Abstract
Hemangiomas are benign slow growing vascular tumors of endothelial origin, commonly seen in young. Laryngeal hemangiomas are rare entities with varied clinical presentations depending upon their location and size. We hereby report a rare case of recurrent hemoptysis in a 65-year-old lady with epiglottic hemangioma.
Keywords: Hemangioma, Epiglottis, Head and neck, Case report
Introduction
Hemangiomas are idiopathic common benign tumours, derived from endodermal elements commonly found in children but are rarer in adults. Approximately 60% arises in the head and neck region [1–3]. Paediatric hemangiomas occur in approximately 2.5% of neonates and are most common in children below 2 years of age [1]. They are further divided into congenital and infantile type. While hemangiomas in adults can occur at any age. Laryngeal hemangiomas are rare, particularly in adults [4]. Approximately 50% of the tumors are self-limiting by the age of 5 in children but fail to regress spontaneously in adults [4]. Adult hemangiomas most commonly occur at or above the true cords [5]. The clinical presentation depends upon the site of origin and may include foreign body sensation throat, hoarseness, dysphagia, hemoptysis. We here present a case of Epiglottic growth who presented with recurrent episodes of hemoptysis, the histopathological examination of which proved it to be a benign vasoformative tumor.
Report of Case
A 65-year-old female presented with recurrent episodes of hemoptysis and progressive dysphagia, more for solids of 06 months duration with no hoarseness/ dyspnoea. Her videolaryngoscopic examination showed a large sessile fleshy mass with bluish grey cystic area within and hemorrhagic changes arising from the laryngeal aspect of epiglottis (Fig. 1). The non contrast and contrast CT scan neck showed an enhancing polypoidal mass arising from the epiglottis with no cervical lymphadenopathy (Fig. 2) and diagnosis of hemangioma was offered clinico-radiologically. Patient underwent direct laryngoscopy with debulking biopsy of the lesion. Tissue examination was suggestive of a benign vasoformative tumor. Following which patient underwent CO2 Laser assisted excision of epiglottic hemangioma. Definitive histopathological examination of the excised hemangioma showed an encapsulated vasoformative lesion comprising of proliferative capillary sized vascular channels with mild to moderate nuclear atypia of the endothelial cells with occasional mitosis without any evidence of malignancy. The endothelial cells showed CD 31, 34, Vimentin positivity on immunohistochemistry. Patient had an uneventful postoperative recovery with no recurrence on six months follow up period (Fig. 3).
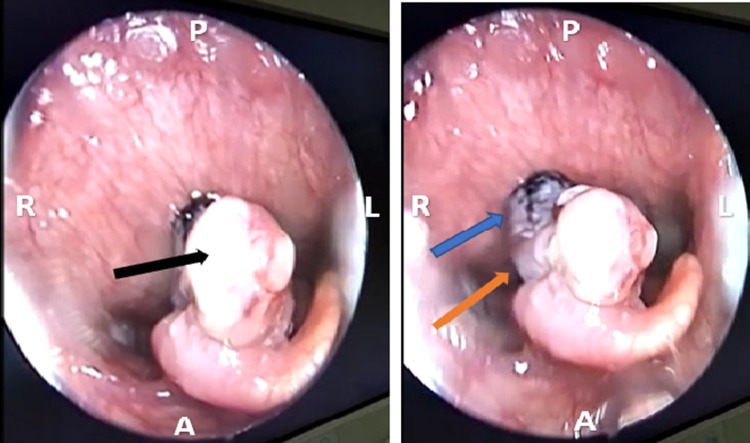
Fig. 1.
Large fleshy mass (black arrow) with bluish grey cystic area (orange arrow) and hemorrhagic changes (blue arrow) over the laryngeal aspect of epiglottis
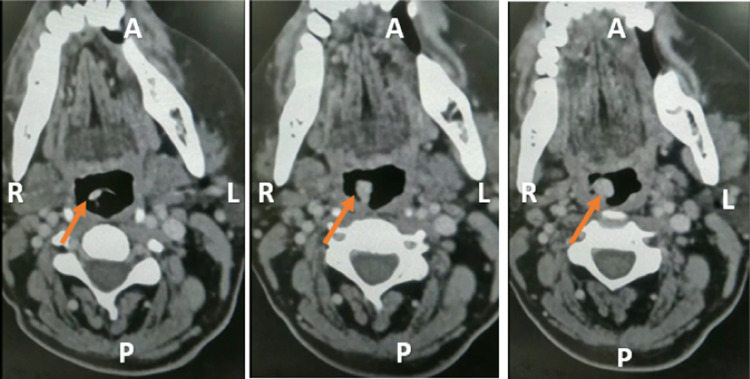
Fig. 2.
Enhancing lesion arising from epiglottis (orange arrow)
Fig. 3.
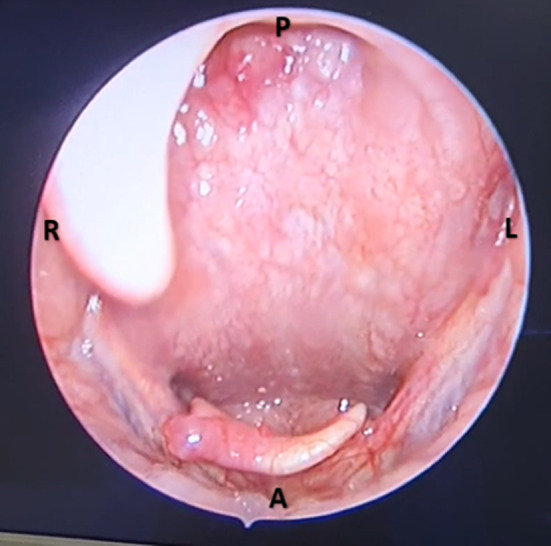
06 month postoperative videolaryngoscopic picture
Discussion
Hemangiomas are common benign tumors of head and neck region arising from endothelial tissues. Infantile hemangiomas of larynx have an incidence rate of 4–5% whereas the adult form has an unknown incidence rate due to scarcity of reports [5]. Subglottis is the most common site in infantile forms and may accompany cutaneous hemangiomas whereas supraglottis in adults [5]. No predisposing/causal factors have been found. Histologically depending upon the vessel size and wall thickness, hemangiomas are classified into cavernous, capillary or mixed type [6]. Most commonly found cavernous hemangiomas are benign but locally destructive and are composed of enlarged dilated vessels with thin walls whereas capillary hemangioma comprises of proliferating small capillary sized vessels. Thin fragile mucosa covers the vascular stroma in mixed type [6].
The symptomatology depends upon the size of lesion and the site of involvement. The individual may remain asymptomatic with an incidental examination finding of the same or may be having symptoms which usually incudes foreign body sensation throat, dysphagia, hoarseness, stridor, hemoptysis. Laryngeal hemangiomas are suspected based on videolaryngoscopic finding assisted by radiological finding of enhancement on a non contrast computed tomographic scan. The various modalities that may aid in the diagnosis include doppler USG, CT scan, MRI, angiography by determining dimension and extent of hemangiomas. The vascular lesions of such sort give excellent signal strength on T2 weighted MR images [7]. The possibility of vascular malformation should be kept as a differential which is histologically differentiated from a hemangioma on the basis of normal endothelial cell turnover and lack of excessive cellular proliferation [8].
There is lack of well-established treatment protocol for the management of adult laryngeal hemangiomas due to paucity of literature [1, 9]. The management option varies from wait and watch policy for asymptomatic patients or for patients with smaller lesions to definitive management in the form of medical and surgical techniques depending upon the site and size of the lesion [9]. The various definitive techniques include systemic/intralesional steroids, sclerosing therapy, cryotherapy, microlaryngoscopic excision, laser technique, ultrasonic scalpel, radiation therapy [10]. Laser assisted excision of the hemangioma gives an advantage of relatively effective treatment with better hemostasis over cold steel technique. The different lasers being used for excision include.
CO2, KTP, Argon, Nd:YAG. CO2 laser utilizing the photothermal reaction is converted into heat by the absorbing substance. In our case, successful CO2 assisted excision of the hemangioma was performed in super pulse mode at intensity varying between 2 and 6 W. Patient was initially followed up fortnightly for 02 months then on monthly basis till 06 months post operatively with no features suggestive of any recurrence in post operative period.
Declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical Approval
Not applicable as it is a case report.
Informed Consent
Informed consent was obtained from the individual participating in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zheng J, Zhou Q, Yang X, Wang Y, Fan X, Zhou G, Zhang Z, Suen J. Treatment guideline for hemangiomas and vascular malformations of the head and neck. Head Neck. 2010;32:1088–1098. doi: 10.1002/hed.21274. [DOI] [PubMed] [Google Scholar]
- 2.Martins RH, Lima Neto AC, Semenzate G, Lapate R. Laryngeal hemangioma. Braz J Otorhinolaryngol. 2006;72:574. doi: 10.1016/S1808-8694(15)31009-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shpitzer T, Noyed AM, Witterick I, et al. Noncutaneous cavernous hemangiomas of the head and neck. Am J Otolaryngol. 1997;18:367–374. doi: 10.1016/S0196-0709(97)90055-7. [DOI] [PubMed] [Google Scholar]
- 4.Mulliken JB, Fishman SJ, Burrows PE. Vascular anomalies. Curr Probl Surg. 2000;37:517–584. doi: 10.1016/S0011-3840(00)80013-1. [DOI] [PubMed] [Google Scholar]
- 5.Kilcline C, Frieden IJ. Infantile haemangiomas: how common are they? A systematic review of the medical literature. Pediatr Dermatol. 2008;25(2):168–173. doi: 10.1111/j.1525-1470.2008.00626.x. [DOI] [PubMed] [Google Scholar]
- 6.Mulliken J, Glowacki J. Hemangioma and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412–420. doi: 10.1097/00006534-198203000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Gelbert F, Riche MC, Reizine D, Guichard JP, Assouline E, Hodes JE, Merland JJ. MR imaging of head and neck vascular malformations. J Magn Reson Imaging. 1991;1:579–584. doi: 10.1002/jmri.1880010511. [DOI] [PubMed] [Google Scholar]
- 8.Haggstrom AN, Drolet BA, Baselga E, et al. Hemangioma Investigator Group. Prospective study of infantile hemangiomas: demographic, prenatal, and perinatal characteristics. J Pediatr. 2007;150:291–294. doi: 10.1016/j.jpeds.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Mulliken JB, Fishman SJ, Burrows PE. vascular anomalities. Curr Probl Surg. 2000;37(8):517–584. doi: 10.1016/S0011-3840(00)80013-1. [DOI] [PubMed] [Google Scholar]
- 10.Huang CM, Lee KW, Huang CJ. Radiation therapy for life threatening huge laryngeal Hemangioma involving pharynx and parapharyngeal space. Head Neck. 2013;35:E98–E101. doi: 10.1002/hed.21919. [DOI] [PubMed] [Google Scholar]