Abstract
This is the first description of condylar jugular diverticulum (CJD) by means of contrast-enhanced computed tomography scan in the medical literature. CJD is a rare anatomical variant of jugular bulb that should be known to avoid radiological and surgical errors and achieve an appropriate pre-surgical planning of skull base pathologies.
Keywords: Imaging, Skull base, Jugular foramen, Jugular bulb pseudolesion, Jugular bulb diverticulum, Occipital condyle.
Introduction
The jugular bulb (JB) is a venous structure located in the posterolateral part of the jugular foramen (pars vascularis) along with vagus (X), spinal accessory (XI), and Arnold’s nerve [1]. The jugular foramen is situated on the floor of the posterior fossa, between the petrous temporal bone and the occipital bone [2]. The JB receives venous drainage from the sigmoid sinus and inferior petrosal sinus, while internal jugular vein provides its main outflow [3].
The development of the JB occurs in childhood, when the erect posture is attained (around 2 years of age) and becomes stable in adulthood. It is postulated that the ascending negative pulse waves originating from the right atrium are transmitted rostrally into the jugular sinus leading to the formation and dilation of the JB [4].
Jugular bulb diverticulum (JBD) is an outpouching of the jugular bulb that extends superiorly, medially, and posteriorly in the petrous bone; it is considered an under-reported variation, more common than previously thought (prevalence on imaging series ranges 1–8%) [1]. Often JBD is an incidental finding, but some patients may present with sensorineural hearing loss caused by erosion of the internal acoustic canal or Meniere’s syndrome from encroachment of the endolymphatic duct within the vestibular aqueduct [5].
In very rare cases, the JB may extend into the occipital condyle; this condition was first described in 2009 and named as “condylar jugular diverticulum” (CJD) [6]. We present the contrast-enhacenced computed tomography (CT) findings of an incidental discovered CJD followed by a discussion about the possible clinical implications of this anomaly.
Case Report
We discuss the case of a 73-year-old woman, in oncological follow-up for renal (clear cell renal carcinoma) and lung (lung adenocarcinoma) neoplasms treated with surgery; the hematological history also included a chronic lymphocytic leukemia. The subject did not report any hearing impairment or dizziness. The patient underwent several whole-body CT examinations for oncology purposes from 2016 to 2022. The unenhanced head CT scans (Fig. 1) documented a well-defined corticated defect that extended medially and inferiorly from the right jugular foramen into the ipsilateral occipital condyle; no evidence of bone destruction was noted. The enhanced head CT scans (Fig. 2) confirmed the communication between the JB and the occipital condyle diverticulum, specifically showing the same post-contrast enhancement of the venous vessels. Thus, the radiological diagnosis of CJD was made. CJD remained unchanged in size and densitometry throughout the time span examined (about 6 years).
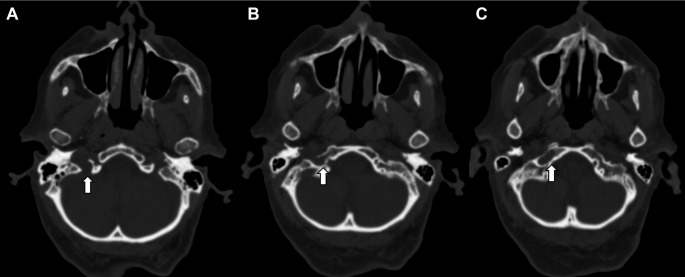
Fig. 1.
Unenhanced CT scan of the skull base on axial plane from jugular foramen to occipital condyle (from A to C), using bone window. The images demonstrate a well-corticated defect in the right occipital condyle communicating superiorly and laterally with the right jugular foramen, without evidence of cortical bone destruction (arrow). Note the normal left occipital condyle
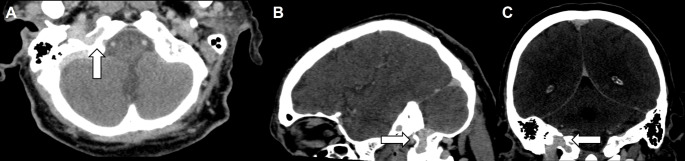
Fig. 2.
Contrast-enhanced CT scan of the skull base on axial plane (A), sagittal plane (B) and coronal plane (C). The images show the communication between the right jugular bulb and the right occipital condyle diverticulum, with the same post-contrast enhancement of the venous vessels (arrow)
Discussion
To the best of our knowledge this represents the tenth case of CJD described in the literature and the first with contrast-enhanced CT scan documentation. In the previous two case series, CJD was documented as an incidental finding in radiological investigations [CT, magnetic resonance imaging (MRI), and cone-beam CT), and in all 9 patients, jugular foramen syndrome was never reported (as in our case) [6, 7]. It is reasonable to assume that the prevalence of CJD will tend to increase over time in relation to the widespread use of imaging techniques in both oncological and non-oncological patients [8, 9].
The etiology of JBD is poorly understood; it has been suggested that abnormal venous flow, whether it is turbulence or hypertension, could be a contributing factor [4].
We believe that the clinical importance of CJD should be sought in three different aspects, although there is no specific scientific literature on this topic. Firstly, a CJD could be a source of hemorrhage in patients with fractures through the occipital condyle. Secondly, a CJD could be injured during surgical skull base procedures, such as transcondylar-transtubular approach and retrosigmoid craniectomy, that can expose the posterior condyle and the hypoglossal canal and open up the posterior rim of the jugular foramen [7]. In addition, knowledge of this venous anomaly may be desirable before performing a surgical procedure [10] or biopsy of the occipital condyle to prevent hemorrhagic complications. Thirdly, the awareness and recognition of a CJD will help to avoid misdiagnosis in radiological images interpretation. On CT, this variant is characterized by a well-corticated bone defect in the occipital condyle, communicating with the jugular foramen, without evidence of erosion on jugular spine (a small ledge that separates the jugular foramen into the pars nervosa anteriorly and pars vascularis posteriorly) [6, 7]. MRI shows venous flow within the occipital condyle defect, contiguous with the JB, especially when magnetic resonance venography is performed [6]. In both MRI and CT scans the diverticulum enhanced avidly and homogeneously when intravenous contrast media is administered (as shown in our case). Differential diagnosis is mandatory especially when these anatomical variants are found in cancer patients (such as in our case). Jugular foramen lesions include several pseudo-lesions (e.g., JB flow variants, high dehiscent JB, vascular and inflammatory lesions), primary jugular foramen neoplasms (e.g., glomus jugulare paraganglioma, schwannoma and primary jugular foramen meningioma) and secondary jugular foramen neoplasms (e.g., metastatic disease, infiltrative malignancy, and skull-base tumors) [1]. On the other hand, the most frequent occipital condyle lesions in symptomatic patients are metastases. In all imaging modalities the key for the proper diagnosis of CJD is the communication with the JBD, without signs of bone disruption.
In conclusion, CJD is a rare, probably under-reported, anatomical variant of JB; knowledge of this anomaly is necessary to avoid diagnostic errors and for appropriate pre-surgical planning in skull base pathologies.
Authors’ Contribution
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MP, FV, CAM and CCQ. The first draft of the manuscript was written by MP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript
Funding
The authors did not receive support from any organization for the submitted work.
Declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics Approval
Ethical approval was waived by the local Ethics Committee of Campus Bio-Medico University in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Consent to Participate
Written informed consent for the possible use of existing anonymized data for research purposes is obtained from all patients as an institutional policy.
Consent for Publication
The participant consented to the case report submission to the journal.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ong CK, Fook-Hin Chong V. Imaging of jugular foramen. Neuroimaging Clin N Am. 2009;19:469–482. doi: 10.1016/j.nic.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Fernandes CL, Fernandes CMC. A Limited Approach to the Jugular Bulb: anatomical considerations in a Rare Jugular Foramen Tumour. Indian J Otolaryngol Head Neck Surg. 2013;65:619–621. doi: 10.1007/s12070-013-0631-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasad KC, Basava CH, Gopinathan PN, et al. A revisit to high jugular bulb: a newer clinical grading. Indian J Otolaryngol Head Neck Surg. 2018;70:527–530. doi: 10.1007/s12070-018-1456-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manjila S, Bazil T, Kay M, et al. Jugular bulb and skull base pathologies: proposal for a novel classification system for jugular bulb positions and microsurgical implications. Neurosurg Focus. 2018;45:E5. doi: 10.3171/2018.5.FOCUS18106. [DOI] [PubMed] [Google Scholar]
- 5.Paulose AA, Ranju RL, Lepcha A, et al. Etiopathology and prevalence of Pulsatile Tinnitus in a Tertiary Care Referral Hospital. Indian J Otolaryngol Head Neck Surg. 2021 doi: 10.1007/s12070-021-02761-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raghuram K, Curé JK, Harnsberger HR. Condylar jugular diverticulum. J Comput Assist Tomogr. 2009;33:309–311. doi: 10.1097/RCT.0b013e31817f8d11. [DOI] [PubMed] [Google Scholar]
- 7.Jagtap R, Wazzan T, Hansen M, Kashtwari D. Condylar jugular diverticulum: a report of 3 cases. Imaging Sci Dent. 2019;49:251–256. doi: 10.5624/isd.2019.49.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parillo M, Quattrocchi CC, Pilato F, et al. Whole-body computed tomography as first-line imaging procedure to exclude cancer in patients with neurological suspicion of paraneoplastic syndromes: shall clinical practice adhere to recommendations? Radiography (Lond) 2022;29:8–13. doi: 10.1016/j.radi.2022.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Parillo M, Vaccarino F, Quattrocchi CC. Imaging findings in a case of leptomeningeal myelomatosis, a rare but critical central nervous system complication of multiple myeloma. Neuroradiol J 19714009221150850. 2023 doi: 10.1177/19714009221150849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kataria T, Sehra R, Grover M, et al. Correlation of Preoperative High-resolution computed tomography temporal bone findings with intra-operative findings in various ear pathologies. Indian J Otolaryngol Head Neck Surg. 2022;74:190–199. doi: 10.1007/s12070-020-01950-6. [DOI] [PMC free article] [PubMed] [Google Scholar]