Abstract
Foreign body aspiration is potentially life-threatening in paediatric age group. Early recognition and emergency intervention by Rigid bronchoscopy is life-saving. To highlight various difficulties in emergency paediatric bronchoscopy and discuss our experience in 138 patients. < 12 years children with suspected foreign body aspiration were included. Data of 138 patients < 12 years of age were studied. The most common foreign body found was peanut and organic foreign bodies constituted of total foreign bodies removed. Choking, Cough and sudden onset breathlessness were common symptoms. Tachypnoea, asymmetric breath sound, rhonchi, stridor, reduced chest movements were common signs. Obstructive emphysema was commonest radiological findings. Majority of the patients were discharged within 72 h & only two patients expired. History, clinical and radiological findings are highly indicative of foreign body in the airway. Inspite of being a high risk procedure, Rigid bronchoscopy when performed with necessary expertise,trained anaesthesia team and a paediatric ICU, saves majority of lives of children with tracheobronchial foreign bodies.
Keywords: Airway obstruction, Bronchscopy, Choking
Introduction
Foreign body aspiration is an important cause of morbidity and death in paediatric population, although mortality is low if the child reaches medical care early. Presenting symptoms of an inhaled foreign body depends on time since aspiration. Immediately after inhalation the child starts to cough, wheeze or have laboured breathing. If early signs are missed, the child usually presents with fever and other signs and symptoms of chest infection.
Foreign body aspiration is more prevalent in paediatric age group compared to adults with peak incidence occurring between 1 and 3 years of age [1]. Without early treatment it is a cause of morbidity in children, sometimes resulting in a fatal outcome. Children have a tendency to explore the environment by placing objects in the mouth, moreover they lack molars necessary for proper grinding of food and coordinated swallowing, laryngeal elevation and glottic closure is still immature. [2].
The gold standard for diagnosis and management of foreign body aspiration is a rigid open tube bronchoscopy. The rigid bronchoscope is preferred by many [3, 4] for safety reason, speed of action, surgeons comfort. Basically the wide channel rigid bronchoscope allows direct access for foreign body retrieval while adequately ventilating the patient, along with effective suction.
But Rigid bronchoscopy is a potentially hazardous technique [3, 5, 6] and chances of complications is inversely proportional to the experience and expertise of surgical team.
So if any child presents with a history Suggestive or suspicious of any foreign body aspiration coupled with clinical and/or radiographic features of tracheo-bronchial foreign body it is considered an emergency and to be intervened immediately.
In the present study we share our experience in evaluation and management of children with foreign body aspiration.
Materials and Methods
The present study was conducted in the Institute of Otorhinolaryngology And Head neck surgery at IPGMER & SSKM hospital, Kolkata, India, for a period of 18 months from October 2018 to March 2020. Children up to 12 years of age attending ENT and Paediatric OPD and emergency were included in the study.
Inclusion criteria:
Children (12 years or less) With definite history of foreign body aspiration
History of choking with sudden onset in an otherwise healthy child
Children with recurrent Lower respiratory tract infection (LRTI) or chronic cough with suspicion of tracheobronchial foreign body
Exclusion criteria:
Children with diagnosed bronchial asthma, acute Laryngotracheobronchitis, bronchiolitis, bronchiectasis.
The evaluation of the patient was based on clinical history, through examination and radiological assessment. CT scan of thorax/Virtual CT bronchoscopy were done in those cases where the condition of the patient was stable and chest x-ray was not providing sufficient information. And informed written consent was taken from parents of the children in every case explaining necessity and risks involved with the procedure and chances of different complications and possible outcomes. Oxygen saturation (SpO2) was noted in every case.
Results and Statistical Analysis
Among the total 138 patients we studied majority of the patients were male (71.01%, n = 98) And M:F ratio stands at 2.45:1. The commonest age group affected was between 1 and 3 years (53.62%, n = 74). 13.77% (n = 19) Were less than one year of age and 25.36% (n = 35) belonged to 4–6 years of age group. So overall 92.75% (n = 128) were under six years of age.
The time lapse between aspiration of foreign body and attending our health facility, was found that only 21.01% (n = 29) patients came within 24 h of aspiration. Majority 38.41%, (n = 53) came between day 2 and day 3 after aspiration. 18.84% (n = 26) attended our hospital between day 4 and day 7 after aspiration. 10.87% (n = 15) patients attended our hospital after one week but before one month since aspiration. 10.87% (n = 15) patients attended our hospital after more than one month after aspiration.
When history was taken from parents 73.19% (n = 101) gave history of choking and 50% (n = 69) gave a definite history of foreign body aspiration. The common presenting symptoms were Cough (91.30%, n = 126), breathlessness (76.09% n = 105), Wheeze (35.51%, n = 49), Fever was present in (16.67%, n = 23) patients. On clinical examination patients had tachypnoea (81.16% n = 112), asymmetric breath sound (65.22%, n = 90), rhonchi (45.65%, n = 63), reduced chest movements (40.56% n = 56), stridor (36.23% n = 50), intercostal retraction (14.49% n = 20), tracheal tug (13.77%, n = 19), recurrent lower respiratory tract infections (10.14%, n = 14), persistent cough (9.42%,n = 13) And cyanosis (5.80%, n = 8) in decreasing order of frequency. 13.77% (n = 19) patients had no clinical signs at presentation. (Table 1).
Table 1.
Clinics
| History | n (%) |
| Choking | 101 (73.19) |
| Foreign body aspiration | 69 (50) |
| Symptoms | n (%) |
| Cough | 126 (91.3) |
| Breathlessness | 105 (76.09) |
| Wheeze | 49 (35.51) |
| Fever | 23 (16.67) |
| Signs | n (%) |
| Tachypnoea | 112 (81.16) |
| Asymmetric breath sounds | 90 (65.22) |
| Rhonchi | 63 (45.65) |
| Reduced chest movements | 56 (40.56) |
| Stridor | 50 (36.23) |
| Intercostal retraction | 20 (14.49) |
| Tracheal tug | 19 (13.77) |
| Recurrent LRTI | 14 (10.14) |
| Persistent cough | 13 (9.42) |
| Cyanosis | 8 (5.80) |
| No signs | 19 (13.77) |
Chest x-ray, posteroanterior and lateral views were obtained in every case. Normal chest x-ray was found in 31.16% (n = 43) cases and radioopaque foreign bodies were found in 15.22% (n = 21) cases. Obstructive emphysema with or without atelectasis lobar or whole lung was most common radiological finding in the study 39.13% (n = 54). Among other radiological findings, mediastinal shift (12.32%, n = 17), pneumothorax (1.45%, n = 2) and subcutaneous emphysema (0.72%, n = 1) were detected. (Table 2/Fig. 1).
Table2.
Radiological findings
| Chest X-Ray | n (%) |
|---|---|
| Normal | 43 (31.16) |
| Obstructive emphysema | 31 (22.46) |
| Radio opaque foreign body | 21 (15.22) |
| Mediastinal shift | 17 (12.32) |
| Obstructive emphysema with lobar atelectasis | 14 (10.14) |
| Obstructive emphysema with whole lung atelectasis | 9 (6.52) |
| Pneumothorax | 2 (1.45) |
| Subcutaneous emphysema | 1 (0.72) |
Fig. 1.
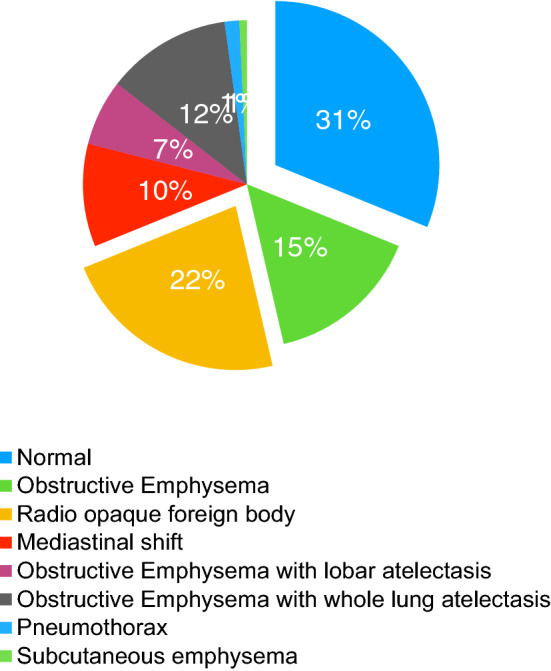
X-ray findings in the patients who underwent bronchoscopy for foreign body aspiration
Rigid bronchoscopy was done in all the cases. Additional tracheostomy was done in 11.59% (n = 16) cases in various circumstances. Large foreign bodies which could not be extracted through the glottis were delivered by tracheotomy in 2.9% cases (Fig. 2, 3, 4, 5, 6).
Fig. 2.

Instruments: flexible fibre optic bronchoscope, rigid bronchoscope, bronchoscopy forceps, suction cannulae, telescope and telescope forceps
Fig. 3.
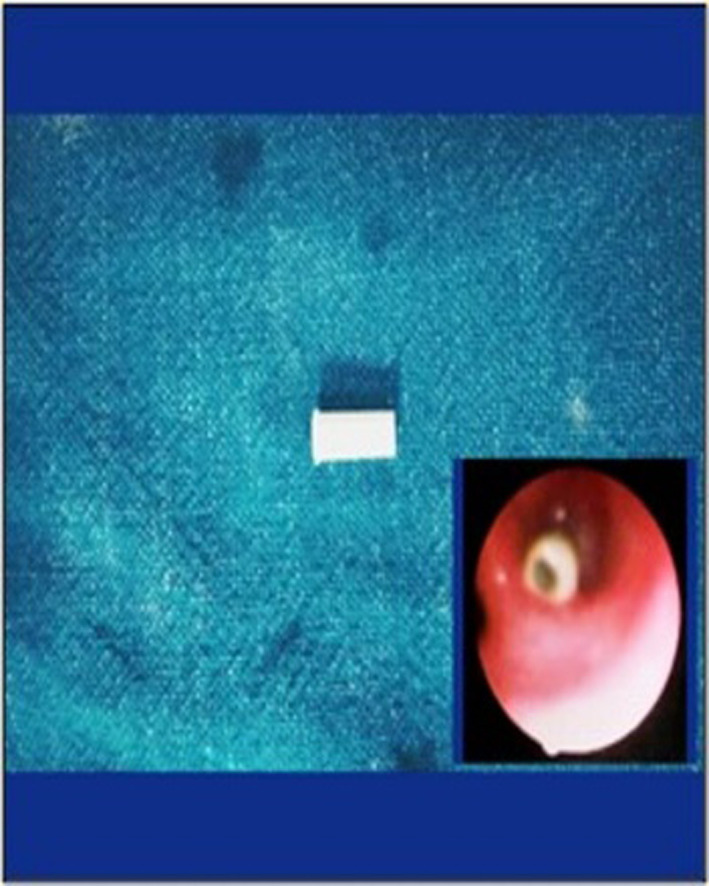
Whistle removed from bronchus
Fig. 4.

X-ray and Foreign Body picture after removal: (Top left to bottom left) peanut, whistle, shrimp and (Top right to bottom right) LED bulb, needle and broken safety pin
Fig. 5.
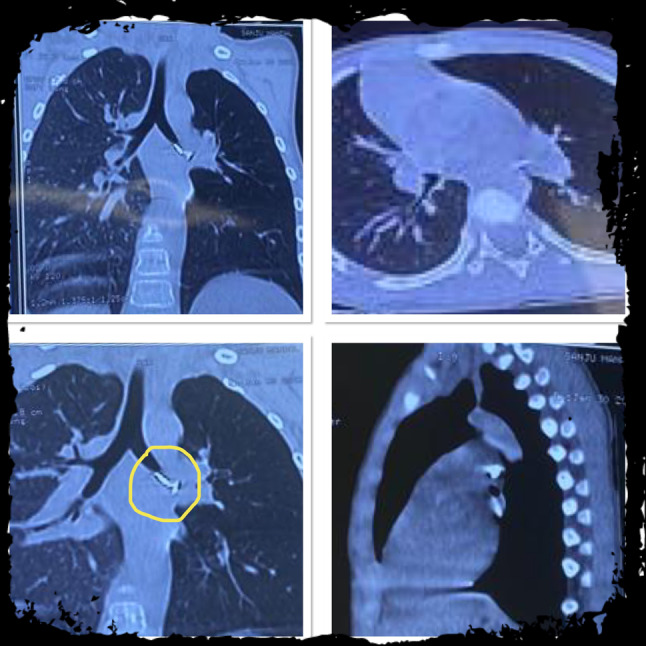
Left main bronchus metallic Foreign Body (nail) seen on a CT scan of thorax
Fig. 6.
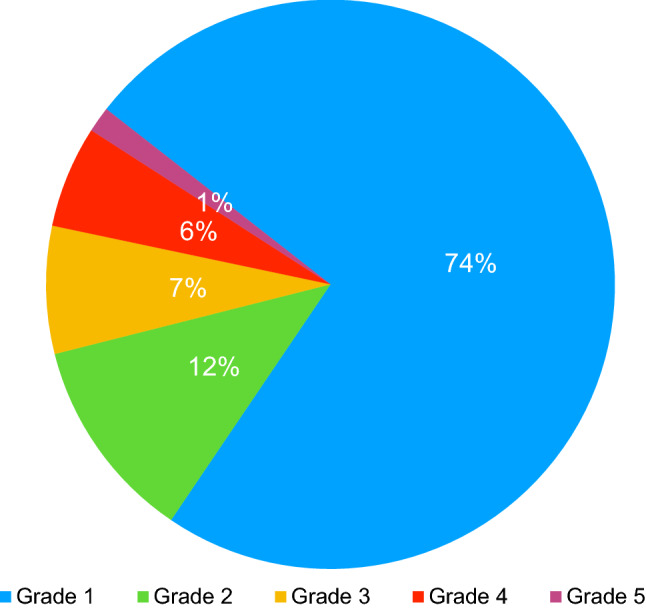
Ghosh and Kumar Grades of bronchoscopy field visibility
No foreign body was found in 8.7% (n = 12) cases. Right bronchus was the commonest site of enlodgement 47.62%, n = 60. Following left bronchus 26.98%, n = 34, trachea 23.81%, n = 30 and sub-glottis 1.59%, n = 2.
Among the foreign bodies recovered, 74.61% (n = 94) were organic and 25.39%, n = 32 were in organic. Peanuts and chickpeas were the most common 26.98%, n = 34 and 21.43%, n = 27 respectively. Among other inorganic foreign bodies were Watermelon seeds (5.57%), Tamarind seed (3.97%), papaya seed (1.59%), aspirated food materials (10.32%), fishbone (2.38%), chicken bone (1.59%) and shrimp (0.79%) (Fig. 3). Among the inorganic foreign bodies different metallic objects (9.52%), plastic toy whistle 8.73% (Fig. 2), plastic pen cap (3.97%), LED bulb (2.38%) and watch battery (0.79%) were found (Table 3).
Table 3.
Types of Foreign bodies retrieved after bronchoscopy
| Types of foreign body | n (%) | |
|---|---|---|
| Peanut | 34 (26.98) | |
| Chickpeas | 27 (21.43) | |
| Watermelon seed | 7 (5.56) | |
| Organic (n = 94,74.64%) | Tamarind seed | 5 (3.97) |
| Papaya seed | 2 (1.59) | |
| Aspirated food material | 13 (10.32) | |
| Fish bone | 3 (2.38) | |
| Chicken bone | 2 (1.59) | |
| Shrimp | 1 (0.79) | |
| Metallic object | 12 (9.52) | |
| Plastic toy whistle | 11 (8.73) | |
| Inorganic (n = 32,25.39%) | Plastic pen cap | 5 (3.97) |
| LED bulb | 3 (2.38) | |
| Watch battery | 1 (0.79) | |
| Total | 125 (100) |
Different complications encountered in Perioperative period are listed in Table 4. Mortality occurred in two cases; One by corrosive injury causing tracheal perforation in a case of a watch battery and enlodgement in the trachea and another case was a swollen peanut stuck at the carina occluding the airway.
Table 4.
Complication encountered after Rigid bronchoscopy
| Complications | n (%) |
|---|---|
| Hypoxaemia (SPO2 < 95%) | 112 (81.16) |
| Minor lip injury | 7 (5.07) |
| Broken deciduous teeth | 5 (3.62) |
| Tracheal perforation | 1 (0.72) |
| Peroperative tracheobronchial haemorrhage | 36 (26.09) |
| Transient respiratory failure | 12 (8.7) |
| Peroperative arrhythmia | 4 (2.9) |
| Pulmonary oedema | 5 (3.62) |
| Laryngobronchospasm | 2 (1.45) |
| Convulsion | 2 (1.45) |
| Post operative cough | 84 (60.87) |
| Pneumonia | 19 (13.77) |
| Pneumothorax | 1 (0.72) |
| Subcutaneous emphysema | 1 (0.72) |
| Death | 2 (1.45) |
We encountered Tracheobronchial haemorrhage in 26.09% (n = 36) cases. And according to our bronchoscopy field visibility grading system,amongst the 36 cases we encountered grade 2 (44.44%, n = 16), grade 3 (27.78%, n = 10), grade 4 (22.22% n = 8) and grade 5 (5.55%, n = 2) field visibility. Rest 73.91% (n = 102) cases were a grade 1. (Table 5/Fig. 6).
Table 5.
Ghosh & Kumar grading system for rigid bronchoscopy field visibility
| Grade of field visibility | Degree of haemorrhage | Number of suctioning required in case of haemorrhage | Foreign body/lesion localisation |
|---|---|---|---|
| 1 | Nil | 0 | A (excellent) |
| 2 | Minimal | 0 | B (very good) |
| 3 | Mild | 1–5 | C (good) |
| 4 | Moderate | 6–10 | D (Fair) |
| 5 | Moderately severe | 11–15 | E (poor) |
| 6 | Severe | > 15 | F (not visible) |
During post operative recovery phase 70.29% (n = 97) and 16.67% (n = 23) patients were observed at general ward and at paediatric ICU after extubation respectively. Rest 13.04% (n = 18) patients were managed at paediatric ICU and kept on ventilation and extubated later. 70.29% (n = 97) patients were discharged after 48 h. Rest were discharged after 72 h (15.94%, n = 22), between 4 and 7 days (8.70%, n = 12) and after 7 days (3.62%, n = 5).
Discussion
Upper airway obstruction due to foreign body aspiration is one of the common causes of paediatric airway emergency which necessitates emergency intervention by rigid bronchoscopies.
In our study male–female ratio was 2.45:1. In different studies male:female ratio varies between 1.5 and 4.5:1 [7–10]. Approximately 2/3rd, 67.39% cases occurred in under 3yrs of age which is consistent with different studies [7, 9, 10]. Occurrence in this age group is common because the childrens innate tendency to learn and explore their world by putting everything at hand in their mouth. Moreover their chewing and swallowing functions are yet to develop fully.
Signs and symptoms of foreign body aspiration occur in three stages:
Acute stage–occurs due to sudden airway obstruction, lasting for few seconds to several minutes manifested by choking, coughing, breathlessness.
Quiescent stage–each follows the acute stage and in this stage patient is asymptomatic.
Late stage–it is when symptoms of infection develop.
The clinical presentation depends on the age of the child, what object was aspirated, when it was aspirated, and where it was enlodged. 21.01% children came to our hospital within 24 h of foreign body aspiration and 78.26% within seven days. While recovering history from the parents, history of choking was found to be encountered in 73.19 and in 50% (n = 69) cases there were definite history of foreign body aspiration. In literature, history of choking was as high as around 90% [11, 12]. The most common symptoms of foreign body aspiration encountered was coughing (91.3%), breathlessness (76.09%) and wheeze (35.5%) which are at par with various studies [8, 13, 14]. Fever occurred less frequently in 16.67% and particularly in long-standing cases.
Physical signs of a study showed on clinical examination patients had tachypnoea (81.16%), asymmetric breath sound (65.22%), rhonchi (45.65%), reduced chest movements (40.56%), stridor (36.23%), intercostal retraction (14.49%), tracheal tug (13.77%), recurrent lower respiratory tract infections (10.14%), persistent cough (9.42%) And cyanosis (5.80%) in decreasing order of frequency. 13.77% (n = 19) patients had no clinical signs at presentation. These findings were in agreement with many other studies [15–17].
X-ray chest and neck or most important initial radiological investigations as it can be done easily and quickly in patients with suspected foreign body aspiration [18]. We did both posteroanterior and lateral radiographs and Normal chest x-ray was found in 31.16%, n = 43 cases and Radio opaque foreign bodies were found in 15.22%, n = 21 cases.In different studies radio opaque foreign bodies were found in 10–20% cases [19, 20]. Chest x-rays were abnormal in 40–80% cases in different studies [13, 19, 18]. Obstructive emphysema with or without atelectasis (lobar or whole lung) was most common radiological finding in the study (39.13% n = 54) followed by mediastinal shift (12.32%) which is coherent with previous studies [13, 21, 22]. Less common findings were aeration within areas of atelectasis (3.62%) suggesting incomplete consolidation, pneumothorax (1.45%), subcutaneous emphysema (0.72%). Chest x-ray alone is not reliable to diagnose tracheobronchial foreign bodies and CT scan of thorax should be done if the child is stable to detect radiolucent foreign bodies.
Rigid bronchoscopies under GA is regarded as a gold standard procedure for removal of aspirated foreign bodies [23–26]. This procedure allows direct visualisation of airway and localisation of foreign bodies, maintain good control of airway [27], controlled manipulation of foreign body with a variety of forceps and minimal morbidity and mortality in trained hands. In our study we performed rigid bronchoscopies in all 138 cases; additionally tracheotomy was done in 2.90% (n = 4) cases and tracheostomy in 11.59% cases, as some foreign bodies were large, could not be removed through the glottis [28–30]. Tracheostomy was done when children presented with cyanosis and serious stridor at Emergency before performing Rigid bronchoscopies and in cases to post operatively temporary tracheostomy was done at paediatric ICU when those children required prolonged ventilation (> 7 days). Another 6cases required peroperative tracheotomy due to decreased saturation level, due to bronchial oedema. Distribution of location of foreign body lodgement showed right bronchus as the commonest site in 47.62% cases followed by the left bronchus and trachea at 26.98 and 23.81% respectively. In two cases foreign body found trapped at subglottis and in both cases the child presented with severe stridor and cyanosis. The higher incidence of foreign body in right bronchus compared to left, is due to less angulation and more aligned to the trachea compared to the left [31–33]. In our study there were 8.70% negative bronchoscopies, where no foreign body was found. In different series it varied between 3.8 and 16% [10, 15, 26]. Bronchoscopies should be performed in all cases with history of choking [34] crisis, aptly named “penetration syndrome” [35, 36].
Among the foreign bodies recovered, 74.61% were organic and 25.39% were in organic. Peanuts and chickpeas were the most common 26.98 and 21.43% respectively. Among other inorganic foreign bodies Watermelon seeds (5.57%,) Tamarind seed (3.97%), papaya seed (1.59%), aspirated food materials (10.32%), fishbone (2.38%), chicken bone (1.59%) and shrimp (0.79%). One interesting case we encountered was a shrimp inside the trachea (Fig. 3). In various studies peanuts aspiration were found to be the most common 22–55% [8, 9, 13, 37].
Aspiration of inorganic or non-food foreign bodies were more common in older children [38]. Inorganic foreign bodies were recovered in 25.46% cases. Among the inorganic foreign bodies different metallic objects (9.52%), plastic toy whistle (8.73%), plastic pen cap (3.97%), LED bulb (2.38%) and watch battery (0.79%) were found.
In minimising complication, experience and technical expertise of the Surgeon, synergy with the anaesthesia team and proper instrumentation play crucial role. There are series’ [39] that showed complications associated with tracheobronchial foreign body removal by bronchoscopy and fatalities are also described in literature. The unexpected and unknown nature of foreign body and local mucosal response to it influences the incidence of complications.When patients came to our emergency we performed pulse oximetry in each patient and found hypoxaemia (SpO2 < 95%) in 81.16% cases and tachypnoea was found to be a good clinical indicator of hypoxaemia.
During introduction of rigid bronchoscope minor lip injury (5.07%) and broken deciduous teeth (3.62%) occurred. Posterior tracheal wall laceration or bronchial perforation did not occur in our series though in one case trachea was found perforated by alkali burn by watch battery aspiration. We encountered tracheobronchial haemorrhage during the procedure in 36 cases (26.09%) and according to our field visibility grading System, out of the 36 cases, grade II was found in (44.44%), grade 3(27.78%), grade 4 (22.22%) and grade 5(5.55%). Rest were Grade 1(74%). Haemorrhage depends on size and shape of foreign bodies, longer duration of infection, local tissue reaction, oedema, granulation tissue formation to foreign body and instrumentation by the surgeon. A good Anaesthesia team with expertise in managing paediatric emergency in is very important as Anesthesia could cause problems [40–42]. In our study we encountered some pre-operative problems such as a transient respiratory failure (8.70%, n = 12), arrhythmia (2.90%, n = 4) laryngobronchospasm (1.45%, n = 2) which were managed successfully. PostObstructive pulmonary oedema a potentially fatal complication was found in (3.62%, n = 5), detected clinically by pink frothy secretion from the lungs and later correlated with chest x-ray. Convulsions precipitated by cerebral hypoxia occurred in (1.45%, n = 2) and associated with mortality. The idea of anaesthesia for rigid bronchoscopies should provide rapid induction, minimal haemodynamic instability, adequate ventilation, smooth recovery and minimal post-operative complications [40, 43]. In post-operative recovery phase mild to moderate cough was a common finding (60.87%, n = 84) and managed well with antibiotics, steroids and nebulisation with bronchodilators. Pneumonia found in (13.77%, n = 19) cases and was particularly common with organic foreign bodies stuck for long durations. One patient developed pneumothorax and later subcutaneous emphysema following tracheal perforation. Mortality occurred in two cases (1.45%), in our series. Among them one case attended our emergency with cyanosis and severe stridor, prompt rigid bronchoscopy revealed a swollen peanut impacted at the carina obstructing both bronchi. That patient developed a hypoxic ischaemic encephalopathy and later expired at the paediatric ICU.The other patient came with aspirated alkaline watch battery which perforated trachea and resultant pneumothorax, subcutaneous emphysema, mediastinitis had developed and succumbed to injury at paediatric ICU. In various studies mortality rate varies between 0.21% and 7.8% [44–49]. And some studies claimed no mortality [50]. A delayed diagnosis increased morbidity and chance of mortality. Diagnosis may be delayed in absence of a clear clinical history, negligence of parents or miss diagnosis by the physician [13].
Paediatric rigid bronchoscopy must be done with paediatric ICU back up. 13.04%, (n = 18) cases of a series developed complications and were kept in the paediatric ICU under ventilation for variable periods depending on the severity. Total 29.71%, (n = 41) patients needed post-operative transfer to paediatric ICU.Those children who smoothly recovered from general anaesthesia and maintained saturation of greater than 95% without oxygen support were sent to the General ENT ward and monitored closely with pulse oximetry for 24 h 70.29%, (n = 97). Majority of our patients (70.29%) were discharged after 48 h and 94.93%, (n = 131) were fully recovered and discharged within seven days. Prolonged hospital stay maybe required to treat long infections in cases of longer duration of foreign body entrapment or if there is any complications [17, 51].
To prevent occurrence guidance to be provided to parents and caregivers when child attains six months of age [52].Parents and caregivers are advised not to offer any chewable food, items until the child develops proper chewing functions and to feed their child in sitting posture. Child should be encouraged to sit calmly during eating. Any small objects can become aero-digestive tract foreign body in children and these should be kept out of reach of children.
Conclusion
Tracheobronchial foreign body aspiration in children is an acute airway emergency. It most commonly affects under 3 year children with incidence of male preponderance.
Foreign body aspiration may present as symptomatic or asymptomatic cases and also with or without any positive history of aspiration. So high index of suspicion by the surgeon is essential.
History of choking, diagnostic symptom triad of sudden onset cough,breathlessness and wheeze and reduced air entry on the affected side on auscultation clinches the diagnosis in most of the cases.
Chest x-rays in posteroanterior and lateral view may show a radioopaque foreign body, obstructive emphysema, atelectasis, mediastinal shift, pneumothorax etc. in tracheobronchial foreign body aspiration. But a normal chest x-ray does not exclude presence of tracheobronchial foreign body.
Rigid bronchoscopy is gold standard instrumentation for removal of tracheobronchial– bronchial foreign bodies and it should be performed on emergency basis in any children with clinical or radiological evidence or any suspicion of foreign body aspiration.
Educating and guiding parents and caregivers can minimise occurrence of foreign body aspiration.
Funding
Non-Funded work with no conflict of interest.
Declarations
Conflict of interest
There are no conflicts of interest.
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of relevant national and institutional guidelines and with the Helsinki Declaration of 1975, as revised in 2008.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Debasish Ghosh, Email: debasishghoshsskm@gmail.com.
Ritabrata Mitra, Email: dr.r.mitra.chest@gmail.com.
Sripurna Mondal, Email: sripurna.mandal@gmail.com.
Soutrik Kumar, Email: dr.soutrikkumar@gmail.com.
Arunabha Sengupta, Email: arunabhasengupta2008@gmail.com.
References
- 1.Watkinson JC, Clarke RW (eds), Scott-Brown’s otorhinolaryngology head & neck surgery. 8th Ed. Vol 1. chapter 34. p 364; CRC press, Taylor & Francis Group, Boca Raton, US
- 2.McGuirt WF, Holmes KD, Feehs R, Browne JD. Affiliation. Tracheobronchial foreign bodies. Laryngoscope. 1988;98(6 Pt 1):615–618. doi: 10.1288/00005537-198806000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Beamis JF, Mathur P, Mehta AC McGraw Hill, New York 1999:17–28. Interventional pulmonary medicine (Lung Biology in Health and Disease Book 189)
- 4.Turner JF, Ernst A, Becker HD. Rigid bronchoscopy: how I do it. J Bronchol. 2000;7(2):171–176. doi: 10.1097/00128594-200007020-00015. [DOI] [Google Scholar]
- 5.Elias J, Fishman J, Pack A, Senior R, Kotloff R. Fishman’s pulmonary diseases and disorders by michael grippi. New York: McGraw Hill; 1997. pp. 589–602. [Google Scholar]
- 6.Ramon P, Brichet A. Complications of interventional bronchoscopy. Rev Mal. 1999;16:693–698. [PubMed] [Google Scholar]
- 7.Rothmann BF, Boeckman CR. Foreign bodies in the larynx and tracheobronchial tree in children. Ann Otol Rhinol Laryngol. 1980;89(51):434–436. doi: 10.1177/000348948008900512. [DOI] [PubMed] [Google Scholar]
- 8.Zahran M, Youssef A. The role of rigid bronchoscopy in pediatric foreign body aspiration. Egyptian J Otolaryngol. 2019;35(2):213–218. doi: 10.4103/ejo.ejo_61_18. [DOI] [Google Scholar]
- 9.Sinha V, Gurnani D, Barot DA. A study of applications of rigid bronchoscopy in pediatric patients. Indian J Otolaryngol Head Neck Surg. 2014;66(2):142–144. doi: 10.21037/jtd.2016.11.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naragund AI, Mudhol RS, Harugop AS, Patil PH, Hajare PS, Metgudmath VV. Tracheo-bronchial foreign body aspiration in children: a one year descriptive study. Indian J Otolaryngol Head Neck Surg. 2011;66(Suppl.1):180–185. doi: 10.1007/s12070-011-0416-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cramer N, Jabbour N, Tavarez MM et al. (2018) Foreign body aspiration. Review from Stat Pearls publishing, Treasure Island (FL). PMID 30285375 [PubMed]
- 12.Sehgal A, Singh V, Chandra J, Mathur NN. Foreign body aspiration. Indian Paediatrics. 2002;39:1006–1016. [PubMed] [Google Scholar]
- 13.Tan HK, Brown K, McGill T, Kenna MA, Lund DP, Healy GB. Airway foreign bodies (FB): A 10-year review. Int J Paediatr Otorhinolaryngol. 2000;56(2):91–99. doi: 10.1016/S0165-5876(00)00324-4. [DOI] [PubMed] [Google Scholar]
- 14.Even L, Heno N, Talmon Y, Samet E, Zonis Z, Kugelman A. Diagnostic evaluation of foreign body aspiration in children: a prospective study. J Paediatr Surg. 2005;40(7):1122–1127. doi: 10.1016/j.jpedsurg.2005.03.049. [DOI] [PubMed] [Google Scholar]
- 15.Mallick MS. Tracheobronchial foreign body aspiration in children: a continuing diagnostic challenge. Afr J Paediatr Surg. 2014;11(3):225–228. doi: 10.4103/0189-6725.137330. [DOI] [PubMed] [Google Scholar]
- 16.Soysal O, Kuzucu A, Ulutas H. Tracheobronchial foreign body aspiration: a continuing challenge. Otolaryngol Head Neck Surg. 2006;135(2):223–226. doi: 10.1016/j.otohns.2005.09.035. [DOI] [PubMed] [Google Scholar]
- 17.Zerella JT, Dimler M, McGill LC, et al. Foreign body aspiration in children: value of radiography and complications of bronchoscopy. J Paediatr Surg. 1998;33(11):1651–1654. doi: 10.1016/s0022-3468(98)90601-7. [DOI] [PubMed] [Google Scholar]
- 18.Svedstrom E, Puhakka H, Kero P. How accurate is chest radiography in the diagnosis of tracheo-bronchial foreign bodies in children? Pediatr Radiol. 1989;19:520–522. doi: 10.1007/BF02389562. [DOI] [PubMed] [Google Scholar]
- 19.Mu L, He P, Sun D. Inhalation of foreign bodies in Chinese children: a review of 400 cases. Laryngoscope. 1991;101(6):657–660. doi: 10.1288/00005537-199106000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Tokar B, Ozkan R, Ilhan H. Tracheobronchial foreign bodies in children: importance of accurate history and plain chest radiography in delayed presentation. Clin Radiol. 2004;59(7):609–615. doi: 10.1016/j.crad.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 21.Rovin JD, Rodgers BM. Pediatric foreign body aspiration. Pediatr Rev. 2000;21(3):86–90. doi: 10.1542/pir.21-3-86. [DOI] [PubMed] [Google Scholar]
- 22.Paşaoğlu I, Doğan R, Demircin M, Hatipoğlu A, Bozer AY. Bronchoscopic removal of foreign bodies in children: retrospective analysis of 822 cases. Thoracic Cardiac Surg. 1991;39(2):95–98. doi: 10.1055/s-2007-1013940. [DOI] [PubMed] [Google Scholar]
- 23.Yadav SP, Singh J, Aggarwal N, Goel A. Airway foreign bodies in children: experience of 132 cases. Singapore Med J. 2007;48(9):850–853. [PubMed] [Google Scholar]
- 24.Cotton E, Yasuda K. Foreign body aspiration. Paediatr Clin North Am. 1984;31(4):937–941. doi: 10.1016/s0031-3955(16)34655-7. [DOI] [PubMed] [Google Scholar]
- 25.Oğuzkaya F, Akçali Y, Kahraman C, Bilgin M, Sahin A. Tracheobronchial foreign body aspirations in childhood: a 10-year experience. Eur J Cardiothoracic Surg. 1998;14(4):388–392. doi: 10.1016/s1010-7940(98)00205-x. [DOI] [PubMed] [Google Scholar]
- 26.Hasdiraz L, Oguzkaya F, Bilgin M, Bicer C. Complications of bronchoscopy for foreign body removal: experience in 1,035 cases. Ann Saudi Med. 2006;26(4):283–287. doi: 10.5144/0256-4947.2006.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banerjee A, Rao KS, Khanna SK, Narayanan PS, Gupta BK, Sekar JC. Laryngo-tracheo-bronchial foreign bodies in children. J Laryngol Otol. 1988;102(11):1029–1032. doi: 10.1017/s0022215100107170. [DOI] [PubMed] [Google Scholar]
- 28.Ülkü R, et al. The value of open surgical approaches for aspirated pen caps. J Paediatr Surg. 2005;40(11):1780–1783. doi: 10.1016/j.jpedsurg.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 29.Marks SC, et al. Indications for open surgical removal of airway foreign bodies. Ann Otol Rhinol Laryngol. 1993;102(9):690–694. doi: 10.1177/000348949310200908. [DOI] [PubMed] [Google Scholar]
- 30.Yang X, Ni X, Guo Y, Zhang J. Combined low tracheotomy and rigid bronchoscopy to remove an irregular tracheal foreign body. Paediatric Invest. 2018;2(3):196–197. doi: 10.1002/ped4.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bittencourt PFS, Camargos PAM. Foreign body aspiration: clinical, radiological findings and factors associated with its late removal. Int J Paediatr Otorhinolaryngol. 2006;70(5):879–884. doi: 10.1016/j.ijporl.2005.09.024. [DOI] [PubMed] [Google Scholar]
- 32.Girardi G, Contador AM, Castro-Rodriguez JA. Two new radiological findings to improve the diagnosis of bronchial foreign-body aspiration in children. Pediatr Pulmonol. 2004;38(3):261–264. doi: 10.1002/ppul.20065. [DOI] [PubMed] [Google Scholar]
- 33.Hua H, Na L, Zhijun CJ, Fugao ZG, Yan S, Niankai ZK, et al. Therapeutic experience from 1428 patients with pediatric tracheobronchial foreign body. J Paediatr Surg. 2008;43(4):718–721. doi: 10.1016/j.jpedsurg.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 34.Barrios Fontoba JE, Gutierrez C, Lluna J, Vila JJ, Poquet J, Ruiz-Company S. Bronchial foreign body: should bronchoscopy be performed in all patients with a choking crisis? Pediatr Surg Int. 1997;12:118–120. doi: 10.1007/BF01349976. [DOI] [PubMed] [Google Scholar]
- 35.Baharloo F, Veyckemans F, Francis C, Biettlot M-P, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999;115(5):1357–1362. doi: 10.1378/chest.115.5.1357. [DOI] [PubMed] [Google Scholar]
- 36.Hoeve LJ, Rombout J, Pot DJ. Foreign body aspiration in children. The diagnostic value of signs, symptoms and pre-operative examination. Clin Otolaryngol Allied Sci. 1993;18(1):55–57. doi: 10.1111/j.1365-2273.1993.tb00810.x. [DOI] [PubMed] [Google Scholar]
- 37.Fazal-I-Wahid N, Ur-Rehman H, Amin G, Ahmad I. Rigid Bronchoscopy for extraction of foreign bodies tracheobronchial tree: an experience of 232 cases. JPMI. 2011;25(2):152–157. [Google Scholar]
- 38.Lemberg PS, Darrow DH, Hollinger LD. Aerodigestive tract foreign bodies in the older child and adolescent. Ann Otol Rhinol Laryngol. 1996;105(4):267–271. doi: 10.1177/000348949610500404. [DOI] [PubMed] [Google Scholar]
- 39.Emir H, Tekant G, Beşik C, Eliçevik M. Bronchoscopic removal of tracheobroncheal foreign bodies: value of patient history and timing. Paediatr Surg Int. 2001;17:85–87. doi: 10.1007/s003830000485. [DOI] [PubMed] [Google Scholar]
- 40.Perrin G, Colt HG, Martin C, et al. Safety of interventional rigid bronchoscopy using intravenous anesthesia and spontaneous assisted ventilation: a prospective study. Chest. 1992;202:1526–1530. doi: 10.1378/chest.102.5.1526. [DOI] [PubMed] [Google Scholar]
- 41.Hanowell LH, Martin WR. Complications of general anesthesia for Nd:YAG laser resection of endobronchial tumors. Chest J. 1991 doi: 10.1378/chest.99.1.72. [DOI] [PubMed] [Google Scholar]
- 42.Dumon JF, Shapshay S, Bourcereau J, Cavaliere S, Meric B, Garbi N, Beamis J. Principles for safety in application of neodymium-YAG laser in bronchology. Chest. 1984;86(2):163–168. doi: 10.1378/chest.86.2.163. [DOI] [PubMed] [Google Scholar]
- 43.Miligan KR, Howe JP, O’Toole DP, et al. Outpatient anaesthesia: recovery after propofol, methohexitol and thiopental. Anaesthesia Analgesia. 1987;66(2):s118. doi: 10.1213/00000539-198702001-00118. [DOI] [Google Scholar]
- 44.Aydogan LB, Tuncer U, Soylu L, et al. Rigid bronchoscopy for the suspicion of foreign body in the airway. Int J Paediatr Otolaryngol. 2006;70(5):823–828. doi: 10.1016/j.ijporl.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 45.Roberts CA, et al. Morbidity and mortality in children undergoing bronchoscopy for foreign body removal. Laryngoscope. 2018;128(5):1226–1229. doi: 10.1002/lary.26817. [DOI] [PubMed] [Google Scholar]
- 46.Divarci E, Toker B, Dokumcu Z, Musayev A, Ozcan C, Erdener A. The multivariate analysis of indications of rigid bronchoscopy in suspected foreign body aspiration. Int J Paediatr Otorhinolaryngol. 2017;100:232–237. doi: 10.1016/j.ijporl.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 47.Fidkowski CW, Zheng H, Firth P. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesthesia Analgesia. 2010;111(4):1016–1025. doi: 10.21037/jtd.2016.12.69.2101. [DOI] [PubMed] [Google Scholar]
- 48.Latifi X, Mustafa A, Hysenaj Q. Rigid tracheobronchoscopy in the management of airway foreign bodies: 10 years experience in Kosovo. Int J Pediatr Otorhinol. 2006;70(12):2055–2059. doi: 10.1016/j.ijporl.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 49.Ernst A, Simoff M, Ost D, et al. Prospective risk-adjusted morbidity and mortality outcome analysis after therapeutic bronchoscopic procedures: results of a multi-institutional outcomes database. Chest. 2008;134(3):514–519. doi: 10.1378/chest.08-0580. [DOI] [PubMed] [Google Scholar]
- 50.Zhang J, Zhang Y et al. (2004) How to reduce the incidence of complications and mortality in Paediatric tracheobronchial foreign body patients. Zhonghua Er B, Yan Hou Ke Za Zhi [Article in Chinese] 39(11): 658–662. PMID 15835815 [PubMed]
- 51.Reilly J, Thompson J, MacArthur C, et al. Pediatric aerodigestive foreign body injuries are complications related to timeliness of diagnosis. Laryngoscope. 1997 doi: 10.1097/00005537-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 52.American Academy of Paediatrics (1997:91) Guidelines for health supervision III. 3rd Ed ELK Grove village III: American Academy of Paediatrics


