Abstract
Infantile fibrosarcoma is an uncommon soft tissue tumour in infants and children mostly located in the extremities. Its occurrence in the head and neck, particularly in the oral cavity is extremely rare. Here, we report a case of infantile fibrosarcoma of the tongue base in a 9-year-old boy and discuss the complexities in arriving at diagnosis and its management. The patient underwent wide local excision of the tumour. Histopathology was essential in confirming the diagnosis. As per search in English literature, this is the first case of infantile fibrosarcoma of the tongue base to be reported till date. Treatment of choice is wide local excision with or without chemotherapy.
Keywords: Fibrosarcoma, Chemotherapy, Surgery
Introduction
Infantile fibrosarcoma is an uncommon soft tissue tumour in children accounting for about 10% of all sarcomas in children. It can be present at birth or develop during the first few years of life. These tumours typically occur in the extremities. The trunk, gastrointestinal tract, and head and neck are less commonly involved [1].
Here, we report a rare case of infantile fibrosarcoma of the tongue base in a 9-year-old boy.
Case Report
A 9-year-old boy, born to an uncomplicated full term normal pregnancy, presented with complains of progressive difficulty in swallowing since 1 month and difficulty in breathing since 1 week. On examination, there was a multilobulated firm mass in the base of tongue in midline, measuring approximately 3 × 2 cm (Fig. 1). There was no associated cervical lymphadenopathy. On fibreoptic laryngoscopy, the mass was multilobulated, occupying the oropharynx, with a normal larynx. Contrast enhanced computed tomography (CECT) (Fig. 2) revealed a well defined lobulated hyperattenuating mass lesion measuring 20 × 21x28 mm in the base of tongue in midline, with partial attenuation of the oropharynx.
Fig. 1.
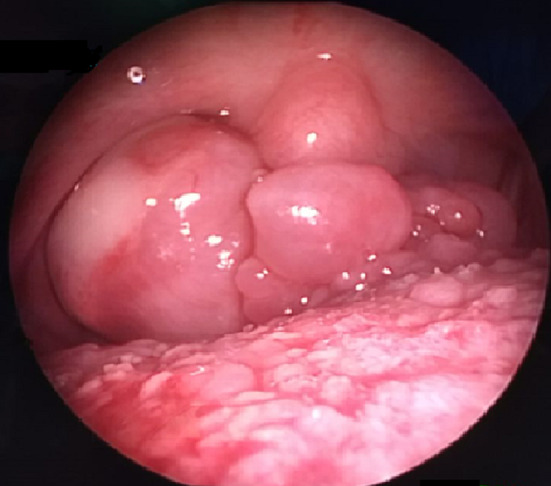
Multilobulate firm mass in base of tongue
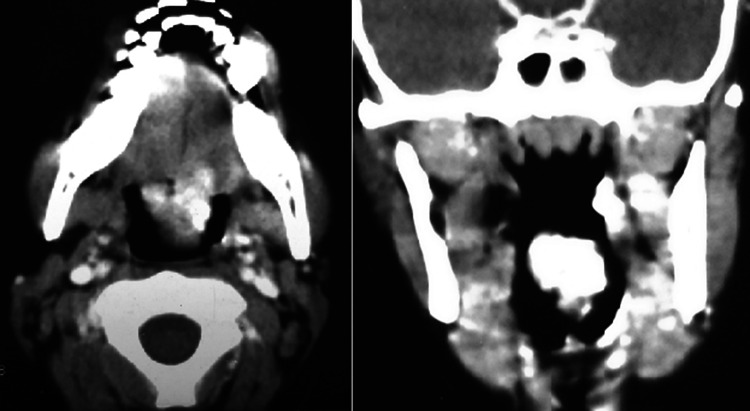
Fig. 2.
CECT (axial and coronal) showing well defined lobulated lesion measuring 20 × 21x28 mm in the base of tongue in midline, with partial attenuation of the oropharynx
Biopsy was taken from the mass. Histopathological examination (Fig. 3) showed round to oval to spindle cells arranged around proliferating vessels. The cells showed minimal to mild pleomorphism and focal areas of necrosis with 1–2 mitosis per high power field. On immunohistochemistry, the tumour cells were positive for vimentin, and negative for CD 34, CD 31, leukocyte common antigen (LCA), desmin synaptophysin, chromogranin, CD 99, neuron specific enolase, cytokeratin, Bcl 2, smooth muscle actin and HMB 45. The histopathology and immunohistochemistry indicated a diagnosis of infantile fibrosarcoma. Under general anaesthesia, the patient underwent wide local excision of the tumour along with cuff of normal tissue (Fig. 4). The tumour was narrow at its base and attached to the base of tongue. Post operative histopathological examination of the mass confirmed the diagnosis of infantile fibrosarcoma, with negative margins. Following surgery, the patient was followed up 3 monthly for 2 years. At 2 years follow up, the patient is asymptomatic and disease free.
Fig. 3.
Histopathology showing: A Tumour composed of round to oval cells arranged in sheets with mild to moderate pleomorphism, frequent mitosis and prominent vessels (HEx400). B Tumour cells positive for vimentin (IHCx200). C Tumour cells negative for CD34 (IHCx200). D Tumour cells negative for SMA (IHCx200)
Fig. 4.
A Intraoperative image showing tumour being excised. B After excision of tumour
Discussion
Infantile fibrosarcoma is a rare, malignant, highly vascularised, mesenchymal tumour that grows rapidly from soft tissues. The main cause remains unknown, but some gene fusions due to translocation and some trisomies have been reported. It usually presents in the first 5 years of life, with most of them occurring in early infancy. It rarely appears at older ages between 10–15 years of age [2].
Infantile fibrosarcoma typically occurs in the extremitites, but has also been reported in the trunk, head and neck, and gastrointestinal tract. In the head and neck region, it has been reported in the mandible [3], nasal cavity [4], ethmoid sinus [5], maxillary sinus [6] and oral cavity. Within the oral cavity, infantile fibrosarcoma has been reported to occur in the tongue [7], lip [8] and buccal vestibule [9]. As per our knowledge, this is the first study to report infantile fibrosarcoma of the tongue base.
The tumour presents as a rapidly growing, poorly circumscribed, non tender mass. In some cases, the surface is necrotic or ulceritic which makes the appearance similar to vascular malformations like hemangioma. Biopsy is essential to exclude hemangiomas, vascular malformations, rhabdomyosarcomas, malignant histiocytoma, and peripheral nerve sheath tumours. On immunohistochemistry, infantile fibrosarcoma is vimentin positive, S100 negative and desmin negative. The prognosis of infantile fibrosarcoma is much more favourable than its adult counterpart [1].
The treatment of choice is wide local excision. A complete resection with negative surgical margins is the goal, but it is often limited by the fact that these tumours often invade muscles and neurovascular structures [10]. It has been reported that complete tumour resection has a 100% 5-year survival probablility but those with residual disease after resection who receive adjuvant therapy fare well with a 76% 5-year survival [10]. Neoadjuvant chemotherapy can be used preoperatively for tumour shrinkage but is typically used in large lesions. If margins are positive after initial resection, chemotherapy is recommended. The most common regimen is VAC regimen (vincristine, actinomycin-D and cyclophosphamide). The role of radiotherapy is controversial, but it is not used often because of the deleterious effects on growth plates and the risk of development of secondary malignancies. In our patient, due to the negative margins after primary resection, the patient was followed up 3 monthly to rule out tumour recurrence. At 2 years follow up, the patient is asymptomatic and disease free.
Funding
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial interests to disclose. No source of funding.
Declarations
Conflict of interest
No conflict of interest (for all authors).
Ethical approval
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Informed consent
Informed consent not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Enzinger FM, Weiss SW. Soft tissue tumors. St. Louis, Toronto, London: Mosby; 1983. pp. 116–122. [Google Scholar]
- 2.Schofield DE, Fletcher JA, Grier HE, Yunis EJ. Fibrosarcoma in infants and children. Application of new techniques. Am J Surg Pathol. 1994; 18: 14–24. [DOI] [PubMed]
- 3.Bang G, Baardsen R, Gilhuus-Moe O. Infantile fibrosarcoma of the mandible: case report. J Oral Pathol Med. 1989;18:339–343. doi: 10.1111/j.1600-0714.1989.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 4.Kim KI, Yoo SL. Infantile fibrosarcoma in the nasal cavity. Otolaryngol Head Neck Surg. 1996;114:98–102. doi: 10.1016/S0194-59989670291-7. [DOI] [PubMed] [Google Scholar]
- 5.Geramizadeh B, Khademi B, Karimi M, Shekarkhar G. infantile fibrosarcoma of ethmoid sinus misdiagnosed as an adenoid in a 5-year-old child. J Oral Maxillofac Pathol. 2015;19:271. doi: 10.4103/0973-029X.164567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palacios E, Lam EC. Infantile fibrosarcoma of the maxillary sinus: significant response. Ear Nose Throat J. 2012;91:98–100. doi: 10.1177/014556131209100305. [DOI] [PubMed] [Google Scholar]
- 7.Wahid FI, Zada B, Rafique G. Infantile fibrosarcoma of tongue: a rare tumour. APSP J Case Rep. 2016;7:23. doi: 10.21699/ajcr.v7i3.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bellfield EJ, Beets-Shay L. Congenital infantile fibrosarcoma of the lip. Pediatr Dermatol. 2014;31:88–89. doi: 10.1111/pde.12213. [DOI] [PubMed] [Google Scholar]
- 9.Tarsitano BF. Oral infantile fibrosarcoma: report of a case. J Oral Maxillofac Surg. 1990;48:1228–1230. doi: 10.1016/0278-2391(90)90545-D. [DOI] [PubMed] [Google Scholar]
- 10.Orbach D, Rey A, Cecchetto G, Oberlin O, Casanova M, Thebaud E, et al. Infantile fibrosarcoma: management based on the European experience. J Clin Oncol. 2010;28:318–323. doi: 10.1200/JCO.2009.21.9972. [DOI] [PubMed] [Google Scholar]