Abstract
Study design
Retrospective cross-sectional study.
Objective
To investigate the prevalence, characteristics, and risk factors of spine-related malpractice claims in China in a 2-year period.
Methods
The arbitration files of the Chinese Medical Association (CMA) were reviewed for spine-related malpractice claims. Descriptive statistics and correlation analysis were conducted on claim characteristics, clinical data, plaintiff’s main allegations, and arbitration outcomes.
Results
A total of 288 cases of spinal claims filed in the CMA between January 2016 and December 2017 were included. Most claims were found in lumbar degenerative disorders (59.4%), lumbar trauma (13.2%), and cervical degenerative disorders (11.8%). The most common adverse events (AEs) leading to claims were new neurologic deficit (NND) (47.6%), infection (11.5%), and insufficient symptom relief (10.4%). The most common patient allegation was surgical error (66.0%), although the main arbitrated cause of AEs was disease/treatment itself (49.0%), while providers were judged as mainly responsible in only 47.3% cases. In multivariate regression analysis, cervical spine, misdiagnosis/mistreatment, and unpredictable emergency correlated with more severe damage to patients; minimally invasive surgery was predictive of judgment in plaintiff’s favor, while claims in the eastern region and unpredictable emergencies were predictive of defendant’s favor; only NND was associated with being arbitrated as surgical error in surgical cases where surgeons accepted major liability.
Conclusion
The current study provided a descriptive overview and risk factor analysis of spine-related malpractice claims in China. Gaining improved understanding of the facts and causes of malpractice claims may help providers reduce the risk of claims and subsequent litigation.
Introduction
The Hippocratic Oath, held sacred by physicians for thousands of years, is full of useful guidelines to keep both physicians and their patients out of trouble. However, when a medical professional performs the job in a way that deviates from the standard of care and thereby causes damage or dissatisfaction to patients, medical malpractice claims often arise. As marked monetary, emotional, and temporal burdens for clinicians, malpractice claims come not only from actual negligence but also from other non-technical factors such as miscommunication or economic reasons. The motivation for most malpractice claims is not just the expected compensation but also the patients’ need to find out what has actually happened to them. 1 In China, there are typically four solutions of medical malpractice claims which are as follows: private settlement, meditation by people’s mediation committee (PMC), settlement by health administration, or judicial litigation. However, medical arbitrations are often required prior to these solutions to assess severity, liability, and actual cause of malpractice claims by the arbitration board consisting of clinicians, forensic experts, and healthcare management professionals. Nearly half of court-mandated arbitrations are implemented by medical associations, and the Chinese Medical Association (CMA)—the largest non-governmental medical organization in China—summarizes all arbitration files of medical associations across the nation. 2
Spine surgery represents one of the most litigious subspecialties globally within the current medicolegal landscape for its random functional results as well as certain risks of neurologic complications.3-5 However, limited data are available regarding spine-related malpractice claims in China. This study provided a descriptive overview and risk factor analysis of spine-related malpractice claims by exploring a national medical arbitration database, with the aim to inform risk management in spine patients.
Methods
Data Source and Selection
A retrospective cross-sectional study was conducted by utilizing arbitration database of the CMA from January 2016 to December 2017. Duplicate cases, irrelevant cases, or cases with insufficient information were excluded.
Data Extraction and Synthesis
The information of each arbitration report included four elements which are the following: litigation characteristics, clinical data, plaintiff’s main allegation, and arbitration outcomes. Litigation characteristics included grade of defendant institutions, grade of arbitrating medical association, and geographic distribution of defendant institutions. 6 Clinical data included treatment/diagnosis, types of practice, and the suspected adverse events (AEs). Plaintiff’s main allegation referred to the main problem of surgeons perceived by the patients. Arbitration outcomes included severity of damage, liability distribution, and main cause of the AE (for details see Supplementary File 1).
For the purpose of identifying the risk factors of unfavorable arbitration results for the providers, the arbitration outcomes were further classified into dichotomous variables. The severity of damage to the patient was further classified as major (grades one and two) and minor (grades three and four), and the liability distribution was further classified as plaintiff’s favor (providers accepted no less than 50% liability) and defendant’s favor (providers accepted less than 50% liability). Furthermore, to investigate the actual cause of surgical cases in favor of plaintiffs, the main cause of AE was categorized into surgical error and non-surgical error.
Data were collected by two researchers (YL and SMS) independently using Excel 2016 (Microsoft, Redmond, WA, USA) and were then checked and merged by a third researcher (MGZ). If any recording of the first two researchers was inconsistent, consensus-based decision was then implemented by all authors.
Statistical Analysis
An independent statistician (SMX) performed statistical analysis using SPSS 23.0 software (IBM, Armonk, NY, USA). Categorical variables were compared using the χ2 test or Fisher’s test, as appropriate. For significant variables, multivariate analysis was performed using binary logistic regression in the imputed datasets and fitted for the outcome of arbitration, controlling for available variables. Variables with observed frequency of zero in univariate analysis were not included in multivariate analysis. The results reported here represent the pooled coefficients and 95% confidence intervals (CIs). All statistical analyses were performed by two-sided tests, and P < .05 was considered statistically significant. Data were anonymized regarding all involved parties, and the study was deemed exempt from informed consent under the approval by our institutional review board (IRB number: 2019-057).
Results
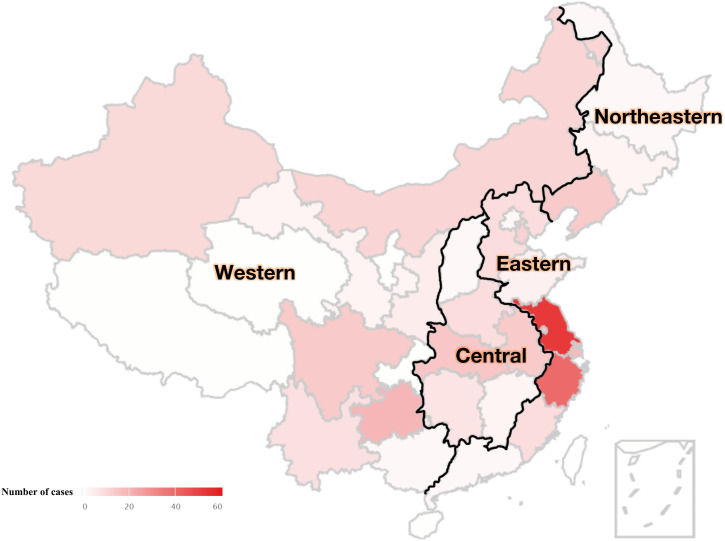
A total of 344 cases of spine-related malpractice claims spanning 26 provinces were filed in the CMA from January 2016 to December 2017 (Figure 1). After excluding 26 duplicated cases, 24 cases with spinal diseases but irrelevant to claims, and six cases with insufficient information, a total of 288 claims were included in the final analysis.
Figure 1.
Geographical distribution map and corresponding spine-related malpractice claims of 26 provinces in China from January 2016 to December 2017.
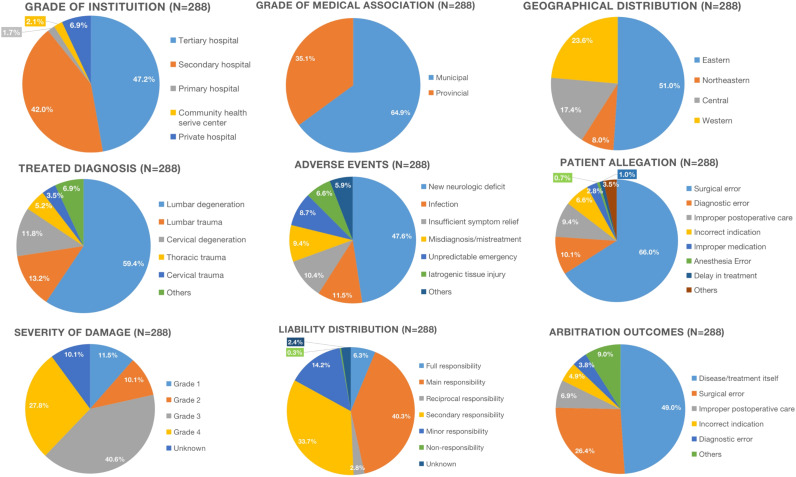
Summary of Arbitration Reports
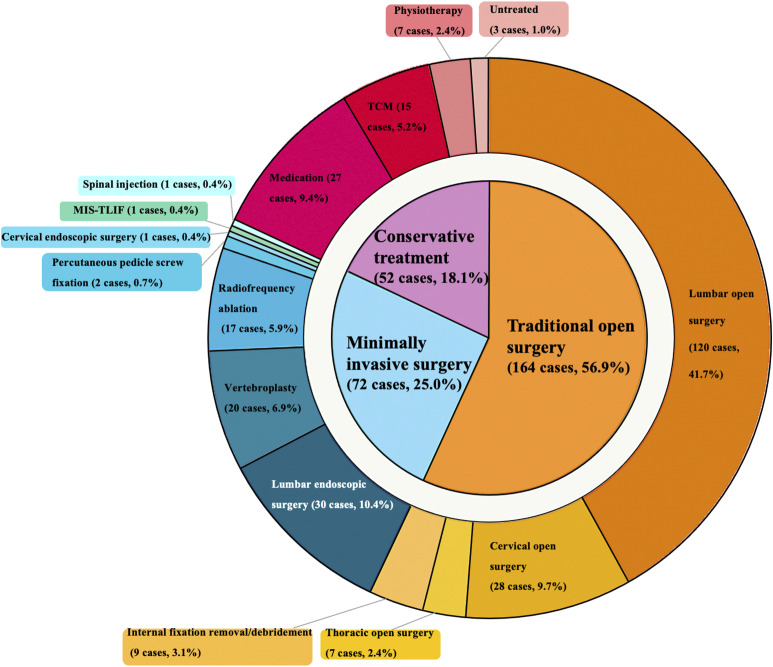
Figure 2 illustratively describes litigation characteristics, clinical data, plaintiff’s main allegation, and arbitration outcomes. Geographically, 147 cases were from the eastern, 23 cases were from the northeastern, 50 cases were from the central, and 68 cases were from the western China. Defendant institution included tertiary hospitals (47.2%, 136 cases), secondary hospitals (42.0%, 121 cases), primary hospitals (1.7%, 5 cases), community health service centers (2.1%, six cases), and private hospitals (6.9%, 20 cases). The treatment included traditional open surgery (56.9%, 164 cases), minimally invasive surgery (MIS) (25.0%, 72 cases), and conservative therapies (18.1%, 52 cases). The greatest number of claims was found in lumbar degenerative disorders (59.4%, 171 cases), followed by lumbar trauma (13.2%, 38 cases), and cervical degenerative disorders (11.8%, 34 cases), as shown in Figure 3. Most common AEs leading to claims were new neurologic deficit (NND) (47.6%, 137 cases), infection (11.5%, 33 cases), and insufficient symptom relief (10.4%, 30 cases).
Figure 2.
Pie charts showing the description of litigation characteristics, clinical data, and arbitration outcomes of 288 spine-related malpractice claims in China from January 2016 to December 2017.
Figure 3.
Pie chart showing the distribution of types of practice in malpractice claims involving the spine in China from January 2016 to December 2017.
The most common patient allegation was surgical error (66.0%, 190 cases), although the most common arbitrated cause of AEs was disease/treatment itself (49.0%, 141 cases). The severity of damage to patients in most claims was arbitrated as minor (68.4%, 197 cases), and hospitals and physicians were arbitrated as having major liability in only 47.3% cases. For surgical cases in which doctors took major responsibility, only 56.7% (134 cases) of all cases were arbitrated as actual surgical error.
Analysis of Risk Factors of Arbitration Outcomes
Tables 1 and 2 show the results of risk factor analysis of malpractice claims. Univariate analysis showed that the proportion of major damage to patients was higher in the following claims: tertiary hospitals [37 cases (59.7%) vs 85 cases (43.1%), P = .023], cervical region [20 cases (32.3%) vs 26 cases (13.2%), P < .001], patient death [26 cases (41.9%) vs 0 (0%), P < .001], misdiagnosis/mistreatment [10 cases (16.1%) vs 14 cases (7.11%), P = .033], and unpredictable emergency [14 cases (22.6%) vs 10 cases (5.08%), P < .001]; but it was lower in degenerative disorders [37 cases (59.7%) vs 153 cases (77.7%), P = .005]. Multivariate analysis revealed that claims involving misdiagnosis/mistreatment (OR, 2.968; 95% CI, 1.143–7.709; P = .025) and unpredictable emergencies (OR, 5.380; 95% CI, 2.094–13.821; P < .001) were associated with major damage. Moreover, cervical spine, compared with lumbar spine (OR, 2.792; 95% CI, 1.317–5.919; P = .007), was more predictive of major damage.
Table 1.
Univariate Analysis of Dispute Characteristics and Outcomes of Spine-Related Malpractice Claims in China from January 2016 to December 2017.
| Severity of damage to patients | P | Liability distribution | P | Cause of adverse events | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| Major n = 62 | Minor n = 197 | Plaintiff’s favor n = 134 | Defendant’s favor n = 149 | Surgical error n = 76 | Non-surgical error n = 58 | ||||
| Grade of defendant institution | |||||||||
| Non-tertiary | 25 (40.3%) | 112 (56.9%) | .023 | 79 (59.0%) | 70 (47.0%) | .044 | 47 (61.8%) | 32 (55.2%) | .437 |
| Tertiary | 37 (59.7%) | 85 (43.1%) | 55 (41.0%) | 79 (53.0%) | 29 (38.2%) | 26 (44.8%) | |||
| Geographical distribution | |||||||||
| Eastern | 28 (45.2%) | 94 (47.7%) | .443 | 51 (38.1%) | 91 (61.1%) | <.001 | 26 (34.2%) | 25 (43.1%) | .339 |
| Northeastern | 3 (4.84%) | 20 (10.2%) | 19 (14.2%) | 4 (2.68%) | 13 (17.1%) | 6 (10.3%) | |||
| Central | 11 (17.7%) | 35 (17.8%) | 32 (23.9%) | 18 (12.1%) | 21 (27.6%) | 11 (19.0%) | |||
| Western | 20 (32.3%) | 48 (24.4%) | 32 (23.9%) | 36 (24.2%) | 16 (21.1%) | 16 (27.6%) | |||
| Grade of medical association | |||||||||
| Provincial level | 23 (37.1%) | 59 (29.9%) | .291 | 40 (29.9%) | 57 (38.3%) | .137 | 20 (26.3%) | 20 (34.5%) | .306 |
| Municipal level | 39 (62.9%) | 138 (70.1%) | 94 (70.1%) | 92 (61.7%) | 56 (73.7%) | 38 (65.5%) | |||
| Spinal region | |||||||||
| Cervical | 20 (32.3%) | 26 (13.2%) | <.001 | 19 (14.2%) | 28 (18.8%) | .197 | 6 (7.89%) | 13 (22.4%) | .055 |
| Thoracic | 8 (12.9%) | 12 (6.09%) | 14 (10.4%) | 8 (5.37%) | 8 (10.5%) | 6 (10.3%) | |||
| Lumbar | 34 (54.8%) | 159 (80.7%) | 101 (75.4%) | 113 (75.8%) | 62 (81.6%) | 39 (67.2%) | |||
| Type of practice | |||||||||
| Traditional open | 37 (59.7%) | 111 (56.3%) | .898 | 68 (50.7%) | 93 (62.4%) | .001 | 44 (57.9%) | 24 (41.4%) | .019 |
| Minimally invasive | 15 (24.2%) | 52 (26.4%) | 48 (35.8%) | 24 (16.1%) | 27 (35.5%) | 21 (36.2%) | |||
| Non-operative | 10 (16.1%) | 34 (17.3%) | 18 (13.4%) | 32 (21.5%) | 5 (6.58%) | 13 (22.4%) | |||
| Treated diagnosis as degenerative disorders | |||||||||
| No | 25 (40.3%) | 44 (22.3%) | .005 | 37 (27.6%) | 39 (26.2%) | .785 | 22 (28.9%) | 15 (25.9%) | .692 |
| Yes | 37 (59.7%) | 153 (77.7%) | 97 (72.4%) | 110 (73.8%) | 54 (71.1%) | 43 (74.1%) | |||
| Patient death | |||||||||
| No | 36 (58.1%) | 197 (100%) | <.001 | 124 (92.5%) | 131 (87.9%) | .194 | 76 (100%) | 48 (82.8%) | .001 |
| Yes | 26 (41.9%) | 0 (.00%) | 10 (7.46%) | 18 (12.1%) | 0 (.00%) | 10 (17.2%) | |||
| Misdiagnosis/mistreatment | |||||||||
| No | 52 (83.9%) | 183 (92.9%) | .033 | 124 (92.5%) | 132 (88.6%) | .259 | 76 (100%) | 48 (82.8%) | .001 |
| Yes | 10 (16.1%) | 14 (7.11%) | 10 (7.46%) | 17 (11.4%) | 0 (.00%) | 10 (17.2%) | |||
| New neurologic deficit | |||||||||
| No | 37 (59.7%) | 103 (52.3%) | .308 | 59 (44.0%) | 89 (59.7%) | .008 | 20 (26.3%) | 39 (67.2%) | <.001 |
| Yes | 25 (40.3%) | 94 (47.7%) | 75 (56.0%) | 60 (40.3%) | 56 (73.7%) | 19 (32.8%) | |||
| Unpredictable emergency | |||||||||
| No | 48 (77.4%) | 187 (94.9%) | <.001 | 130 (97.0%) | 128 (85.9%) | .001 | 76 (100%) | 54 (93.1%) | .070 |
| Yes | 14 (22.6%) | 10 (5.08%) | 4 (2.99%) | 21 (14.1%) | 0 (.00%) | 4 (6.90%) | |||
| Additional surgery needed | |||||||||
| No | 37 (59.7%) | 91 (46.2%) | .064 | 67 (50.0%) | 74 (49.7%) | .955 | 32 (42.1%) | 35 (60.3%) | .036 |
| Yes | 25 (40.3%) | 106 (53.8%) | 67 (50.0%) | 75 (50.3%) | 44 (57.9%) | 23 (39.7%) | |||
Table 2.
Multivariate Analysis of Dispute Outcomes of Spine-Related Malpractice Claims in China From January 2016 to December 2017.
| Arbitrated as major damage n = 259 | Arbitrated as plaintiff’s favor n = 283 | Arbitrated as actual surgical error n = 134 | ||||
|---|---|---|---|---|---|---|
| Variable | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P |
| Tertiary hospital, yes vs. no | 1.861 (.983–3.523) | .056 | .714 (.414–1.232) | .226 | — | — |
| Geographical distribution | — | — | — | <.001 | — | — |
| Northeastern vs. eastern | — | — | 9.434 (2.882–30.876) | <.001 | — | — |
| Central vs. eastern | — | — | 3.268 (1.598–6.683) | .001 | — | — |
| Western vs. eastern | — | — | 2.026 (1.067–3.845) | .031 | — | — |
| Spinal segment | — | .023 | — | — | — | — |
| Cervical vs. lumbar | 2.792 (1.317–5.919) | .007 | — | — | — | — |
| Thoracic vs. lumbar | 1.885 (.606–5.862) | .273 | — | — | — | — |
| Type of practice | — | — | — | .006 | — | .188 |
| Traditional open vs. minimally invasive | — | — | .389 (.203–.744) | .004 | 1.995 (.846–4.703) | .114 |
| Non-operative vs. minimally invasive | — | — | .310 (.135–.713) | .006 | .861 (.220–3.377) | .830 |
| Treated diagnosis as degenerative disorders, yes vs. no | .645 (.305–1.365) | .252 | — | — | — | — |
| Misdiagnosis/mistreatment, yes vs. no | 2.968 (1.143–7.709) | .025 | — | — | — | — |
| New neurologic deficit, yes vs. no | — | — | 1.606 (.925–2.787) | .092 | 5.719 (2.522–12.971) | <.001 |
| Unpredictable emergency, yes vs. no | 5.380 (2.094–13.821) | <.001 | .286 (.088–.928) | .037 | — | — |
| Additional surgery needed, yes vs no | — | — | — | — | 1.604 (.723–3.556) | .245 |
Abbreviations: OR: odds ratio; CI: confidence interval.
Differences in liability distribution were noticed between different grades of defendant institution (P = .044), geographical regions (P < .001), and types of practice (P = .001). The proportion of outcomes in plaintiff’s favor was higher in cases of NND [75 cases (56.0%) vs 60 cases (40.3%), P = .008], but lower in unpredictable emergency [four cases (2.99%) vs 21 cases (14.1%), P = .001] claims. Multivariate analysis showed that MIS was an independent risk factor for the outcome in plaintiff’s favor (P < .05), while claims in eastern China were a predictor of defendant’s favor (P < .01). Besides, unpredictable emergency (OR, .286; 95% CI, .088–.928; P = .037) was a powerful indicator of arbitration in defendant’s favor.
For arbitration outcomes of actual surgical error in surgical cases, difference was noticed between different types of practices (P = .019). A higher percentage of surgical error was associated with NND [56 cases (73.7%) vs 19 cases (32.8%), P < .001] and additional surgeries [44 cases (57.9%) vs 23 cases (39.7%), P = .036], while patient death [0 (.00%) vs 10 cases (17.2%), P = .001] and misdiagnosis/mistreatment [0 (.00%) vs 10 cases (17.2%), P = .001] were related to lower proportion of actual surgical negligence outcomes. However, only NND was found to be an independent risk factor of actual surgical error (OR, 5.719; 95% CI, 2.522–12.971; P < .001) by logistic regression.
Discussion
Medical malpractice claim and its perceived deterrence are increasingly affecting health professionals in many countries, including China. According to the 2016 China Health Statistical Yearbook, the number of physicians in China was 2.65 million, and the number of malpractice lawsuits was 21,480; therefore, it has been estimated that annually at least every 123 physicians face one malpractice lawsuit. 7 Meanwhile, professional liability insurance has no coverage for most Chinese medical professionals; hence, compensation expenses are often covered by medical staff and institutions themselves. Therefore, overburdened physicians are often forced to practice “defensive medicine” by ordering unnecessary tests and procedures to minimize the risk of malpractice claims. However, this only leads to the increase of medical care costs as well as resentment in patients, which in turn favors lawsuits, creating a vicious circle. 8 The purpose of treatment of spinal diseases is pain relief and/or functional recovery; however, dramatic and rapid improvement after treatment is often expected by patients or their next of kin. Spinal surgery typically encounters more technical challenge as well as higher neurological hazards compared with other surgical specialties; it represents one of the most risky subspecialties in the USA, France, the UK, Germany, and Sweden (see Table 3).9-13 The current investigation presents a detailed description and analysis of spine-related medical litigation in mainland China representing a coverage of 1.35 billion inhabitants. This study is the first, to our knowledge, to describe and analyze spine-related medical malpractice in China.
Table 3.
Summary of Literature Detailing Spine-Related Malpractice Litigation.
| Author year | Country | Sample size | Time period | Data source | Spinal region | Pathologies | Patient allegations |
|---|---|---|---|---|---|---|---|
| Öhrn et al (2011) | Sweden | 182 | 2003–2005 | County Councils’ Mutual Insurance Company and Swespine | NM | Dural lesion (28.8%) | NM |
| Wound infection (21.6%) | |||||||
| Nerve tear (15.8%) | |||||||
| Machin et al (2018) | England | 978 | 2012–2017 | National Health Service (NHS) Resolution database | NM | Iatrogenic nerve damage (23%) | Judgment/timing (52.35%) |
| Cauda equina syndrome (22.82%) | Interpretation of results/clinical picture (26.07%) | ||||||
| Inadequate decompression (15.85%) | Unsatisfactory outcome to surgery (19.63%) | ||||||
| Quraishi et al (2012) | England | 235 | 2002–2010 | NHS Litigation Authority (NHSLA) database | NM | Missed fractures (19.14%) | NM |
| Prolapsed intervertebral disc disease (16.17%) | |||||||
| Infections of the spine (14.46%) | |||||||
| Debono et al (2020) | France | 193 | 2015–2019 | Mutuelle d'Assurances du Corps de Santé Français (MACSF) | Cervical 27 (14.0%) | Decompensation of a preexisting myelopathy (15%) | Surgical negligence (29.5%) |
| Thoracic 11 (5.7%) | Cauda equina syndrome (12.5%) | Delay in diagnosis (18.7%) | |||||
| Lumbar 144 (74.6%) | Radicular injury (10%) | Surgical site infection (16.6%) | |||||
| Multiple 11 (5.7%) | Malposition of cages/prostheses with radiculalgia requiring revision surgery 10%) | ||||||
| Ahmadi et al (2019) | Germany | 340 | 2012–2016 | Review Board of the North Rhine Medical Council (NRMC) | NM | New neurological deficit (37.6%) | NM |
| Chronic pain (22.1%) | |||||||
| Insufficient symptom relief (15%) | |||||||
| Agarwal et al (2018) | USA | 98 | 2010–2015 | Westlaw online legal database | Cervical 22 22.5%) | NM | Lack of informed consent (29.9%) |
| Thoracic 7 (7.1%) | Failure to diagnose (19.5%) | ||||||
| Lumbar 45 (45.9%) | Failure to treat (20.8) | ||||||
| Sacral 1 (1%) | |||||||
| Not specified 23 (23.5%) | |||||||
| Grauberger et al (2017) | USA | 233 | 1980–2015 | WestlawNext database | Cervical 52 (22.3%) | NM | Surgical negligence (30.1%) |
| Thoracic 8 (3.4%) | Failure to diagnose or treat (20.7%) | ||||||
| Lumbar 132 (56.7%) | General malpractice (12.2%) | ||||||
| Not specified 41 (17.6%) | |||||||
| Makhni et al (2018) | USA | 103 | 2010 - 2014 | WestlawNext database | Cervical 27 (26.21%) | NM | Technical or judgment (65.05%) |
| Thoracic 8 (7.67%) | Nerve injury (40.77%) | ||||||
| Lumbar 64 (62.14%) | Lack of informed consent (33.98%) | ||||||
| Not specified 4 (3.88%) |
Abbreviations: NM: not mentioned.
Geographical Risks of Malpractice Claims
The present investigation showed that most malpractice claims occurred in the eastern region, especially in Jiangsu (52 cases, 18.1%) and Zhejiang (39 cases, 13.5%). Similar situation was found in the US, where litigation originated in the most populated states (New York, California, Texas, Ohio, Massachusetts, Pennsylvania, Florida, and Washington), and in Germany (the North Rhine).12,14,15 However, we also found that providers were less likely to be arbitrated with major liability in the eastern region. Apart from the uneven distribution of population and medical resources, other factors might contribute to the observed contradiction. First, as reported by Wang et al, 16 eastern China has higher incidence of medical malpractice litigation per million population and per 1000 physicians compared with other parts of China; however, scholars attributed the geographical differences partly to better legally armed population in developed areas. In addition, Barbieri et al proposed that patients of lower socioeconomic status are less likely to file claims, 17 which could partly explain the reluctance to sue in less developed areas. It should be noted that, however, during the inspected time frame, the malpractice claims in Jiangsu and Zhejiang were more inclined to resolving through medical associations than other appraisal approaches, compared with other provinces in China. 18
Patients’ Allegations vs Arbitration Outcomes
The current study indicated that surgical error (66.0%, 190 cases) was the major plaintiff allegation, which is similar to previous studies.5,19,20 However, arbitration boards judged that only 26.4% (76 cases) of AEs were caused by actual surgical errors, while the main cause of AEs was disease/treatment itself (49.0%, 141 cases) (ie, the AE was mainly due to natural progress of the diseases or inevitable complications of treatment, other than physicians’ errors). This is consistent with the findings from the study by Ahmadi et al 12 in which 65.4% of the patients perceived their spinal surgeries as improper or erroneous, while only 26.2% were judged as treatment errors by the advisory committee. Such a divergence could be largely explained by individual nature of the patient–physician relationship, as 37–40% of medical disputes had no actual medical technical errors and up to 64.4% of disputes resulted from miscommunication.15,21-23 Grauberger et al 20 noted that the most common informed consent allegations were failure to explain risks/AEs of surgery and failure to explain alternative treatment options. From a risk management perspective, adequate communication consists of informing patients or their families of not just estimates of outcomes (risks, benefits, and harms) but also alternative options and possible countermeasures of AEs, and implementing these contents into a shared decision-making on the both providers’ and patients’ part.
Risk Factors Needing Awareness of Spine Physicians
We noted that some of the risk factors mentioned and, subsequently, some malpractice claims could have been prevented through careful practice or adequate informed consent, such as those related to misdiagnosis/mistreatment and neurological complications. Misdiagnosis refers to wrong diagnosis, missed diagnosis, delayed diagnosis, or failure to utilize the appropriate test, while mistreatment refers to the subsequent treatment based on the misdiagnosis. Among the 27 cases involved in misdiagnosis/mistreatment, interestingly, the majority were cases of trauma (15 cases). We found that misdiagnosis and mistreatment were more likely to result in more severe damage to patients [2.968 (1.143–7.709), P = .025]. A study by Fan et al 24 showed that the mortality rate of misdiagnosed patients was higher than that of the correctly diagnosed patients. Clinicians should be aware of the spinal trauma conditions and take extra precautions to seek and confirm the diagnosis and keep in mind that the difficulty of accurate diagnosis often correlates with the severity of the trauma. NNDs, including treatment-associated nerve root deficit, cauda equina deficit, and spinal cord deficit, had more chances to be arbitrated as surgical error according to our results [5.719 (2.522–12.971), P < .001] 25 . NNDs were not just found in the surgical claims (80 cases of open surgery, 24 cases of endoscopic surgery, 15 cases of percutaneous vertebroplasty, and one case of MIS-TLIF), but also in the medication (two cases), traditional Chinese medical therapies (seven cases), and physiotherapy (three cases). Therefore, there is no treatment related to spine that is absolutely free of neurological injury, as even the commonly perceived “safe” medications led to a spinal cord deficit in one case (pharmacoprophylaxis resulted in intraspinal edema and paralysis). Informing the spine patients of neurological risks is as important as the treatment itself.
However, some risk factors are difficult to avoid, such as unpredictable emergencies, including ischemic stroke (10 cases), acute respiratory failure (five cases), acute venous thromboembolism (four cases), acute cerebral hemorrhage (one case), acute heart failure (one case), acute coronary syndrome (one case), epilepsy attack (one case), and acute renal failure (one case). Despite the fact that those cases were involved in more severe patient damage, arbitration judged most of the unpredictable emergencies (21 cases) in favor of hospitals and physicians. Therefore, for providers, better understanding of risk factors for these dreadful complications would allow them to more accurately advise patients regarding the risks and make optimal treatment plans for spinal diseases.
Cautiousness of Minimally Invasive Surgeries
It is worth noting that although MIS has been proved more advantageous than conventional open surgery in terms of anatomic preservation and complication reduction, MIS is not free of complications or dangers. Indeed, our results showed that the claims related to MIS were more likely to be judged in plaintiffs’ favor, compared with other treatments. Here, MIS cases consisted of endoscopic discectomy (31 cases), percutaneous vertebroplasty (20 cases), radiofrequency ablation (17 cases), transforaminal lumbar interbody fusion (MIS-TLIF) (one case), percutaneous pedicle screw fixation (two cases), and spinal injection (one case), while over half (39 cases) of these cases required additional surgeries. It should be noted that the major cause of endoscopic discectomy claims was NND (24 cases). MIS is technically more demanding than traditional open surgery, while the failure rate of endoscopic discectomy can be as high as 17.1% before dropping to 10.0% after the learning curve has stabilized.26,27 Lu 28 believes that the spinal MIS is immoderately performed in China where many doctors, in order to cater to the patients’ expectations of small incision, often exaggerate the effects of MIS and do not fully inform patients about the possible risks or complications. Moreover, inappropriate indication of MIS decreases the therapeutic effects, which in turn leads to dissatisfaction or litigation, considering that 11.1% of the MIS cases resulted in dissatisfied outcomes in the current study. It is therefore suggested that consciousness should be taken regarding indication as well as communication to minimize risk of litigation in performing MIS for spine patients.
Limitations
Our study has certain limitations. First, data from some provinces were not available, and a considerable number of malpractice claims were arbitrated by judicial authentication agencies, the counterpart of medical associations; thus, our conclusions may not be an exact representation of spinal malpractice claims in China. Second, demographic characteristics, such as gender, age, and ethnicity, were not included in the analysis due to data heterogeneity, which hindered subgroup analysis and further sensitivity verification. Third, the recording of arbitration data was largely categorical but not specific. For example, though NND was recorded as a “yes” or “no,” the severity of the condition was mostly not described. Despite these shortcomings, the data provided are solid, reliable, and of relevance to spine surgeons in China and worldwide.
Conclusion
Spine-related healthcare providers are confronting a conundrum of growing tendency to receive malpractice claims; they consequently perform defensive medicine, leading to even more hostile landscape. Understanding the characteristics and risk factors associated with malpractice claims is of great significance due to their complex essence. To minimize the risk of medicolegal issues, spine physicians should be as cautious in the treatment indication and the whole perioperative process and non-operative treatments as in performing surgeries. The findings of our study may provide reference to protect spinal professionals and reduce the risk of claims and subsequent litigation.
Supplemental Material
Supplemental Material, sj-pdf-1-gsj-10.1177_21925682211041048 for Spine-Related Malpractice Claims in China: A 2-year National Analysis by Lei Yue, Ming-Shuai Sun, Guan-Zhang Mu, Mei-Xia Shang, Ying-Ze Zhang, Hao-Lin Sun and Chun-De Li in Global Spine Journal
Supplemental Material, sj-pdf-2-gsj-10.1177_21925682211041048 for Spine-Related Malpractice Claims in China: A 2-year National Analysis by Lei Yue, Ming-Shuai Sun, Guan-Zhang Mu, Mei-Xia Shang, Ying-Ze Zhang, Hao-Lin Sun and Chun-De Li in Global Spine Journal
Supplemental Material, sj-pdf-3-gsj-10.1177_21925682211041048 for Spine-Related Malpractice Claims in China: A 2-year National Analysis by Lei Yue, Ming-Shuai Sun, Guan-Zhang Mu, Mei-Xia Shang, Ying-Ze Zhang, Hao-Lin Sun and Chun-De Li in Global Spine Journal
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplementary Material: Supplementary material for this article is available online.
ORCID iD
References
- 1.Amirthalingam K. Medical dispute resolution, patient safety and the doctor-patient relationship. Singapore Med J. 2017;58(12):681-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang F, Liu J, Zhou H, Liu P. Inequality in the last resort: how medical appraisal affects malpractice litigations in China. Int J Leg Med. 2021;135(3):1047-1054. [DOI] [PubMed] [Google Scholar]
- 3.Din RS, Yan SC, Cote DJ, Acosta MA, Smith TR. Defensive medicine in U.S. spine neurosurgery. Spine. 2017;42(3):177-185. [DOI] [PubMed] [Google Scholar]
- 4.Jackson KL, Rumley J, Griffith M, Linkous TR, Agochukwu U, DeVine J. Medical malpractice claims and mitigation strategies following spine surgery. Global Spine J. 2020;7:2192568220939524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Debono B, Gerson C, Houselstein T, et al. Litigations following spinal neurosurgery in France: “out-of-court system,” therapeutic hazard, and welfare state. Neurosurg Focus. 2020;49(5):E11. [DOI] [PubMed] [Google Scholar]
- 6.National Bureau of Statistics of China . 2011. http://www.stats.gov.cn/ztjc/zthd/sjtjr/dejtjkfr/tjkp/201106/t20110613_71947.htm. Accessed Feburary 2, 2021.
- 7.Li Y, Gao D, Liang W, et al. A comparison of malpractice lawsuits mediated and judged in court in China. J Forensic Leg Med. 2018;54:109-113. [DOI] [PubMed] [Google Scholar]
- 8.Tena-Tamayo C, Sotelo J. Malpractice in Mexico: arbitration not litigation. Br Med J Int Ed. 2005;331(7514):448-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dambrino RJ, Zuckerman SL, Guidry BS, et al. Do neurosurgeons receive more patient complaints than other physicians? describing who is most at risk and how we can improve. J Neurosurg. 2020;31:1-8. [DOI] [PubMed] [Google Scholar]
- 10.Guillain A, Moncany AH, Hamel O, et al. Spine neurosurgeons facing the judicialization of their profession: disenchantment and alteration of daily practice-a qualitative study. Acta Neurochir (Wien). 2020;162(6):1379-1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Machin JT, Hardman J, Harrison W, Briggs TWR, Hutton M. Can spinal surgery in England be saved from litigation: a review of 978 clinical negligence claims against the NHS. Eur Spine J. 2018;27(11):2693-2699. [DOI] [PubMed] [Google Scholar]
- 12.Ahmadi SA, Sadat H, Scheufler KM, Steiger HJ, Weber B, Beez T. Malpractice claims in spine surgery in Germany: a 5-year analysis. Spine J. 2019;19(7):1221-1231. [DOI] [PubMed] [Google Scholar]
- 13.Ohrn A, Olai A, Rutberg H, Nilsen P, Tropp H. Adverse events in spine surgery in Sweden: a comparison of patient claims data and national quality register (Swespine) data. Acta Orthop. 2011;82(6):727-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daniels AH, Ruttiman R, Eltorai AEM, DePasse JM, Brea BA, Palumbo MA. Malpractice litigation following spine surgery. J Neurosurg Spine. 2017;27(4):470-475. [DOI] [PubMed] [Google Scholar]
- 15.Agarwal N, Gupta R, Agarwal P, et al. Descriptive analysis of state and federal spine surgery malpractice litigation in the United States. Spine. 2018;43(14):984-990. [DOI] [PubMed] [Google Scholar]
- 16.Wang Z, Li N, Jiang M, Dear K, Hsieh CR. Records of medical malpractice litigation: a potential indicator of health-care quality in China. Bull World Health Organ. 2017;95(6):430-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barbieri JS, Kovarik CL. Physician spending and risk of malpractice claims: what about the effects of socioeconomic status? Bmj. 2015;351:h6765. [DOI] [PubMed] [Google Scholar]
- 18.Lv H, Li D, Li C, et al. Characteristics of the medical malpractice cases against orthopedists in China between 2016 and 2017. PloS One. 2021;16(5):e0248052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Makhni MC, Park PJ, Jimenez J, et al. The medicolegal landscape of spine surgery: how do surgeons fare? Spine J. 2018;18(2):209-215. [DOI] [PubMed] [Google Scholar]
- 20.Grauberger J, Kerezoudis P, Choudhry AJ, et al. Allegations of failure to obtain informed consent in spinal surgery medical malpractice claims. JAMA Surg. 2017;152(6):e170544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shouhed D, Beni C, Manguso N, IsHak WW, Gewertz BL. Association of emotional intelligence with malpractice claims: a review. JAMA Surg. 2019;154(3):250-256. [DOI] [PubMed] [Google Scholar]
- 22.Aoki N, Uda K, Ohta S, Kiuchi T, Fukui T. Impact of miscommunication in medical dispute cases in Japan. Int J Qual Health Care. 2008;20(5):358-362. [DOI] [PubMed] [Google Scholar]
- 23.Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. [DOI] [PubMed] [Google Scholar]
- 24.Fan Y, Bai X-j, Li Z-f. Analysis of misdiagnosis in patients with multiple trauma. Chin J Traumatol. 2011;14(1):20-24. [PubMed] [Google Scholar]
- 25.Hamilton DK, Smith JS, Sansur CA, et al. Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: a report of the scoliosis research society morbidity and mortality committee. Spine. 2011;36(15):1218-1228. [DOI] [PubMed] [Google Scholar]
- 26.Wang H, Zhou Y, Li C, Liu J, Xiang L. Risk factors for failure of single-level percutaneous endoscopic lumbar discectomy. J Neurosurg Spine. 2015;23(3):320-325. [DOI] [PubMed] [Google Scholar]
- 27.Sharif S, Afsar A. Learning curve and minimally invasive spine surgery. World Neurosurg. 2018;119:472-478. [DOI] [PubMed] [Google Scholar]
- 28.Lu G. On the consensus and controversy of minimally invasive concept and technology in spine surgery. Chin J Surg. 2018;56(7):503-506. (in Chinese). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-gsj-10.1177_21925682211041048 for Spine-Related Malpractice Claims in China: A 2-year National Analysis by Lei Yue, Ming-Shuai Sun, Guan-Zhang Mu, Mei-Xia Shang, Ying-Ze Zhang, Hao-Lin Sun and Chun-De Li in Global Spine Journal
Supplemental Material, sj-pdf-2-gsj-10.1177_21925682211041048 for Spine-Related Malpractice Claims in China: A 2-year National Analysis by Lei Yue, Ming-Shuai Sun, Guan-Zhang Mu, Mei-Xia Shang, Ying-Ze Zhang, Hao-Lin Sun and Chun-De Li in Global Spine Journal
Supplemental Material, sj-pdf-3-gsj-10.1177_21925682211041048 for Spine-Related Malpractice Claims in China: A 2-year National Analysis by Lei Yue, Ming-Shuai Sun, Guan-Zhang Mu, Mei-Xia Shang, Ying-Ze Zhang, Hao-Lin Sun and Chun-De Li in Global Spine Journal