Abstract
Introduction
Venous malformations are commonly seen in muscles like masseter, temporalis, tongue musculature, oral and airway mucosa in the head and neck region but is rarely seen in parapharyngeal space.
Case Summary
We report a case of a 60 year female patient who presented with foreign body sensation of throat, sticky sensation and dysphagia to solids for 2 years. She was subjected to relevant investigations including MRI and USG guided FNAC. Following which she underwent endoscopic parapharyngeal space tumour excision and specimen was sent for HPE. Post operatively patient is doing well and symptomatically better. She is being followed up on regular basis.
Conclusion
Parapharyngeal space tumours accounts for only 0.5% of head and neck tumours, of which 70 to 80% are benign and the rest are malignant. Out of the benign tumours of parapharyngeal space we should also keep in mind rare tumours like venous malformations.
Keywords: Venous malformation, Parapharyngeal space, Tumours
Introduction
Among vascular malformations, venous malformations occurs commonly in muscle groups and rarely in skin and mucosa. Less than 1% of head and neck tumours are accounted for by parapharyngeal space tumours amongst which venous malformations are very rare, only 1 case report has been noted in literature [1,2, 3].
Case Report
We are reporting the case of a 60 year old female patient who presented with foreign body sensation and sticky sensation in throat, difficulty in swallowing for past 2 years. She gives history of occasional episodes of throat pain for the past 1 year. She gave no complains of change in voice, neck swelling, ear pain or odynophagia. She had no co morbidities. She underwent 2 surgeries in the past for the same complaint – tonsillectomy a year back and paratonsillar cyst excision 6 months back. On clinical examination there was a bulge noted in the region of right anterior pillar pushing it medially(Fig. 1). Bilateral tonsillar fossa was clear. Indirect laryngoscopic examination was normal. Neck examination was also normal.
Fig. 1.

Preoperative appearance of right parapharyngeal space tumour
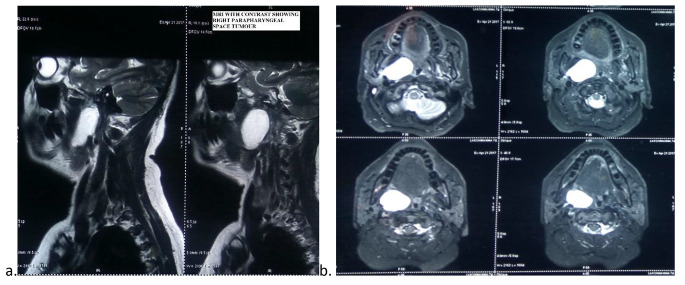
She was subjected to MRI with contrast which showed a hyperintense lesion in the prestyloid compartment of size 3 × 3 cm suggestive of neurogenic tumour (Fig. 2). Superiorly lesion appeared to extend till the soft palate, inferiorly upto epiglottis, anteriorly upto pterygoid plates, laterally abutting medial pterygoid muscle and medially obliterating the oropharynx. USG guided FNAC was done transorally and was inconclusive. Although an excision biopsy was planned in another hospital, they failed at performing the same. We then attempted to perform a deep punch biopsy, although an accurate pathological diagnosis was not arrived at, the differentials were as follows – lymphoma, minor salivary gland tumour and low grade squamous cell carcinoma.
Fig. 2.
a, b MRI scans of right parapharyngeal space tumour
We performed a transoral endoscopic excision of the right sided parapharyngeal space tumour by extracapsular dissection technique. It was a soft red tumour which was sent for histopathological examination. There was no significant intraoperative bleeding. Wound was closed in layers. Patient was put on ryles tube feed for 2 days. The immediate post operative period was uneventful.
Cut section of the tumour showed greyish white tissue sections. The histopathological report for the tumour came as venous malformation characterized by vessels of different sizes with stroma containing inflammatory infiltrate and fibrosis. The patient is being followed up on a regular basis for the past 3 years and patient has no features of any residual or recurrent disease.
Discussion
The International Society for the Study of Vascular Anomalies (ISSVA) adopted a classification system that distinguishes vascular tumors (lesions with clear manifestations of cell proliferation) from vascular malformations (due to innately perturbed vascular morphogenesis). The latter are classified according to the type of vessel involved—hence, capillary, venous, lymphatic, and arteriovenous malformations. However, combined forms are also found, including venolymphatic and arteriovenolymphatic malformations [4].
It is commonly diagnosed in the fourth decade of life with a clear female predominance. Clinically, these vascular malformations are seen as slow-growing, soft, mobile masses with no facial nerve palsy. They often enlarge during puberty and pregnancy (due to hormonal influence) and do not regress. Most patients are asymptomatic and rarely present with dyspnoea or dysphagia. CT with contrast and USG are first-intention explorations for the initial workup but MRI remains the gold standard for the exploration of tumours located in the parapharyngeal space [5]. In principle, fine-needle aspiration is contraindicated in highly vascularized tumours because of the risk of bleeding [3].
Patients often receive surgery as this will permit to obtain a histologic analysis. These tumours may occasionally be very advanced or aggressive, thus requiring dissection of the facial nerve or even its total resection to avoid recurrence. Other treatment modalities using sclerosing agents such as ethanol directly introduced by percutaneous puncture can be used alone or in combination with surgery [1]. In the literature, there have been only two reported cases of recurrence subsequent to incomplete resection due to poorly controlled bleeding [6]. Laser therapy can be useful in very superficial forms of venous malformations and in oromucosal lesions. Photocoagulation can be performed with argon, yellow dye, or a neodymium yttrium aluminum garnet laser. For deeper lesions, laser probes can be inserted subcutaneously [7].
The classical histological appearance shows benign vascular proliferation with endothelial cells in the vessel walls. The lumen is either congested with thromboses and/or calcifications (phleboliths).
Venous malformations have a regular, encapsulated appearance and are bordered by regular-sized endothelial cells. Moreover, they can be associated with lymphatic vessels [1].
Conclusion
We present a rare case of venous malformation in the parapharyngeal space which was surgically excised and histologically confirmed. Biopsy of vascular lesions in this region is risky due to chance of haemorrhage. MRI is the gold standard for diagnosis. The upcoming modalities of treatment includes laser and also transoral robotic excision of the lesion.
Acknowledgements
None.
Funding -
None.
Declarations
Disclosure of interest-
There are no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16:405–418. doi: 10.1111/j.1601-0825.2010.01661.x. [DOI] [PubMed] [Google Scholar]
- 2.Fagan J (2014) Open access atlas of otolaryngology. head & neck operative surgery
- 3.Nicolas Fakhry MD1, Varoquaux A, Michel MD2J MD1, and Antoine Giovanni, MD, PhD1, ‘Venolymphatic vascular malformation in the Parapharyngeal Space’,Otolaryngology–Head and Neck Surgery147(4) [DOI] [PubMed]
- 4.Hassanein AH, Mulliken JB, Fishman SJ, Greene AK. Evaluation of terminology for vascular anomalies in current literature. Plast Reconstr Surg. 2011;127:347–351. doi: 10.1097/PRS.0b013e3181f95b83. [DOI] [PubMed] [Google Scholar]
- 5.Ernemann U, Kramer U, Miller S, et al. Current concepts in the classification, diagnosis and treatment of vascular anomalies. Eur J Radiol. 2010;75:2–11. doi: 10.1016/j.ejrad.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 6.Achachea M, Fakhrya N, Varoquauxb A, Coulibalyc B, Michela J, Lagiera A, Antoninia F, Turnera F, Dessia P, Giovannia A (2013) Management of vascular malformations of the parotid area, European Annals of Otorhinolaryngology, Head and Neck diseases 130, 55–60 [DOI] [PubMed]
- 7.Josée Dubois MD, Gilles Soulez MD, Vincent L, Oliva MD, Marie-Josée Berthiaume MD (2001) Chantale Lapierre, MD, and Eric Therasse, MD, Soft-Tissue Venous Malformations in Adult Patients: Imaging and Therapeutic Issues, RadioGraphics ; 21:1519 – 1531 [DOI] [PubMed]