could potentially affect the immune environments characteristic of these respective tumors.
Results
Colorectal Cancer Cohort Characteristics
The cohort comprised 308 colorectal cancers, all taken prior to chemotherapy. Subtyping of the 308 samples classified 260 samples, with 60 samples in CMS1, 145 in CMS2, 38 in CMS3, and 17 in CMS4. For subsequent analysis, we focused on the 260 classified samples.
The mean age of the 260 patients was 71.78 years. There were 139 females and 121 males. The majority of the tumors were from the colon (81.15%) while the rest were from the rectum (18.85%). Of the colon tumors, 113 were right-sided (proximal tumors) while 98 were left-sided. Together, the left-sided and rectal tumors are categorized as distal tumors (147 in total). Table 1 summarizes these characteristics, and gives more details of demographics per CMS group.
Table 1.
Cohort Characteristics by Consensus Molecular Subtype (CMS).
| All (n = 260) | CMS1 (n = 60) | CMS2 (n = 145) | CMS3 (n = 38) | CMS4 (n = 17) | |
|---|---|---|---|---|---|
| Age (years), mean ± SD | 71.78 ± 11.39 | 76.2 ± 10.00 | 70.11 ± 11.18 | 71.03 ± 12.99 | 72.06 ± 10.71 |
| Sex | |||||
| Male | 121 (46.54%) | 16 (27.67%) | 83 (57.24%) | 14 (36.84%) | 8 (47.06%) |
| Female | 139 (53.46%) | 44 (73.33%) | 62 (42.76%) | 24 (63.16%) | 9 (52.94%) |
| Site | |||||
| Colon | 211 (81.15%) | 59 (98.33%) | 110 (75.86%) | 32 (84.21%) | 11 (64.71%) |
| Rectum | 49 (18.85%) | 1 (1.67%) | 35 (24.14%) | 6 (15.79%) | 6 (35.29%) |
| Side | |||||
| Proximal | 113 (43.46%) | 48 (80.00%) | 42 (28.97%) | 19 (50.00%) | 4 (23.53%) |
| Distala | 147 (56.54%) | 12 (20.00%) | 103 (71.03%) | 19 (50.00%) | 13 (76.47%) |
| Stage | |||||
| 1 | 48 (18.46%) | 10 (16.67%) | 25 (17.24%) | 11 (28.95%) | 2 (11.76%) |
| 2 | 112 (43.08%) | 33 (55.00%) | 65 (44.83) | 10 (26.32%) | 4 (23.53%) |
| 3 | 83 (31.92%) | 16 (26.67%) | 43 (29.66%) | 16 (42.10%) | 8 (47.06%) |
| 4 | 17 (6.54%) | 1 (1.67%) | 12 (8.28%) | 1 (2.63%) | 3 (17.65%) |
n number of patients.
aDistal = contains both left-sided and rectal cancers.
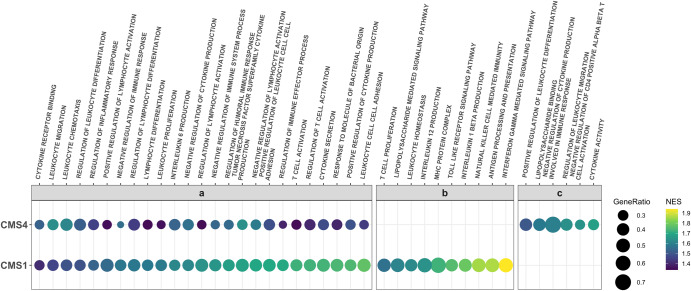
CMS1 and CMS4 have enriched gene sets involved in immune response
In order to compare which gene sets were enriched in different subtypes of CRC, we first used DESeq2 to compare gene expression in CMS1 samples with the average of the CMS2, CMS3 and CMS4 samples. There were 4736 genes that were significantly over expressed (adjusted p-value < 0.05) in CMS1 compared to the other subtypes. We carried out gene-set enrichment analysis (GSEA) on the list of genes as described in the methods section, and obtained those with positive normalized enrichment scores (NES) as gene sets enriched in CMS1. We obtained a total of 318 gene sets that had positive NES in CMS1, with adjusted p-value < 0.05. Several of the most enriched gene sets were related to immune responses (cytokines, antigen processing and presentation, and cell killing processes) as well as nuclear organization and replication processes. We therefore subset the enriched gene sets in CMS1 using immune-related keywords (see “Methods”). As it has been theorized that microbes might affect the balance of immune responses in the tumor microenvironment (TME), we sought to identify if response to microbes is captured among the enriched gene sets of our subtypes by including “BACTERIA” in the keywords.
We performed the same analyses for CMS2, CMS3, and CMS4, against the average of the other three subsets. We obtained no enriched gene sets using the immune-related keywords above in CMS2 and CMS3, consistent with previous studies describing these as “immune-neglected”24. There were 2481 upregulated genes in CMS4 compared to the other subtypes. The top enriched gene sets for CMS4 primarily comprised terms corroborating its epithelial-mesenchymal-transition (EMT) and angiogenic characteristics. As studies have suggested a role for immune cells in immunosuppression in CMS410–12, we examined the 1142 enriched gene sets in CMS4, and found 59 enriched gene sets that contained immune-related keywords.
We found an overlap of enriched immune-related gene sets between CMS1 and CMS4 (Fig. 1a). These included production of Interleukin 6, cytokine secretion, and T-cell activation, all of which could lead to immune-induced cytotoxic activity that could destroy cancer cells, or chronic inflammation and escape in favor of cancer progression3,25–27. Some gene sets had prominently higher enrichment scores in CMS1 compared to CMS4; among these was the gene set for T-cell activation. T-cell infiltration in CRC has been associated with better survival28,29. We also found Response to Molecule of Bacterial Origin among these enriched gene sets, indicating the role microbes likely play in the characteristics of these subtypes.
Fig. 1. Immune-related enriched gene sets in CMS1 and CMS4.
a Immune related enriched gene sets common to CMS1 and CMS4. b Representative enriched immune-related gene sets unique to CMS1. c Representative enriched immune-related gene sets unique to CMS4. NES normalized enrichment score. Gene Ratio genes contributing to enrichment of the gene set from our dataset divided by total set size of the gene set in question. All gene sets have adjusted p-values < 0.05, as calculated through GSEA analysis.
We found 79 immune-related gene sets unique to CMS1. Several of these (e.g. antigen processing and presentation, MHC protein complex) indicate increased levels of antigen presentation, an early critical process in the induction of antitumor responses30. Gene sets indicating activity of natural killer cells and production and response to interleukins, including Interleukin-12 and Interleukin-1 beta, were also unique to CMS1 (Fig. 1b), in addition to a wide array of functions indicating regulation and homeostasis of immune responses, including regulation of apoptosis of leukocytes, lymphocytes, and T-cells. Genes associated with Toll-like receptor activity and lipopolysaccharide signaling pathways were also identified in CMS1, again suggesting that bacteria and their LPS may play a role in the responses observed.
CMS4 had 34 unique immune-related enriched gene sets, several of which are associated with negative regulation of T-cells and other immune responses (Fig. 1c). Lipopolysaccharide binding was also enriched in CMS4, suggesting a link to bacterial regulation, as seen in CMS1.
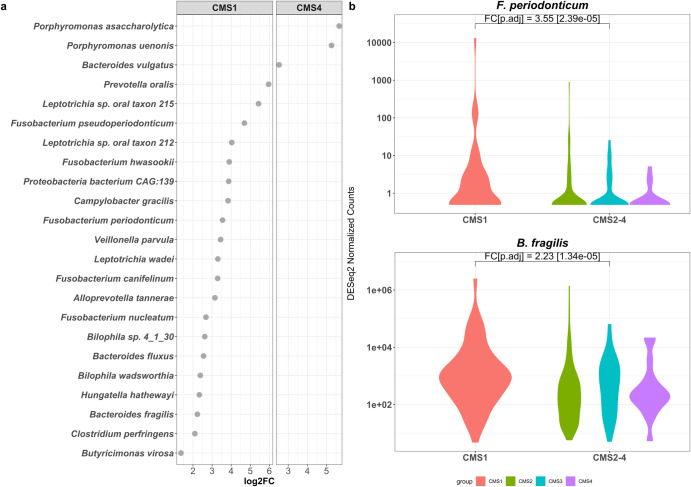
Differentially abundant bacteria that contribute to LPS biosynthetic processes in CMS1 include Fusobacteria and Bacteroides fragilis species
From sequencing reads that did not map to the human genome, we obtained matches to microbial species. We found 296 microbial species that were differentially more abundant (DA) in CMS1 compared to the other CMS subtypes (adjusted p-value < 0.05, as calculated in DESeq2). As our host GSEA had identified a ‘response to microbes’ among the enriched gene sets in CMS1 and CMS4, and that these may be related to LPS processes, we selected for bacteria that had proteins annotated with “Lipid A Biosynthetic Process” or “Lipopolysaccharide Biosynthetic Process” Gene Ontology terms, which identified 20 bacterial species in CMS1 (Fig. 2a, left). Notably, we identified Fusobacterium and Bacteroides as among the abundant bacteria with LPS processes. These two genera have previously been implicated in the progression of CRC17,22,23,31. We focused on F. periodonticum and B. fragilis to further investigate the potential interaction between their LPS molecules and immune responses in host cells (Fig. 2b).
Fig. 2. Abundant Microbes in CMS1 and CMS4 with lipopolysaccharide processes.
a Differentially abundant Bacteria in CMS1 and CMS4 with LPS processes annotations, showing their fold changes in CMS1 (left) or CMS4 (right) against the average abundance of the other three subtypes. b F. periodonticum and B. fragilis normalized counts in CMS1 compared to the other subtypes. log2FC log2Fold Change, FC log2Fold Change, p.adj adjusted p-value as calculated in DESeq2.
In contrast, only 127 microbes were found to be differentially more abundant in CMS4 compared to the other three subtypes, and only three bacterial species had proteins annotated with LPS or Lipid-A biosynthetic processes (Fig. 2a, right). Of these, we chose Porphyromonas asaccharolytica to investigate further for its effects on immune response in in vitro experiments, as P. asaccharolytica has been identified as a CRC marker in multi-cohort analyses17,18.
LPS from different bacterial species have different effects on cytokine release
Stock cultures of peripheral blood mononuclear cells (PBMCs) were incubated with increasing concentrations of LPS, extracted from F. periodonticum (strains 1/1/54 (D10), 2/1/31, and 1/1/41 FAA), B. fragilis (strains 3/2/5, 2/1/16, and 2/1/56 FAA), or P. asaccharolytica (strains CC44 001F, and CC1/6 F2) overnight. The concentrations of cytokines present in the supernatants were then analyzed by flow cytometry and compared to untreated PBMCs. We focused on IFN-γ, IL-6, IL-10, IL-12p70, IL-1β, and IL-18, as these were prominent cytokines identified in our gene-set enrichment analysis; IL-18 has been found to synergize with IL-12 to increase production of IFN-γ in T-cells32 and IL-10 is known as a regulatory cytokine26,27,33. All strains of a given species had similar effects on cytokine production.
The highest concentration of LPS tested from B. fragilis or P. asaccharolytica (600 ng/mL) was found to inhibit the release of the measured cytokines, compared to untreated PBMCs. Lower concentrations of LPS from these species also caused a decrease in cytokine production, but to a lesser degree (Supplementary Fig. 1a, b). Conversely, LPS from F. periodonticum strains showed stimulatory effects on the cytokines of interest, with low concentrations of LPS (6 ng/mL) causing an increase in their secretion compared to baseline PBMC levels (Supplementary Fig. 1c). No further increases were observed at higher LPS levels.
As all strains exhibited the same properties (Supplementary Fig. 1), we chose a single strain from each species, F. periodonticum 2/1/31, B. fragilis 2/1/16, and P. asaccharolytica CC1/6 F2, to use in subsequent experiments.
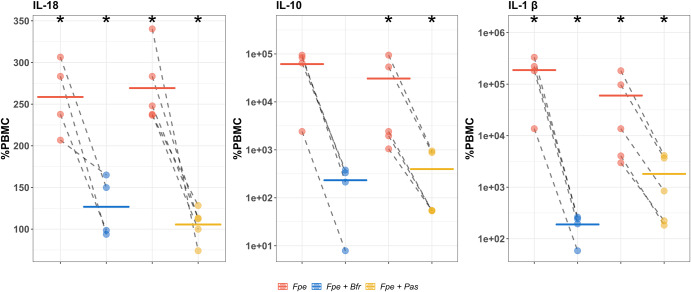
B. fragilis and P. asaccharolytica LPS exhibit immunoinhibitory properties when co-cultured with stimulatory LPS from F. periodonticum
To further investigate the immune modulatory effects of different LPS, we tested whether LPS from B. fragilis 2/1/16 or P. asaccharolytica CC1/6 F2 could retain their immunoinhibitory effects on PBMCs when co-cultured with LPS from immunostimulatory F. periodonticum 2/1/31.
PBMCs were incubated with either F. periodonticum LPS alone, or in combination with either B. fragilis or P. asaccharolytica LPS, and cytokine production was measured. Figure 3 and Supplementary Fig. 2 show that the increased cytokine production observed in the presence of F. periodonticum LPS alone was attenuated by co-incubation with LPS from B. fragilis or P. asaccharolytica. In Fig. 3, we show that B. fragilis or P. asaccharolytica LPS, when co-cultured with LPS from F. periodonticum, reduced cytokine secretion towards baseline levels in IL-18, IL-10, and IL-1β. These cytokines are considered protective against CRC, a regulatory cytokine, and detrimental in CRC, respectively. This reduction was significant for IL-1β, and IL-18 when B. fragilis LPS was co-incubated with F. periodonticum LPS (Fig. 3, 1st and 3rd panels), and significant for all three cytokines when P. asaccharolytica LPS was co-incubated with F. periodonticum LPS (Fig. 3). All significant comparisons had absolute effect sizes (Cohen’s d) greater than 0.8, indicating large effects (Supplementary Tables 2, 3).
Fig. 3. Changes in cytokine expression in peripheral blood mononuclear cells (PBMCs) following treatment with F. periodonticum alone (red), or in combination with B. fragilis (blue) or P. asaccharolytica (yellow) for cytokines IL-18, IL-10, and IL-1β.
For these experiments we used the lowest concentration of F. periodonticum LPS (6 ng/mL) and the highest concentration of LPS from B. fragilis or P. asaccharolytica (600 ng/mL), as these respective concentrations had the largest effects on cytokine production in earlier experiments. Values are shown as percentages of PBMC baseline secretion, which is set at 100%. Dashed lines indicate a single experimental run. Colored, solid horizontal lines represent the means of repeat experiments. Y-axes of IL-10 and IL-1β are in log10 scale, while Y-axis of IL-18 is in the linear scale. Fpe = F. periodonticum (6 ng/mL), Fpe + Bfr = F. periodonticum (6 ng/mL) + B. fragilis (600 ng/mL), Fpe + Pas = F. periodonticum (6 ng/mL) + P. asaccharolytica (600 ng/mL); * = Paired Student’s t tests p-value < 0.05 (F. periodonticum vs PBMC, F. periodonticum + B. fragilis vs F. periodonticum alone, or F. periodonticum + P. asaccharolytica vs F. periodonticum alone).
Discussion
We combined gene-expression data from both tumor and associated microbiota to better understand how the microbiome could influence the differences seen in immune responses in CRC, in a way that could be tested in vitro. Several previous studies attributing function to the microbiome have largely been associative17,18,34, and while important analytical results regarding functional contributions of the microbiome had been made, these have seldom been linked to host gene expression and functional contributions. Here, we show a potential link between enriched microbial species and immune responses seen in CRC, through the action of bacterial lipopolysaccharide.
Studies of immune responses in CRC have reported conflicting findings, where they can either induce tumor regression or lead to cancer progression. This delicate balance between pro- and anti-tumor effects is reflected in the consensus molecular subtypes (CMS) of CRC5, with good prognosis CMS1 and poor prognosis CMS4 having immune infiltrates of differing compositions10–12. Our analysis of host gene sets confirms previously published reports that CMS1 and CMS4 are immune infiltrated and inflamed, respectively, while CMS2 and CMS3 have little immune activation24. Enriched gene sets unique to CMS1 involve antigen presentation and processing, natural killer cell activity, and homeostasis of immune responses, and regulation of T-cell apoptosis. These processes, as well as their regulation may affect how CMS1 tumors progress. Enriched gene sets in CMS4 meanwhile indicate an association with immunosuppression, consistent with previous studies2,10.
Among the enriched immune gene sets common to CMS1 and CMS4, we identified those related to response to microbes and lipopolysaccharide, indicating a potential role for the microbiome in the characteristics of these subtypes. Focusing on bacteria in the tumor microenvironment with proteins annotated with LPS biosynthetic processes identified F. periodonticum and B. fragilis as differentially abundant in CMS1, and P. asaccharolytica as differentially abundant in CMS4. B. fragilis was among the most enriched bacterial species in a multi-cohort analysis of CRC17, while toxigenic strains of the bacteria are associated with immune activation, reactive oxygen species (ROS) production and DNA damage, as well as E-cadherin cleavage leading to cell proliferation23,31. Fusobacteria species have been shown to associate with CRC in a multitude of studies35 and F. periodonticum was reported to be enriched in mismatch repair (MMR) deficient (dMMR) tumors compared to MMR proficient (pMMR) tumors16. P. asaccharolytica, meanwhile, has been identified as a CRC biomarker in previous studies (Dai et al 2018, Thomas et al 2019).
As CMS1 and CMS4 are thought to represent tumor-immune inhibitory and stimulatory environments, respectively, we hypothesized that F. periodonticum and B. fragilis would stimulate anti-tumor cytokines (IFN-γ, IL-12 IL-18), and decrease tumor-promoting cytokines (IL-1β and IL-6)26,27, while the opposite effect may be seen with P. asaccharolytica. However, our results using human PBMCs indicate that F. periodonticum LPS stimulated the production of all cytokines of interest, including IL-10, while both P. asaccharolytica and B. fragilis inhibited the production of all of these cytokines. In addition, LPS from both P. asaccharolytica and B. fragilis could attenuate the immunogenicity of LPS from F. periodonticum, indicating that interactions between these microbes may add to the complexity of immune responses.
Although general attributes such as pro- or anti-tumor have been ascribed to many cytokines in the context of cancer, many cytokines display pleiotropic functions that may have opposing effects in CRC. For instance, decreased levels of IL-1β, along with IL-18, are correlated with increased colitis-associated cancer (CAC) in an inflammasome context36,37 despite IL-18 being commonly viewed as anti-tumorigenic26,27. IL-6 has anti-tumorigenic properties in the form of priming effector T-cells25; and unchecked IFN-γ could compromise the colonic epithelial barrier26,38 allowing an influx of microbiota that could influence cancer progression despite IL-6 being described as pro-tumorigenic, and IFN-γ being protective in CRC26,27.
Our findings imply that balance and control in cytokine production is critical to determining whether the immune microenvironment is pro- or anti-tumorigenic. The balance, we hypothesize, may be reflected in the interactions we see in response to the bacterial LPS we have tested.
Although our results with B. fragilis LPS were unexpected, as high abundance of B. fragilis was associated with the immunogenic CMS1 tumors, previous studies have shown that LPS activity, conserved among the Bacteroidales order, can be immunosuppressive and promote immune tolerance to the high microbial load found in the gut, which hosts a complex microbial ecosystem39. Indeed, species of the Bacteroides genus, including B. fragilis, have been found to have immunoregulatory properties40–42.
However, it was identified that enterotoxigenic B. fragilis could promote colonic tumors and induce inflammatory processes but not its non-toxigenic counterpart23, indicating that it may be the toxin that is necessary for its inflammatory role and not LPS. We were unable to identify whether the B. fragilis in our CRC samples were toxigenic or non-toxigenic, or whether toxigenic strains were expressing the BFT (B. fragilis toxin); the BFT may also only be produced within a certain timeframe during carcinogenesis43. There is also a possibility of a mixture of non-toxigenic and toxigenic B. fragilis in our tumor samples, and this combination may indicate a nuanced balance between LPS and B. fragilis toxin, along with the more immunogenic LPS of other microbes such as F. periodonticum.
Our findings lead us to hypothesize that while LPS from B. fragilis may be immunosuppressive, interaction with immunogenic molecules produced by the same or other microbes adds a layer of complexity to the balance of immune responses in colorectal cancer. In CMS1, we postulate that this balance skews towards immune activation, contributing to anti-tumor effects and positively affecting prognosis, while the immunosuppressive LPS of P. asaccharolytica may contribute to immune evasion and escape of tumors in CMS4. Further work is recommended to confirm this, with characterization of LPS structures, and determining their signaling pathways and what these affect, among the necessary studies to demonstrate how LPS from different species contribute to CRC characteristics. Further work on the characteristics of immune cell populations affected by LPS is also warranted, as well as their effects on CRC cell lines.
The cytokine release-inhibiting capabilities of LPS from B. fragilis and P. asaccharolytica are notable as previous studies emphasize the pro-inflammatory activities of CRC-associated microbiota13,23,44–46. While we acknowledge that these events also occur within our tumor samples, we also suggest that microorganisms play a role in immunosuppression, either by aiding the tumor progression through immune evasion and escape, or contributing to homeostasis of immunogenic processes.
The limitations of the study include the use of PBMCs as a proxy for immune cells in the tumor microenvironment. PBMCs may not adequately reflect the effects of LPS on tumor-infiltrating lymphocytes. In vitro cultures of single cell types do not allow for crosstalk between different cell populations, which would be expected in the complex tumor microenvironment. Furthermore, we acknowledge that while we have tested the effects of LPS from single species and pairs of species, colorectal tumors may harbor up to hundreds of different species, and each may elicit an effect dependent on LPS structure and absolute bacterial counts, which could contribute to the nuanced immune-modulation within the TME. In addition, the effects of LPS may be countered or exacerbated by other known bacterial mechanisms, e.g. bacterial toxins, or as yet undiscovered interactions. These warrant future studies involving a more representative model of the tumor microenvironment.
In this study, we identified gene sets involved in immune response to microbial triggers in both CMS1 and CMS4 colorectal cancer subtypes and identified LPS from particular bacterial species that associate with immune responses. In vitro analyses showed that F. periodonticum LPS, found in CMS1 tumors, increased production of cytokines IL-1β, IFN-γ, IL-18, IL-10, IL-6, and IL-12p70, while LPS from B. fragilis, found in CMS1 tumors, and P. asaccharolytica LPS, found mainly in CMS4 tumors, decreased production of these cytokines and could also attenuate the immunogenic effect of F. periodonticum LPS. Where most previous studies focus on the inflammation-inducing capabilities of CRC-associated microorganisms, our results indicate that their immunosuppressive potential should not be overlooked and adds another layer of complexity to immune responses in CRC.
Methods
Sample collection and handling
A total of 308 distinct samples were collected during surgical resection of colorectal tumors from patients who had not received chemotherapy prior to surgery. Patients with diagnosed Hereditary Non-Polyposis Colorectal Cancer (HNPCC) or Familial Adenomatous Polyposis (FAP) were excluded. All participants provided written, and informed consent and the study was approved by the University of Otago Human Ethics Committee with approval number H16/037. During surgery, samples were taken, frozen in liquid nitrogen, and stored at −80 °C. Before RNA extraction, samples were first equilibrated for at least 48 h at −20 °C in RNAlater ICETM (Qiagen).
RNEasy Plus Mini Kit (Qiagen) was used to extract RNA from 15-20 mg of tissue, disrupted using a Retsch Mixer Mill, including a DNAse treatment step in the procedure. Purified RNA was quantified using a NanoDrop 2000c spectrophotometer (Thermo Scientific, Asheville, NC, USA) and subsequently stored in −80 °C.
RNA Sequencing
Library preparation for RNA sequencing was carried out using the Illumina TruSeq Stranded Total RNA Library preparation kit (Illumina), with ribosomal RNA depletion using Ribo-Zero Gold. The Illumina Hi-Seq 2500 V4 platform was used for RNA sequencing, producing 125 bp paired-end reads. Each sample library was split into lanes to avoid technical bias and were later merged during the data processing phase. Merged raw data can be found under Bioproject ID PRJNA788974 in the NCBI SRA database.
Consensus molecular subtype classification
Fastq-mcf from ea-utils47,48 and SolexaQA++49 were used for quality control and trimming of reads before merging of sequences from different lanes. Salmon50 was then used to quantify transcript expression. The publicly available CRC CMS classifier5 was used to categorize samples into one of four CMSs.
Bioinformatics analysis
After trimming, the 260 samples were run through the MetaFunc pipeline51 using default settings, except for setting reverse stranded option for featureCounts52, a species needing at least 0.01% abundance in at least one of the 260 samples to be included in the microbiome analysis, and setting TaxChoices in the configuration file to include Bacteria, Archaea, Fungi, and Viruses. Databases used were those provided in https://metafunc.readthedocs.io/en/latest/usage.html#databases.
Differential expression and gene set enrichment analysis in host
From the results of the MetaFunc analysis, we gathered the host-gene expression raw counts table into a matrix for input into DESeq253 with metadata information on their respective CMS. Using the 260 samples that had been classified into a subtype, DESeq2 was used to obtain differentially expressed genes (DEGs) in one CMS compared to the average of the other three subtypes. Genes were considered differentially expressed if their Benjamini–Hochberg (BH) adjusted p-values were < 0.05. Raw p-values and log-fold change generated through DESeq2 were then used for ranking and sign information, respectively, in gene set enrichment analysis (GSEA) using the clusterProfiler package54 with the C5 Ontology Gene Sets collection (version 7) from the molecular signatures database (MSigDB)55,56. We considered a gene set enriched in a subtype if it had adjusted p-values of <0.05 and positive Normalized Enrichment Score (NES). We interrogated the enriched gene sets in the CMS subtypes using immune-related keywords as follows: “IMMUN”, “T CELL”, “INTERFERON”, “CYTOKINE”, “TOLL LIKE”, “LYMPHOCYTE”, “LEUKOCYTE”, “PATTERN RECOGNITION”, “LIPOPOLYSACCHARIDE”, “MHC”, “INFLAMMATORY”, “ANTIGEN”, “INTERLEUKIN”, and “BACTERIA”.
Differential abundance of microbes in the microbiomes of CRC subtypes
From the results of the MetaFunc analysis, raw counts of microbial taxonomies were gathered into a Phyloseq object57, with metadata information on their respective CMS. DESeq2 was used to identify differentially abundant microbes in either CMS1 or CMS4 compared to the average of the other three subtypes. Microbes were considered differentially abundant in a CMS if they had a log2 fold change > 0 and adjusted p-value < 0.05.
Lipopolysaccharide-associated bacteria
MetaFunc produces a table that indicates which bacterial taxonomy IDs have proteins that are annotated with gene ontology terms. All bacterial species with proteins annotated with “lipopolysaccharide biosynthetic process” or “lipid A biosynthetic process” were obtained for CMS1 and CMS4 samples, and then cross-referenced with differentially abundant microbes in CMS1 or CMS4, respectively, to obtain a list of differentially abundant bacteria that have proteins annotated with LPS-related processes.
Detailed analysis may be found at https://gitlab.com/alsulit08/2021_uoc_massey_lps-crc/-/tree/master/Bioinformatics. Information on read counts per stage of the analysis is detailed in Supplementary Table 1.
Lipopolysaccharide from bacterial strains
LPS was extracted from strains of Fusobacterium periodonticum (1/1/54 (D10), 2/1/31, and 1/1/41 FAA), Bacteroides fragilis (3/2/5, 2/1/16, and 2/1/56 FAA), and Porphyromonas asaccharolytica (CC44 001F, and CC1/6 F2) using Bacterial Lipopolysaccharides (LPS) Extraction Kit (Alpha Diagnostic International, Catalog # 1000-100-LPS) as per the manufacturer’s instructions, resulting in a final yield of 30 μg/mL of LPS.
PBMC Treatment with LPS from Bacterial Species
PBMCs (2 × 105 cells) were incubated with LPS preparations (at least 16 h) of varying concentrations (600 ng/mL, 60 ng/mL or 6 ng/mL) from B. fragilis (3/2/5, 2/1/16, and 2/1/56 FAA), F. periodonticum (1/1/54 (D10), 2/1/31, and 1/1/41 FAA) or P. asaccharolytica (CC44 001F, and CC1/6 F2). For co-incubation tests, we used B. fragilis strain 2/1/16, F. periodonticum strain 2/1/31, and P. asaccharolytica strain CC1/6 F2. We treated the PBMCs with 6 ng/mL of F. periodonticum (strain 2/1/31) LPS and 600 ng/mL of B. fragilis (strain 2/1/16) or P. asaccharolytica (strain CC1/6 F2) LPS. As no-treatment controls, PBMC medium (RPMI, 10%FCS, 1% glutamine, 0.2% Penicillin/Streptomycin) or RPMI alone was added to the initial culture of PBMCs. Co-incubation experiments were conducted at least three times. For each repeated experiment, PBMCs were obtained from a different individual (ethics approval number: URA/06/12/083/AM06).
Measurement of cytokine production and statistical analysis
Secreted cytokine expression was measured using LegendPlex Human Inflammation Panel 1 (Cat no. 740809) on a Beckman Coulter Cytomics FC500 Flow Cytometry Analyzer, following the manufacturer’s instructions. For all runs, baseline values of the cytokines from untreated PBMCs were obtained. Legendplex Software (Windows version 8 or MacOS version 7.1, using the 5-parameter curve fitting model) was used to assess the final concentrations of the cytokines of interest. Paired Student’s t tests were used to test for differences in cytokine production between baseline PBMC and F. periodonticum treatment, and F. periodonticum treatment and F. periodonticum with either P. asaccharolytica or B. fragilis treatment. Effect sizes were obtained using Cohen’s d, with Hedges correction, to account for small sample sizes.
Detailed analyses may be accessed at https://gitlab.com/alsulit08/2021_uoc_massey_lps-crc/-/tree/master/LPS_Experiments.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
The authors would like to thank Helen Morrin at the Cancer Society Tissue Bank, Christchurch, and the patients involved and their whānau for generously participating in this study. The authors would also like to thank the Maurice and Phyllis Paykel Trust, the Gut Cancer Foundation (NZ) with support from the Hugh Green Foundation, the Colorectal Surgical Society of Australia and New Zealand (CSSANZ), and the Health Research Council of New Zealand for funding towards this study. The funding bodies had no role in the design of the study or collection, analysis, and interpretation of data or in writing the manuscript
Author contributions
A.K.S. carried out bioinformatics and laboratory-based analyses, and was a major contributor to manuscript writing. M.D. carried out laboratory-based analysis. E.A.-V. provided guidance on study design and methods. O.K.S. provided guidance about bioinformatics and data analyses. B.H. provided guidance on laboratory analyses and data analyses. J.M. provided guidance on laboratory analyses and data analyses. S.S. carried out bioinformatics analysis. J.P. was involved in study design, bioinformatics and data analysis, and manuscript preparation. F.A.F. was involved in study design and clinical aspects of the study. R.P. was involved in study design and manuscript preparation. All authors read and approved the final manuscript.
Data availability
Sequencing data can be found under Bioproject ID PRJNA788974 in the NCBI SRA database. Limited patient metadata may be provided upon reasonable request to authors.
Code availability
Details for bioinformatics and statistical analyses may be found at https://gitlab.com/alsulit08/2021_uoc_massey_lps-crc.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41522-023-00429-w.
References
- 1.Angell HK, Bruni D, Barrett JC, Herbst R, Galon J. The immunoscore: colon cancer and beyond. Clin. Cancer Res. 2020;26:332–339. doi: 10.1158/1078-0432.CCR-18-1851. [DOI] [PubMed] [Google Scholar]
- 2.Colangelo T, et al. Friend or foe? The tumour microenvironment dilemma in colorectal cancer. Biochim. Biophys. Acta (BBA)—Rev. Cancer. 2017;1867:1–18. doi: 10.1016/j.bbcan.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Markman JL, Shiao SL. Impact of the immune system and immunotherapy in colorectal cancer. J. Gastrointest. Oncol. 2015;6:208–223. doi: 10.3978/j.issn.2078-6891.2014.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Sousa E, et al. Poor-prognosis colon cancer is defined by a molecularly distinct subtype and develops from serrated precursor lesions. Nat. Med. 2013;19:614–618. doi: 10.1038/nm.3174. [DOI] [PubMed] [Google Scholar]
- 5.Guinney J, et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 2015;21:1350–1356. doi: 10.1038/nm.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marisa L, et al. Gene expression classification of colon cancer into molecular subtypes: characterization, validation, and prognostic value. PLoS Med. 2013;10:e1001453. doi: 10.1371/journal.pmed.1001453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Salas N, et al. Clinical relevance of colorectal cancer molecular subtypes. Crit. Rev. Oncol./Hematol. 2017;109:9–19. doi: 10.1016/j.critrevonc.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Roepman P, et al. Colorectal cancer intrinsic subtypes predict chemotherapy benefit, deficient mismatch repair and epithelial-to-mesenchymal transition. Int. J. Cancer. 2014;134:552–562. doi: 10.1002/ijc.28387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadanandam A, et al. A colorectal cancer classification system that associates cellular phenotype and responses to therapy. Nat. Med. 2013;19:619–625. doi: 10.1038/nm.3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becht E, et al. Immune and stromal classification of colorectal cancer is associated with molecular subtypes and relevant for precision immunotherapy. Clin. Cancer Res. 2016;22:4057–4066. doi: 10.1158/1078-0432.CCR-15-2879. [DOI] [PubMed] [Google Scholar]
- 11.Dienstmann R, et al. Consensus molecular subtypes and the evolution of precision medicine in colorectal cancer. Nat. Rev. Cancer. 2017;17:79–92. doi: 10.1038/nrc.2016.126. [DOI] [PubMed] [Google Scholar]
- 12.Karpinski P, Rossowska J, Sasiadek MM. Immunological landscape of consensus clusters in colorectal cancer. Oncotarget. 2017;8:105299–105311. doi: 10.18632/oncotarget.22169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janney A, Powrie F, Mann EH. Host–microbiota maladaptation in colorectal cancer. Nature. 2020;585:509–517. doi: 10.1038/s41586-020-2729-3. [DOI] [PubMed] [Google Scholar]
- 14.Reddy BS, Weisburger JH, Narisawa T, Wynder EL. Colon carcinogenesis in germ-free rats with 1,2-dimethylhydrazine and n-methyl-n′-nitro-n-nitrosoguanidine. Cancer Res. 1974;34:2368–2372. [PubMed] [Google Scholar]
- 15.Yu AI, et al. Gut microbiota modulate CD8 T cell responses to influence colitis-associated tumorigenesis. Cell Rep. 2020;31:107471. doi: 10.1016/j.celrep.2020.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hale VL, et al. Distinct microbes, metabolites, and ecologies define the microbiome in deficient and proficient mismatch repair colorectal cancers. Genome Med. 2018;10:78. doi: 10.1186/s13073-018-0586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dai Z, et al. Multi-cohort analysis of colorectal cancer metagenome identified altered bacteria across populations and universal bacterial markers. Microbiome. 2018;6:70. doi: 10.1186/s40168-018-0451-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas AM, et al. Metagenomic analysis of colorectal cancer datasets identifies cross-cohort microbial diagnostic signatures and a link with choline degradation. Nat. Med. 2019;25:667–678. doi: 10.1038/s41591-019-0405-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loftus M, Hassouneh SA-D, Yooseph S. Bacterial community structure alterations within the colorectal cancer gut microbiome. BMC Microbiol. 2021;21:98. doi: 10.1186/s12866-021-02153-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakatsu G, et al. Gut mucosal microbiome across stages of colorectal carcinogenesis. Nat. Commun. 2015;6:8727. doi: 10.1038/ncomms9727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Purcell RV, Visnovska M, Biggs PJ, Schmeier S, Frizelle FA. Distinct gut microbiome patterns associate with consensus molecular subtypes of colorectal cancer. Sci. Rep. 2017;7:11590. doi: 10.1038/s41598-017-11237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ye X, et al. Fusobacterium Nucleatum subspecies Animalis influences proinflammatory cytokine expression and monocyte activation in human colorectal tumors. Cancer Prev. Res. 2017;10:398–409. doi: 10.1158/1940-6207.CAPR-16-0178. [DOI] [PubMed] [Google Scholar]
- 23.Wu S, et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat. Med. 2009;15:1016–1022. doi: 10.1038/nm.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fidelle M, et al. Resolving the paradox of colon cancer through the integration of genetics, immunology, and the microbiota. Front. Immunol. 2020;11:600886. doi: 10.3389/fimmu.2020.600886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher DT, Appenheimer MM, Evans SS. The two faces of IL-6 in the tumor microenvironment. Semin Immunol. 2014;26:38–47. doi: 10.1016/j.smim.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mager LF, Wasmer M-H, Rau TT, Krebs P. Cytokine-induced modulation of colorectal cancer. Front. Oncol. 2016;6:96. doi: 10.3389/fonc.2016.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.West NR, McCuaig S, Franchini F, Powrie F. Emerging cytokine networks in colorectal cancer. Nat. Rev. Immunol. 2015;15:615–629. doi: 10.1038/nri3896. [DOI] [PubMed] [Google Scholar]
- 28.Galon J, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960–1964. doi: 10.1126/science.1129139. [DOI] [PubMed] [Google Scholar]
- 29.Ganesh K, et al. Immunotherapy in colorectal cancer: rationale, challenges and potential. Nat. Rev. Gastroenterol. Hepatol. 2019;16:361–375. doi: 10.1038/s41575-019-0126-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reeves E, James E. Antigen processing and immune regulation in the response to tumours. Immunology. 2017;150:16–24. doi: 10.1111/imm.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goodwin AC, et al. Polyamine catabolism contributes to enterotoxigenic Bacteroides fragilis-induced colon tumorigenesis. Proc. Natl Acad. Sci. 2011;108:15354–15359. doi: 10.1073/pnas.1010203108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tominaga K, et al. IL-12 synergizes with IL-18 or IL-1β for IFN-γ production from human T cells. Int. Immunol. 2000;12:151–160. doi: 10.1093/intimm/12.2.151. [DOI] [PubMed] [Google Scholar]
- 33.Li J, Huang L, Zhao H, Yan Y, Lu J. The role of interleukins in colorectal cancer. Int J. Biol. Sci. 2020;16:2323–2339. doi: 10.7150/ijbs.46651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wirbel J, et al. Meta-analysis of fecal metagenomes reveals global microbial signatures that are specific for colorectal cancer. Nat. Med. 2019;25:679–689. doi: 10.1038/s41591-019-0406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hussan H, Clinton SK, Roberts K, Bailey MT. Fusobacterium’s link to colorectal neoplasia sequenced: A systematic review and future insights. World J. Gastroenterol. 2017;23:8626–8650. doi: 10.3748/wjg.v23.i48.8626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Allen IC, et al. The NLRP3 inflammasome functions as a negative regulator of tumorigenesis during colitis-associated cancer. J. Exp. Med. 2010;207:1045–1056. doi: 10.1084/jem.20100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baker KJ, Houston A, Brint E. IL-1 family members in cancer; two sides to every story. Front. Immunol. 2019;10:1197. doi: 10.3389/fimmu.2019.01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferrier L, et al. Stress-induced disruption of colonic epithelial barrier: role of interferon-γ and myosin light chain kinase in mice. Gastroenterology. 2003;125:795–804. doi: 10.1016/s0016-5085(03)01057-6. [DOI] [PubMed] [Google Scholar]
- 39.d’Hennezel E, Abubucker S, Murphy LO, Cullen TW. Total lipopolysaccharide from the human gut microbiome silences toll-like receptor signaling. mSystems. 2017;2:e00046–17. doi: 10.1128/mSystems.00046-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Di Lorenzo F, et al. Pairing Bacteroides vulgatus LPS structure with its immunomodulatory effects on human cellular models. ACS Cent. Sci. 2020;6:1602–1616. doi: 10.1021/acscentsci.0c00791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tan H, Zhao J, Zhang H, Zhai Q, Chen W. Novel strains of Bacteroides fragilis and Bacteroides ovatus alleviate the LPS-induced inflammation in mice. Appl. Microbiol. Biotechnol. 2019;103:2353–2365. doi: 10.1007/s00253-019-09617-1. [DOI] [PubMed] [Google Scholar]
- 42.Yoshida N, et al. Bacteroides vulgatus and Bacteroides dorei reduce gut microbial lipopolysaccharide production and inhibit atherosclerosis. Circulation. 2018;138:2486–2498. doi: 10.1161/CIRCULATIONAHA.118.033714. [DOI] [PubMed] [Google Scholar]
- 43.Purcell RV, et al. Colonization with enterotoxigenic Bacteroides fragilis is associated with early-stage colorectal neoplasia. PLoS ONE. 2017;12:e0171602. doi: 10.1371/journal.pone.0171602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen J, Pitmon E, Wang K. Microbiome, inflammation and colorectal cancer. Semin. Immunol. 2017;32:43–53. doi: 10.1016/j.smim.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Cremonesi, E. et al. Gut microbiota modulate T cell trafficking into human colorectal cancer. Gut gutjnl-2016-313498. 10.1136/gutjnl-2016-313498 (2018). [DOI] [PubMed]
- 46.Rubinstein MR, et al. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell Host Microbe. 2013;14:195–206. doi: 10.1016/j.chom.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aronesty E. Comparison of sequencing utility programs. TOBIOIJ. 2013;7:1–8. [Google Scholar]
- 48.Aronesty, E. ea-utils: Command-line tools for processing biological sequencing data. https://github.com/ExpressionAnalysis/ea-utils (2011).
- 49.Cox MP, Peterson DA, Biggs PJ. SolexaQA: At-a-glance quality assessment of Illumina second-generation sequencing data. BMC Bioinform. 2010;11:485. doi: 10.1186/1471-2105-11-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patro R, Duggal G, Love MI, Irizarry RA, Kingsford C. Salmon provides fast and bias-aware quantification of transcript expression. Nat. Methods. 2017;14:417–419. doi: 10.1038/nmeth.4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sulit AK, Kolisnik T, Frizelle FA, Purcell R, Schmeier S. MetaFunc: taxonomic and functional analyses of high throughput sequencing for microbiomes. Gut Microbiome. 2023;4:e4. doi: 10.1017/gmb.2022.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liao Y, Smyth GK, Shi W. featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics. 2014;30:923–930. doi: 10.1093/bioinformatics/btt656. [DOI] [PubMed] [Google Scholar]
- 53.Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. 10.1101/002832 (2014). [DOI] [PMC free article] [PubMed]
- 54.Yu G, Wang L-G, Han Y, He Q-Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16:284–287. doi: 10.1089/omi.2011.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liberzon A, et al. Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27:1739–1740. doi: 10.1093/bioinformatics/btr260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Subramanian A, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McMurdie PJ, Holmes S. phyloseq: An R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE. 2013;8:e61217. doi: 10.1371/journal.pone.0061217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Sequencing data can be found under Bioproject ID PRJNA788974 in the NCBI SRA database. Limited patient metadata may be provided upon reasonable request to authors.
Details for bioinformatics and statistical analyses may be found at https://gitlab.com/alsulit08/2021_uoc_massey_lps-crc.