Abstract
Infraorbital nerve schwannoma is an infrequent entity that is rarely reported in the paediatric population. This case report is a summed-up report of this infrequent diagnosis, its presentation, and management from an otorhinolaryngologist’s perspective. It is reported here for its rarity, inherent surgical challenge, and academic interest. We report a case of a 13-year-old boy with infraorbital nerve schwannoma arising from its two terminal branches. We performed its surgical excision without any disabling deformity. The peculiarity of this case gives insight into the varied presentation of schwannoma. It is important to identify such cases with a high degree of suspicion and treat them accordingly.
Keywords: Schwannoma, Infraorbital nerve
Introduction
Schwannoma is a benign encapsulated rare tumour arising from Schwann cells. Schwann cells form the peripheral nervous system’s (PNS) outer nerve sheath layer. They protect and support the nerve cells of the PNS.
Schwannoma is very well reported in the head and neck region, mainly from lower cranial nerves. Other name for schwannoma are neurlemmomas, neurolemoms, or neuromas.
We outline a rare case report of pediatric schwannoma arising from the infraorbital nerve.
Case Report
A 13-year-old boy presented in the outpatient department with progressively increasing non-tender swelling of the nose extending to the left cheek. Physical examination revealed two solitary subcutaneous swellings; first one of approximately 5–6 cm in size on the dorsum of the nose, extending more on the left than right. Another midline spherical swelling about 2 cm in size was present in the philtrum area, pushing the upper lip to droop downwards. The nasolabial fold was slightly obliterated on the left side. The skin over the swelling was distended and fixed (Fig. 1). There was no sensory deficit on either side. However, the swelling was in the line of vision and was obstructing the bilateral nasal visual field. Ophthalmological examination was within the normal limits. There was no cervical lymphadenopathy or similar lesion on the trunk or limbs. No familial history of similar illness. Intraoral examination was also within the standard limit.
Fig. 1.
Preoperative picture with an arrow pointing towards swelling
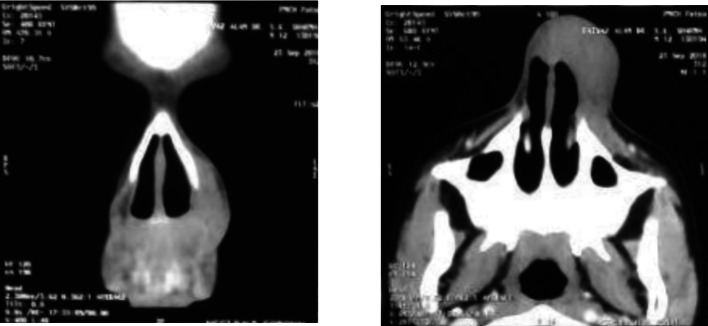
A computed tomography scan of the case showed a well-defined soft tissue iso-hypodense lesion at the nasal dorsum extending more to the left than right, causing thinning and erosion of underlying nasal cartilage (Fig. 2). The provisional diagnosis of schwannoma was given.
Fig. 2.
Preoperative coronal and axial CT scan of the patient, respectively
Patient was posted for surgery after proper counselling and after obtaining required consent. Surgical excision was planned after an anesthetic evaluation. Under general anesthesia. Rethi Meyer’s incision was given with an extension lateral to the frenulum. A flap was elevated off the swelling with sharp dissection. The lesion emerged from the nerve trunk of the peripheral branch of the left Infraorbital nerve. The mass was excised in toto by sacrificing the involved nerve. The lateral cartilage was thinned out due to the pressure of the mass. The incision was closed in layers with anterior nasal packing. The postoperative period was uneventful.
Gross examination showed an elongated growth of around 12 cm and 4 cm in width. It was well encapsulated, had homogenous consistency, and was pale yellow in colour (Fig. 3).
Fig. 3.

Intraoperative picture of the swelling and the gross specimen, respectively
The patient reported a minor localized area of numbness over the left cheek area around nasolabial fold which improved over a period of 6 months.
Histopathological examination of the specimen showed it was composed of spindle cells arranged in bundles. Spindle cells were well-differentiated, and mild nuclear pleomorphism was present. Mitotic figures were rare. A palisading arrangement was observed. A biphasic pattern was seen composed of Antoni A and Antoni B cells. It also displayed strong diffuse nuclear positivity with S-100.
Diagnosis of schwannoma was confirmed, arising from the terminal nasal and superior labial branch of the infraorbital nerve. No recurrence was noted in 1-year duration.
Discussion
Schwann cells are named after German physiologist Theodor Schwann, who discovered them back in the 19th century. However, the first description of schwannoma dates back to 1910 by Verocay [1]. First trigeminal nerve schwannoma was reported by smith in 1835.
Schwannomas are the fourth most common primary neoplasms affecting the brain and cranial nerves. Central lesions commonly arise from sensory nerve roots, and a common intracranial site is the vestibular branch of the eighth nerve (> 85% of central schwannomas and 8–10% of all intracranial tumors) [2]. Schwannomas are reported more frequently in males than females, mostly in the 2nd to 4th decade of life [3].
The majority (> 90%) of cranial nerve schwannomas arise from the vestibulocochlear nerve, followed by trigeminal and facial nerves, then by the lower cranial nerves [4]. Trigeminal schwannomas are extremely rare, accounting for less than 0.5% of intracranial tumours. Of the 12 cranial nerves, schwannomas do not develop from the first two cranial nerves, i.e. olfactory and optic nerve, as they do not have Schwann cells in their sheaths.
Although very frequently reported in the head and neck region only nine [5] benign and five malignant cases have been reported so far after extensive search of literature to originate from the infraorbital nerve. Most of the extracranial schwannomas are present in the head and neck (25–45%) [6].
The infraorbital nerve is a branch of the maxillary division of the trigeminal nerve and branches just after emerging from the Foramen rotundum to enter the pterygopalatine fossa. It is a sensory branch and the terminal branch of the second division. There can be variations in the anatomy of the infraorbital nerve [7]. It courses laterally through the inferior orbital fissure to enter orbit. It then runs into an infraorbital groove in the floor of orbit to supply maxillary sinus and teeth through three sensory branches posterior superior alveolar nerve, middle superior alveolar nerve, and anterior superior alveolar nerve. It then enters the infraorbital canal and emerges through the infraorbital foramen on the face. This part further gives three branches palpebral branch, nasal branch, and superior labial branch supplying the skin of the cheek, lateral nose, upper lip, and mucosa of the upper lip and lower part of the nose. The external nasal nerve can be absent in 34.53% of cases [7]. Accessory superior labial nerves can be present in 9.52% of the nerves. These variations need to be considered, especially during facial surgeries and infraorbital nerve blocks.
Previously published cases of infraorbital schwannomas were mainly described as arising from the main trunk or within the inferior orbital fissure. None of the cases was reported in the terminal part involving the nasal and superior labial branch making this case an exception.
The variant malignant schwannoma are uncommon sarcomas reported from the sheath of Schwann cells of surrounding nerve fibres. Only a handful of cases are known to arise from the infraorbital nerve. The diagnosis can be suggested based on rapid growth or extensive nerve involvement. Still, it can be confirmed only by histopathological diagnosis by features such as diffuse cellular atypia, p53 positivity, and high MIB1 staining [6].
The symptoms produced by schwannoma depend upon the lesion’s site and size. Infraorbital nerve schwannoma causes swelling in the cheeks, pressure necrosis of cartilage and bones, pain, paraesthesia of the surrounding area, and diplopia or exophthalmos. The only symptom was cosmetic deformity and visual field obstruction in our case.
The treatment of choice is surgical, and the approach is dictated by the size and the site of the lesion. Various approaches can be implemented, including intraoral incisions [7], Caldwell luc [5], sub- ciliary [1], Weber Ferguson, sub labial transoral or endoscopic approaches, Le fort I maxillary osteotomy approach, osteoplastic maxillectomy approach, midfacial degloving, and limited transzygomatic or limited rhytidectomy approach.
The differential diagnosis for schwannoma includes haemangioma, leiomyoma, fibrosarcoma, leiomyosarcoma, fibrosarcoma, or meningioma [8]. It can also present with a cystic component, misleading the diagnosis to mucocele, mucocele, or even epidermoid cyst [9]. To differentiate all the possibilities and reach the diagnosis, one needs radiological and histopathological investigations. Traditionally CT scan is done to localize the site and its extension to surrounding tissue. However, MRI gives a better idea of invasion into the surrounding soft tissue. MRI has high sensitivity, especially with the application of contrast agents. On CT scan, the schwannoma can appear as circumscribed growth with a displacement of local structures and smooth expansion of bony foramina. The growth can display varying degrees of solid enhancement with cystic spaces on MR and heterogenous high signal intensity specifically on T2 weighted MR images [4].
The microscopic picture shows degenerative changes with a variable mixture of compact spindled (Antoni A) areas and hypocellular microcystic (Antoni B) areas rich in macrophages and collagen fibres. The hallmark cells of schwannoma Antoni type A and B. Antoni Type A are characterized by closely packed spindle cells having fusiform nuclei and eosinophilic cytoplasm. Type B pattern is characterized by haphazardly distributed cells with distinct cytoplasmic margins. It is bounded by a collagenous capsule and hyalinised vessels. Immunohistochemistry shows diffuse, strong expression of S100 protein and abundant pericellular collagen type IV. The S100 protein is expressed by the peripheral Schwann cells and is the main differentiating point from neurofibromas and other non-neural origin tumors [10].
Extracranial trigeminal nerve schwannoma has a good prognosis compared to intracranial presentation. The physical deformity by this type of lesion predisposed the child to depression and lack of self-confidence. Physical appearance has a very close relationship with the mental status of the child in this impressionable age. Treating a case like this not only cured the physical component but also restored self-confidence.
Conclusion
The authors describe a rare case of a pediatric infraorbital nerve schwannoma that presented as a nasal dorsum swelling, its workup, its differentials, its treatment, and a review of the literature. The use of a preoperative computed tomographic scan permitted the use of the accurate technique with good visual access to the lesion. The use of appropriate radiological investigation enhances the accuracy of preoperative diagnosis. The treatment modality should be adopted based on the individual clinical status of the patient.
Funding
Nil.
Declarations
Conflict of interest
The author declares that there is no conflict of interest.
Ethical Approval
Approved by Institute’s ethical committee.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ayushree, Email: ayushree.sharma@gmail.com.
Vivek Kumar, Email: vicky2705@gmail.com.
Richa, Email: Dr.richa4741@gmail.com.
References
- 1.Kim KS, Jung JW, Yoon KC, Kwon YJ, Hwang JH, Lee SY. Schwannoma of the Orbit. Arch Craniofac Surg. 2015;16(2):67–72. doi: 10.7181/acfs.2015.16.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Köhler LR, Filho PMM, Santos FP, Sawasaki R, Giacomelli R, Cordeiro R, et al. Trigeminal ophthalmic branch schwannoma: case report and literature review. Arq Bras Neurocir Braz Neurosurg. 2021;40(01):091–096. doi: 10.1055/s-0040-1718421. [DOI] [Google Scholar]
- 3.Tezer MS, Ozcan M, Han Ö, Unal A, Ozlugedik S. Schwannoma originating from the infraorbital nerve: a case report. Auris Nasus Larynx. 2006;33(3):343–5. doi: 10.1016/j.anl.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Skolnik AD, Loevner LA, Sampathu DM, Newman JG, Lee JY, Bagley LJ, et al. Cranial nerve schwannomas: diagnostic imaging approach. Radiogr Rev Publ Radiol Soc N Am Inc. 2016;36(5):1463–1477. doi: 10.1148/rg.2016150199. [DOI] [PubMed] [Google Scholar]
- 5.Kok YO, Yeo MSW, Nallathamby V, Lee SJ. Infraorbital nerve schwannoma presenting as an upper lip mass in an adolescent boy. Ann Plast Surg. 2013;71(2):196–197. doi: 10.1097/SAP.0b013e318248b8a2. [DOI] [PubMed] [Google Scholar]
- 6.Naina P, Masih D, Mathews SS. Infraorbital nerve schwannoma: a rare cause of upper jaw swelling. Indian J Dent Res Off Publ Indian Soc Dent Res. 2014;25(2):263–265. doi: 10.4103/0970-9290.135940. [DOI] [PubMed] [Google Scholar]
- 7.Nderitu JM, Butt F, Saidi H. Variant anatomy of the nasal and labial branches of the Infraorbital nerve. Craniomaxillofacial Trauma Reconstr. 2016;9(4):294–6. doi: 10.1055/s-0036-1584404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malone JP, Lee WJ, Levin RJ. Clinical characteristics and treatment outcome for nonvestibular schwannomas of the head and neck. Am J Otolaryngol. 2005;26(2):108–112. doi: 10.1016/j.amjoto.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Tsuzuki N, Katoh H, Ohnuki A, Ishihara S, Miyazawa T, Nawashiro H, et al. Cystic schwannoma of the orbit: case report. Surg Neurol. 2000;54(5):385–387. doi: 10.1016/S0090-3019(00)00278-0. [DOI] [PubMed] [Google Scholar]
- 10.Rodriguez FJ, Folpe AL, Giannini C, Perry A. Pathology of Peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta Neuropathol (Berl) 2012;123(3):295–319. doi: 10.1007/s00401-012-0954-z. [DOI] [PMC free article] [PubMed] [Google Scholar]