Abstract
The use of operating microscope and rigid telescope in laryngeal surgery represents one of the most exciting advances. Both systems provide good illumination, magnification and relative ease of operation. Microlaryngeal surgery (MLS) with suspension laryngoscope is currently considered the gold standard for surgical approach to the larynx for excision of benign lesions of vocal folds.
The limitation of this technique is intubation, general anesthesia (GA) related and in difficult exposure of larynx. The development of ideal anesthetic system has not been successful in satisfying both the surgeon and the anesthesiologist. Fiberoptic Laryngeal Surgery (FLS) is convenient as it avoids GA, is an outpatient procedure with less morbidity and reduced costs. FLS is preferable for the patients who have medical contraindications for general GA. To compare the efficacy of MLS and FLS surgical procedures in terms of functional outcome. This is a comparative clinical study done on 42 patients who were diagnosed to have benign vocal fold pathology. Pre and post-operative speech evaluation was done for all the patients by the same examiner, which included GRABS scale, Maximum Phonation Time, voiced consonants, voiceless consonants, s/z ratio along with stroboscopy. In Group A, MLS was the treatment modality, done under GA, while in Group B, FLS was the treatment modality done under Local Anesthesia (LA). After one-month, post-operative evaluation of voice was done. When the Maximum Phonation Time, S/Z ratio and stroboscopic parameters (mucosal wave) were compared between the two study groups there appeared no statistically significant difference between the two groups. Our study shows that when benign vocal cord pathologies were treated by MLS or FLS the voice Quality improvement remains the same. FLS is the procedure of choice when MLS under general anesthesia is contraindicated.
Keywords: Benign vocal cord pathology, Micro laryngeal surgery, Fiberoptic laryngeal surgery, Hyperbolic output distance function, Voice quality improvement
Introduction
Genesis of modern surgery of the vocal fold stems from Hiranos discovery of the layered microarchitecture of the lamina propria and synthesis of the anatomy and physiology of the vocal folds into his cover body theory of vocal fold vibration [1].Stroboscopy is an integral part of assessment of vocal function in the clinical voice laboratory and has proven to be one of the most useful methods for evaluating the vibratory movements of the vocal folds [2]. The use of operating microscope and rigid telescope in laryngeal surgery represents one of the most exciting advances. Both systems provide good illumination, magnification and relative ease of operation [3].
Microlaryngeal surgery (MLS) with suspension laryngoscope is currently considered the gold standard for surgical approach to the larynx for excision of benign lesions of vocal folds, however it is not without its limitations like sharing of the airway by the surgeon and anaesthetist, injury to teeth and taste disturbance. The limitation of this technique is intubation and anaesthesia related and in difficult exposure of larynx. MLS under General anaesthesia (GA) requires hospitalization. The development of ideal anesthetic system has not been successful in satisfying both the surgeon and the anesthesiologist. Operating microscope and endoscopes in laryngeal surgery are widely used as both systems provide good illumination and magnification. Fiberoptic Laryngeal Surgery (FLS) is convenient as it avoids general anaesthesia, is an outpatient procedure with less morbidity and reduced costs. Fiberoptic Laryngeal Surgery (FLS) is preferable for the patients who have medical contraindications for GA [4].
Aim and Objective
To compare the efficacy of MLS and FLS surgical procedures in terms of functional outcome.
Materials and Methods
A comparative hospital-based study was carried out among patients diagnosed with benign vocal cord pathology admitted at our ENT Hospital, during the period of June 2017 to November 2019. Ethical Clearance to perform this study was obtained. Informed consent from the patients were obtained after explaining the nature of the proposed treatment. A total of 42 cases were admitted with benign vocal cord (VC) pathology during this period and surgical intervention was done by either micro laryngeal or fiberoptic laryngeal surgery alternatively. For example, if first patient was treated with micro laryngeal surgery, the next case was treated with fiberoptic laryngeal surgery. Thus, a total of 22 cases were operated by micro laryngeal surgery done under GA and 20 by fiberoptic laryngeal surgery done under Local anesthesia (LA).
Patients in both the groups were examined in detail with pre operative stroboscopy using an Atmos stroboscopy Unit and a 70-degree Storz laryngeal endoscope and speech evaluation was also done. The following parameters were used in speech evaluation GRABS scale (scored as 0, 1, 2, 3), Maximum Phonation Time (MPT), voiced consonants, voiceless consonants, S/Z ratio. These patients were reviewed after 10 days and at the end of 8 weeks post-operatively for stroboscopy and speech evaluation. Stroboscopy and speech evaluation was done by the same person pre-operatively and post-operatively.
Micro Laryngeal Surgery
Anaesthetic Technique
All the patients undergoing MLS were pre-medicated with injection Glycopyrolate 10–20 mic/kg and injection Hydrocortisone 1–1.5 mg/kg, both given intra-muscular 45 min before the procedure. Induction was done with Injection propofol 2–3 mg/kg followed by injection Scoline 2 mg/kg. The patients were intubated with a relatively small sized cuffed endotracheal tube 4.5–6.5 mm internal diameter. 10% xylocaine was sprayed into the pharynx and larynx. Anesthesia was maintained with Oxygen, nitrous oxide and sevoflurane. Skeletal muscle relaxation was given with injection vecuronium 0.1 mg/kg.
Surgical Technique
The patient was placed in Boyce’s position and using the kleinsasser laryngoscope, the endolaryngeal structures were visualized with a binocular microscope through a 400 mm lens. About 0.5 ml of preformed solution of 2% Xylocaine and 1 in 200,000 adrenaline was injected into the base of the lesion. A cotton ball soaked in saline was placed in the subglottis to prevent any blood entering the trachea. Dissection was usually carried out using a combination of a small forceps and a scissors. The polyp was grasped with a forceps and dissected and excised by scissor. Hemostasis was usually achieved by placing a moist cotton ball. An intraoperative view of vocal cord (VC) polyp through MLS shown in Fig. 1.
Fig. 1.

Intraoperative view of vocal cord (VC) polyp through MLS
Fiberoptic Laryngeal Surgery
Anaesthetic Technique
FLS was done under Local Anesthesia in the Out Patient Department. All the patients were premedicated with injection promethazine 25 mg intramuscular and injection glycopyrrolate 0.2 mg intravenously 30 min before surgery. A topical 4% Lignocaine gargle is administered to the laryngo-pharynx just prior to the procedure with curved cannula and syringe under visual control.
Surgical Technique
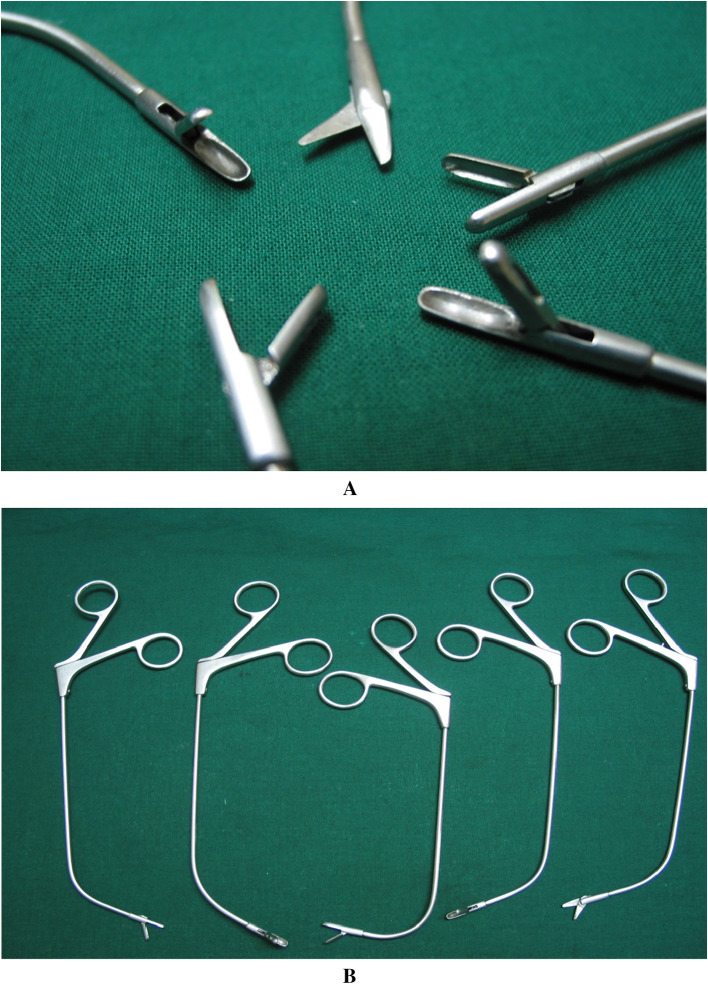
Patient was comfortably seated with surgeon standing in front of the patient. A chip on tip, PENTAX CP 1000 (3 mm diameter) video Fibreoptic nasopharyngoscope attached to STROZ Digital Camera System, with a Xenon Aesculap Axel 180 (OP 930) light source was passed through the nose and positioned to get an optimal image of the glottis on the monitor. The patient was instructed to open his/her mouth and hold the tongue forward with his hand. The custom-made curved laryngeal forceps (shown in Fig. 2 A and B) was passed intra-orally and the lesions were removed. The assistant stands to the left of the surgeon to help in guiding the scope and the Scrub nurse to the right of the surgeon as shown in Fig. 3.
Fig. 2.
A Custom made curved laryngeal forceps (closer view of the tip). B Custom made curved laryngeal forceps
Fig. 3.
Position of patient and the surgeon during FLS
Patients with neoplastic lesions, patients not willing for manipulations under LA, patients lost to follow up, lesions with a tendency to bleed like hamartomas, sulcus vocalis and vocal fold cysts were excluded from the study.
Results
Our study constituted of 42 patients. We had 14 male and 8 female patients in group A (MLS) and 9 male and 11 female patients in group B (FLS) as shown in Table 1. Hoarseness of voice was the most common complaint in both groups (100%). A positive history of Voice abuse was seen in all the patients 42(100%).
Table 1.
Age and sex distributions
| Age distribution | Group A (n = 22) MLS |
Group B (n = 20) FLS |
||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| < 40 | 9 | 5 | 3 | 6 |
| > 40 | 5 | 3 | 6 | 5 |
| 14 | 8 | 9 | 11 | |
In Group A 90% had vocal fold polyp and 10% had vocal fold nodule whereas in Group B majority had vocal fold polyp (100%) as shown in Table 2
Table 2.
Clinical findings
| Vocal cord polyp (%) | Vocal cord nodule | |
|---|---|---|
| Group A (n=22) | 20 (90) | 2 (10%) |
| Group B (n=20) | 20 (100) | 0 |
In Group A the mean pre- and post-operative MPT was 12.82 ± 4.22 s and 18 ± 2.99 s respectively. In Group B pre-operative MPT was 10.77 ± 3.73 s, which improved to 17.46 ± 1.5 s in the post-operative period (Table 3). Thus, we find that MPT in group A show greater variation than group B being in the ratio of 16.61/8.57 = 1.94: 1
Table 3.
Comparative results of MPT in 2 groups
| Pre-operative | Post-operative | |
|---|---|---|
| Group A [MLS] | 12.82 ± 4.22 | 18 ± 2.99 |
| Group B [FLS] | 10.77 ± 3.73 | 17.46 ± 1.5 |
The comparative post-operative mucosal wave appearance results demonstrate that around 86% in group A and 80% in Group B had obtained good results as shown in Table 4. The results were compared and analyzed using chi square test.
Table 4.
Comparative post operative results of mucosal wave and S/z ratio in the 2 study groups
| Mucosal wave | S/Z ratio in seconds | |||
|---|---|---|---|---|
| Present | Absent | 1–2 | 2–3 | |
| Group A [MLS] | 19(86.36%) | 3(13.5%) | 20(90.90%) | 2(9.09%) |
| Group B [FLS] | 16(80%) | 4(20%) | 18(90%) | 2(10%) |
| Total | 35 | 7 | 38 | 4 |
When the post operative results of S/Z ratio were compared in both the groups the results were found to be the same 90.90% as shown in Table 4. Using the chi square test there was no statistical difference between the 2 groups as the p value was more than 0.05.
When the MPT, S/Z ratio and stroboscopic parameters (mucosal wave) were compared between the two study groups there appeared to be no statistically significant difference between the two groups.
The comparative post-operative GRABS scale (hoarseness) evaluation demonstrates that around 95% in group A and Group B had obtained good results (Table 5).
Table 5.
Comparative results of GRABS scale (hoarseness) in both group
| Post-operative hoarseness | ||
|---|---|---|
| Absent | Present | |
| Group A [MLS] | 21 (95.45%) | 1 (4.54%) |
| Group B [FLS] | 19 (95%) | 1 (5%) |
Hence, these results show that when benign vocal fold pathologies like vocal fold polyp or vocal fold nodule are treated by MLS or FLS there is no statistically significant difference in the results. With either of the surgeries the voice Quality improvement remains almost the same.
Discussion
The first specifically designed rigid laryngoscope to be used in the office setting was described by Andrews and Gould in 1977. In 1981, a simple method of attaching a rigid scope to a video camera was described by Yanangisawa et al. [5].
In our study both the groups were well matched in the grade of hoarseness of voice. Pre operatively 90% of patients in both the group had G1-G2 grade of hoarseness, postoperatively the degree of hoarseness was G0 in all the patients, a good surgical and vocal outcome was achieved in all the cases. As seen in the study done by Omori et al. [6] in 2000 following videoendoscopic laryngeal surgery there was significant improvement in the scores for roughness and breathiness post-operatively.
The use of the s/z ratio as a clinical indicator of laryngeal pathology was investigated, in 1981 by Frances C. Eckel and Daniel R. Boone et al. [7] with 28 dysphonic subjects with laryngeal pathology (nodules or polyps), 36 dysphonic subjects without laryngeal pathology, and 86 normal-speaking subjects. The computed s/z ratios were significantly higher for the dysphonic subjects with laryngeal pathology; they found that s/z ratio appears to be an excellent indicator of poor laryngeal function as a result of laryngeal lesions. Omori et al. has showed a good postoperative vocal function with video endoscopic laryngeal surgery they noted prolonged maximum phonation time and improvement in voice quality [6].
Our method is similar to the technique proposed by Omori et al. A two-handed technique can also be performed where the assistant parks the flexible scope at a suitable site and the surgeon uses both hands for operating [6].
Omori et al. has documented in 2000, 114 patients of video assisted laryngeal surgery. They have used flexible video endoscope ENF type 200 with an aspiration channel and flexible video endoscope ENF type 7200 with an aspiration channel and have concluded that this is minimally invasive procedure for benign laryngeal lesions [6]. We have used a chip on tip, PENTAX CP 1000 (3 mm diameter) video Fibreoptic nasopharyngoscope without an aspiration channel, where in the image Quality is even better.
Omori et al. has used specially designed fine tipped cup forceps and scalpels. We have designed cutting edge cup forceps with various angulations and scissors for transoral laryngeal surgery. Vocal fold polyp excision was accomplished by 89% by Omori 6, our results was consistent with Omori et al. Vocal fold polyp excision was accomplished in most of the patients. Out of the 22 selected patients for FLS, 2 were not able to tolerate and the procedure could not be done. Hence the 2 patients were excluded from the study.
Cost analysis between MLS and FLS has shown that FLS is more economical as it is done under local anesthesia and as a day care surgery, whereas MLS done under GA requires at least 1–2 days of hospitalization. However, Maestre et al. conducted a study in which 22 patients underwent MLS in ambulatory setting that is the patients being discharged home the same day. They noted that there was no readmission. They concluded that MLS in selected patients can be safely performed on a day care basis [8]. Kojima et al. have been carrying out Fiberoptic laryngomicrosurgery with a stroboscope under LA as a day care surgery [9].
From our study FLS is the procedure of choice in patients where exposure of the larynx by suspension laryngoscopy was difficult due to trismus, receding lower jaw, short neck, stiff neck, morbid obesity, large tongue and in patients who are medically unfit for GA. A similar study was done in 2000 by Masahiro Kawaida et al., who found significant improvement in MPT following video assisted rigid endoscopic laryngeal surgery in 13 patients with benign laryngeal lesions. They concluded that this surgical method seems to be one of the best possible procedures for treating Dysphonia in cases with difficult laryngeal exposure [10].
Conclusion
Our study shows that when benign vocal cord (VC) pathologies like VC polyp or VC nodules were treated by MLS or FLS the voice Quality improvement remains the same. FLS is the procedure of choice when MLS under general anesthesia is contraindicated.
Funding
None.
Declarations
Conflict of interest
None.
Ethical approval
Obtained
Informed constent
Taken.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Anand Velusamy, Email: anand@entanand.com.
Santosh Sivasamy, Email: drsanthosh.s@gmail.com.
Aishwarya Anand, Email: aishwaryacmc@yahoo.in.
Sridurga Janarthanan, Email: jsdurga2021@gmail.com.
References
- 1.Yanagisawa E, Yanagisawa K. Stroboscopic video laryngoscopy: a comparison of fiberscopic and telescopic documentation. Ann Otol Rhinol Laryngol. 1993;102:255–265. doi: 10.1177/000348949310200403. [DOI] [PubMed] [Google Scholar]
- 2.Zeitels SM. Premalignant epithelium and microinvasive cancer of the vocal fold: the evolution of phonomicrosurgical management. Laryngoscope. 1995;105:1–5. doi: 10.1288/00005537-199503001-00001. [DOI] [PubMed] [Google Scholar]
- 3.Dailey SH, Spanou K, Zeitels SM. The evaluation of benign glottic lesions: rigid telescopic stroboscopy versus suspension microlaryngoscopy. J Voice. 2006;6:1–7. doi: 10.1016/j.jvoice.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Arad-Cohen A, Blitzer A. Office based direct fiberoptic laryngoscopic surgery, operative techniques in otolaryngology. Head Neck Surg. 1998;09(4):238–242. [Google Scholar]
- 5.Gould WJ, Korovin GS. Historical and future perspectives. In: Benninger S, Jacobson B, editors. Vocal arts medicine, the care and prevention of professional voice disorders. 1. New York: Thieme Medical Publishers; 1994. [Google Scholar]
- 6.Omori K, Shinohara K, Tsuji T, Kojima H. Videoendoscopic laryngeal surgery. Ann Otol Rhinol Laryngol. 2000;109:149–155. doi: 10.1177/000348940010900207. [DOI] [PubMed] [Google Scholar]
- 7.Frances C, Boone RD. The S/Z ratio as an indicator of laryngeal pathology. J speech Hear Disorders. 1980;46:147–149. doi: 10.1044/jshd.4602.147. [DOI] [PubMed] [Google Scholar]
- 8.Maestre JM, Morales C, Carrera F, Bezos J, Garcia J, et al. Microlaryngeal surgery on a day case basis. Ambulated Surg ENT J. 1995;3:189–193. doi: 10.1016/0966-6532(95)00034-8. [DOI] [Google Scholar]
- 9.Guo YC, Tai SK, Tsai TL, Huang JL, et al. Removal of unapproachable laryngopharyngeal foreign bodies under flexible videolaryngoscopy. Laryngoscope. 2003;113:1262–65. doi: 10.1097/00005537-200307000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Kawadia M, Fukuda H, Kohno N. Video–assisted rigid endoscopic laryngo surgery: application to cases with difficult laryngeal exposure. J Voice. 2001;15(2):305–12. doi: 10.1016/S0892-1997(01)00032-7. [DOI] [PubMed] [Google Scholar]