Abstract
Background: Plasmacytomas are tumors involving plasma cells that can be either osseous or extraosseous. Solitary extraosseous plasmacytomas are rarely found in the head and neck region. Various pathological, immuno-histochemistry, and radiological investigations must be done to distinguish it from multiple myeloma. Case: A 41-year-old female presented with a progressively increasing mass in right submandibular region for 1 year. She also had complaints of dysphagia and dyspnea for 3 months. Histopathological examinations showed lymphoplasmacytic infiltrate and possibility of plasma cell neoplasm was suspected. On further investigations like immunohistochemistry, bone marrow biopsy, quantitative immunoglobulin, immunoelectrophoresis, and urine analysis, diagnosis of extraosseous plasmacytoma was made. Positron emission tomography-computed tomography (PET-CT) scan did not show any distant foci of the disease. The patient received definitive radiotherapy to the primary region and tolerated well. The patient is asymptomatic after 1 month of radiotherapy and is on regular follow-up. Conclusions: Extraosseous plasmacytoma of the submandibular region is very rare but radiosensitive tumor. Multiple myeloma must be ruled out prior to start of any treatment. Long term follow ups are required to comment on disease progression, dissemination, or recurrence.
Keywords: Extramedullary, Extraosseous, EMP, SEP, Plasmacytoma, Radiotherapy, Submandibular Gland
Introduction
Plasmacytomas are monoclonal differentiation of plasma cells. Solitary Extraosseous plasmacytomas (SEP) occur mainly in the head and neck region (oropharynx, nasopharynx, and paranasal sinus). SEP can occur at rare locations like gastrointestinal tract, skin, lymph nodes, and adrenal glands [1–3]. Involvement of salivary glands by plasmacytoma is very rare. Extraosseous plasmacytoma accounts for 4% of all non-epithelial tumors of the upper respiratory tract [4]. Patients with plasmacytoma tend to convert into multiple myeloma in the future; therefore such patients need regular and long follow up.
Case Report
A 41-year-old female presented with a non-tender right submandibular mass, progressively increasing in size for 1 year. She also had complaints of dysphagia and dyspnea for 3 months. On palpation, a soft to firm, non-tender, diffuse swelling in the right submandibular region was felt which was laterally extending into masticator space and causing a bulge in the tonsillar fossa and soft palate.
Contrast-enhanced magnetic resonance imaging (CEMRI) of the neck showed a large lobulated mass measuring 10.6 cm x 8.6 cm x 9.4 cm, involving right submandibular, parotid, masticator, carotid, and parapharyngeal space with extension into retropharyngeal space, sublingual space causing marked compression of the naso-oro-hypo pharyngeal airway.
Fine needle aspiration cytology (FNAC) showed moderate cellular smears with inflammatory cells, predominantly comprising plasma cells, admixed few lymphocytes, and macrophages. At places, bi-nucleate, tri-nucleate, and quadri-nucleate plasma cells were also seen as suspicious of plasma cell disorder.
The patient then underwent incisional biopsy from right submandibular gland which showed salivary gland tissue comprising of acini, ducts, and fibro-collagenous tissue with lymphoplasmacytic infiltrate along with hemorrhage (Fig. 1). Infiltrate was negative for CD3, CD19, and CD20. Diffuse strong cytoplasmic activity for CD38 and CD138. BCL2 positivity was seen in the mantle zone and interfollicular area, with decreased Kappa and Lambda expression in lymphoplasmacytic, infiltrate suggestive of plasma cell disorder.
Fig. 1.
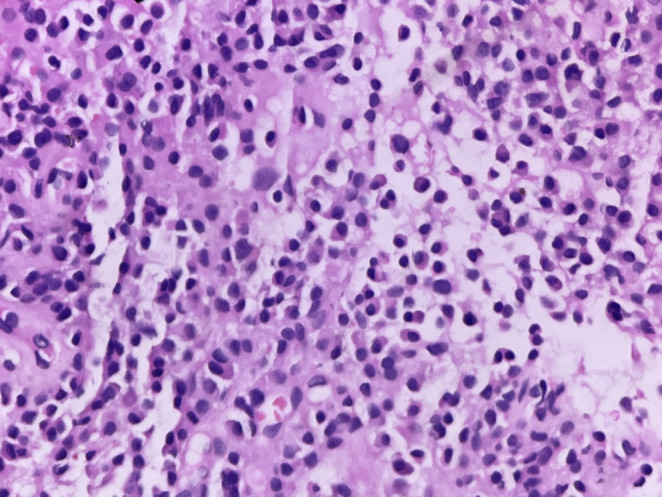
Tumour comprised of diffuse proliferation of plasma cells having eccentrically placed nuclei with paranuclear hoff (H & E, 400 × )
No monoclonal plasma cells were seen on bone marrow biopsy. Other tests like complete blood counts, liver and renal function tests, serum calcium, immunoglobulin, immunoelectrophoresis, and urine analysis for Bence-Jones proteins were done and found to be within normal range.
Positron emission tomography-computed tomography (PET-CT) scan showed FDG avid soft tissue density mass in the right submandibular region with no separate visualization of the right submandibular gland (Fig. 2). The lesion was 9.9 × 7.4 × 8.8 cm, extending to involve the oropharynx and nasopharynx causing near complete obliteration of posterior nasal choana. Laterally the lesion was noted infiltrating into right parotid. No distant foci of the disease were seen. In view of all the above findings, multiple myeloma was excluded and a diagnosis of solitary extraosseous plasmacytoma was made. She underwent an emergency tracheostomy because of progressive dyspnea. The patient was planned for definitive radiotherapy to the primary region. She received a total of 50.4 Gy in 28 fractions of 1.8 Gy, five days a week (Fig. 3). The patient was asymptomatic 1 month after radiotherapy and is on regular follow up.
Fig. 2.
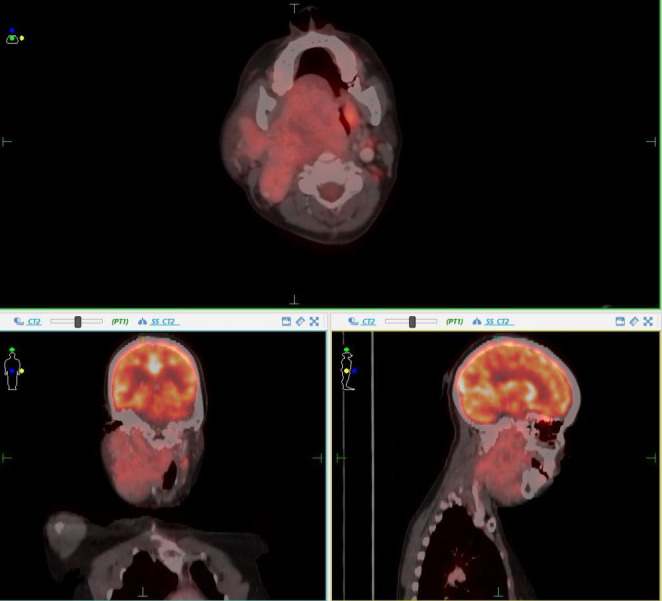
PET-CT image showing tumor extension
Fig. 3.
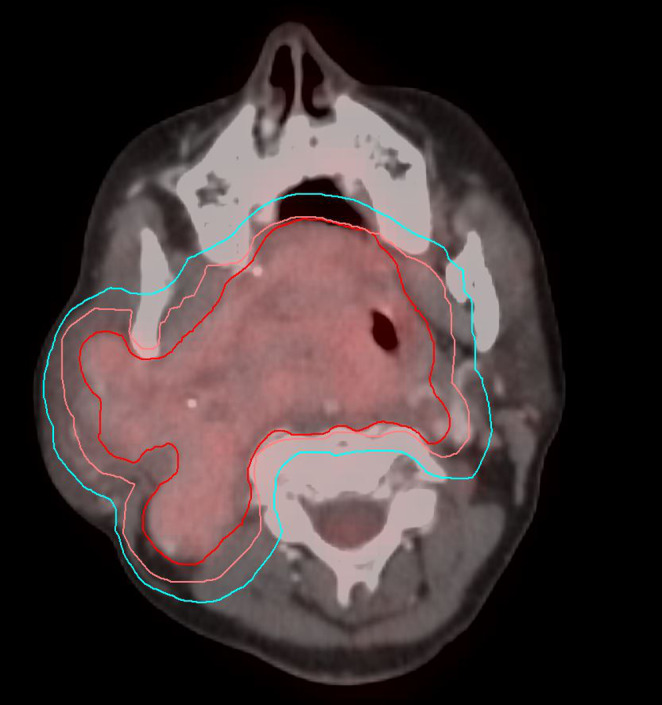
Radiotherapy target volume ( Red = GTV; Orange = CTV; Cyan = PTV)
Discussion
Extraosseous plasmacytoma of the salivary gland are very rare, accounting for less than 1% of all the upper aerodigestive tract plasmacytomas [5]. Majority of cases are reported in the oropharynx, nasopharynx, and paranasal sinusand it affects males more than females. Almost 80% of extraosseous plasmacytoma occur in the upper airway [6, 7].
In a case series by Kapadia et al., 80% patients (n = 20) with SEP head and neck presented with the complaint of a swelling. Other complaints were airway obstruction, epistaxis, localized pain, proptosis, and regional lymphadenopathy [8]. In head and neck extraosseous plasmacytoma the symptoms corresponds to location of primary disease [9]. Diagnosis is confirmed by biopsy of the lesion and it provides sufficient material for detailed immuno-histochemistry. However only histopathological examination cannot distinguish an Extraosseous plasmacytoma from multiple myeloma therefore other investigations like routine blood tests, bone marrow biopsy, serum biochemistry, serum protein, immunoelectrophoresis, and a skeletal survey must be done to exclude the possibility of multiple myeloma. Approximately 40% of SEP presents with lymphadenopathy [10]. A whole-body PET-CT can help with the evaluation of any locoregional or distant spread. Extraosseous plasmacytomas are treated with surgery or radiotherapy or both. Approximately 20–30% of the patients eventually develop multiple myeloma and almost half of them will develop osseous plasmacytoma. SEP may relapse even after complete treatment.
Conclusion
Extraosseous plasmacytoma of the submandibular gland is rare. The clinical presentation mimics multiple myeloma therefore thorough investigations must be done to rule out multiple myelomaprior to start of any treatment. Plasmacytomas are radiosensitive tumor thus can be treated successfully by radiotherapy only. However, long term follow ups are required to comment on its conversion into multiple myeloma, disease progression, dissemination, or recurrence.
Author Contribution
All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Funding
The author declares that no funds, grants, or other support were received during the preparation of this manuscript.
Data Availability
The dataset analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethics statement
This is an observational study and no ethical approval is required.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shiv Shankar Mishra, Email: Drshivmishra11188@gmail.com.
Manish Kumar Ahirwar, Email: manish.ahirwar25@gmail.com.
Siddhartha Nanda, Email: sidnanda@yahoo.com.
References
- 1.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al (2012) “IARC Publications Website - WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues.“ WHO/IARC Classification of Tumours, 4th Edition, Volume 2. IARC Publications; France
- 2.Scholl P, Jafek BW. Extramedullary plasmacytoma of the parotid gland. Ear Nose Throat J. 1986;65:564–567. [PubMed] [Google Scholar]
- 3.Townend PJ, Kraus G, Coyle L, Nevell D, Engelsman A, Sidhu SB. Bilateral extramedullary adrenal plasmacytoma: case report and review of the literature. Int J EndocrOncol. 2017;4:67–73. doi: 10.2217/ije-2016-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fu YS, Perzin KH (1978 Nov) Nonepithelial tumors of the nasal cavity, paranasal sinuses and nasopharynx. A clinicopathologic study. IX Plasmacytomas Cancer 42(5):2399–2406 [DOI] [PubMed]
- 5.Batsakis JG, Medeiros JL, Luna MA, et al. Plasma cell dyscrasias and the head and neck. Ann DiagnPathol. 2002;6:129–140. doi: 10.1053/adpa.2002.33458. [DOI] [PubMed] [Google Scholar]
- 6.Tesei F, Caliceti U, Sorrenti G, Canciulla A, Pileri S, Neri S, et al. Extramedullary plasmacytoma of the head and neck: a series of 22 cases. ActaOtorhinolaryngol Ital. 1995;15:437–442. [PubMed] [Google Scholar]
- 7.Wax MK, Yun KJ, Omar RA. Extramedullary plasmacytoma of the head and neck. Otolaryngol Head Neck Surg. 1993;109:877–885. doi: 10.1177/019459989310900517. [DOI] [PubMed] [Google Scholar]
- 8.Kapadia SB, Desai U, Cheng VS. Extramedullary plasmacytoma of the head and neck. Medicine. 1982;61:317–329. doi: 10.1097/00005792-198209000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Shah C, Roy D, Naronha B (2001 Dec) Extramedullary plasmacytoma of the submandibular gland. J Laryngol Otol 115(12):1023–1025 [DOI] [PubMed]
- 10.Tatsis D, Sotiropoulos D, Baliaka A, Kalaitsidou I (2021 Mar) Solitary extramedullary plasmacytoma of the parotid gland in a patient with mixed connective tissue disease. J Oral MaxillofacPathol 25(Suppl 1):S18–S21 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analysed during the current study are available from the corresponding author on reasonable request.


