Abstract
A pharyngocutaneous fistula (PCF) is the most common complication after salvage total laryngectomy (STL) with an incidence ranging from 5 to 73%, causing an increase in morbidity and delaying the patient’s recovery. A surgical technique to prevent PCF formation is the use of the stapler to suture the pharyngeal mucosa. We have reviewed the medical files of 91 patients who had undergone STL, dividing the patients into two groups (manual suture vs. stapler), based on the type of pharyngeal suture performed during the STL. We found 12/49 (24.5%) cases of a PCF in group A (manual) and 5/42 (11.9%) cases of a PCF in group B (stapler). There is a statistically significant difference between the two groups with the patients in group B presenting better results in terms of the reduction of the surgical time, the length of the hospital stay and also in the restarting of oral feeding. The advantages of mechanical suturing with the stapler are reduced surgical times, a lower PCF formation rate, which involves an early removal of the nasogastric tube, and reduced hospitalization times. Further studies with a larger case series will be necessary to confirm the results obtained and to standardize the surgical technique.
Keywords: Pharyngocutaneous fistula, Surgical staplers, Total laryngectomy, Laryngeal neoplasms
Introduction
Carcinoma of the larynx is the most frequent tumour of the upper digestive aerial tract (28%), accounting for about 2.5% of all malignant tumours in men and 0.5% in women.
Despite the major advances in ‘organ preservation’ strategies, a significant number of patients still experience residual or recurrent disease and will ultimately require salvage laryngectomy (STL). This type of surgery poses technical difficulties because of post-radiotherapy fibrosis and entails a high rate of post-operative complications [1, 2].A pharyngocutaneous fistula (PCF) is the most common complication after STL. In the literature there has been a wide variability in the rates of PCF formation, ranging from 5.6 to 73% with an average incidence of 28.9%. A PCF increases morbidity, hospitalization time and expense, and delays the beginning of adjuvant treatment. Multiple risk factors have been related to the onset of a PCF: previous haemoglobin < 12.5 g/dL, chronic obstructive pulmonary disease, blood transfusion, radiotherapy (RT) or chemoradiotherapy (CRT), a supraglottic subsite, advanced primary tumour, hypopharyngeal tumour site, positive surgical margins and a neck dissection in addition to the STL [3–5].To decrease the incidence of this serious complication various techniques have been described in the literature, including free or pedicled flap, broad spectrum antibiotic therapy and stapler pharyngeal closure [3]. The use of the stapler to close the pharynx during total laryngectomy was described for the first time in 1973. Over the years this surgical technique has been discussed, revealing conflicting opinions on account of some limitations that this “closed technique” presents. The stapler cannot be used in patients with hypopharyngeal carcinoma, an extra laryngeal tumour or a tumour involving the base of the tongue, except for laryngeal cancer with an invasion of the thyroid cartilage [6, 7]. Instead, this device is recommended in the case of tumours of the anterior portion of the larynx. This preoperative indication is first confirmed clinically (with a fibrolaryngoscopy) and then radiologically. The stapler is a suturing device, which allows the achievement of a leak resistant and haemostatic closure line using metal staples. This tool is handy, easy to use and safe, especially in challenging tissue [2].The aim of this study is to describe the surgical stapler technique in order to evaluate the incidence of PCF formation in STL and to verify if this technique can bring other benefits, which can affect the quality of life of the patient, such as a reduction of the hospitalization stay, a decrease in the surgical time and a faster application of oral feeding, compared to the manual suture technique.
Materials and Methods
All patients affected by laryngeal squamous cell carcinoma (LSCC), who had been surgically treated by means of a STL between January 2006 and January 2021, were retrospectively reviewed using information retrieved from a database dedicated to such procedures in a single tertiary care referral institute. The study was performed in compliance with the Helsinki Declaration and with policies approved by the local board of ethics. Each STL was performed by the same surgeon.
The inclusion criteria were as follows: (1) a histologically-proven case of endolaryngeal squamous cell carcinoma (ELSCC); (2) a primary treatment failure, either by radiotherapy (RT), chemoradiotherapy (CRT) or previous surgery; (3) a complete head and neck examination, by videolaryngoscopy with narrow-band imaging (NBI), chest computed tomography (CT) and magnetic resonance imaging (MRI) or CT of the larynx and neck and neck ultrasound; (4) the absence of any involvement of the tongue base (5) the absence of any hypopharyngeal carcinoma and (6) the absence of any extralaryngeal tumour. The exclusion criteria for the stapler group were a posterior extension of the tumour, an infiltration of the suprahyoid epiglottis, a pyriform sinus or a retro cricoid region. All the tumours were retrospectively staged according to the TNM classification (eighth edition) [8]. From a histological viewpoint, the ELSCCs were categorized according to the World Health Organization/International Agency for Research on Cancer classification of human tumours, which is accepted and used worldwide [9].Our sample was divided into two groups (A and B) based on the type of pharyngeal suture performed during the STL. Group A (the manual suture group) included 49 patients while group B (the stapler pharyngeal closure group) consisted of 42 patients. These two groups were compared in relation to gender, age, diabetes mellitus, alcohol consumption, smoking habit, clinical stage, tumor extension, primary treatment and neck dissection (Table 1).
Table 1.
Patients’ clinical data (n = 91)
| Group A, manual suture (49 patients) | Group B, stapler suture (42 patients) | P value | |
|---|---|---|---|
| Gender (M/F) | 45/4 | 37/5 | |
| Age (years) | 65.73 | 66.81 | 0.23 |
| Diabetes mellitus | 8 | 7 | 0.96 |
| Alcohol consumption | 5 | 7 | 0.36 |
| Smoking | 47 | 42 | 0.18 |
| Clinical staging | |||
| T2 | 2 | 3 | 0.70 |
| T3 | 12 | 8 | |
| T4a | 35 | 31 | |
| Tumour extension | |||
| Supraglottic | 26 | 14 | 0.05 |
| Glottic | 21 | 28 | |
| Hypoglottic | 2 | 0 | |
| Primary treatment | |||
| CRT | 15 | 11 | 0.85 |
| RT | 24 | 23 | |
| Surgery | 10 | 8 | |
| Neck dissection | |||
| Yes | 45 | 39 | 0.86 |
| No | 4 | 3 |
In Group A the site of the tumor was supraglottic region in 26 patients, glottic area in 21 patients and hypoglottic in 2 patients. In Group B we reported in 14 patients a lesion arising from supraglottic area and in 28 patients a tumor of the glottic area. They were also compared in terms of the incidence of the PCF formation, the restarting of oral feeding after the surgical procedure, the surgical time and the length of the hospitalization stay (Table 2).
Table 2.
Incidence of PCF formation, surgical time, restarting of oral feeding and length of hospitalization stay
| Group A, manual suture (49 patients | Group B, stapler suture (42 patients) | P value | |
|---|---|---|---|
| Incidence of PCF formation | 12 | 5 | 0.12 |
| Surgical time (mins) | 285.37 ± 120.53 | 245 ± 43.92 | < 0.05 |
| Restarting of oral feeding (days) | 18.82 ± 9.11 | 13.23 ± 11.31 | < 0.05 |
| Lenght of hospitalization stay (days) | 24.84 ± 12.34 | 15.23 ± 8.54 | < 0.05 |
Written informed consent was obtained from all the patients prior to any diagnostic or therapeutic procedure. All the patients provided a written informed consent for the publication of their data in an anonymous form. They all consented to the use of all photographs, illustrations and data for the purposes of educational content. The signed consent forms are on file at the maxillofacial and ENT department of the National Cancer Institute “G. Pascale” of Naples, Italy, containing personally identifiable patient information and signatures.
Statistical Analysis
For the categorical variables the chi square test for multiple comparisons was used and for the continuous variables, the Mann Witney non-parametric test. Differences were considered significant at a p value < 0.05.The statistical analysis was performed using Matlab R2021b (MathWorks, Natick, MA, USA).
Stapler Surgical Technique
The surgical procedure begins with the dissection of the soft tissues of the neck, following which the thyroid isthmus is reached and divided. The trachea is detached at the required level, depending on the subglottic extension, and the tracheoesophageal membrane is dissected to expose the posterior cricoarytenoid muscles. The larynx is completely mobilized and remains connected to the pharynx by the mucosa. The free edge of the epiglottis is pulled into the larynx and passed through the tracheal lumen, to avoid including the epiglottis in the suture line. The larynx is then elevated and retracted by two Allis clamps, one positioned inferiorly on the remaining trachea, the other superiorly grasping the hyoid bone (Fig. 1). At this point the stapler ECHELON FLEX™ ENDOPATH® (Johnson & Johnson Medical Devices Companies**) is positioned parallel to the pharyngeal mucosa and actioned and a linear suture is obtained in order to preserve the proper oesophageal calibre (Fig. 2). In particular, the performance of the stapler provides for the closure of the jaws with a subsequent affixing of the staples while the flaps of the mini-pharyngotomy are raised above the jaws. The opening of the jaws therefore results in a linear suture, performed in a few minutes, hermetic, stable in the long-term and with rapid healing times, significantly reducing the patient management costs1. (Fig. 3). At the end of the surgical procedure, a nasogastric tube was applied to allow enteral feeding. The assessment of the fistula onset in both groups was performed between the tenth and the eleventh postoperative day using a methylene blue test. In the absence of any PCF formation, the nasogastric tube was removed and the patients were discharged a few days after the restarting of the oral feeding. In the case of a PCF, local wound dressing was performed for two weeks and, if the PCF persisted, further measures were taken. such as the injection of autologous fat or the application of a locoregional or free flap.
Fig. 1.
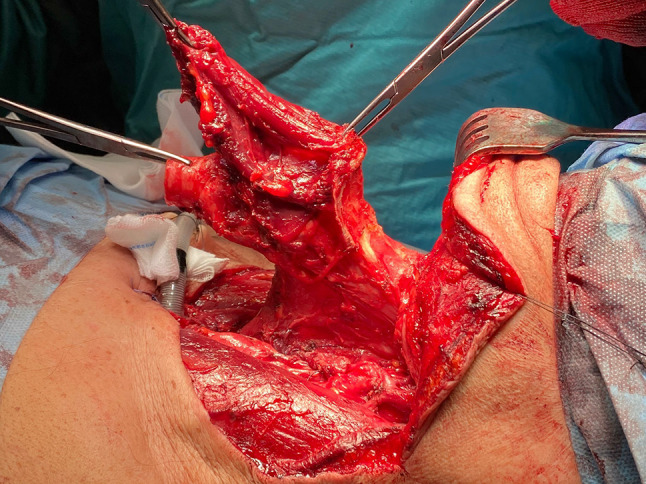
View of the mobilized larynx, suspended at the ends by two Allis clamps connected to the pharynx through the mucous membrane
Fig. 2.
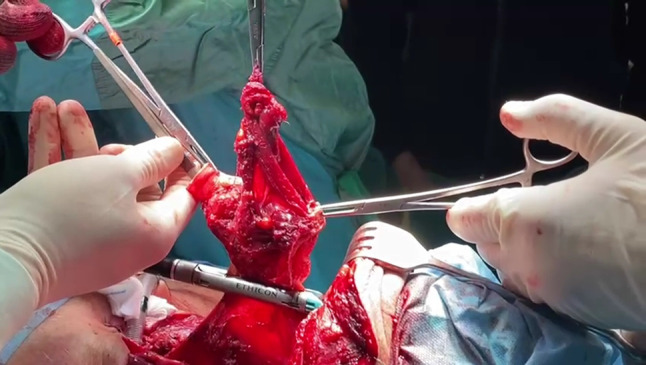
Application of the stapler on the pharyngeal mucosa
Fig. 3.
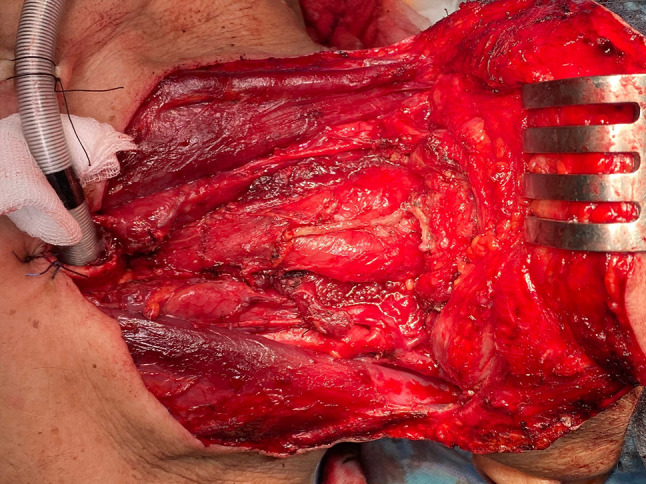
View of the linear suture resulting from the use of the stapler
Results
The 91 patients who respected the inclusion criteria for the present analysis were enrolled in the study. The median age at the time of diagnosis was 65.73 years in Group A and 66.81 years in Group B. The demographic and clinical characteristics of both groups are detailed in Table 1. All the tumors were treated with a total laryngectomy, A bilateral neck dissection was performed in 84 cases out of 91 (92.3%), 45 out of 49 (91.8%) in group A and 39 out of 42 (92.8%) in group B. With regard to the T classification, 5 patients were staged as T2, 20 as T3 and 66 as T4a without any significant statistical difference between the two groups. Regarding the evaluation of the incidence of a PCF there was no significant statistical difference between the two groups in terms of the presence of diabetes mellitus, primary treatment or nutritional status. We found 12/49 (24.5%) cases of PCF formation in group A and 5/42 (11.9%) cases of PCF formation in group B. Despite this great reduction, this difference (p = 0.12) was not considered statistically significant according to our range (p < 0.05).
The STL was performed after CRT, RT or surgical treatment, respectively, in 15, 24 and 10 patients in group A and in 11, 23 and 8 patients in group B. In the A and B groups, the duration of the surgery was 285.37 ± 120.53 min in group A versus 245 ± 43.92 min in group B; the mean oral feeding restarting time was 18.82 ± 9.11days versus 13.23 ± 11.31days; and the length of the hospitalization stay was 24.84 ± 12.34 days versus 15.23 ± 8.54 days, respectively. All of these differences were statistically significant (p < 0.05). (Table 2).
Discussion
The development of a PCF after total laryngectomy is one of the most common complications of this surgery. Various types of significant risk factors for the formation of a PCF have been described in the international literature, including smoking, alcohol consumption, the age of the operated patient, malnutrition, positive surgical margins, heart disease and especially diabetes mellitus. In fact, the consequences of hyperglycaemia are glucosuria and impaired wound healing and these diabetic patients are at an increased risk of an adverse outcome after surgery [10–13]. Several studies report that the PCF formation rate is higher in the case of patients who have already undergone an operation or have been previously irradiated. Some investigations have identified an RT dose greater than 5000 cGy as a high risk factor. The influence of high-dose radiation on wound healing includes hypoxia, reduced leukocyte migration, fibrosis and delayed wound closure[3]. This type of serious complication continues to occur with an incidence ranging from 5 to 73%, causing an increase in morbidity and delaying the patient’s recovery. In fact, treatment of a PCF requires a prolonged hospital stay and further medical-surgical procedures [14, 15].A surgical aid described in the literature to prevent PCF formation is the use of the stapler to suture the pharyngeal mucosa. The linear stapler technique in total laryngectomy is a safe and time-saving method due to the fact that manual suturing is more challenging, although it is performed with a continuous closure. It is a simple technique with potential benefits that lie mainly in its simplicity and the standardization of the suture, together with the reduction of surgical times.The suture resulting from the use of the stapler has a reduced tension in the margins. a lower probability of dehiscence and a tighter closure so it reduces the risk of contamination by oral and pharyngeal secretions. The material applied by the mechanical stapler has an excellent tolerance by the tissue due to the minimal inflammatory reaction2.The use of the stapler is widely described in general surgical procedures but has some limitations in the case of total laryngectomies. It is essential to know the extent of the primary tumour to establish whether or not it is possible to use the stapler. This can be inferred from preoperative clinical and radiological investigations but must be confirmed by a previous suspension laryngoscopy performed in the operating room.It is recommended to reserve this procedure for cases in which the endolaryngeal site of the tumour is confirmed. It should be excluded if the neoplasm involves the suprahyoid epiglottis, the pyriform sinus, and the retro cricoid region. Clearly, in the event that the patient is not correctly selected, the use of the stapler could compromise the patient’s oncological healing. According to Bedrin et al. [16] to the best of our knowledge the largest retrospective study regarding stapler suturing in STL, a reduction in the PCF formation rate was found in the group of patients undergoing mechanical suturing, leading to an early removal of the nasogastric tube. In our study we found 12/49 (24.5%) cases of PCF formation in group A (the manual suture group) and 5/42 (11.9%) cases of PCF formation in group B (the stapler suture group). Despite this strong reduction, this difference is not considered statistically significant (Table 2). To the best of our knowledge only Dedivitis et al. have found a higher rate of PCF formation in the stapler group compared to those treated with a manual suture [14].In addition to decreasing the rate of PCF formation, the use of the stapler can be an important aid in terms of a reduction in the surgical time, a reduction in the length of the hospitalization stay and a restarting of oral feeding. Galli et al. [1] showed a reduction in operating times of about 26 min (268 min vs. 294 min), a reduction in the hospitalization of about 6 days (17.6 days vs. 23.7 days), and a reduction in the restarting of oral feeding of about 5 days in relation to the stapler group as compared to the manual suture group (15 vs. 20).In our study, also, a statistically significant difference was revealed between the two groups as regards a reduction of the surgical time of about 40 min (245 min in the stapler group vs. 285 min in the manual suture group), in the length of the hospital stay (15 days vs. 24 days) and in the restarting of oral feeding (13.23 days vs. 18.82) (Table 2). In conclusion, the advantages of mechanical suturing are the reduction of the surgical time, a tighter and safer closure with less contamination from oropharyngeal secretions, a lower PCF formation rate, which involves an earlier removal of the nasogastric tube, and a reduced hospitalization time. A significant disadvantage consists in the extension of the primary tumour, as the technique can only be used in relation to endolaryngeal carcinomas, which have previously been evaluated by endoscopy and imaging. Furthermore, the mechanical stapler does not allow a direct visualization of the tumour during the procedure. Our study is not free from limitations, such as its retrospective nature, the exclusion of patients who had not undergone a primary laryngectomy as a surgical treatment and the small sample size. However, a strength of the study is that the 91 total laryngectomies were all performed by the same surgeon in a tertiary referral centre.
Conclusion
The use of a stapler for pharyngeal closure after total laryngectomy is indicated only for endolaryngeal tumours. The stapler suture seems to decrease the rate of PCF formation and can be an important aid in terms of a reduction in the surgical time, a reduction in the length of the hospitalization stay and an earlier restarting of oral feeding. Further studies with a larger case series will be necessary to confirm the results obtained and to standardize the surgical technique.
Author contributions
All authors contributed significantly to the work and have read and approved the final version of the manuscript.
Funding
None.
Declarations
Conflict of interest
The authors declare no conflict of interest
Ethical Approval
Approval was obtained from the ethics committee of University Federico II of Naples, Italy . The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent
Informed consent was obtained from all individual participants included in the study
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Galli J, Salvati A, Di Cintio G, et al. Stapler use in salvage total laryngectomy: a useful tool? Laryngoscope. 2021;131:473–478. doi: 10.1002/lary.28737. [DOI] [PubMed] [Google Scholar]
- 2.Aires FT, Dedivitis RA, Castro MA, et al. Efficacy of stapler pharyngeal closure after total laryngectomy: a systematic review. Head Neck. 2014;36:739–742. doi: 10.1002/hed.23326. [DOI] [PubMed] [Google Scholar]
- 3.Liang JW, Li ZD, Li SC, et al. Pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis of risk factors. Auris Nasus Larynx. 2015;42:353–359. doi: 10.1016/j.anl.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Hasan Z, Dwivedi RC, Gunaratne DA, et al. Systematic review and meta-analysis of the complications of salvage total laryngectomy. Eur J Surg Oncol. 2017;43:42–51. doi: 10.1016/j.ejso.2016.05.017. [DOI] [PubMed] [Google Scholar]
- 5.Tsetsos N, Poutoglidis A, Vlachtsis K, et al. Twenty-year experience with salvage total laryngectomy: lessons learned. J Laryngol Otol. 2021;135:729–736. doi: 10.1017/S0022215121001687. [DOI] [PubMed] [Google Scholar]
- 6.Simoncelli C, Altissimi G. Mechanical sutures of the pharynx during total laryngectomy: proposal of a closed technique. Acta Otorhinolaryngol Ital. 1990;10:465–474. [PubMed] [Google Scholar]
- 7.Altissimi G, Frenguelli A. Linear stapler closure of the pharynx during total laryngectomy: a 15-year experience (from closed technique to semi-closed technique) Acta Otorhinolaryngol Ital. 2007;27:118–122. [PMC free article] [PubMed] [Google Scholar]
- 8.Edge SB. American Joint Committee on Cancer (AJCC) cancer staging manual. 8. New York: Springer; 2017. [Google Scholar]
- 9.El-Naggar AK. WHO classification of tumors pathology and genetics of head and neck tumors. 4. Lyon: IARC Press; 2017. [Google Scholar]
- 10.Dedivitis RA, Aires FT, Cernea CR, et al. Pharyngocutaneous fistula after total laryngectomy: systematic review of risk factors. Head Neck. 2015;37:1691–1697. doi: 10.1002/hed.23804. [DOI] [PubMed] [Google Scholar]
- 11.Kim YH, Roh JL, Choi SH, et al. Prediction of pharyngocutaneous fistula and survival after salvage laryngectomy for laryngohypopharyngeal carcinoma. Head Neck. 2019;41:3002–3008. doi: 10.1002/hed.25786. [DOI] [PubMed] [Google Scholar]
- 12.Basheeth N, O’Leary G, Sheahan P. Pharyngocutaneous fistula after salvage laryngectomy: impact of interval between radiotherapy and surgery, and performance of bilateral neck dissection. Head Neck. 2014;36:580–584. doi: 10.1002/hed.23337. [DOI] [PubMed] [Google Scholar]
- 13.Casasayas M, Sansa A, García-Lorenzo J, et al. Pharyngocutaneous fistula after total laryngectomy: multivariate analysis of risk factors and a severity-based classification proposal. Eur Arch Otorhinolaryngol. 2019;276:143–151. doi: 10.1007/s00405-018-5200-4. [DOI] [PubMed] [Google Scholar]
- 14.Dedivitis RA, Aires FT, Pfuetzenreiter EG, Jr, et al. Stapler suture of the pharynx after total laryngectomy. Acta Otorhinolaryngol Ital. 2014;34:94–98. [PMC free article] [PubMed] [Google Scholar]
- 15.Lee YC, Fang TJ, Kuo IC, Tsai YT, Hsin LJ. Stapler closure versus manual closure in total laryngectomy for laryngeal cancer: a systematic review and meta-analysis. Clin Otolaryngol. 2021;46:692–698. doi: 10.1111/coa.13702. [DOI] [PubMed] [Google Scholar]
- 16.Bedrin L, Ginsburg G, Horowitz Z, et al. 25-year experience of using a linear stapler in laryngectomy. Head Neck. 2005;27:1073–1079. doi: 10.1002/hed.20280. [DOI] [PubMed] [Google Scholar]


