Abstract
Rationale and objective
Demographic data collected about Canadian radiologists and trainees has been limited primarily to binary gender and geographic location. The purpose of this study was to investigate: (1) demographic characteristics of Canadian radiologists and trainees; (2) types of diversity important to radiologists; (3) relationship of radiologist demographics to practice characteristics; and (4) relationship of radiologist demographics to years in practice, (YIP).
Materials and methods
French and English surveys were distributed via email through radiology associations and social media. Frequency counts of demographic variables were calculated, and chi-square and Fisher's Exact tests were performed to explore the relationships between demographic characteristics and role.
Results
611 individuals responded to the survey. 573 respondents were included in the analysis. 454 (78.8%) were practicing radiologists and 119 (20.7%) were residents/fellows. Half identified as women (50.4%). English was the primary language for most respondents. There was an association between role and sexual orientation (p = 0.02), visible minority (χ2 = 4.79, p < 0.05), religion (χ2 = 4.11, p < 0.05), and having children (χ2 = 136.65, p < 0.05). For radiologists, being a visible minority (χ2 = 11.59, p < 0.05) and age (χ2 = 56.3, p < 0.05) were associated with academic rank while gender (χ2 = 3.83, p < 0.05) and age (χ2 = 13.74, p < 0.05) were related to part-/full-time status. Less women, visible minorities, and women with children had been in practice for long.
Discussion
This study represents a comprehensive analysis of Canadian radiology demographics. Results suggest there is increasing diversity among trainees; however, significant demographic underrepresentation compared to the diversity of Canada exists.
Keywords: Diversity, Radiology, Equity, Inclusivity, Inclusion, Representation, Demographics, Canada, Resident
Abbreviations
- ARQ
Association des Radiologistes du Québec
- CAR
Canadian Association of Radiologists
- CMA
Canadian Medical Association
- EDI
Equity, Diversity, and Inclusion
1. Introduction
The importance of equity, diversity, and inclusion (EDI) in the workplace is now recognized as an important topic in medicine. Increasing diversity within medicine has been shown to have many benefits, which include improved patient outcomes and satisfaction, reduced risk of hospitalization for ambulatory care sensitive conditions, as well as improved research agendas, creativity, and innovation [[1], [2], [3], [4], [5]]. In an effort to increase the diversity of healthcare workers, many associations and institutions have implemented strategies and committed to create a medical workforce that better reflects the diversity of the population it serves [[6], [7], [8]].
Over the past twenty years, the radiology community has highlighted the need for a more diverse medical workforce, especially in regard to women and underrepresented minorities [[9], [10], [11], [12], [13]]. In Canada there have been many recent EDI initiatives. In 2020, Lebel et al. published a review of the status of diversity in Canadian radiology and suggested targeted recommendations for improvement. One of the most critical recommendations was for organizations and institutions to increase data collection to determine the demographics of the Canadian radiology workforce. In an effort to assess and address EDI issues in Canada, the Canadian Association of Radiologists (CAR) created five EDI subcommittees respectively addressing: diversity statements; encouraging radiology residency applications; bias in recruitment, hiring, promotion, and awards; the development of an EDI toolkit; and gender pay gap. Most of the subcommittees repeated the call to increase demographic data collection to base their strategies and initiatives on the status of the Canadian radiology workforce [14].
In Canada, available demographic data for practicing radiologists and postgraduate trainees are geography, gender, and age [15]. No comprehensive data regarding other demographic variables including gender identity, sexual orientation, ethnicity, visible minority, religion, ability status, and language – of the Canadian radiology workforce are currently reported. While the available limited binary gender and geographic data can be helpful to identify and acknowledge gaps in diversity, they do not provide a robust understanding of what stage in the professional pipeline requires intervention or what professional barriers should be addressed to improve diversity. For example, women represent 63% of medical students but only 32% of radiologists in Canada [16].
The purpose of this study was to establish national baseline demographic parameters of the Canadian radiology workforce. Our research questions, posed to a sample of Canadian radiologists and radiology postgraduate trainees, were: (1) what are respondent demographic characteristics (i.e., gender identity, sexual orientation, ethnicity, visible minority, primary language, religious affiliation, having children, having a disability, and age) and are those characteristics related to the respondents’ Role (i.e., practicing radiologists versus postgraduate trainees) and (2) which types of diversity (i.e., gender, ethnic, and religious) are most important to respondents by Role. Our research questions for practicing Canadian radiologists were: (1) are demographic characteristics related to practice characteristics, such as years of practice, type of practice (i.e., academic vs. non-academic), faculty rank, full-/part-time status, and flexible/non-flexible schedule and (2) is there a relationship between years in practice and demographic characteristics (e.g., gender identity, ethnicity, visible minority, and having children). The relationship between gender identity (man vs woman) and self-reported income of Canadian radiologists has been previously described [17].
2. Methods
A French and English version of the Radiology Demographic survey was developed for this project. The survey was refined multiple times after being piloted with a small group of radiologists and radiology trainees. The survey was created in a University of Alberta REDCap secure web survey platform and approved by the local Research Ethics Board (H21-01253) and distributed from May 2021 to July 2021. Partial results of this survey relating to gender pay gap have previously been published [17].
Survey distribution was described in detail in an earlier publication [17]. In summary, the survey was distributed via an email link using three methods: (1) email distribution from Canadian radiology organizations; (2) posting on social media by members of radiology organizations; and (3) snowball sampling, requesting that radiologists forward the email invitation to radiology contacts.
The latest 2019 Canadian Medical Association (CMA) report indicates there are 2569 diagnostic radiologists, 14 pediatric radiologists, and 19 neuro radiologists for a total of 2602 Canadian radiologists [15]. There are currently 480 Canadian radiology residents, as per compilation from the 16 residency programs. To our knowledge, no clear data exists for the number of fellows in radiology. Respondents who identified as residents or fellows were included under “trainees” in our analysis. From this data, we established the denominator of the individuals who received the survey as 2602 radiologists and 480 residents.
Participants were asked to indicate in which of several possible ways they had received the survey; they could indicate more than one method. A screening question thanked retired radiologists who opened the survey, but indicated they were not able to complete the survey. People working or studying in either Canada or the United States could respond to the survey, but only those in Canada were included in the data analysis. The responses to the English and French surveys were merged into one database. All data analyses were conducted using SPSS V28.01 (1989, 2021).
We calculated frequency counts for categorical self-reported demographic variables (i.e., gender identity, sexual orientation, ethnicity, visible minority, age, language, affiliated religion, and disability), and self-reported practice characteristic variables for radiologists (i.e., years in practice, academic position [yes/no], academic rank, full-time/part-time, and flexible/non-flexible schedule). Categories were collapsed when categories had none or a small number of counts. For example, given the small number or no respondents in some ethnicity categories, the variable measuring ethnicity was recoded to “ethnic group” to include the broad categories of ethnicity in our sample (i.e., Arab, Asian, Black, Indigenous, Latin-X, Multi-ethnic, and White) versus the more discrete categories offered to respondents, such as Black African and Black Caribbean. All categories, except missing/blank data and “other” responses, are included for demographic data, including “prefer not to say.” “Prefer not to say” was included as an answer on questions to accommodate respondents who may have felt uncomfortable or unsafe answering any specific questions.
Chi-square analyses were performed for: (1) each demographic variable by Role (practicing radiologists vs. postgraduate trainees) and (2) radiologists' demographic variables by practice characteristics, e.g., gender identity vs. academic rank. When any cells in a chi-square analysis had expected counts less than five, a Fisher's Exact test (using a 2 × 2 contingency table), was also conducted. For Chi-square tests and Fisher's Exact tests, missing data, “other,” and “prefer not to say” were not included in the analyses.
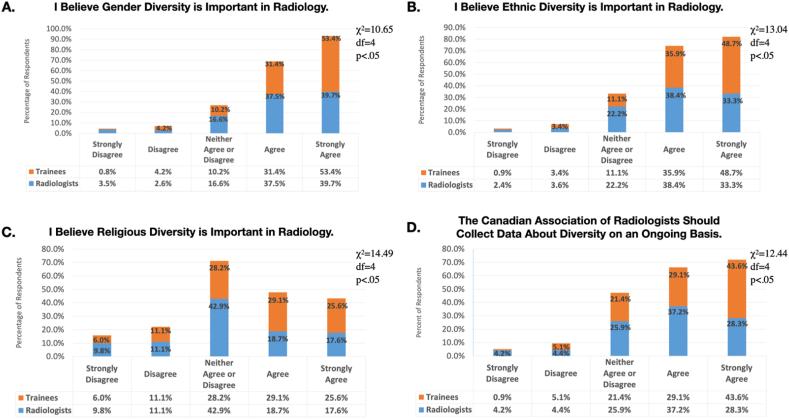
Respondents were asked to rate their level of agreement with three statements related to their attitudes on diversity categories (i.e., gender, ethnic, and religious) “XX diversity in radiology is important to me” with the choices: “strongly disagree; ” “disagree; ” “neither agree nor disagree; ” “agree; ” and “strongly agree.” Chi-square analyses were run for each item by role. A fourth question on diversity asked respondents if they agreed, on the same five-point Likert-like scale, with the following statement, “The Canadian Association of Radiologists (CAR) should collect demographic data about diversity on an ongoing basis.”
3. Results
A total of 611 individuals responded to the survey. 15 responses were excluded as they did not meet study inclusion criteria (n = 3 medical students, n = 6 retired radiologists, and n = 1 radiologist and n = 5 trainees who were outside of Canada). 454 radiologists practicing in Canada (454/2602, 17.4% response rate) and 91 Canadian residents responded to the survey (91/480, 18.9% response rate). A total of 573 responses were included in the final analytic sample. Of respondents in the final analytic sample, of these, 454 (79.2%) were practicing radiologists; 28 (4.9%) radiology fellows, and 91 (15.9%) radiology residents. See Fig. 1 for the overall response rate by province for practicing radiologists and radiology residents.
Fig. 1.
Response rate of practicing radiologists and radiology residents by province.
A large majority of radiologists (n = 374, 84.0%) and radiology trainees (n = 100, 87.7%) reported being members of the Canadian Association of Radiologists (CAR). Most respondents reported receiving the survey through CAR (radiologists: n = 216, 47.6%; trainees: n = 51, 42.9%), while 43 (9.5%) radiologists and 3 (2.5%) of trainees reported receiving the survey from the Association des Radiologistes du Québec (ARQ). A similar percentage of radiologists and trainees reported receiving the survey via social media (14.5% and 12.6%, respectively) and/or from a friend (19.4% and 22.7%, respectively).
Numbers and percentages for all categories of the demographic variables (gender identity, sexual orientation, ethnicity, visible minority, religious affiliation, having children, and having disabilities) by role (radiologists vs. trainees) can be found in Table 1, along with tests for association between demographic characteristics and role.
Table 1.
Demographic characteristics of respondents by Role (i.e., practicing radiologists vs. radiology trainees) working or studying in Canadaa.
| Demographic Characteristics | Practicing Radiologists | Radiology Trainees | χ2 |
|---|---|---|---|
| Gender Identity | N (%) | N (%) | |
| Woman | 227 (50.4) | 59 (50.9) | |
| Man | 216 (48.0) | 53 (45.7) | NS |
| Transgender Man | 0 (0%) | 0 (0%) | |
| Transgender Woman | 0 (0%) | 0 (0%) | |
| Gender Queer | 0 (0%) | 2 (1.7) | |
| Two-spirit | 0 (0%) | 0 (0%) | |
| Prefer not to say | 7 (1.6) | 2 (1.7) | |
| Total | 450 | 116 | |
| Sexual Orientation (within Role) | N (%) | N (%) | |
| Heterosexual | 418 (93.5) | 100 (87.7) | |
| Lesbian, Gay, Bisexual, Transgender, Queer, plus | 14 (3.1) | 10 (8.8) | |
| Prefer not to say | 15 (3.4) | 4 (3.5) | |
| Total ¥ | 447 | 114 | (Fisher's Exact test 2-sided p = 0.02) |
| Ethnic Group You Most Closely Identify with (within Role) | N (%) | N (%) | |
| Arab | 4 (1.0) | 12 (11.0) | |
| Black African | 7 (1.7) | 1 (.9) | |
| Black Caribbean | 4 (1.0) | 2 (1.8) | |
| Black North American | 0 | 0 | |
| Canadian First Nations | 3 (.7) | 0 | |
| Canadian Metis | 0 | 1 (.9) | |
| Canadian Inuit | 0 | 0 | |
| Chinese | 31 (7.4) | 10 (9.2) | |
| Filipino | 1 (.2) | 0 | |
| Japanese | 1 (.2) | 1 (.9) | |
| Korean | 1 (.2) | 1 (.9) | |
| Latin-X | 8 (1.9) | 5 (4.6) | |
| South Asian | 39 (9.3) | 7 (6.4) | |
| Southeast Asian | 10 (2.4) | 2 (1.8) | |
| West Asian | 1 (.2) | 1 (.9) | |
| White | 298 (71.0) | 60 (55.0) | |
| Multi-ethnic | 12 (2.9) | 6 (5.5) | |
| Prefer not to say | 13 (3.0) | 4 (3.5) | |
| Total | 433 | 113 | |
| Dichotomous Ethnicity (within Role)a | N (%) | N (%) | |
|
122 (29.0) | 49 (45.0) | |
|
298 (71.0) | 60 (55.5) | |
| Total¥ | 420 | 109 | 10.01, p < 0.05 |
| Do You Consider Yourself A Visible Minority | N (%) | N (%) | |
| Yes | 125 (27.8) | 45 (38.5) | |
| No | 317 (70.4) | 71 (60.7) | |
| Prefer not to say | 8 (1.8) | 1 (.9) | |
| Total¥ | 450 | 117 | 4.79, p < 0.05 |
| Religion You Most Strongly Identify Witha(within Role) | N (%) | N (%) | |
| Buddhism | 5 (1.1) | 2 (1.8) | |
| Christianity | 178 (40.0) | 33 (29.7) | |
| Hinduism | 12 (2.7) | 2 (1.8) | |
| Judaism | 26 (5.8) | 2 (1.8) | |
| Islam | 10 (2.2) | 13 (11.7) | |
| Sikhism | 7 (1.6) | 2 (1.8) | |
| Traditional Aboriginal Spirituality | 0 (0%) | 0 (0%) | |
| No religious affiliation | 193 (43.4) | 52 (46.8) | |
| Prefer not to say | 14 (3.1) | 5 (4.5) | |
| Total | 445 | 111 | |
| Dichotomous Religious Identity (within Role) | N (%) | N (%) | |
|
60 (25.2) | 21 (38.9) | |
|
178 (74.8) | 33 (61.1) | |
| Total (χ2 = 4.11, df = 1, p < 0.05) | 238 | 54 | |
|
193 (44.8) | 52 (49.1) | |
|
238 (55.2) | 54 (50.9) | |
| Total | 431 | 106 | NS |
| Do you have children (biological or adopted)?a | N (%) | N (%) | |
| Yes | 367 (81) | 30 (25.9) | |
| No | 80 (17.7) | 84 (72.4) | |
| Prefer not to say | 6 (1.3) | 2 (1.7) | |
| Total¥ | 453 | 116 | 136.65, p < 0.05 |
| Do you have any of the following disabilities or long-lasting conditions (check all that apply)a | N (%) | N (%) | |
| Deaf or hard of hearing | 6 (1.3) | 1 (.8) | |
| Visually Impaired | 3 (.7) | 2 (1.7) | |
| Impaired Physical Activity | 8 (1.8) | 2 (1.7) | |
| None | 398 (87.7) | 103 (86.6) | |
| Prefer Not to Say | 16 (3.5) | 5 (4.2) | |
| Total is not included since respondents could respond to all that applied. | |||
| Age | N (%) | N (%) | |
| Less than 25 | 0 (0%) | 3 (2.6) | |
| 25–30 | 0 (0%) | 59 (50.9) | |
| 31–35 | 38 (8.4) | 37 (31.9) | |
| 36–40 | 69 (15.2) | 11 (9.5) | |
| 41–45 | 78 (17.2) | 2 (1.7) | |
| 46–50 | 73 (16.1) | 1 (.9) | |
| 51–55 | 63 (13.9) | 1 (.9) | |
| 56–60 | 53 (11.7) | 0 | |
| 61–65 | 39 (8.6) | 0 | |
| 66 and older | 35 (7.7) | 0 | |
| Prefer not to say | 5 (1.1) | 2 (1.7) | |
| Total | 453 | 116 | |
| Age with 4 categories (within Role)a | |||
| 30 and below | 0 (0%) | 62 (54.4) | |
| 31–40 | 107 (23.9) | 48 (42.1) | |
| 41–55 | 214 (47.8) | 4 (3.5) | |
| Above 55 | 127 (28.3) | 0 (0%) | |
| Total | 448 | 114 | 332.8, p < 0.05 |
¥ “Prefer not to say” was not included in any chi-square or Fisher's Exact tests.
The “other” category and missing/blank values are not included in the table.
The “prefer not to say” category was used infrequently. Most people did not use this category even once (90.1%), and 6–8% used “prefer not to say” one to two times. However, “prefer not to say” was used more frequently for some variables, such as sexual orientation (n = 19, 3.4%), ethnicity (n = 17, 3.1%), language (n = 11, 2.2%), religious affiliation (n = 19, 3.4%), and disability status (n = 21, 3.7%)
Most responding radiologists’ primary language is English (n = 307, 79%). The same was true for radiology trainees (n = 65, 76.5%). Approximately 2% of radiologists and trainees reported both English and French as their primary languages. Of those whose primary language was French (21.8% radiologists, 21.2% trainees), the vast majority worked or studied in Quebec (94.3% radiologists, 88.9% trainees). There was no relationship between role and primary language.
For tests of association between role and: sexual identity; sexual orientation; ethnic group, and affiliated religion, and any disability, there were a lack of respondents who self-reported having a sexual identity other than man or woman, being LGBTQ+, being from an ethnic minority, being non-Christian, or having any disability. In these cases, the variables were dichotomized and the Fisher's Exact test (2 × 2 contingency tables) was used in addition to chi-square tests. See Table 1 for results of demographic characteristics vs. role. Notably, there was not statistical difference between the number of men and women for both practicing radiologists (women: 227, men: 216, p > 0.05) and trainees (women: 59, men: 53, p > 0.05) based on our respondents. However, practicing radiologists were more likely to be heterosexual, white, not a visible minority, and have children (Table 2). Radiology trainees were more likely to be heterosexual, white, and not have any children.
Table 2.
Associations between Practicing Canadian Radiologists Demographic Characteristics and their Practice Characteristics.
| Demographic Characteristics |
Academic Rank |
Full-time or Part-time Employment |
|||||
|---|---|---|---|---|---|---|---|
| Clinical N (%) |
Lecturer N (%) |
Assistant Professor N (%) |
Associate Professor N (%) |
Professor N (%) |
Full-time N (%) |
Part-time N (%) |
|
| Within Gender | |||||||
|
44 (26%) | 13 (8%) | 49 (30%) | 38 (23%) | 22 (13%) | 176 (82%) | 39 (18%) |
|
42 (28%) | 9 (6%) | 45 (29%) | 44 (29%) | 13 (8%) | 166 (74%) | 58 (26%) |
| Not Significant | χ2 = 3.83, df = 1, p ≤ 0.05 | ||||||
| Within Ethnicity | |||||||
|
20 (23%) | 4 (4%) | 36 (41%) | 22 (25%) | 6 (7%) | 97 (80%) | 24 (20%) |
|
61 (29%) | 18 (8%) | 53 (25%) | 54 (26%) | 26 (12%) | 224 (76%) | 72 (24%) |
| χ2 = 9.20, df = 4, p = 0.056 | Not Significant | ||||||
| Within Visible Minority | |||||||
|
24 (25%) | 4 (4%) | 39 (41%) | 24 (25%) | 5 (5%) | 99 (80%) | 25 (20%) |
|
62 (28%) | 18 (8%) | 55 (25%) | 55 (25%) | 30 (14%) | 241 (77%) | 73 (23%) |
| χ2 = 11.59, df = 4, p < 0.05 | Not Significant | ||||||
| Within Age | |||||||
|
28 (35%) | 10 (12%) | 34 (42%) | 8 (10%) | 0 (0%) | 91 (86%) | 15 (14%) |
|
40 (26%) | 9 (6%) | 46 (30%) | 46 (30%) | 11 (7%) | 171 (81%) | 41 (19%) |
|
18 (20%) | 4 (4%) | 16 (18%) | 29 (32%) | 23 (26%) | 85 (67%) | 42 (33%) |
| χ2 = 56.3, df = 8, p < 0.05 | χ2 = 13.74, df = 2, p < 0.05 | ||||||
There were significant relationships between role and all three items querying the importance of diversity in radiology (i.e., gender, ethic, and religious) and with the item querying whether CAR should regularly collect demographic data (see Fig. 2A–D).
Fig. 2.
Attitude responses on “demographic (i.e., gender identity, visible minority, and religious affiliation) diversity is important.
Chi-square tests and Fisher's Exact tests were used to determine if there were significant associations between radiologists' demographic characteristics (i.e., gender identity [woman/man], sexual orientation [heterosexual/LGBTQ+], ethnicity [white/non-white], visible minority [yes/no], age [31–40, 41–55, greater than 55] and their self-reported practice characteristics (Fig. 3A–C). Most responding radiologists reported being in practice less than or equal to 10 years (n = 162, 36.4%); 27.2% between 11 and 20 years (n = 121); 22.9% 21–30 years (n = 102); and 13.5% more than 30 years (n = 60). Radiologists' self-reported years in practice was significantly related to: (a) gender identity (women vs. men); (b) being a visible minority (yes vs. no); (c) whether the respondent had children (yes vs. no); and (d) religious affiliation. With more years in practice being associated with men, of a non-visible minority, and no religious affiliation. The number of respondents for the different ethnic groups and sexual orientation was too small to interpret the data related to years of practice. There were no significant relationships between years of practice and primary language (only English, only French, or both) or disability (any disability or none). For more detailed information on the demographic variables that could delay entry into radiology, see Fig. 3 (graphs A-C).
Fig. 3.
Years in practice by demographic variables (i.e., gender identity, visible minority, and having children within gender identity).
4. Discussion
To our knowledge, this is the first comprehensive, national demographic survey for Canadian radiologists and radiology trainees (residents and fellows) that collected data outside of binary gender, geography, and age. This reported data provides insight into the status of diversity characteristics of the Canadian radiology workforce and may be used to assess the efficacy of current and future processes and interventions to improve diversity and inclusion.
Overall, our national survey response rate was an estimated 18% of all practicing Canadian radiologists and 20% of radiology residents. All provinces (see Fig. 1) and a wide age distribution (see Table 1) were represented. Women were more likely to respond than men. 51.2% of respondents identified as women, which is higher than the reported percentage of women Canadian radiologists from the CMA of 32% [15].
One study, reported that America's physician population was aging, as more than 20% of practicing radiologists were over the age of 65 [18]. According to 2019 CMA data, the distribution of age categories for practicing Canadian radiologists were 26.6% ages 45–54, 24.3% ages 35–44 and 22.6% ages 55–64; radiologists >65 years old represented 14.9% and 5.8% were <35 years old [15]. Although our age categories were not identical with the breakdown of age categories in the CMA report, our sample appears somewhat younger than the Canadian population of radiologists considering that 30.4% (n = 136) of respondents were ages 46–55, only 7.8% (n = 35) were older than 65 years of age and the 31–35 category represented 8.5% (n = 38) of responding radiologists.
The majority of survey respondents reported that they speak English as their primary language, identified as male or female (with equal response rates), are heterosexual, and identify as white. These results suggest that there may be a significant underrepresentation of diversity of sexual orientation and visibly minorities within Canadian radiology. With this data, we can further analyze if diversity within the Canadian radiology workforce mirrors the population it serves.
Our data does suggest that there is increased diversity within the radiology trainee population, as this group had an increase in representation of sexual identity, sexual orientation, being non-white, and being a visible minority. These findings are consistent with results from a 2014 study that reported a significant difference in the distribution of individuals underrepresented in medicine (i.e., blacks, Hispanics, Native Americans, Alaskan Natives, Native Hawaiians, and Pacific Islanders) in the United States, with higher rates of representation present in radiology residents when compared to practicing radiologists [19]. While the findings of increased representation of diversity in trainees is heartening, underrepresentation of minority groups across a number of demographic characteristics in radiology trainees persists. The same study from 2014 acknowledged that while there was a historical increase in representation of women and underrepresented minority groups in radiology residents in the United States, no significant change over the preceding decade was observed.
Physicians with disabilities offer unique insights that can enrich the learning and clinical environment, increase empathy for patients, and provide better care for patients with disabilities. Therefore, collecting data on the presence of radiologists with disabilities is an important variable to assess in the context of improving patient care. In our survey, 12.3% (n = 56) of radiologists and 13.4% (n = 16) of trainees reported that they had one or more disabilities. In comparison, the 2017 Canadian Survey on Disability reported that 22% of the Canadian population over 15 years old had one or more disabilities. Notably, 3.5% (n = 16) of radiologists and 4.2% (n = 5) of trainees in our survey selected “prefer not to say” when asked if they had a disability or long-lasting condition.
The results of our survey demonstrate that there is a relationship between identifying as a woman, identifying as a visible minority, having children, and number of years in practice as a radiologist. Radiologists with more years in practice were more likely to be male, not identify as a visible minority, and were less likely to have children.
Setting target diversity metrics is a potential strategy to measure progress towards a more inclusive and diverse field of radiology. It is imperative to exercise caution to ensure such metrics don't evolve into quotas. Ideally, the field of Radiology would include a proportional representation of individuals who identify as women, non-white, non-heterosexual, with or without children, and individuals with disabilities, among other characteristics.
The methods to set these targets should consider multiple factors. Firstly, national demographic data could serve as a benchmark, providing data on representation. Additionally, the demographic characteristics of the communities served by radiologists should also be factored in, ensuring that the field is representative of the diverse populations it serves. Alongside these demographic considerations, it is vital to ensure that talent, qualifications, and competencies remain the core considerations for any individual's potential to succeed in the field.
5. Limitations
This study has some important limitations. One main limitation is the response rate, 17.4% for Canadian radiologists and 18.9% for residents. Another important limitation is likely sampling bias. Potential areas of bias are: (a) survey distribution (20% of respondents received the survey from a friend, 14% through social media, and 47% from CAR); (b) possible under estimation of response rate (although the denominator of response rate was the total number of Canadian radiologists, it is possible not all Canadian radiologists received the survey) (c) age with possible underrepresentation of radiologists older than 65 (8% of respondents) versus CMA data showing that 15% of Canadian radiologists are older than 65; (d) gender with women over-represented in the sample (51% of our respondents), while women represent 32% of Canadian radiologists; and (e) the proportion of women/minority/or academic radiologists or trainees may be under-represented as those who are members of CAR are not known. Another important limitation highlighted by the study is the underrepresentation of responses from radiologists practicing in the northern parts of Canada, and there are several underlying reasons that could account for this discrepancy. The distinct demographic and geographic nature of northern Canada plays a significant role in this underrepresentation. Specifically, the northern regions of Canada are characterized by lower population densities. Consequently, fewer radiologists practice in these areas as compared to other regions, which naturally limits the potential for responses from these remote regions. CAR data has reported 1 radiologist per a population of 100,000 people in the Canadian territories.
Additionally, the methods used to disseminate the survey might have inadvertently contributed to the low response rate. Social media channels or email lists, might not be as accessible or popular among radiologists practicing in northern Canada. This lack of access or usage could have led to these radiologists being unaware of the survey, thereby lowering their response rates.
Moreover, the professional circumstances of radiologists in these remote and rural regions might also affect their participation in surveys. These practitioners might face higher workloads due to a lack of adequate support staff, leaving them with less free time for activities outside their immediate work responsibilities. This increased workload, coupled with possibly limited resources, might discourage these radiologists from participating in surveys. Hence, future studies should aim to devise strategies to improve the participation of underrepresented groups, such as those practicing in northern Canada, to ensure a more balanced and accurate reflection of the Canadian radiology workforce. Additionally, the lack of information about the demographics of applicants to radiology is a limitation. Underrepresentation can only be investigated for individuals within the Canadian radiology workforce, not about potential barriers in the professional pipeline out of medical school to get into Canadian radiology practice.
6. Conclusion
While not comprehensive, this national survey provides the most comprehensive analysis of the demographics of the Canadian radiology workforce to date and can serve as a national baseline of the status of diversity in Canadian radiology. While our results suggest there is increasing diversity among radiology trainees (residents and fellows), there remains significant underrepresentation of minorities and women when compared to the diversity of the Canadian population. There remains great opportunity for improved and ongoing data collection to identify where initiatives to improve diversity in Canadian radiology would be most effective.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution statement
Elizabeth Hillier: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper. Carol Hodgson and Charlotte J Yong-Hing: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper. Kiana Lebel: Performed the experiments; Analyzed and interpreted the data; Wrote the paper. Lucy B Spalluto, Isabelle Trop, Wan Yap, Kathryn E. Darras and Sonali Sharma: Analyzed and interpreted the data; Wrote the paper. Tracey Hillier: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Data availability statement
Data will be made available on request.
Additional information
No additional information is available for this paper.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to acknowledge Kaitlin Zaki-Metias, MD for the map in Fig. 1.
References
- 1.Hewlett S.A., Marshall M., Sherbin L. How diversity can drive innovation. Harv. Bus. Rev. 2013 [Google Scholar]
- 2.Cohen J.J., Gabriel B.A., Terrell C. The case for diversity in the health care workforce. Health Aff. 2002;21:90–102. doi: 10.1377/hlthaff.21.5.90. [DOI] [PubMed] [Google Scholar]
- 3.Fine C., Sojo V. Women's value: beyond the business case for diversity and inclusion. Lancet. 2019;393:515–516. doi: 10.1016/S0140-6736(19)30165-5. [DOI] [PubMed] [Google Scholar]
- 4.Norbash A., Kadom N. The business case for diversity and inclusion. J. Am. Coll. Radiol. 2020;17:676–680. doi: 10.1016/j.jacr.2019.11.018. [DOI] [PubMed] [Google Scholar]
- 5.Hillier E., Keglowitsch K., Panas M., Anderson B., Widder S., Wirtzfeld D. Improving physician diversity and inclusion benefits physicians and patients. CJPL. 2021;7:108–114. doi: 10.37964/cr24736. [DOI] [Google Scholar]
- 6.Allen B.J., Garg K. Diversity matters in academic radiology: acknowledging and addressing unconscious bias. J. Am. Coll. Radiol. 2016;13:1426–1432. doi: 10.1016/j.jacr.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 7.DeBenedectis C.M., Heitkamp D.E., England E., Gaviola G.C., Hirsch J.A., Ho C.P., et al. A program director's guide to cultivating diversity and inclusion in radiology residency recruitment. Acad. Radiol. 2020;27:864–867. doi: 10.1016/j.acra.2019.07.027. [DOI] [PubMed] [Google Scholar]
- 8.Carnes M.M., Fine E., Sheridan J. Promises and pitfalls of diversity statements: proceed with caution. [Miscellaneous article] Acad. Med. 2019;94:20–24. doi: 10.1097/ACM.0000000000002388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bucknor M.D., Villanueva-Meyer J.E., Kumar V., Talbott J.F., Wall S.D., Glastonbury C.M., et al. Diversity and inclusion efforts in university of California, San Francisco radiology: reflections on 3 Years of pipeline, selection, and education initiatives. J. Am. Coll. Radiol. 2019;16:1716–1719. doi: 10.1016/j.jacr.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 10.Spalluto L.B., Arleo E.K., Macura K.J., Rumack C.M. 35 Years of experience from the American association for women radiologists: increasing the visibility of women in radiology. J. Am. Coll. Radiol. 2017;14:426–430. doi: 10.1016/j.jacr.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Spottswood S.E., Spalluto L.B., Washington E.R., Donnelly E.F., Birch A.A., Bradshaw M.L., et al. Design, implementation, and evaluation of a diversity program for radiology. J. Am. Coll. Radiol. 2019;16:983–991. doi: 10.1016/j.jacr.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Cater S.W., Yoon S.C., Lowell D.A., Campbell J.C., Sulioti G., Qin R., et al. Bridging the gap: identifying global trends in gender disparity among the radiology physician workforce. Acad. Radiol. 2018;25:1052–1061. doi: 10.1016/j.acra.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 13.Lebel K., Hillier E., Spalluto L.B., Yap W., Keglowitsch K., Darras K.E., et al. The status of diversity in Canadian radiology—where we stand and what can we do about it. Can. Assoc. Radiol. J. 2020 doi: 10.1177/0846537120978258. [DOI] [PubMed] [Google Scholar]
- 14.Khatchikian A.D., Spalluto L.B., Patlas M.N., Yong-Hing C.J. Canadian association of radiologists commitment to equity, diversity and inclusion in Canadian radiology. Can. Assoc. Radiol. J. 2022 doi: 10.1177/08465371221112663. [DOI] [PubMed] [Google Scholar]
- 15.Canadian Medical Association Diagnostic Radiology Profile. 2019 [Google Scholar]
- 16.The Canadian Medical Association New Strategic Plan:CMA 2020 n.d.:14..
- 17.Yap W.W., Hodgson C.S., Spalluto L., Lebel K., Trop I., Hillier E., et al. Canadian radiology gender pay gap-reality or myth? Can. Assoc. Radiol. J. 2022 doi: 10.1177/08465371221132465. [DOI] [PubMed] [Google Scholar]
- 18.Raskin M.M. Of a certain age: When are radiologists too old to practice? AR. 2018:6–7. doi: 10.37549/AR2534. [DOI] [Google Scholar]
- 19.Chapman C.H., Hwang W.-T., Both S., Thomas C.R., Deville C. Current status of diversity by race, hispanic ethnicity, and sex in diagnostic radiology. Radiology. 2014;270:232–240. doi: 10.1148/radiol.13130101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.